
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 17 July 2023
Sec. Stroke
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1206846
 Diandian Huang1
Diandian Huang1 Yuxuan Lu1
Yuxuan Lu1 Yongan Sun1
Yongan Sun1 Wei Sun1
Wei Sun1 Yining Huang1
Yining Huang1 Liwen Tai2
Liwen Tai2 Guozhong Li3
Guozhong Li3 Huisheng Chen4
Huisheng Chen4 Guiru Zhang5
Guiru Zhang5 Lei Zhang6
Lei Zhang6 Xuwen Sun7
Xuwen Sun7 Jinhua Qiu8
Jinhua Qiu8 Yan Wei9
Yan Wei9 Haiqiang Jin1*
Haiqiang Jin1* on behalf of the CASTOR Investigators
on behalf of the CASTOR InvestigatorsBackground: Due to disparities in medical resources in rural and urban areas as well as in different geographic regions in China, the effect of weekend versus weekday admission on the outcomes of acute ischemic stroke (AIS) patients is unknown. Our aim was to investigate whether the outcomes of AIS patients differ according to the day of admission in China.
Methods: The data were extracted from the Chinese Acute Ischemic Stroke Treatment Outcome Registry (CASTOR), a multicenter prospective study database of patients diagnosed with AIS. The chi-square test (χ2) and logistic regression were used to assess mortality for weekday and weekend admissions among AIS patients stratified by rural or urban status and geographic region (including the eastern, northeastern, central, and western regions).
Results: In total, 9,256 patients were included in this study. Of these patients, 57.2% were classified as urban, and 42.8% were classified as rural. A total of 6,760 (73%) patients were admitted on weekdays, and 2,496 (27%) were admitted on weekends. There was no significant difference in the mortality rate among patients admitted on weekends compared with those admitted on weekdays in urban (7.5% versus 7.4%) or rural areas (8.8% versus 8.1%; p > 0.05). The mortality rate was the highest among patients admitted on weekends and weekdays (11.6% versus 10.3%) in the northeastern area, without statistical significance before and after adjusting for the patients’ background characteristics (p > 0.05). In addition, regression analysis revealed that the mortality of patients admitted on weekdays was more likely to be influenced by regional subgroup, hospital level and intravenous thrombolysis than that of patients admitted on weekends.
Conclusion: The weekend effect was not observed in the mortality of patients with AIS regardless of rural–urban status or geographic region in China.
Stroke is the second leading cause of death worldwide (1, 2). The Global Burden of Diseases showed that the annual number of strokes and deaths due to stroke increased substantially from 1990 to 2019 (3). Among the most common types of stroke, acute ischemic stroke (AIS) is the major player (4). Although intravenous thrombolysis and endovascular treatment (EVT) can provide considerable benefits to patients with AIS within a certain time frame (5, 6), stroke ranks as the third leading cause of death in China and is a major component of disability-adjusted life years in China (7).
Stroke mortality is associated with sex and urban and rural disparities in China. According to a previous study, the crude mortality rate for men was higher than that for women. The age-adjusted stroke mortality rates in rural areas are substantially increased compared with those in urban areas (8, 9). The prevalence of stroke was higher in urban areas than rural areas, but the incidence rate and mortality rate of stroke were higher in rural areas than urban areas which illustrated the existence of urban–rural disparity in the burden of stroke in China (10). However, another interesting phenomenon in which the incidence of stroke is increased during off-hour hospital admissions has been dubbed the “weekend effect” (11, 12). A previous study illustrated that this phenomenon was attributed to the decrease in the number of experienced medical service personnel and first-aid provider delays (13), a decline in care quality or a more serious absence of instantaneous neurological deciders (14). Some previous studies have demonstrated the weekend effect, while many studies have reported entirely different results. A study that covered 47,885 patients in Japan found no significant influence on in-hospital mortality by admission day regardless of the initial admission medical ward (15). Another study showed increased mortality owing to weekend emergency admission in Scotland (16). According to the abovementioned reports, it is controversial whether admission to a hospital on a weekday or throughout the weekend leads to a poor prognosis for patients (17).
In China, some studies have explored the weekend effect on acute myocardial infarction (18), subarachnoid hemorrhage (19), and sepsis patients (20). A longer hospital length of stay was observed among stroke patients with weekend admissions in a Taiwanese study (21). A study showed that intracerebral hemorrhage patients admitted during off-hours had a higher risk of poor functional outcomes at 3 months than those admitted during working hours in Chongqing (14). To our knowledge, no study has simultaneously analyzed the weekend effect on mortality among AIS patients by rural and urban differences and regional diversity in stroke care in China. Our study examined the mortality of patients with ischemic stroke independently through data from the Chinese Acute Ischemic Stroke Treatment Outcome Registry (CASTOR) by weekend and weekday admission, rural–urban status and geographic differences to evaluate the influence of the weekend effect throughout China.
The study protocol was approved by the ethics committee of Peking University First Hospital (IRB approval number: 2015[922]) and all participating hospitals. Written informed consent was obtained from all patients or an appropriate family member (if the patient was unable to provide consent).
Data were directly derived from the CASTOR, a multicenter prospective study database. The CASTOR is designed to evaluate the patterns and cost-effectiveness of current treatments for AIS in real-world settings in China (22). A total of 10,002 patients with AIS were recruited in our study; 3 patients were excluded due to the absence of admission day information, 743 patients were excluded because of tracking loss and 9,256 patients were ultimately investigated. The flow chart were added in Figure 1.The experimental project and parameters have been described previously (22). A total of 80 hospitals (including the major tertiary hospitals, sub-tertiary hospitals and the secondary hospitals) participated in our registry, and 35 hospitals (43.75%) had teaching status. It required the National Stroke Center certificate and received guidance from higher-level stroke centers due to the evaluation of the tertiary hospitals required the comprehensive stroke centers (CSC) construction. Secondary hospitals in China were defined as having 100-499 beds, and tertiary hospitals were defined as having more than 500 beds in rural and urban. A total of 5 hospitals were secondary hospitals, and 2 were sub-tertiary hospitals in our study and the rest were major tertiary hospital. A general neurology ward and an intensive care unit (ICU) were evaluated in the investigated hospital. According to the Urban–Rural Classification and Codes (URCC) provided by the China National Bureau of Statistics, which use population and economic development indicators (23), three main urban–rural categories, district, township and countryside, were investigated in our trials. A previous study had the characteristic that cities included only urban areas, excluding counties under the jurisdiction of the cities (24). We defined districts as urban and townships and the countryside as rural.
Therapeutic methods were chosen by the investigators depending on the clinical symptoms, physical signs and medical histories of the patients following the Chinese Guidelines for the Diagnosis and Treatment of Acute Ischemic Stroke (25).
The main outcome of our study was mortality, a binary variable that was evaluated and defined by the Modified Rankin Scale (mRS) score at discharge and 90 days after the ischemic stroke event. The primary predictor variable was the date of admission. Admission on a Saturday or Sunday was coded as 1, and admission from Monday to Friday was coded as 0. The secondary predictor variable included rural–urban location and regional diversity among AIS patients. Regional distribution was divided into four groups: the eastern region, northeastern region, central region and western region (26) (Figure 2).
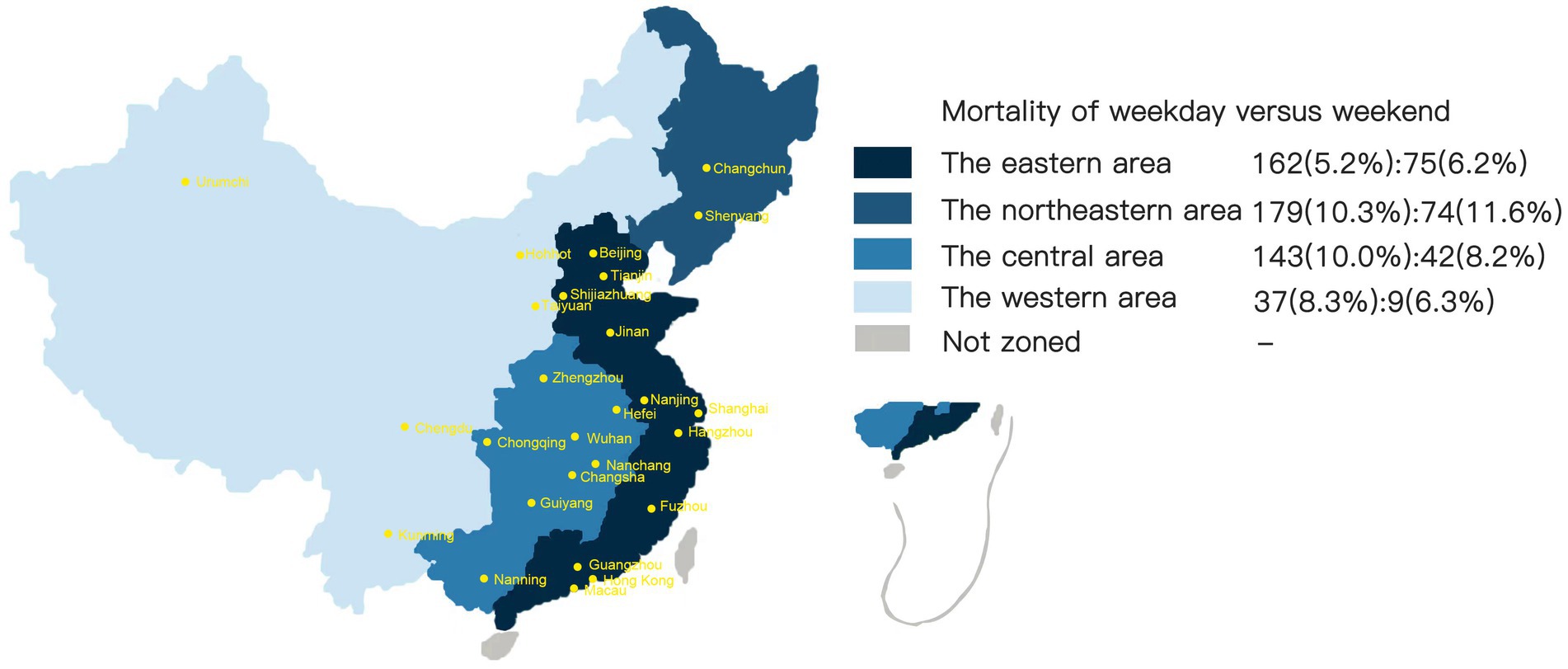
Figure 2. Mortality of acute ischemic stroke patients in different regions of China divided by weekend and weekday admissions.
The confounding variables were sex, age, payment type, in-hospital complications, hospital level, ICU admission, National Institutes of Health Stroke Scale (NIHSS) score on admission, Charlson Comorbidity Index score and thrombolysis.
The age groups were classified as 18–44 years, 45–64 years, 65–74 years, and 75 years and older. Payment type was mainly separated into two groups: the self-pay group and the medical insurance group. In-hospital complications included infection, deep venous thrombosis, cardiac events and hemorrhage. The designation of in-hospital complications was identical to that in previous studies (27). Infection mainly included pulmonary infection, urinary infection and so on. Hemorrhage primarily occurred in the gastrointestinal tract and urinary and integumentary systems, and hemorrhagic stroke stemmed from ischemic stroke (28). Hospital level was separated into tertiary hospitals and secondary hospitals. Tertiary hospitals (with more than 501 beds) were defined as regional and advanced medical service centers that provide comprehensive medical services for patients and perform advanced education and scientific research tasks within the region and surrounding areas. Secondary hospitals (with more than 100 beds) were defined as regional hospitals that are county centered, provide urgent and preventative medical services to multiple communities for over 10,0000 patients and perform certain teaching and research tasks (26). NIHSS scores were ascertained on the date of admission, and patients were divided into mild (0–5), moderate (6–10) and severe (> 10) groups (29). The Charlson Comorbidity Index was the primary evaluation method for the number of comorbidities, and patients were divided into two groups: a group with 1 comorbidity and a group with 2 or more comorbidities. Comorbidities in our study were classified as prior stroke, hypertension, coronary heart disease (CHD), diabetes mellitus (DM), and atrial fibrillation (AF). Prior stroke included ischemic stroke and hemorrhagic stroke. Hypertension was defined as a diagnostic history of increased arterial blood pressure (systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg) on two subsequent occasions or the use of antihypertensive drugs. DM was defined as a history of increased blood glucose levels on two substantive occasions or the use of drugs for DM. CHD was classified as any previous heart attack and/or myocardial infarction, angina, or coronary heart disease. AF was defined as previous AF or AF determined with ECG during the hospital stay. In the CASTOR investigation, the mRS scores were evaluated in the admission day, the discharge day, and the 90 days and the 360 day of occurrence, respectively. We use the mRS score for binary selection, selection only included the death and alive.
Statistical analysis was performed by evaluating the complete data and excluding patients with missing data (9,256 patients were ultimately enrolled). ICD-10 codes and the HCUPNet recommended coding instructions1 were used to evaluate stroke patients independently, and the two methods were used equally.
First, we investigated the background characteristics of the patients categorized by the day of admission and AIS mortality by personal-and hospital-level factors using Pearson’s Chi-square test (χ2).
Then, logistic regression was conducted for mortality between AIS patients with weekend and weekday admissions, modified by sex, age, payment type, medical history, location (urban and rural), in-hospital complications, geographic region, hospital level, ICU admission, NIHSS score at admission and thrombolysis. These confounding variables were selected based on a previous study that illustrated differences in mortality by patient variance and distinct Chinese hospital characteristics (29, 30). SPSS (version 27.0) software was used for statistical analysis.
9,256 patients were included in our study ultimately. For the CASTOR results, in the rural AIS patients, 90.2% were admitted to major tertiary hospitals (n = 4,771), 2.2% were admitted to sub-tertiary hospitals (n = 119) and 7.6% were admitted to secondary hospitals (n = 402). In the urban AIS patients, 90.0% were admitted to major tertiary hospitals (n = 3,569), 1.8% were admitted to sub-tertiary hospitals (n = 70) and 8.2% were admitted to secondary hospitals (n = 325). The percentages of AIS patients living in rural and urban areas and in separated geographic regions are shown in Figure 3. The mortality rate in the mild group was 6.5% (n = 5,882), the mortality rate in the moderate group was 7.4% (n = 2,112), and the mortality rate in the severe group was 14.3% (n = 1,259).
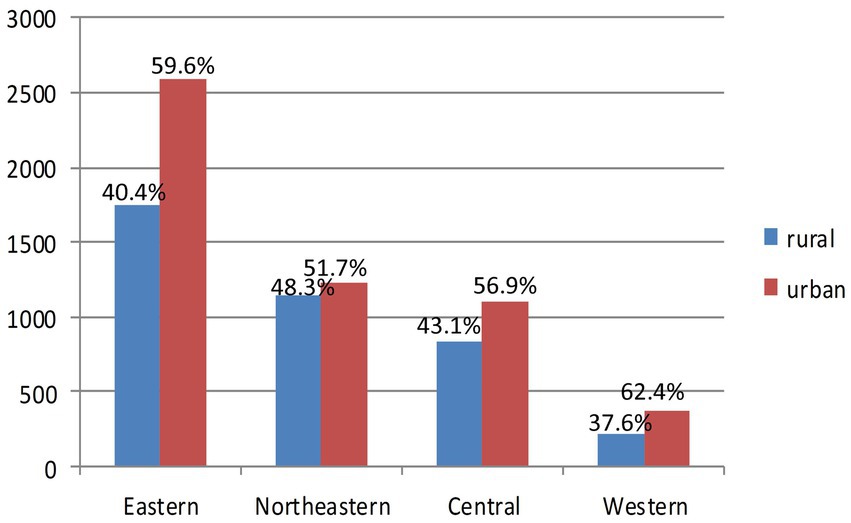
Figure 3. Comparison between rural and urban acute ischemic stroke (AIS) patients in the regional groups.
The background characteristics of AIS patients by weekday versus weekend admission and mortality are presented in Table 1. Approximately 60% of all admissions and deaths occurred among males. Over 65% of the patients were male, and most patients were aged 45–64 years, accounting for 40.6% of deaths. Payment type did not show a discrepancy in mortality between patients with weekday admissions and those with weekend admissions. More than 90% of patients were admitted to a major tertiary hospital. ICU admissions were increased on weekends (5.7%) compared with weekdays (3.3%), which was statistically significant (p < 0.05). NIHSS scores showed that over 60% of the participants had a mild case of stroke. There was no obvious statistically significant difference in the number of patients who received thrombolysis therapy between patients admitted on weekends and weekdays (p > 0.05). In addition, there was no statistical significance between weekday and weekend admission AIS patients who underwent thrombectomy in our study.

Table 1. Patient characteristics by weekday versus weekend admission and stroke mortality among patients with ischemic stroke in the CASTOR database (n = 9,256).
The χ2 tests for subgroup analyses of the weekend effect revealed no difference between patients from urban and rural areas (Table 2) or in regional variance (Table 3, Figure 2). After adjusting for confounding variables, the difference in mortality by urban–rural status or regional subgroup was not statistically significant. Table 3 also shows that the northeastern region had the highest mortality on weekdays (10.3%) and weekends (11.6%) compared to other regions.
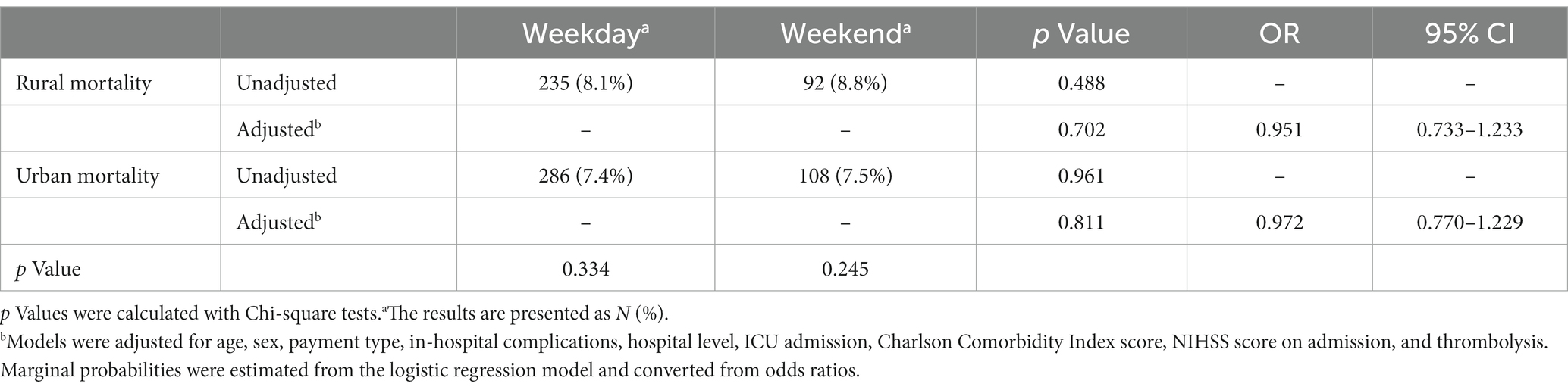
Table 2. Mortality between weekday and weekend admissions among ischemic stroke patients by rural–urban status.
Overall, logistic regression for the confounding variables, including the hospital level, thrombolysis and regional subgroups, suggested significant differences (p < 0.05) in the analyses of mortality on weekdays compared with weekends (Table 4).
The overall mortality rate in our study was 7.8%, with rates of 7.4% for urban patients and 8.2% for rural patients with AIS. The mortality rate among AIS patients in our study was similar to that in a study from Japan (15) but higher than that in a study from the United States (31). The mortality rate of the group with a mild NIHSS score was 6.3%, which was in line with the range of the previous study, which ranged from 9.4% (mechanical thrombectomy group) to 3.5% (best medical management group) (32). There was no rural–urban difference in the mortality rate between patients admitted on weekdays and weekends in our study; this was contrary to the urban–rural bias in China reported in another study, which disregarded the date difference (33). A Korean study investigated 8,957 AIS patients and reported that the weekend effect on ischemic stroke patients was associated with increased in-hospital and 30-day mortality rates, while the 7-day mortality rate showed no statistical significance, which was partially in accordance with our study (34). In China, Ding et al. stated that off-hours admission was related to latency in the reperfusion time of EVT among AIS patients, but the delay was not associated with deteriorated functional appearance or higher mortality (35). However, their study included only some adult patients with acute large vessel occlusion who received EVT, which did not cover all AIS patients. Regarding regional subgroups, the mortality rate associated with weekday and weekend admissions showed no statistically significant difference (p > 0.05), even though the northeastern area had a higher mortality rate than other geographical areas.
Patient clinical characteristics and backgrounds at admission were practically consistent regardless of admission day, but ICU admission significantly differed between weekdays and weekends. A Japanese study demonstrated a tendency of delaying admission of nonfatal patients from the weekend to a weekday (36). Patients experiencing disease on the weekend are regularly admitted to an ICU due to ICU hospital staffing on these days (15). In addition to ICU admission, the majority of our patients’ characteristics were similar to those of patients in multiple formal studies (37–39).
Multiple studies on the off-hours admissions of patients with cerebrovascular and cardiovascular events have explained the weekend effect (35, 40–44). In a study involving 8 CSCs in the Specialized Programs of Translational Research in Acute Stroke (SPOTRIAS) cohort, the weekend effect was not observed (42). Zha et al. (45) indicated that the off-hours effect could be eliminated by considering clinical consequences and in-hospital workflows in anterior circulation large vessel occlusion patients receiving EVT. Profiting from 7/24 capabilities of stroke expertise, proficient stroke nursing specialists, and neuroimaging abilities, CSCs might eliminate the previously reported weekend effect among AIS patients (37). In addition, neurointerventional groups, which involve neurologists, nurses and cerebrovascular interventional radiologists, could perform multiplex treatment, such as intravenous thrombolysis and EVT (46). These studies elucidated how differences between weekday and weekend admission among stroke patients could be eliminated over time and with different developed treatment methods.
Based on 2016 National Inpatient Sample data, a United States study did not observe a relationship between mortality and admission day among AIS patients with rural–urban diversity, which was attributed to updated investigations and the efforts of modern stroke care quality promotion (31). A study reported that rural AIS patients treated in hospitals in agricultural regions had similar benefits and safety from thrombolytic treatment in Portland and even had a lower chance of intravenous thrombolysis at night, and improvements in telecommunication and patient transport from rural areas during the night weakened the weekend effect (47). A recent study showed that there was no difference in intravenous recombinant tissue plasminogen activator (IV-tPA) treatment times, acute stroke measurement times, or mortality between patients who received delayed or on-time treatment. All-hours telecommunication with stroke experts can ensure appropriate treatment and adequate care for AIS patients regardless of the admission time or day, which could reduce the weekend effect in urban and rural and geographically different areas (48). In China, telemedicine application was shown to accelerate the bed occupancy rate of township health centers in the national range. Furthermore, telemedicine was found to improve the number of annual outpatient visits in Western China and the bed occupancy rate in eastern China, which may contribute to the elimination of the weekend effect in rural and urban areas (49). In addition, the narrowing of the gap between urban and rural mortality might be related to improved health care in rural regions after several poverty alleviation campaigns and increased rural medical insurance coverage after the implementation of the New Rural Cooperative Medical Scheme in 2003 (33). In the stable domestic environment, the increase in public revenue and the updating of the public health system promoted county CSC construction and the training of stroke specialists. Besides, about 90% of admissions were in tertiary centers, but about 57% of patients were in urban locations. On one side, due to the considerable gaps in healthcare resources and medical techniques between tertiary hospitals and primary health centers and patients’ distrust of primary health centers, the majority of Chinese patients prefer to choose tertiary hospitals after the occurrence of disease (50). On the other side, with the improvement of infrastructure in rural areas, the cost of time from rural areas to urban areas is also shortening. Besides, our definition of the urban and rural was in accordance with the living status which may affect by the urbanization process (51) and the rural–urban immigrations (52). Due to the aforementioned methods, the definition of the rural and the urban may be weakened.
Regarding the prediction of mortality on weekdays and weekends, following a previous study, age (53), Charlson Comorbidity Index score (54), NIHSS score (54), and in-hospital complications (55) were the apparent predictors for both weekday and weekend admissions. Our study also indicated that intravenous thrombolysis, hospital level and regional differences may affect mortality on weekdays. Compared with no reperfusion therapy, IV-tPA has been shown to improve functional outcomes after AIS in randomized trials (5, 56). The accurate factors for the conflicting outcomes of the weekend effect among AIS patients are not entirely understood. The reported IVT rates on weekends have been rather higher than (57, 58) or equal (59) to weekdays and do not therefore provide an explanation. In addition, the concept of the weekend effect has recently been queried with a more sophisticated correlation of admission time and outcomes (60). Hospital-level outcomes varied considerably for AIS patients in America in terms of mortality and rehospitalization (61). In addition, stroke occurrence, mortality, and prevalence fluctuate extensively among various regions within China, with a conspicuous North–South gradient (62), which may compromise the variation in the regression for our study.
This study had several limitations. First, due to the retrospective nature of this study, selection bias may have occurred, as the day of stroke occurrence was uncontrollable, which may have influenced the treatment strategy. Second, the regional data were not sufficient, and most of the AIS patients were admitted to first-class hospitals. Future studies require more comprehensive data coverage and analysis. Third, the mortality and demographic data came from manual medical records, and recording errors are probable. Fourth, the possibility of unrecorded comorbid conditions and other interrelated confounders cannot be excluded. Finally, our definition of urban and rural was in accordance with living status, which may be affected by the urbanization process and rural–urban immigrations.
In summary, our study did not show any weekend effect on the mortality of AIS patients after adjusting for the patients’ background characteristics, regardless of location and regional differences.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the ethics committee of Peking University First Hospital (IRB approval number: 2015[922]) and all participating hospitals. Written informed consent was obtained from all the patients or an appropriate family member (if the patient was unable to provide it) to participate. The patients/participants provided their written informed consent to participate in this study.
HJ and YH: conceptualization. DH and YL: data curation. YS, WS, LT, GL, HC, GZ, LZ, XS, and JQ: investigation. DH: methodology and writing—original draft. YH: supervision. JH: writing—review and editing. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China (No. 82071306). The CASTOR study was funded by Techpool Bio-Pharma Co., Ltd. All funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication. All authors declare no other competing interests.
We thank all study the participants and staff in the CASTOR study.
1. GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. (2019) 18:439–58. doi: 10.1016/S1474-4422(19)30034-1
2. Maigeng, Z, Haidong, W, Jun, Z, Wanqing, C, Linhong, W, Shiwei, L, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. (2016) 387:251–72. doi: 10.1016/S0140-6736(15)00551-6
3. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
4. Wang, YJ, Li, ZX, Gu, HQ, Zhai, Y, Zhou, Q, Jiang, Y, et al. China Stroke Statistics: an update on the 2019 report from the National Center for Healthcare Quality Management in Neurological Diseases, China National Clinical Research Center for Neurological Diseases, the Chinese Stroke Association, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention and Institute for Global Neuroscience and Stroke Collaborations. Stroke Vasc Neurol. (2022) 7:415–50. doi: 10.1136/svn-2021-001374
5. Emberson, J, Lees, KR, Lyden, P, Blackwell, L, Albers, G, Bluhmki, E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. (2014) 384:1929–35. doi: 10.1016/S0140-6736(14)60584-5
6. Man, S, Xian, Y, Holmes, DN, Matsouaka, RA, Saver, JL, Smith, EE, et al. Association between thrombolytic door-to-needle time and 1-year mortality and readmission in patients with acute ischemic stroke. JAMA. (2020) 323:2170–84. doi: 10.1001/jama.2020.5697
7. Yang, G, Wang, Y, Zeng, Y, Gao, GF, Liang, X, Zhou, M, et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. (2013) 381:1987–2015. doi: 10.1016/S0140-6736(13)61097-1
8. Wang, W, Wang, D, Liu, H, Sun, H, Jiang, B, Ru, X, et al. Trend of declining stroke mortality in China: reasons and analysis. Stroke Vasc Neurol. (2017) 2:132–9. doi: 10.1136/svn-2017-000098
9. Wang, W, Jiang, B, Sun, H, Ru, X, Sun, D, Wang, L, et al. Prevalence, incidence, and mortality of stroke in china: results from a nationwide population-based survey of 480 687 adults. Circulation. (2017) 135:759–71. doi: 10.1161/CIRCULATIONAHA.116.025250
10. Tu, WJ, Zhao, Z, Yin, P, Cao, L, Zeng, J, Chen, H, et al. Estimated burden of stroke in China in 2020. JAMA Netw Open. (2023) 6:e231455. doi: 10.1001/jamanetworkopen.2023.1455
11. Ogbu, UC, Westert, GP, Slobbe, LC, Stronks, K, and Arah, OA. A multifaceted look at time of admission and its impact on case-fatality among a cohort of ischaemic stroke patients. J Neurol Neurosurg Psychiatry. (2011) 82:8–13. doi: 10.1136/jnnp.2009.202176
12. Kostis, WJ, Demissie, K, Marcella, SW, Shao, YH, Wilson, AC, and Moreyra, AE. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. (2007) 356:1099–109. doi: 10.1056/NEJMoa063355
13. Becker, DJ. Weekend hospitalization and mortality: a critical review. Expert Rev Pharmacoecon Outcomes Res. (2008) 8:23–6. doi: 10.1586/14737167.8.1.23
14. Akram, MJ, Lv, X, Deng, L, Li, Z, Yang, T, Yin, H, et al. Off-hour admission is associated with poor outcome in patients with intracerebral hemorrhage. J Clin Med. (2023) 12:66. doi: 10.3390/jcm12010066
15. Inoue, T, and Fushimi, K. Weekend versus weekday admission and in-hospital mortality from ischemic stroke in Japan. J Stroke Cerebrovasc Dis. (2015) 24:2787–92. doi: 10.1016/j.jstrokecerebrovasdis.2015.08.010
16. Handel, AE, Patel, SV, Skingsley, A, Bramley, K, Sobieski, R, and Ramagopalan, SV. Weekend admissions as an independent predictor of mortality: an analysis of Scottish hospital admissions. BMJ Open. (2012) 2:e001789. doi: 10.1136/bmjopen-2012-001789
17. Reeves, MJ, Smith, E, Fonarow, G, Hernandez, A, Pan, W, Schwamm, LH, et al. Off-hour admission and in-hospital stroke case fatality in the get with the guidelines-stroke program. Stroke. (2009) 40:569–76. doi: 10.1161/STROKEAHA.108.519355
18. Lin, X, Green, JC, Xian, H, Cai, M, Skrzypek, J, and Tao, H. Holiday and weekend effects on mortality for acute myocardial infarction in Shanxi, China: a cross-sectional study. Int J Public Health. (2020) 65:847–57. doi: 10.1007/s00038-020-01443-x
19. Zhang, G, Zhang, JH, and Qin, X. Effect of weekend admission on in-hospital mortality after subarachnoid hemorrhage in Chongqing China. Acta Neurochir Suppl. (2011) 110:229–32. doi: 10.1007/978-3-7091-0353-1_40
20. Zhou, X, Weng, J, Xu, Z, Yang, J, Lin, J, Hou, R, et al. Effect of admission and discharge times on hospital mortality in patients with sepsis. Crit Care Med. (2023) 51:e81–81e89. doi: 10.1097/CCM.0000000000005767
21. Liu, CY, Kung, PT, Chang, HY, Hsu, YH, and Tsai, WC. Influence of admission time on health care quality and utilization in patients with stroke: analysis for a possible july effect and weekend effect. Int J Environ Res Public Health. (2021):18. doi: 10.3390/ijerph182312362
22. Sun, W, Ou, Q, Zhang, Z, Qu, J, and Huang, Y. Chinese acute ischemic stroke treatment outcome registry (CASTOR): protocol for a prospective registry study on patterns of real-world treatment of acute ischemic stroke in China. BMC Complement Altern Med. (2017) 17:357. doi: 10.1186/s12906-017-1863-4
23. Li, L, Ma, J, Cheng, Y, Feng, L, Wang, S, Yun, X, et al. Urban-rural disparity in the relationship between ambient air pollution and preterm birth. Int J Health Geogr. (2020) 19:23. doi: 10.1186/s12942-020-00218-0
24. Song, Y, Zhu, N, and Luo, F. City size and permanent settlement intention: evidence from rural-urban migrants in China. Int J Environ Res Public Health. (2022):19. doi: 10.3390/ijerph19020676
25. Liu, L, Ding, J, Leng, X, Pu, Y, Huang, LA, Xu, A, et al. Guidelines for evaluation and management of cerebral collateral circulation in ischaemic stroke 2017. Stroke Vasc Neurol. (2018) 3:117–30. doi: 10.1136/svn-2017-000135
26. Jin, H, Zhu, S, Wei, JW, Wang, J, Liu, M, Wu, Y, et al. Factors associated with prehospital delays in the presentation of acute stroke in urban China. Stroke. (2012) 43:362–70. doi: 10.1161/STROKEAHA.111.623512
27. Indredavik, B, Rohweder, G, Naalsund, E, and Lydersen, S. Medical complications in a comprehensive stroke unit and an early supported discharge service. Stroke. (2008) 39:414–20. doi: 10.1161/STROKEAHA.107.489294
28. Álvarez-Sabín, J, Maisterra, O, Santamarina, E, and Kase, CS. Factors influencing haemorrhagic transformation in ischaemic stroke. Lancet Neurol. (2013) 12:689–705. doi: 10.1016/S1474-4422(13)70055-3
29. Lu, Y, Sun, W, Shen, Z, Sun, W, Liu, R, Li, F, et al. Regional differences in hospital costs of acute ischemic stroke in China: analysis of data from the Chinese acute ischemic stroke treatment outcome registry. Front Public Health. (2021) 9:783242. doi: 10.3389/fpubh.2021.783242
30. Skyrud, KD, Vikum, E, Hansen, TM, Kristoffersen, DT, and Helgeland, J. Hospital variation in 30-day mortality for patients with stroke; the? Impact of individual and municipal socio-demographic status. J Am Heart Assoc. (2019) 8:e010148. doi: 10.1161/JAHA.118.010148
31. Mekonnen, B, Wang, G, Rajbhandari-Thapa, J, Shi, L, Thapa, K, Zhang, Z, et al. Weekend effect on in-hospital mortality for ischemic and hemorrhagic stroke in US rural and urban hospitals. J Stroke Cerebrovasc Dis. (2020) 29:105106. doi: 10.1016/j.jstrokecerebrovasdis.2020.105106
32. Goyal, N, Tsivgoulis, G, Malhotra, K, Ishfaq, MF, Pandhi, A, Frohler, MT, et al. Medical management vs mechanical thrombectomy for mild strokes: an international multicenter study and systematic review and meta-analysis. JAMA Neurol. (2020) 77:16–24. doi: 10.1001/jamaneurol.2019.3112
33. Chen, M, and Canudas-Romo, V. Urban-rural lifespan disparities and cause-deleted analysis: evidence from China. BMJ Open. (2022) 12:e050707. doi: 10.1136/bmjopen-2021-050707
34. Cho, KH, Park, EC, Nam, CM, Choi, Y, Shin, J, and Lee, SG. Effect of weekend admission on in-hospital mortality in patients with ischemic stroke: an analysis of Korean nationwide claims data from 2002 to 2013. J Stroke Cerebrovasc Dis. (2016) 25:419–27. doi: 10.1016/j.jstrokecerebrovasdis.2015.10.014
35. Ding, Y, Gao, F, Ji, Y, Zhai, T, Tong, X, Jia, B, et al. Workflow intervals and outcomes of endovascular treatment for acute large-vessel occlusion during on-vs. off-hours in China: The ANGEL-ACT registry. Front Neurol. (2021) 12:771803. doi: 10.3389/fneur.2021.771803
36. Turin, TC, Kita, Y, Rumana, N, Ichikawa, M, Sugihara, H, Morita, Y, et al. Case fatality of stroke and day of the week: is the weekend effect an artifact? Takashima stroke registry, Japan (1988-2003). Cerebrovasc Dis. (2008) 26:606–11. doi: 10.1159/000165114
37. Albright, KC, Raman, R, Ernstrom, K, Hallevi, H, Martin-Schild, S, Meyer, BC, et al. Can comprehensive stroke centers erase the 'weekend effect'. Cerebrovasc Dis. (2009) 27:107–13. doi: 10.1159/000177916
38. McKinney, JS, Deng, Y, Kasner, SE, and Kostis, JB. Myocardial infarction data acquisition system (MIDAS 15) study group. Comprehensive stroke centers overcome the weekend versus weekday gap in stroke treatment and mortality. Stroke. (2011) 42:2403–9. doi: 10.1161/STROKEAHA.110.612317
39. Kim, SC, Hong, KS, Hwang, SI, Kim, JE, Kim, AR, Cho, JY, et al. Weekend admission in patients with acute ischemic stroke is not associated with poor functional outcome than weekday admission. J Clin Neurol. (2012) 8:265–70. doi: 10.3988/jcn.2012.8.4.265
40. de Boer, SP, Oemrawsingh, RM, Lenzen, MJ, van Mieghem, NM, Schultz, C, Akkerhuis, KM, et al. Primary PCI during off-hours is not related to increased mortality. Eur Heart J Acute Cardiovasc Care. (2012) 1:33–9. doi: 10.1177/2048872612441581
41. Cubeddu, RJ, Palacios, IF, Blankenship, JC, Horvath, SA, Xu, K, Kovacic, JC, et al. Outcome of patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention during on-versus off-hours (a Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction [HORIZONS-AMI] trial substudy). Am J Cardiol. (2013) 111:946–54. doi: 10.1016/j.amjcard.2012.11.062
42. Albright, KC, Savitz, SI, Raman, R, Martin-Schild, S, Broderick, J, Ernstrom, K, et al. Comprehensive stroke centers and the 'weekend effect': the SPOTRIAS experience. Cerebrovasc Dis. (2012) 34:424–9. doi: 10.1159/000345077
43. Nakajima, M, Inatomi, Y, Yonehara, T, Watanabe, M, and Ando, Y. Outcome in patients admitted outside regular hospital working hours: does time until regular working hours matter. Int J Stroke. (2015) 10:79–84. doi: 10.1111/ijs.12351
44. Sato, S, Arima, H, Heeley, E, Hirakawa, Y, Delcourt, C, Lindley, RI, et al. Off-hour admission and outcomes in patients with acute intracerebral hemorrhage in the INTERACT2 Trial. Cerebrovasc Dis. (2015) 40:114–20. doi: 10.1159/000434690
45. Zha, M, Yang, Q, Liu, S, Huang, K, Zhang, X, Wu, M, et al. Off-hour effect is not significant in endovascular treatment for anterior circulation large vessel occlusion in a multicentre registry. Stroke Vasc Neurol. (2021) 6:640–8. doi: 10.1136/svn-2021-000949
46. Yang, P, Zhang, Y, Zhang, L, Zhang, Y, Treurniet, KM, Chen, W, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med. (2020) 382:1981–93. doi: 10.1056/NEJMoa2001123
47. Sobolewski, P, Szczuchniak, W, Sobota, A, and Grzesik, M. Are there differences between rural and urban populations in long-term outcome after systemic cerebral thrombolysis in a hospital located in an agricultural region. Rural Remote Health. (2014) 14:2867.
48. Cossey, TC, Jagolino, A, Ankrom, C, Bambhroliya, AB, Cai, C, Vahidy, FS, et al. No weekend or after-hours effect in acute ischemic stroke patients treated by telemedicine. J Stroke Cerebrovasc Dis. (2019) 28:198–204. doi: 10.1016/j.jstrokecerebrovasdis.2018.09.035
49. Xu, W, Pan, Z, Lu, S, and Zhang, L. Regional heterogeneity of application and effect of telemedicine in the primary care centres in rural China. Int J Environ Res Public Health. (2020):17. doi: 10.3390/ijerph17124531
50. Dong, E, Liu, S, Chen, M, Wang, H, Chen, LW, Xu, T, et al. Differences in regional distribution and inequality in health-resource allocation at hospital and primary health centre levels: a longitudinal study in Shanghai. China BMJ Open. (2020) 10:e035635. doi: 10.1136/bmjopen-2019-035635
51. Chen, J. Chronic conditions and receipt of treatment among urbanized rural residents in China. Biomed Res Int. (2013) 2013:568959. doi: 10.1155/2013/568959
52. Mou, J, Griffiths, SM, Fong, H, and Dawes, MG. Health of China's rural-urban migrants and their families: a review of literature from 2000 to 2012. Br Med Bull. (2013) 106:19–43. doi: 10.1093/bmb/ldt016
53. Demir, A, and Eren, F. The relationship between age shock index, and severity of stroke and in-hospital mortality in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis. (2022) 31:106569. doi: 10.1016/j.jstrokecerebrovasdis.2022.106569
54. Phan, TG, Clissold, B, Ly, J, Ma, H, Moran, C, Srikanth, V, et al. Stroke severity and comorbidity index for prediction of mortality after ischemic stroke from the virtual international stroke trials archive-acute collaboration. J Stroke Cerebrovasc Dis. (2016) 25:835–42. doi: 10.1016/j.jstrokecerebrovasdis.2015.12.016
55. Bae, HJ, Yoon, DS, Lee, J, Kim, BK, Koo, JS, Kwon, O, et al. In-hospital medical complications and long-term mortality after ischemic stroke. Stroke. (2005) 36:2441–5. doi: 10.1161/01.STR.0000185721.73445.fd
56. IST-3 collaborative group. Effect of thrombolysis with alteplase within 6 h of acute ischaemic stroke on long-term outcomes (the third International Stroke Trial [IST-3]): 18-month follow-up of a randomised controlled trial. Lancet Neurol. (2013) 12:768–76. doi: 10.1016/S1474-4422(13)70130-3
57. Hoh, BL, Chi, YY, Waters, MF, Mocco, J, and Barker, FG 2nd. Effect of weekend compared with weekday stroke admission on thrombolytic use, in-hospital mortality, discharge disposition, hospital charges, and length of stay in the Nationwide Inpatient Sample Database, 2002 to 2007. Stroke. (2010) 41:2323–8. doi: 10.1161/STROKEAHA.110.591081
58. Kazley, AS, Hillman, DG, Johnston, KC, and Simpson, KN. Hospital care for patients experiencing weekend vs weekday stroke: a comparison of quality and aggressiveness of care. Arch Neurol. (2010) 67:39–44. doi: 10.1001/archneurol.2009.286
59. Jauss, M, Schütz, HJ, Tanislav, C, Misselwitz, B, and Rosenow, F. Effect of daytime, weekday and year of admission on outcome in acute ischaemic stroke patients treated with thrombolytic therapy. Eur J Neurol. (2010) 17:555–61. doi: 10.1111/j.1468-1331.2009.02845.x
60. Bray, BD, Cloud, GC, James, MA, Hemingway, H, Paley, L, Stewart, K, et al. Weekly variation in health-care quality by day and time of admission: a nationwide, registry-based, prospective cohort study of acute stroke care. Lancet. (2016) 388:170–7. doi: 10.1016/S0140-6736(16)30443-3
61. Fonarow, GC, Smith, EE, Reeves, MJ, Pan, W, Olson, D, Hernandez, AF, et al. Hospital-level variation in mortality and rehospitalization for medicare beneficiaries with acute ischemic stroke. Stroke. (2011) 42:159–66. doi: 10.1161/STROKEAHA.110.601831
Keywords: acute ischemic stroke, China, mortality, rural, regional difference, weekend
Citation: Huang D, Lu Y, Sun Y, Sun W, Huang Y, Tai L, Li G, Chen H, Zhang G, Zhang L, Sun X, Qiu J, Wei Y and Jin H (2023) Effect of weekend versus weekday admission on the mortality of acute ischemic stroke patients in China: an analysis of data from the Chinese acute ischemic stroke treatment outcome registry. Front. Neurol. 14:1206846. doi: 10.3389/fneur.2023.1206846
Received: 16 April 2023; Accepted: 29 June 2023;
Published: 17 July 2023.
Edited by:
Wen-Jun Tu, Chinese Academy of Medical Sciences and Peking Union Medical College, ChinaReviewed by:
Alicia Zha, The Ohio State University, United StatesCopyright © 2023 Huang, Lu, Sun, Sun, Huang, Tai, Li, Chen, Zhang, Zhang, Sun, Qiu, Wei, Jin and on behalf of the CASTOR Investigators. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haiqiang Jin, amhxOTExQGJqbXUuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.