
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 28 June 2023
Sec. Stroke
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1199745
 Fadi Nahab1*
Fadi Nahab1* Rana Bayakly2
Rana Bayakly2 Mary Elizabeth Sexton3
Mary Elizabeth Sexton3 Manet Lemuel-Clarke4
Manet Lemuel-Clarke4 Laura Henriquez4
Laura Henriquez4 Srikant Rangaraju4
Srikant Rangaraju4 Moges Ido2
Moges Ido2Background: The objective of our study was to evaluate vaccine type, COVID-19 infection, and their association with stroke soon after COVID-19 vaccination.
Methods: In a retrospective cohort study, we estimated the 21-day post-vaccination incidence of stroke among the recipients of the first dose of a COVID-19 vaccine. We linked the Georgia Immunization Registry with the Georgia Coverdell Acute Stroke Registry and the Georgia State Electronic Notifiable Disease Surveillance System data to assess the relative risk of stroke by the vaccine type.
Results: Approximately 5 million adult Georgians received at least one COVID-19 vaccine between 1 December 2020 and 28 February 2022: 54% received BNT162b2, 41% received mRNA-1273, and 5% received Ad26.COV2.S. Those with concurrent COVID-19 infection within 21 days post-vaccination had an increased risk of ischemic (OR = 8.00, 95% CI: 4.18, 15.31) and hemorrhagic stroke (OR = 5.23, 95% CI: 1.11, 24.64) with no evidence for interaction between the vaccine type and concurrent COVID-19 infection. The 21-day post-vaccination incidence of ischemic stroke was 8.14, 11.14, and 10.48 per 100,000 for BNT162b2, mRNA-1273, and Ad26.COV2.S recipients, respectively. After adjusting for age, race, gender, and COVID-19 infection status, there was a 57% higher risk (OR = 1.57, 95% CI: 1.02, 2.42) for ischemic stroke within 21 days of vaccination associated with the Ad26.COV2.S vaccine compared to BNT162b2; there was no difference in stroke risk between mRNA-1273 and BNT162b2.
Conclusion: Concurrent COVID-19 infection had the strongest association with early ischemic and hemorrhagic stroke after the first dose of COVID-19 vaccination. Although not all determinants of stroke, particularly comorbidities, were considered in this analysis, the Ad26.COV2.S vaccine was associated with a higher risk of early post-vaccination ischemic stroke than BNT162b2.
To tackle the emergence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus, multiple coronavirus disease 2019 (COVID-19) vaccines have been approved (1, 2). BNT162b2 and mRNA-1273 are mRNA-based vaccines that encode the prefusion-stabilized full-length spike protein of SARS-CoV-2, whereas Ad26.COV2.S is a recombinant, replication incompetent human adenovirus type 26 vector encoding full-length SARS-CoV-2 spike protein in a prefusion-stabilized conformation (3–5). These vaccines have been shown to be both safe and effective although rare thrombotic events associated with the Ad26.COV2.S vaccine have led to warnings about use in certain high-risk populations and a preference for other available vaccines.
The first case of cerebral venous sinus thrombosis (CVST) associated with thrombocytopenia and disseminated intravascular coagulation after Ad26.COV2.S vaccination was documented in 2021 (6–8). Thrombosis with thrombocytopenia syndrome (TTS) has been reported in 3.83 cases per million doses administered and 0.6 per million deaths, and the Advisory Committee on Immunization Practices (ACIP) subsequently performed a comprehensive review of existing data and made a preferential recommendation for mRNA COVID-19 vaccines over the Ad26.COV2.S vaccine (9).
A systematic review of reported acute ischemic stroke (AIS) soon after COVID-19 vaccination identified 31 patients with vaccine-induced immune thrombotic thrombocytopenia (VITT), 95% of whom received viral vector vaccines (10). Other studies that focused solely on mRNA vaccination have not identified an increased incidence of ischemic stroke in the post-vaccine period (11, 12). However, large-scale population studies assessing factors associated with stroke risk early after COVID-19 vaccinations are limited outside of case reports and a self-controlled case series method in the French population (13). In this study, we report a statewide analysis to assess baseline factors, COVID-19 infection, and vaccination type associated with the early incidence of stroke after the first dose of COVID-19 vaccination.
A retrospective cohort study was performed to assess the incidence of acute stroke among COVID-19 vaccine recipients. All adult residents of Georgia who received any type of COVID-19 vaccine between 1 December 2020 and 28 February 2022 were included in the study. The Georgia Registry of Immunization Transactions and Services (GRITS) database served as the source of information on vaccination status, and it includes demographic and personally identifiable information such as date of birth, sex, race, and first and last names. The GRITS data were linked with the Georgia Coverdell Acute Stroke Registry (GCASR) and the Georgia State Electronic Notifiable Disease Reporting System (SENDSS) data of the corresponding time period. The GCASR collects clinical information on patients diagnosed with acute stroke in non-federal hospitals located in Georgia. The GCASR was established in 2005 for monitoring and improving the quality of stroke care across the state and receives data from 83 hospitals that provide service for more than 96% of stroke patients in Georgia (14). The Georgia SENDSS receives information on all cases with a notifiable disease including COVID-19 infection. The COVID-19 cases in the SENDSS database are subsequently grouped as confirmed for subjects with a confirmatory viral test (positive PCR test result) from a throat or nose swab or saliva for SARS-CoV-2. All three data sources are housed at the Georgia Department of Public Health. Because the data were collected for public health surveillance purposes, this study has qualified for the Department's Institutional Review Board exemption.
The three data sources were linked using a quasi-unique identifier—a 15-digit alphanumerical code called the Georgia Longitudinal ID (LONGID), which consists of letters from the first and last names, the birthdate, and a letter representing sex. The LONGID is collected by hospitals for the GCASR, and it was generated from available variables for the GRITS and SENDSS data; the three datasets were then linked with a deterministic linkage. Records without a valid LONGID value (0.03% of the GRITS records, 0.14% of SENDSS records, and 1.30% of GCASR records) were excluded from the linkage.
Acute ischemic and hemorrhagic stroke within 21 days post-initial vaccination were the outcomes of interest. The 21-day cutoff was chosen to ensure that patients were not yet eligible for a second dose of any of the available vaccines. The type of first vaccine dose was the main predictor, and demographic variables such as age (grouped into 18– < 45 years, 45– < 65 years, 65– < 80 years, and 80+ years), race (grouped as non-Hispanic white, non-Hispanic black, Hispanic, and others), sex, and COVID-19 infection status were considered covariates. A subject with a confirmed COVID-19 infection during the 21 days post-vaccination was considered to have a concurrent infection. Those who had confirmed infection prior to receiving the vaccine were grouped as having a past medical history of COVID-19 infection.
Approximately 0.11% of the GRITS record had unspecified vaccine types and were excluded. Information on race was missing on 7.3% of the records as well. Missing values for the linking and predictor variables were assessed for randomness looking at the distribution of the records by other variables. Data were analyzed assuming the missingness was completely random.
Logistic regression was applied to assess whether the relative risk, measured by odds ratio, of early stroke varies by vaccine type accounting for demographic variables and COVID-19 infection status. To determine if such risk would vary by the status of COVID-19 infection, we tested the statistical significance of an interaction term. All analyses were performed using SAS® Enterprise Guide 7.1 (Copyright © 2017, SAS Institute Inc., Cary, NC, USA).
Approximately 5 million adult Georgians received at least one COVID-19 vaccine between 1 December 2020 and 28 February 2022. The median age was 51 years (IQR: 35–64), and the majority were white (51%) and female (55%; see Table 1). Approximately 9% had COVID-19 infection prior to receiving the vaccine, and 0.4% had acquired the infection during the 21 days post-vaccination. A total of 54% had received the BNT162b2 vaccine, 41% had received mRNA-1273, and 5% had received Ad26.COV2.S.

Table 1. Description of adult COVID-19 vaccine recipients and 21-day post-vaccination incidence of ischemic stroke among adult Georgians, December 2020–February 2022.
Overall, 473 (9.498 per 100 thousand) had ischemic stroke, and 87 (1.747 per 100 thousand) subjects had developed hemorrhagic stroke within 21 days post-vaccination. The 21-day post-vaccination incidence of ischemic stroke was 8.14, 11.14, and 10.48 per 100,000 for BNT162b2, mRNA-1273, and Ad26.COV2.S recipients, respectively; after adjusting for age, race, gender, and COVID-19 infection status, there was a 57% higher risk (OR = 1.57, 95% CI: 1.02, 2.42) for ischemic stroke within 21 days of vaccination associated with Ad26.COV2.S vaccine compared to BNT162b2 (Table 2). There was no difference seen in the risk of stroke between mRNA-1273 compared to BNT162b2. After adjusting for age, race, gender, and COVID-19 infection status, those with concurrent COVID-19 infection had an increased risk of ischemic (OR = 8.00, 95% CI: 4.18, 15.31) and hemorrhagic stroke (OR = 5.23, 95% CI: 1.11, 24.64). There was no statistical evidence for an interaction between vaccine type and concurrent COVID-19 infection.
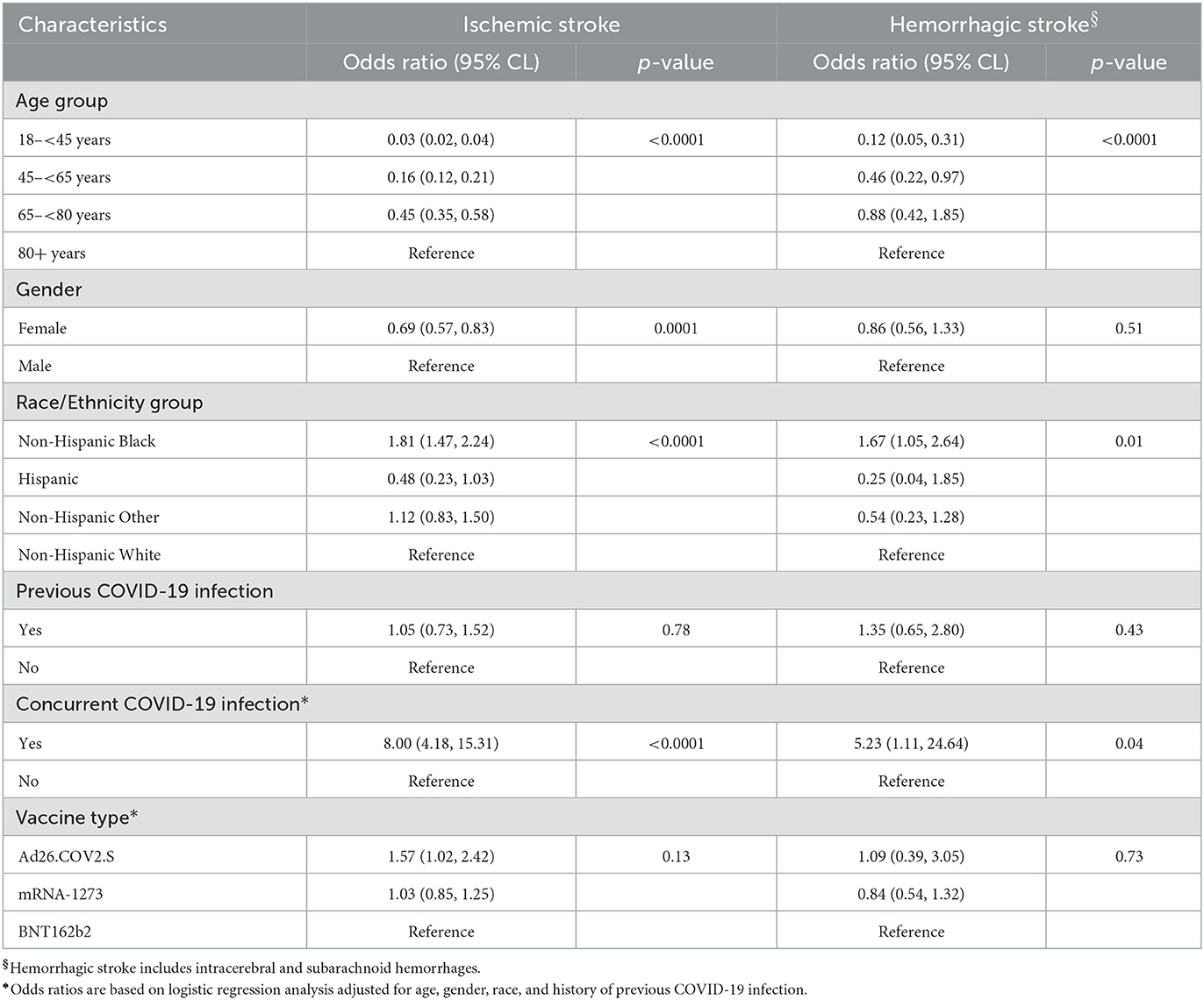
Table 2. Estimated odds ratio of ischemic and hemorrhagic stroke within 21 days of receiving the first dose of COVID-19 among adult Georgians, December 2020–February 2022.
This statewide analysis showed that concurrent COVID-19 infection within the 21 days after vaccination was the strongest association with an increased risk of ischemic and hemorrhagic stroke regardless of vaccine type. Early increased risk of ischemic stroke within 21 days of vaccination with Ad26.COV2.S compared with BNT162b2 was also found after adjusting for age, race, gender, and COVID-19 infection status.
The early increased risk of both ischemic and hemorrhagic stroke in those vaccinated and with concurrent COVID-19 was independent of vaccine type. COVID-19 has been associated with an increased risk of acute ischemic stroke and intracerebral hemorrhage, and compared to stroke patients without infection, COVID-19 stroke patients tend to be younger and to have more severe strokes, a higher frequency of large artery occlusion, and higher in-hospital mortality (15). This suggests that COVID-19 infection leads to a much higher risk of stroke outweighing the risk of stroke associated with the vaccine alone.
COVID-19 vaccines using an adenoviral vector have been reported to have the rare occurrence of thrombotic thrombocytopenia including thrombosis of the cerebral veins (6, 16, 17). These cases have had positive heparin-PF4 HIT antibody ELISA tests in the absence of prior exposure to heparin. The FDA has reported that a causal relationship between Ad26.COV2.S vaccine and TTS is plausible, updating the EUA with a warning about rare clotting events after Ad26.COV2.S vaccination (18). In a self-controlled case series method study of early cardiovascular events after vaccination in France, the incidence of myocardial infarction was increased during the second week after vaccination with a single dose of Ad26.COV2.S; however, no association was seen with stroke (13). In France, the Ad26.COV2.S vaccine was limited to people aged 55 years or older whereas no age limit was present in Georgia which may have accounted for differences in increased rates of ischemic stroke seen compared to BNT162b2 (19).
A key strength of this study is the large registries that were able to link statewide vaccination date and type with statewide stroke diagnoses and COVID-19 test positivity. A limitation of this study is the lack of data on comorbidities that may have contributed to differences in stroke risk across vaccine recipients. Additionally, the increased use of home COVID-19 tests likely contributed to an underreporting of COVID-19 infection in the SENDSS database which may have influenced the study results. Finally, data were unavailable to determine if any of these early post-vaccination strokes were related to thrombotic thrombocytopenia.
Although not all determinants of stroke, particularly comorbidities, were considered in this analysis, concurrent COVID-19 infection had the strongest association with early incidence of ischemic and hemorrhagic strokes in recipients of the first dose of the COVID-19 vaccine compared with those without infection. The Ad26.COV2.S vaccine appears to be associated with a higher risk of early post-vaccination ischemic stroke than the BNT162b2 vaccine further supporting the ACIP preferential recommendation for mRNA COVID-19 vaccines over the Ad26.COV2.S vaccine.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
The studies involving human participants were reviewed and approved by Georgia Department of Public Health. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
FN contributed to concept, drafted article, and interpretation of data. RB contributed to concept and revision of the article. MS, ML-C, LH, and SR contributed to interpretation of data and revision of the article. MI contributed to study concept, analysis, and interpretation of data and manuscript revision. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Johns Hopkins University Coronavirus Resource Center. COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. (2022). Available online at: https://coronavirus.jhu.edu/map.html (accessed March 1, 2023).
2. Krammer F. SARS-CoV-2 vaccines in development. Nature. (2020) 586:516–27. doi: 10.1038/s41586-020-2798-3
3. Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. (2020) 383:2603–15. doi: 10.1056/NEJMoa2034577
4. Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. (2021) 384:403–16. doi: 10.1056/NEJMoa2035389
5. Sadoff J, Gray G, Vandebosch A, Cárdenas V, Shukarev G, Grinsztejn B, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med. (2021) 384:2187–201. doi: 10.1056/NEJMoa2101544
6. Muir K-L, Kallam A, Koepsell SA. Gundabolu K. Thrombotic thrombocytopenia after Ad26COV2S vaccination. N Engl J Med. (2021) 384:1964–5. doi: 10.1056/NEJMc2105869
7. Sadoff J, Gray G, Vandebosch A, Cardenas V, Shukarev G, Grinsztejn B, et al. Final analysis of efficacy and safety of single-dose Ad26COV2S. N Engl J Med. (2022) 386:847–60. doi: 10.1056/NEJMoa2117608
8. See I, Su JR, Lale A, Woo EJ, Guh A, Shimabukuro TT, et al. US case reports of cerebral venous sinus thrombosis with thrombocytopenia after Ad26.COV2.S vaccination, March 2 to April 21, 2021. JAMA. (2021) 325:1–10. doi: 10.1001/jama.2021.7517
9. Oliver SE, Wallace M, See I, Mbaeyi S, Godfrey M, Hadler SC, et al. Use of the Janssen (Johnson & Johnson) COVID-19 vaccine: updated interim recommendations from the advisory committee on immunization practices—United States, December. MMWR. (2021) 71:90–5. doi: 10.15585/mmwr.mm7103a4
10. Kolahchi Z, MohamadHossein K, Mowla A. Acute ischemic stroke and vaccine-induced immune thrombotic thrombocytopenia post COVID-19 vaccination; a systematic review. J Neurol Sci. (2022) 439:120327. doi: 10.1016/j.jns.2022.120327
11. Klein NP, Lewis N, Goddard K, Fireman B, Zerbo O, Hanson KE, et al. Surveillance for adverse events after COVID-19 mRNA vaccination. JAMA. (2021) 326:1390–9. doi: 10.1001/jama.2021.15072
12. Jabagi MJ, Botton J, Bertrand M, Weill A, Farrington P, Zureik M, et al. Myocardial infarction, stroke, and pulmonary embolism after BNT162b2 mRNA COVID-19 vaccine in people aged 75 years or older. JAMA. (2022) 327:80–2. doi: 10.1001/jama.2021.21699
13. Botton J, Jabagi MJ, Bertrand M, Baricault B, Drouin J, Vu SL, et al. Risk for myocardial infarction, stroke, and pulmonary embolism following COVID-19 vaccines in adults younger than 75 years in France. Ann Intern Med. (2022) 175:1250–7. doi: 10.7326/M22-0988
14. George MG, Tong X, McGruder H, Yoon P, Rosamond W, Winquist A, et al. Paul coverdell national acute stroke registry-four states, 2005-2007. MMWR Surveill Summ. (2009) 58:1–23.
15. Nannoni S, de Groot R, Bell S, Markus HS. Stroke in COVID-19: a systematic review and meta-analysis. Int J Stroke. (2021) 16:137–49. doi: 10.1177/1747493020972922
16. Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N Engl J Med. (2021) 384:2092–101. doi: 10.1056/NEJMoa2104840
17. Schultz NH, Sørvoll IH, Michelsen AE, Munthe LA, Lund-Johansen F, Ahlen MT, et al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV-19 vaccination. N Engl J Med. (2021) 384:2124–30. doi: 10.1056/NEJMoa2104882
18. Food Drug Administration. Fact Sheet for Healthcare Providers Administering Vaccine (vaccination providers). The Emergency Use Authorization (EUA) of the Janssen COVID-19 vaccine to prevent coronavirus disease 2019 (COVID-19). Available online at: https://www.fda.gov/media/146304/download (accessed October 30, 2022).
Keywords: COVID-19, vaccine, stroke, ischemic stroke, hemorrhagic stroke
Citation: Nahab F, Bayakly R, Sexton ME, Lemuel-Clarke M, Henriquez L, Rangaraju S and Ido M (2023) Factors associated with stroke after COVID-19 vaccination: a statewide analysis. Front. Neurol. 14:1199745. doi: 10.3389/fneur.2023.1199745
Received: 03 April 2023; Accepted: 08 June 2023;
Published: 28 June 2023.
Edited by:
Gary Kui Kai Lau, The University of Hong Kong, Hong Kong SAR, ChinaReviewed by:
Ahmed Y. Azzam, October 6 University, EgyptCopyright © 2023 Nahab, Bayakly, Sexton, Lemuel-Clarke, Henriquez, Rangaraju and Ido. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fadi Nahab, Zm5haGFiQGVtb3J5LmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.