
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Neurol. , 16 March 2023
Sec. Neurotrauma
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1160382
This article is part of the Research Topic New Advances in Functional Rehabilitation After Central and Peripheral Nervous System Injury View all 8 articles
Editorial on the Research Topic
New advances in functional rehabilitation after central and peripheral nervous system injury
Nervous system injury, including central nerve injury and peripheral nerve injury, often leads to the loss of a patient's intelligence along with motor and sensory functions, and places a heavy burden on both the patient and their family. In adults, severe nerve injury can create significant difficulty for functional rehabilitation. The main reason for this is the death of neurons, demyelination, and nerve fiber regeneration failure at the site of injury. The nervous system is composed of neural tissue, which includes neurons, astrocytes, oligodendrocytes, microglia, and Schwann cells. The transmission of neural information between cells is achieved through complex crosstalk. At present, the regulation and remodeling mechanisms that each cell undergoes following injury to the nervous system remain very unclear. However, significant advances have been made in our understanding of functional rehabilitation following injury to the central and peripheral nervous systems (1). These new advances have reduced the possibility and intensity of side effects, and more importantly, have improved patients' quality of life.
Stroke is a complex disease that remains a global concern and results in nerve cell death and severe inflammation of the brain. According to the systematic review by Wang et al. included in this Research Topic, bone marrow mesenchymal stromal cells (BMSCs) provide an innovative strategy for stroke patients. In the central nervous system, transplanted BMSCs can promote M2 phenotype polarization of the microglia, resulting in the secretion of anti-inflammatory cytokines. Furthermore, the co-culture of BMSCs and astrocytes diminished the apoptosis of astrocytes and enhanced the level of neuroprotection. In the peripheral immune system, BMSCs and regulatory T cells (Treg) have been shown to provide immunomodulatory and neuroprotective functionality, respectively. From a molecular aspect, the transplantation of BMSCs to a lesion can result in the downregulation of several pro-inflammatory cytokines (IL-1, IL-6, TNF-α, and IFN-γ) and increased expression levels of anti-inflammatory cytokines, including IL-10 and TGF-β. Moreover, BMSCs may regulate neuroinflammation via growth factors or neurotrophins such as HGF and VEGF. Thus, BMSCs confer key neuroprotective effects after stroke.
Nerve regeneration is of vital importance when treating stoke. The activation of neurotrophic factors, along with their receptors and downstream pathways, is crucial (2). In this Research Topic, Mu et al. reviewed growth factors, such as nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF), and glial cell lineage-derived neurotrophic factor (GDNF), that are involved in many molecular pathways and that promote the progression of neurogenesis after stroke (Figure 1). However, other factors, such as the myelin proteins Nogo-A, MAG, and OMgp, are thought to inhibit neurogenesis by disturbing the local microenvironment. In addition, the authors also reviewed the research progress on the use of acupuncture to improve functional recovery by promoting neurogenesis after stroke.
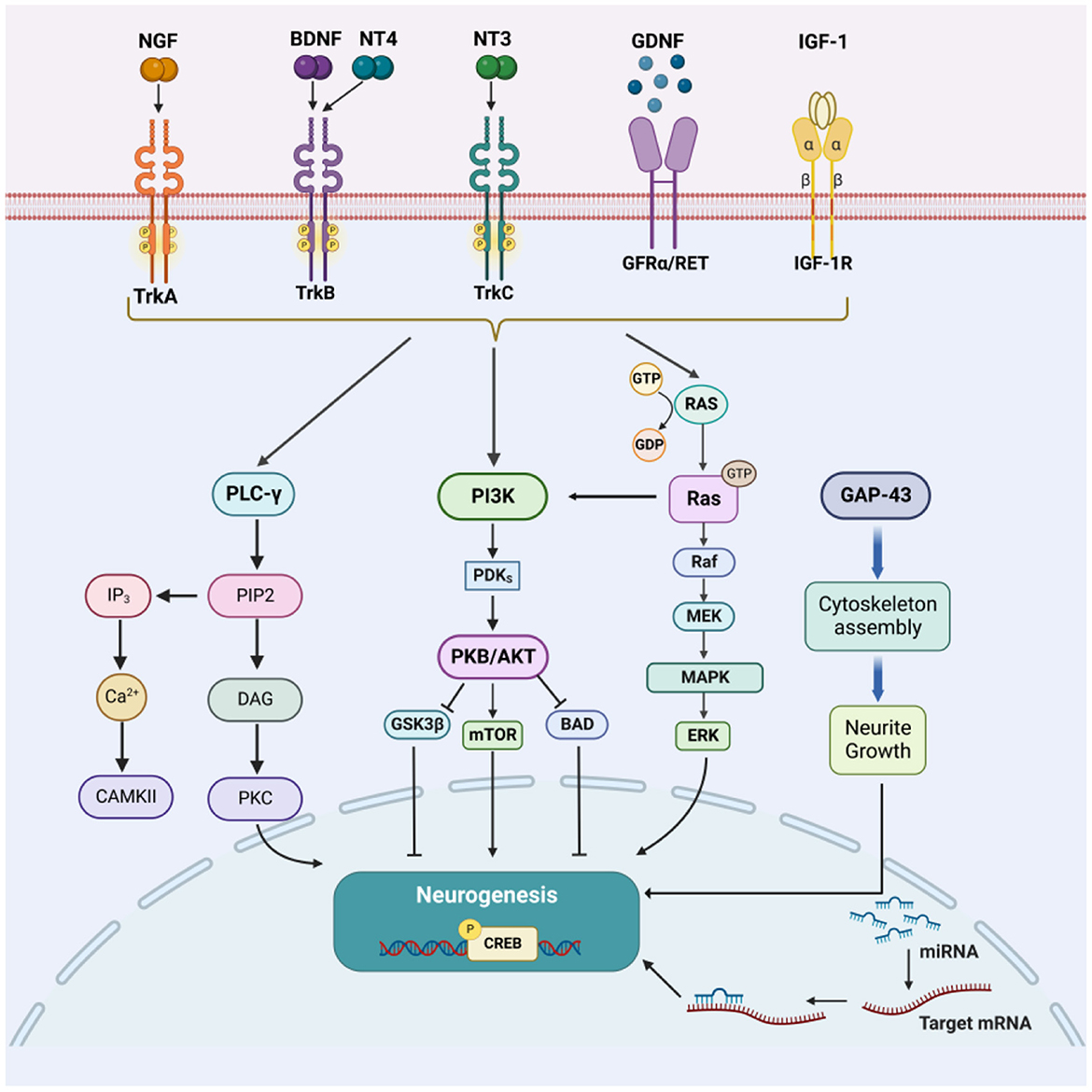
Figure 1. Diagram showing the factors that enhance neurogenesis and their major downstream signaling pathways following brain injury and stroke. Reprinted from Mu et al.
Apart from the direct injury site in the spinal cord, a series of secondary degenerative changes can spread across the entire neuroaxis from the spinal cord to the brain. Previously, researchers found that brain alterations following spinal cord injury (SCI) are associated with lesion severity and long-term outcomes. Thus, Yu et al. conducted a voxel-based meta-analysis to analyze a large dataset. The analysis showed that SCI patients exhibited a significant loss of gray matter volume (GMV) in the left insula and bilateral thalamus, along with a significant loss of white matter volume (WMV) in the bilateral corticospinal tract (CST). Their study was the first voxel-based meta-analysis to use SDM-PSI to evaluate morphological changes in the brains of patients after SCI. This technique estimates the severity of SCI in a visual manner and promotes the development of personalized treatment and clinical management.
As this technique matures, the treatment of nerve disease may become less sophisticated. Yu et al. reported advances in microvascular decompression (MVD) for classical trigeminal neuralgia (CTN) in terms of imaging and endoscopic techniques. High-resolution contrast-enhanced magnetic resonance imaging (MRI) can reveal and evaluate the location, degree, and range of neurovascular compression (NVC). Once the significantly responsible vessel has been identified by imaging, MVD can be targeted by a neurosurgeon. Furthermore, endoscopy provides a more optimized visualization of MVD as well as allowing a shorter surgical incision, thus reducing the possibility of postoperative headache, hearing loss, and other complications. Using this technique, possible pathogenic NVC vessels can be detected more reliably.
Peripheral nerve injuries can be caused by traffic accidents, sports, or other violent events. Trauma leads to nerve rupture, which often requires autologous nerve transplantation to reconstruct continuous nerve circuits. However, autologous nerve transplantation is still limited by a number of key hurdles, including nerve unavailability, size mismatch, and local tissue adhesion. To overcome these problems, Ye et al. developed a potential substitute material, which is referred to as decellularized tissue. This tissue substitute can provide a platform for cell adhesion, and its effects on tissue repair and the coordination of growth factors, cytokines, and chemokines, have already been proven. Of these decellularized tissues, decellularized nerve tissue (dN) is considered superior due to its homology; however, it is limited by longer peripheral nerve deficits. Thus, the authors selected decellularized kidney tissue (dK), which has been rarely studied, and compared this with dN. The authors found that dK played a more significant role in promoting axonal growth and the extension of neural-like cells, thus indicating that dK represents a promising bio-scaffold for nerve regeneration.
Acupuncture, as a traditional form of Chinese medicine, now plays an unexpected role in the treatment of nerve diseases. By inserting needles into the skin or deep tissues at specific locations (acupoints) on the body, the nerve endings beneath can be stimulated. A recent study showed that electroacupuncture treatment can regulate the expression of 173 mRNA, 260 lncRNA, and 153 circRNA differentially expressed genes after SCI, which are highly related to the signal pathways of inflammation, oxidative stress, apoptosis, and neuroprotection (3). In this Research Topic, Feng et al. conducted a meta-analysis to evaluate the effects of acupuncture on pain intensity and safety in patients suffering from neuropathic pain (NP). The analysis showed that the pain relief experienced by the acupuncture group was better than the sham intervention group or blank control group, although there was no significant difference between acupuncture and conventional drug treatments with regards to the treatment of NP. Moreover, acupuncture-induced adverse events were mild and reversible when compared to drug therapy, thus indicating that acupuncture is a relatively safe intervention for patients.
Finally, in recent years, crosstalk between the nerve system and bone has drawn the attention of researchers from different specialties (4, 5). For example, Liu et al. systematically reviewed the structural and functional interrelationships between the nerve system and bone. Innovatively, the authors developed a three-dimensional hard tissue clearing based on the polyethylene glycol (PEG)-associated solvent system, which can provide a more straightforward view of the nerve distribution in bone. Although we have a good understanding of how bone-related diseases can trigger pain, further research is needed to establish the specific mechanisms involved. Furthermore, postoperative nerve recovery and pain relief should be considered when it comes to treatment strategy. Liu et al. concluded that nerve fibers, growth factors, and neural-related cells are indispensable in the process of bone regeneration. Thus, we are more likely to witness a significant breakthrough in the repair of bone defects via nerve-related mechanisms.
Thanks to the efforts made by the abovementioned researchers, key mysteries in the field of nerve regeneration are finally being unraveled. The collection of studies presented in this Research Topic relating to the treatment of central and peripheral nervous diseases has provided some key new strategies and techniques.
YD and GL prepared the original draft. PZ and WZ critically reviewed and edited the manuscript. All authors have reviewed and approved the final manuscript.
YD was supported by the National Natural Science Foundation of China (Project no: 82074528) and the Guangdong Basic and Applied Basic Research Foundation (2023A1515012211). GL was supported by the National Natural Science Foundation of China (Project nos: 82271395 and 82001301), the Guangdong Basic and Applied Basic Research Foundation (2023A1515030073), the Youth Talent Two-way Exchange Project of Guangdong and Macao (KD0120230024), and the Special Project of Dengfeng Program of Guangdong Provincial People's Hospital (Project nos: KY0120220133, DFJHBF202111, and KJ012020630). PZ was supported by the National Natural Science Foundation of China (Project no: 22278003), the Beijing Natural Science Foundation (Project no: 22278003), and the Cross-cooperation project of Beijing Science and Technology New Star Program (Project no: 20220484232).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kathe C, Skinnider MA, Hutson TH, Regazzi N, Gautier M, Demesmaeker R, et al. The neurons that restore walking after paralysis. Nature. (2022) 611:540–7. doi: 10.1038/s41586-022-05385-7
2. Li G, Zhang B, Sun J-H, Shi L-Y, Huang M-Y, Huang L-J, et al. An NT-3-releasing bioscaffold supports the formation of TrkC-modified neural stem cell-derived neural network tissue with efficacy in repairing spinal cord injury. Bioact Mater. (2021) 6:3766–81. doi: 10.1016/j.bioactmat.2021.03.036
3. Xiao X, Deng Q, Zeng X, Lai B-Q, Ma Y-H, Li G, et al. Transcription profiling of a revealed the potential molecular mechanism of governor vessel electroacupuncture for spinal cord injury in rats. Neurospine. (2022) 19:757–69. doi: 10.14245/ns.2244452.226
4. Mi J, Xu J-K, Yao Z, Yao H, Li Y, He X, et al. Implantable electrical stimulation at dorsal root ganglions accelerates osteoporotic fracture healing via calcitonin gene-related peptide. Adv Sci (Weinh). (2022) 9:e2103005. doi: 10.1002/advs.202103005
Keywords: stroke, spinal cord injury, peripheral nerve injury, stem cell transplantation, biomaterials, electrical stimulation, acupuncture, neurogenesis
Citation: Ding Y, Li G, Zhang P and Zhang W (2023) Editorial: New advances in functional rehabilitation after central and peripheral nervous system injury. Front. Neurol. 14:1160382. doi: 10.3389/fneur.2023.1160382
Received: 07 February 2023; Accepted: 27 February 2023;
Published: 16 March 2023.
Edited and reviewed by: Elham Rostami, Uppsala University Hospital, Sweden
Copyright © 2023 Ding, Li, Zhang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Ding, ZGluZ3lpbmdAbWFpbC5zeXN1LmVkdS5jbg==; Ge Li, bGlnZUBnZHBoLm9yZy5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.