- 1Department of Neurology, The First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, China
- 2Department of Neurology, HanCheng People's Hospital, Han Cheng, China
- 3The Diagnostic Center, Shannxi People's Hospital, Xi'an, China
Background: Severe cerebral artery embolism is a rare complication of facial autologous fat injection. However, its incidence has markedly increased with the recent rise in facial cosmetic procedures.
Case presentation: We report a 31-year-old Chinese woman who presented with unconsciousness 6 h after having undergone a facial autologous fat injection. A neurological examination revealed stupor, bilaterally diminished pupillary light reflexes, right-sided central facial palsy, and no reaction to pain stimulation of right limbs. Diffusion-weighted imaging displayed patchy hyperintense lesions in the left frontal, parietal, and temporal lobes. Magnetic resonance angiography demonstrated fat embolism in the left internal carotid artery, anterior cerebral artery, and middle cerebral artery. We immediately performed mechanical thrombectomy under sufficient preoperative preparations but failed to achieve complete recanalization. Pathological examination of the embolus confirmed the presence of adipocytes. Although we actively administered symptomatic and supportive treatments, the patient eventually died due to the progression of cerebral herniation and systemic infection.
Conclusion: Due to the ineffectiveness of current treatment and the inferior prognosis, fat embolism, a severe complication of autologous fat graft, should draw the attention of both plastic surgeons and neurologists so that actions may be taken for both its prevention and treatment.
1. Introduction
With continuous improvements in cosmetic procedures and people's desire to pursue beauty, facial autologous fat injection has become a popular procedure due to its widespread availability, relative safety, permanent results, and low rejection rate. The procedure is widely considered to be a low-risk measure to correct soft-tissue defects with minimal discomfort to the patient (1). However, a growing number of cases of rare but severe vascular complications of facial autologous fat injection, including cerebral artery embolism, are being reported worldwide (2). As these complications have limited treatment options and carry a poor prognosis, they should draw the attention of both doctors and patients. Here, we report an uncommon case of fatal cerebral embolism after a facial autologous fat graft and put forward our recommendations to potentially prevent this devastating complication. This study was reported in agreement with the principles of the CARE guidelines (3).
2. Case presentation
A 31-year-old left-handed Chinese woman was admitted to our hospital due to disordered consciousness. She had undergone abdominal liposuction followed by the bilateral injection of 10.6 mL of autologous fat into the temples and tear troughs under general anesthesia 6 h ago. After the 2-h procedure, the patient was unconscious, and her right limbs were unresponsive to pain stimulation, which was attributed to a lack of recovery from general anesthesia by the cosmetic doctor. However, 1 h after the surgery, the patient had still not woken up, and her heart rate had declined to 60 bpm, which increased to 70 bpm after an intravenous bolus of 0.5 mg atropine. Before the procedure, she had been in good health and had undergone a similar procedure at the same beauty salon 5 months ago and recovered well.
On admission to our hospital, the patient's vital signs were stable. A neurological examination revealed stupor, round and bilaterally equal pupils (3 mm), bilaterally diminished pupillary light reflexes, right-sided central facial palsy, no response to pain stimulation of the right limbs, and a positive Babinski sign on the right. Considering the type of operation and the patient's symptoms and signs, we suspected a cerebral fat embolism, most likely involving a vessel in the left internal carotid artery system. Although the patient had undergone abdominal liposuction, she had no rapid respiratory rate, hypoxemia, or chest CT signs such as the “blizzard sign,” ruling out pulmonary fat embolism. Cranial non-contrast computed tomography (CT) revealed multiple low-density shadows along the blood vessels (Figure 1A). Diffusion-weighted imaging (DWI) confirmed fresh infarctions in the left frontal, parietal, and temporal lobes (Figure 1B). The lesions appeared much smaller on fluid-attenuated inversion recovery (FLAIR) and T2-weighted sequences (Figures 1C, D). Magnetic resonance angiography demonstrated the occlusion of the left internal carotid artery (ICA), left anterior cerebral artery, and left middle cerebral artery (Figure 1E). No obvious hemorrhage was observed on susceptibility-weighted imaging, and the hypointense lesions along the cerebral vessels indicated slowed blood flow caused by fat emboli (Figure 1F).

Figure 1. (A) Non-contrast computed tomography shows multiple low-density shadows along the blood vessels. (B) Diffusion-weighted imaging shows high-signal intensities in the left cerebral hemisphere. (C) Fluid attenuated inversion recovery. (D) T2-weighted sequences show much smaller lesions. (E) Magnetic resonance angiography shows occlusion of the left internal carotid artery, anterior cerebral artery, and middle cerebral artery. (F) Susceptibility-weighted imaging shows hypointensity along the cerebral vessels, indicating slowed blood flow caused by the fat emboli.
Owing to the mismatch between the FLAIR and DWI findings, we performed digital subtraction angiography, which confirmed the occlusion of the left ICA and external carotid artery (Figure 2A). After obtaining consent from the patient's family, we immediately performed mechanical thrombectomy (MT) using the ADAPT (a direct aspiration first pass technology) and SWIM (Solitaire FR/stent with intracranial support catheter for mechanical thrombectomy) techniques but failed to achieve complete recanalization (Figure 2B). Pathological examination of the emboli confirmed the presence of adipocytes (Figure 2C). After the operation, the patient's unconsciousness deepened, and she fell into a deep coma. Her right pupil (4.5 mm) became larger than the left one (3 mm). Immediate cranial non-contrast CT showed a large cerebral infarction in the left cerebral hemisphere and a slight rightward shift of the midline (Figure 2D). Decompressive craniectomy was promptly performed (Figure 3). Mannitol, glycerol fructose, torasemide, and albumin were administered to decrease intracranial pressure. We also actively provided symptomatic and supportive treatments, including nutritional support, antibiotic therapy, mechanical ventilation, neurotrophic factors, and cerebral protection.
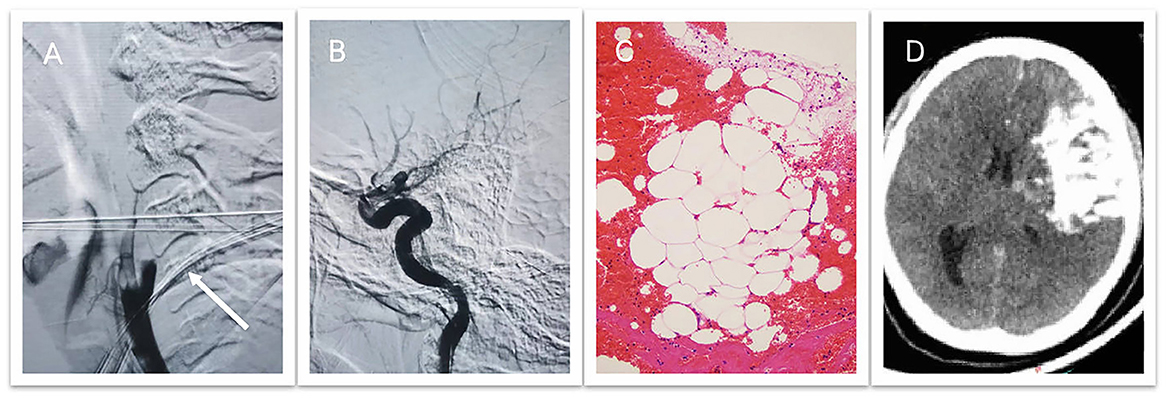
Figure 2. (A) Digital subtraction angiography confirms occlusion of the left internal and external carotid arteries. (B) Mechanical thrombectomy fails to achieve complete recanalization. (C) Pathological examination of the emboli confirms the presence of adipocytes. (D) Postoperative computed tomography demonstrates a large cerebral infarction with extravasation of the contrast agent in the left cerebral hemisphere and a slight rightward shift of the midline.
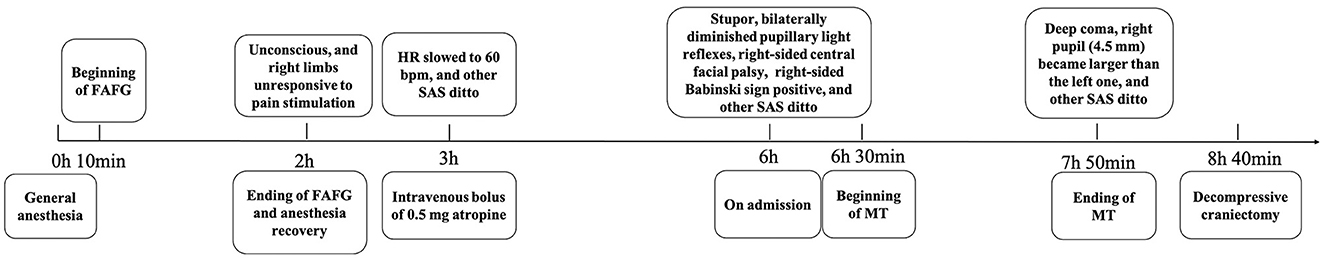
Figure 3. Timeline of symptoms, physical signs, and treatment. FAFG, facial autologous fat graft; HR, heart rate; SAS, symptoms and signs; MT, mechanical thrombectomy.
Unfortunately, due to the large cerebral infarction and edema, the brain herniation progressed, compressing the hypothalamus and brainstem. The patient lost spontaneous respiration and was in a state of metabolic disorder. She also developed a severe infection of multiple systems. Eventually, on the 16th day of hospitalization, she was diagnosed with brain death.
3. Discussion
3.1. Epidemiology
Cerebral embolism as a complication of facial autologous fat graft has been increasingly reported in recent years. We performed a literature review by searching the PubMed, CNKI, and SinoMed databases for relevant articles describing any case of cerebral fat embolism following facial autologous fat graft. For PubMed, we used the following search strategy: “((fat graft*[Title/Abstract]) OR (fat injection[Title/Abstract]) AND (English[Filter])) AND ((stroke[Title/Abstract]) OR (cerebral fat embolism[Title/Abstract]) OR (infarction[Title/Abstract]) OR (cerebral embolism[Title/Abstract]) AND (English[Filter])).” No time limit was applied during the search. We found a total of 62 articles using the above search strategy (32 articles from PubMed, 13 from CNKI, and 17 from SinoMed). After excluding 9 reviews, 11 case reports were unrelated to cerebral embolism following facial autologous fat graft and 12 were repeated articles, and a total of 39 cases from 30 articles were included in the review (Table 1). All retrieved articles were independently reviewed by two authors (GY and YC), and eligible articles were selected by mutual agreement. According to Wang et al., the incidence of this complication has markedly increased since 2010, and most of the cases have occurred in young and middle-aged women from East Asia (2), which may be due to the aesthetic preference for facial three-dimensional contouring in this population.
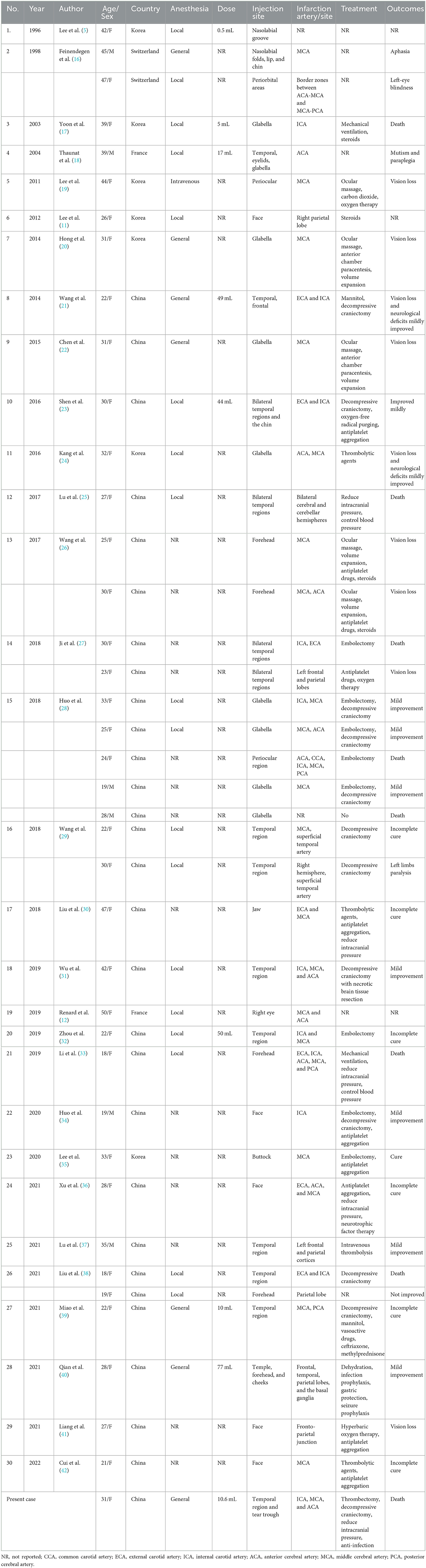
Table 1. Cases of cerebral fat embolism following facial fat injection retrieved from three databases.
3.2. Pathogenesis
Facial autologous fat graft is most commonly performed using multi-tunnel, multi-layered, and multi-point dispersed injections to uniformly fill the space between the periosteum and the muscular layer. However, this surgical approach increases the risk of puncturing blood vessels. One possible mechanism for cerebral fat embolism is that the injection device accidentally punctures the small facial veins or arteries, inducing a reflux of fat particles into the proximal large vessels under excessive pressure, which then flow down into the distal vessels (4). A small amount of fat is sufficient to cause reflux. The smallest fat volume that has been reported to cause a cerebral embolism is 0.5 mL (5).
When fat emboli enter the cerebral circulation through the venous system, the symptoms of neurological deficits may appear late and may be accompanied by some signs of pulmonary embolism such as dyspnea and tachycardia.
When fat embolism occurs via the arterial route, the fat particles inadvertently enter the superficial arteries, such as the extracranial branches of the ophthalmic artery, the facial artery, or the superficial temporal artery, and eventually reach the cerebral circulation due to hemodynamics.
Considering the graft site in our patient, we speculate that the emboli flowed back into the external carotid artery through the superficial temporal artery and then entered the ICA. It is also possible that the tear-trough modification damaged the infraorbital artery, through which the emboli could directly flow into the ophthalmic artery and then into the ICA in a retrograde fashion (6).
Some studies (7, 8) have suggested that the macroscopic pathological changes caused by fat embolism consist of occlusion and immediate ischemia in the case of arterial emboli. The microscopic pathological changes are attributable to the inflammatory cascade induced by the fat particles, which causes damage to the perivascular tissue and delayed symptoms.
3.3. Symptoms and diagnosis
There is no clear time boundary between early and delayed symptoms (9, 10). The severity of symptoms depends on the location and extent of the embolism. Wang et al. concluded that the infarction mainly occurred in the middle cerebral artery territory, and the most common symptoms were consciousness disorder, hemiplegia, aphasia, and vision loss (4). It is difficult to distinguish fat embolism from other types of cerebral infarction on non-contrast CT. DWI often displays sporadic hyperintense lesions resembling “a starry sky.” Lee et al. regarded magnetic resonance spectroscopy to be more helpful than DWI for identifying fat emboli (11). In our patient, the CT value of the shadows ranged from −33 HU to −120 HU, suggesting fat embolism. The diagnosis was finally confirmed by pathology.
3.4. Treatment and prognosis
Treatment options for cerebral fat embolism with large-vessel occlusion are limited and ineffective. Early reperfusion is crucial. Intra-arterial MT or thrombolysis is usually selected; the effect of intravenous thrombolysis is poor. Among the previously reported cases, only one patient experienced a significant improvement in neurological function after undergoing MT at 6 h and 45 min after the onset of symptoms (12). The key to a successful outcome is timely recognition and treatment. Steroids were used as well, probably to inhibit the inflammatory cascade, with unsatisfactory effects. Symptomatic treatments, including intracranial pressure reduction, anti-infection therapy, nutritional support, and brain protection, are indispensable. Even with these treatments, the prognosis is extremely poor. Among the 30 patients reported by Wang et al., four patients died, and those who survived had a poor quality of life due to irreversible hemiplegia and vision loss (2).
In our patient, the failure of MT may be attributed to the following three reasons. First, the symptoms were not recognized in time by the cosmetic doctor. The second reason is the inherent limitation of thrombectomy materials. Fat particles are liquid emboli, and currently, available stents are all open or coiled closed-loop structures, which can effectively embed a solid thrombus in their multiple layers but cannot efficiently contain liquid emboli. The third reason is that the multiple fat emboli in the distal intracranial vessels may have caused microcirculation disturbances, which may benefit little from thrombectomy. Although we performed decompressive craniectomy and administered dehydration treatment immediately after the signs of brain herniation were found and actively applied symptomatic treatments, the patient eventually died due to the progression of brain herniation and systemic infection.
3.5. Prevention and advice
The high fatality rate and lack of effective treatments for cerebral fat embolism highlight the need for preventive measures. We recommend the following measures to minimize the incidence of this life-threatening complication of autologous fat grafting:
Cosmetic doctors should have an in-depth knowledge of the vascular anatomy of the face to avoid inadvertently injecting fat particles into the facial blood vessels.
The fat injection site should be selected very carefully. It is generally believed that transplanted adipose tissue is more likely to survive in highly vascularized areas such as muscle though this carries a higher risk of vascular damage. Hufschmidt et al. recommend separating the cheek into two specific areas according to the depth of injection (6). Ultrasound-guided injection or preoperative epinephrine can reduce vascular damage (9).
The operation should be strictly standardized, and the vital and neurological signs of the patient should be closely monitored. The use of local anesthesia, if possible, rather than general or intravenous anesthesia is preferred. Several authors have proposed that using blunt large-caliber cannulas rather than needles may prevent the puncture of small branch vessels, which is contrary to the findings of the review by Wang et al. (4, 6, 13). Vascular complications may be reduced by injecting less than the volume required to reach the ophthalmic artery or ICA (14). Thus, multi-channel syringes with a capacity of 1 mL may be safely applied. The injection should be very slow and should be followed by pulling back the syringe under low pressure, especially in high-risk areas. Wang et al. reported that minced fat is more likely to cause embolism, and a single injection of 0.05 mL is probably safe (2).
Potent treatments need to be found for patients who do develop cerebral fat embolism. The extremely low rate of recanalization and the high risk of distal vessel embolism lead to a low benefit of MT. Some authors have treated vascular embolism after hyaluronic acid injection by intra-arterial thrombolysis using hyaluronidase combined with urokinase, which resulted in a significant improvement (15). Specific drugs for dissolving fat emboli may be a new therapeutic target for future research.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements. Written informed consent was obtained from the individual(s) and/or minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
The clinical data and figures were collected by CL, JS, and SS. The original manuscript was written by YC, GY, and XH and then reviewed and edited by FL, JH, and GL. All authors read and approved the final manuscript.
Funding
This study was funded by grants from the Key Research and Development Plan of Shaanxi Province (2021SF-059) and the Natural Science Basic Research Program of Shaanxi (2023-JC-QN-0893).
Acknowledgments
The authors would like to thank Medjaden Inc. for the scientific editing of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CT, computed tomography; DWI, diffusion-weighted imaging; FLAIR, fluid-attenuated inversion recovery; ICA, internal carotid artery; MT, mechanical thrombectomy; ADAPT, a direct aspiration first-pass technology; SWIM, Solitaire FR/stent with intracranial support catheter for mechanical thrombectomy.
References
1. Simonacci F, Bertozzi N, Grieco MP, Grignaffini E, Raposio E. Procedure, applications, and outcomes of autologous fat grafting. Annals Med Surg. (2017) 20:49–60. doi: 10.1016/j.amsu.2017.06.059
2. Wang K, Rong X, Dang J, Yang J, Zheng H, Hou M, et al. Severe vascular complications caused by facial autologous fat grafting: a critical review. Ann Plast Surg. (2021) 86:S208–s19. doi: 10.1097/SAP.0000000000002691
3. Riley DS, Barber MS, Kienle GS, Aronson JK, Schoen-Angerer TV, Tugwell P, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epi. (2017) 89:218–35. doi: 10.1016/j.jclinepi.2017.04.026
4. Wang HC Yu N, Wang X, Dong R, Long X, Feng X, et al. Cerebral embolism as a result of facial filler injections: a literature review. Aesthet Surg J. (2022) 42:Np162–np75. doi: 10.1093/asj/sjab193
5. Lee DH, Yang HN, Kim JC, Shyn KH. Sudden unilateral visual loss and brain infarction after autologous fat injection into nasolabial groove. Br J Ophthalmol. (1996) 80:1026–7. doi: 10.1136/bjo.80.11.1026
6. Hufschmidt K, Bronsard N, Foissac R, Baqué P, Balaguer T, Chignon-Sicard B, et al. The infraorbital artery: clinical relevance in esthetic medicine and identification of danger zones of the midface. J Plast Reconstr Aesthet Surg. (2019) 72:131–6. doi: 10.1016/j.bjps.2018.09.010
7. Safran T, Abi-Rafeh J, Alhalabi B, Davison PG. The potential role of corticosteroid prophylaxis for the prevention of microscopic fat embolism syndrome in gluteal augmentations. Aesthet Surg J. (2020) 40:78–89. doi: 10.1093/asj/sjz166
8. Durán H, Cárdenas-Camarena L, Bayter-Marin JE, Ramos-Gallardo G, Robles-Cervantes JA. Microscopic and macroscopic fat embolism: solving the puzzle with case reports. Plast Reconstr Surg. (2018) 142:569e−77e. doi: 10.1097/PRS.0000000000004810
9. Dhooghe NS, Maes S, Depypere B, Claes KEY, Coopman R, Kubat B, et al. Fat embolism after autologous facial fat grafting. Aesthet Surg J. (2022) 42:231–8. doi: 10.1093/asj/sjab252
10. Danesh-Meyer H, Savino P, Sergott R. Ocular and cerebral ischemia following facial injection of autologous fat. Retin Cases Brief Rep. (2011) 5:273–4.
11. Lee KM, Kim EJ, Jahng GH, Chang DI. Magnetic resonance findings in two episodes of repeated cerebral fat embolisms in a patient with autologous fat injection into the face. J Korean Neurosurg Soc. (2012) 51:312–5. doi: 10.3340/jkns.2012.51.5.312
12. Renard D, Charavel P, Dahmani L, Freitag C. Cerebral fat embolism after autologous fat injection for reconstructive eye surgery. Rev Neurol. (2019) 175:94–5. doi: 10.1016/j.neurol.2018.01.382
13. Chatrath V, Banerjee PS, Goodman GJ, Rahman E. Soft-tissue filler-associated blindness: a systematic review of case reports and case series. Plast Reconstr Surg Glob Open. (2019) 7:e2173. doi: 10.1097/GOX.0000000000002173
14. Khan TT, Colon-Acevedo B, Mettu P, DeLorenzi C, Woodward JA. An anatomical analysis of the supratrochlear artery: considerations in facial filler injections and preventing vision loss. Aesthet Surg J. (2017) 37:203–8. doi: 10.1093/asj/sjw132
15. Zhang LX, Lai LY, Zhou GW, Liang LM, Zhou YC, Bai XY, et al. Evaluation of intra-arterial thrombolysis in treatment of cosmetic facial filler-related ophthalmic artery occlusion. Plast Reconstr Surg. (2020) 145:42e−50e. doi: 10.1097/PRS.0000000000006313
16. Feinendegen DL, Baumgartner RW, Schroth G, Mattle HP, Tschopp H. Middle cerebral artery occlusion AND ocular fat embolism after autologous fat injection in the face. J Neurol. (1998) 245:53–4. doi: 10.1007/s004150050177
17. Yoon SS, Chang DI, Chung KC. Acute fatal stroke immediately following autologous fat injection into the face. Neurology. (2003) 61:1151–2. doi: 10.1212/WNL.61.8.1151
18. Thaunat O, Thaler F, Loirat P, Decroix J P, Boulin A. Cerebral fat embolism induced by facial fat injection. Plast Reconstr Surg. (2004) 113:2235–6. doi: 10.1097/01.PRS.0000123627.33690.9E
19. Lee CM, Hong IH, Park SP. Ophthalmic artery obstruction and cerebralophthalmology. KJO. (2011) 25:358–61. doi: 10.3341/kjo.2011.25.5.358
20. Hong DK, Seo YJ, Lee JH, Im M. Sudden visual loss and multiple cerebral infarction after autologous fat injection into the glabella. Dermatol Surg. (2014) 40:485–7. doi: 10.1111/dsu.12426
21. Wang DW, Yin YM, Yao YM. Internal and external carotid artery embolism following facial injection of autologous fat. Aesthetic Surgery J. (2014) 34:NP83–7. doi: 10.1177/1090820X14539973
22. Chen W, Yang RY, A. case of sudden vision loss and multiple cerebral infarctions caused by autologous fat injection between eyebrows. J Pract Dermatol. (2015) 8:400–400.
23. Shen X, Li Q, Zhang H. Massive cerebral infarction following facial fat injection. Aesthetic Plast Surg. (2016) 40:801–5. doi: 10.1007/s00266-016-0681-2
24. Kang JH, Park KH, Park JS. Acute mental change and hemiplegia after autologous fat injection. J Cosmetic Laser Therapy Eur Soc Laser Dermatol. (2016) 18:413–6. doi: 10.1080/14764172.2016.1197400
25. Lu JQ, Liu HW, Wu YD, Xie B, Xiao LL, Li SH, et al. One case of bilateral massive cerebral infarction during autologous fat injection in the temporal region. J Lanzhou Univ. (2017) 43:23–7.
26. Wang XN, Jiang HQ, Lu N, Wang, JW. Clinical study on artery embolization caused by cosmetic facial filler injections. Chin J Stroke. (2017) 10:836–8.
27. Ji RJ, Xu ZQ, Luo BY. Two cases of acute cerebral infarction during facial autologous fat transplantation. Chin J Neurol. (2018) 51:249–55.
28. Huo X, Liu R, Wang Y, Sun J, Lin M, Han J, et al. Cerebral fat embolism as complication of facial fat graft: retrospective analysis of clinical002Ccharacteristics, treatment, and prognosis. World Neurosurg. (2018) 120:249–55. doi: 10.1016/j.wneu.2018.08.148
29. Wang X, Wu M, Zhou X, Liu H, Zhang Y, Wang H. Autologous fat used for facial filling can lead to massive cerebral infarction through middle cerebral artery or facial intracranial branches. J Cranio Surgery. (2018) 29:1341. doi: 10.1097/SCS.0000000000004625
30. Liu SX. Liang GC, Li KS, Xian WC, Zhu YC, Peng YQ, Zhong WT. A case of massive cerebral infarction caused by facial autologous fat injection. Hainan Med J. (2018) 29:1028–9.
31. Liu H, Wu X, Zhang X, Niu C, Zhu H. Internal carotid artery embolism after autologous fat injection for temporal augmentation. Aesthetic Plastic Surg. (2019) 43:383–7. doi: 10.1007/s00266-018-1265-0
32. Zhou K, Cai C. The successful mechanical lipectomy treatment of cerebral fat embolism following autologous fat injection. Plastic Reconst Surg Global Open. (2019) 7:91. doi: 10.1097/GOX.0000000000002091
33. Li F, Chen J, Sun DF, Jin Q, Zhang ZB. Massive cerebral infarction caused by autologous fat injection in the forehead: a case report. Chin J Plastic Surg. (2019) 35:638–40.
34. Huo K, Yuan XY, Chen C, Song WF, Qiao J, Ju XC, et al. Case of mechanical thrombectomy for acute occlusion of internal carotid artery caused by facial contour plastic surgery and literature review. Chin J Stroke. (2020) 15:899–903.
35. Lee HS, Park JJ, Roh HG, Lim SD. Unusual clinicopathological presentation of nontraumatic cerebral fat embolism Two-case report. Medicine. (2020) 45:99. doi: 10.1097/MD.0000000000019574
36. Xu Y, Chen LW, Zhang QB. A case of facial autologous fat transplantation complicated with massive cerebral infarction. Shanghai Med J. (2021)44:112–3.
37. Lu JP, Song XK, Cao YQ, Zhao JM. Acute visual loss and stroke following autologous fat injection into the temporal area. Neurol India. (2021) 69:1080–1. doi: 10.4103/0028-3886.325333
38. Liu C, Cai Z, Zhang L, Zhou M, He L. Case report and literature review: catastrophic embolism following cosmetic injection of autologous fat in the face. Front Med. (2021) 8:6657. doi: 10.3389/fmed.2021.646657
39. Miao J, Sun W, Zhu Z, Yang Z, Xu Y. A massive right hemisphere infarction after autologous fat grafting for facial filling. J Cranio Surg. (2021) 32:E215–7. doi: 10.1097/SCS.0000000000006898
40. Qian H, Ling Y, Zhang M, Lenahan C, Wang C, Zheng Z, et al. Massive cerebral infarction following facial injection of autologous fat: a case report and review of the literature. Front Hum Neurosci. (2021) 15:610945. doi: 10.3389/fnhum.2021.610945
41. Liang XM, Fu GH, Liang Y. Clinical study of facial injection of hyaluronic acid or autologous fat with occlusion of ophthalmic artery and cerebral artery. China Med Cosmetol. (2021) 11:50–3.
Keywords: autologous fat graft, facial injection, fat embolism, massive cerebral, infarction
Citation: Cheng Y, Yan G, Li C, Han X, Shang J, Shang S, Han J, Luo G and Liu F (2023) Case report and literature review: fatal cerebral fat embolism following facial autologous fat graft. Front. Neurol. 14:1180333. doi: 10.3389/fneur.2023.1180333
Received: 06 March 2023; Accepted: 06 July 2023;
Published: 04 August 2023.
Edited by:
Zhaolun Cai, Sichuan University, ChinaReviewed by:
M. Kamran Athar, Thomas Jefferson University, United StatesJian Wang, Ya'an People's Hospital, China
Anwen Shao, Zhejiang University, China
Copyright © 2023 Cheng, Yan, Li, Han, Shang, Shang, Han, Luo and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fude Liu, bGl1ZnVkZTEwMUAxNjMuY29t; Guogang Luo, bGd1b2dhbmdAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Yawen Cheng1†
Yawen Cheng1† Guogang Luo
Guogang Luo Fude Liu
Fude Liu