
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 20 June 2023
Sec. Stroke
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1148846
This article is part of the Research Topic Understanding PFO-associated stroke View all 9 articles
 Qingyang Yao1
Qingyang Yao1 Huahua Xiong2,3†
Huahua Xiong2,3† Daxue Zhang4
Daxue Zhang4 Shuqun Ren5
Shuqun Ren5 Wenwei Qi6
Wenwei Qi6 Xia Zou2,3
Xia Zou2,3 Yingying Zhao2,3
Yingying Zhao2,3 Shanshan Huang2,3
Shanshan Huang2,3 Jing Wang2,3
Jing Wang2,3 Liming Cao7,8*†
Liming Cao7,8*†Background: Right-to-left shunt (RLS) is associated with several conditions and causes morbidity. In this study, we aimed to evaluate the effectiveness of synchronous multimode ultrasonography in detecting RLS.
Methods: We prospectively enrolled 423 patients with high clinical suspicion of RLS and divided them into the contrast transcranial Doppler (cTCD) group and synchronous multimode ultrasound group, in which both cTCD and contrast transthoracic echocardiography (cTTE) were performed during the same process of contrast-enhanced ultrasound imaging. The simultaneous test results were compared with those of cTCD alone.
Results: The positive rates of grade II (22.0%:10.0%) and III (12.7%:10.8%) shunts and the total positive rate (82.1748%) in the synchronous multimode ultrasound group were higher than those in the cTCD alone group. Among patients with RLS grade I in the synchronous multimode ultrasound group, 23 had RLS grade I in cTCD but grade 0 in synchronous cTTE, whereas four had grade I in cTCD but grade 0 in synchronous cTTE. Among patients with RLS grade II in the synchronous multimode ultrasound group, 28 had RLS grade I in cTCD but grade II in synchronous cTTE. Among patients with RLS grade III in the synchronous multimode ultrasound group, four had RLS grade I in cTCD but grade III in synchronous cTTE. Synchronous multimode ultrasound had a sensitivity of 87.5% and specificity of 60.6% in the patent foramen ovale (PFO) diagnosis. Binary logistic regression analyses showed that age (odds ratio [OR] = 1.041) and risk of paradoxical embolism score ≥ 7 (OR = 7.798) were risk factors for stroke recurrence, whereas antiplatelets (OR = 0.590) and PFO closure with antiplatelets (OR = 0.109) were protective factors.
Conclusion: Synchronous multimodal ultrasound significantly improves the detection rate and test efficiency, quantifies RLS more accurately, and reduces testing risks and medical costs. We conclude that synchronous multimodal ultrasound has significant potential for clinical applications.
Patent foramen ovale (PFO) is a common congenital atrial septal defect in adults, with an incidence of 15–35% (1). PFO may lead to a right-to-left shunt (RLS), which is associated with migraine (2), cryptogenic stroke (3), and other conditions. RLS is an underappreciated cause of significant hypoxia, necessitating timely and accurate diagnosis to optimize management (4). The diagnosis of RLS is confirmed when microbubbles are observed in either the left atrium or ventricle on contrast transthoracic echocardiography (cTTE) and contrast transesophageal echocardiography (cTEE) or the middle cerebral arteries/vertebrobasilar artery on contrast transcranial Doppler (cTCD) after contrast injection. Reliable technology for detecting RLS/PFO is essential for the diagnosis and further treatment. Although cTCD, cTTE, and cTEE can be used to detect RLS/PFO (5), the most practical and cost-effective ultrasound modality remains debatable.
cTCD is a non-invasive, inexpensive, and easily repeatable screening tool for the detection of PFO. cTTE is a widespread initial screening tool for PFO because of its low cost, availability, and non-invasiveness (6). cTCD appears to be more sensitive than cTEE (7, 8); however, it is less specific than cTTE (9), cannot differentiate between cardiac and pulmonary shunts, and is easily affected by an inadequate acoustical temporal bone window. cTTE is disturbed by body position, subcutaneous fat in the thorax, and gas in the lungs (10). cTEE is regarded as the gold standard for the diagnosis of PFO (5); however, TEE is less sensitive than TTE in the diagnosis of RLS and underestimates shunt severity (11). The specificity is significantly improved when cTTE is combined with cTCD in detecting PFO (12). Some clinicians have used asynchronous cTCD and cTTE tests (multimode ultrasound) to screen for RLS (13). However, patients must undergo two contrast echocardiography procedures, which increase testing risks and costs.
In this study, we aimed to evaluate the effectiveness and feasibility of synchronous multimode ultrasound imaging to detect RLS by performing cTCD and cTTE during the same process of contrast-enhanced ultrasound.
The study was approved by the Ethics Review Board of the First Affiliated Hospital of Shenzhen University (No. 20220413006). All the enrolled participants signed an informed consent form.
From January 2021 to September 2021, 250 consecutive patients admitted to the First Affiliated Hospital of Shenzhen University with clinical suspicion of RLS were prospectively enrolled. The 423 patients were divided into the cTCD and multimode ultrasound groups according to the decision of the physician in charge. Baseline demographic characteristics are shown in Table 1. In the multimode ultrasound group, 73 participants eventually completed cTEE or TEE.

Table 1. Baseline characteristics of the study population and the comparison of RLS grades in synchronous multimode ultrasound and cTCD groups.
The diagnoses of cryptogenic stroke (14), hypertension (15), diabetes mellitus (16), and migraine (17) were confirmed based on the corresponding guidelines or diagnostic criteria. Patients with stroke are generally given secondary prevention drug treatment within 48 h of admission. Of the patients in this study, 10 out of 109 were stroke-related (the risk of paradoxical embolism [RoPE] score was ≥7) with large RLS and received surgical closure of PFO. The risk of paradoxical embolism was calculated based on the RoPE score, and surgical closure of PFO was proposed according to the Chinese expert consensus on preventive closure of patent foramen ovale (18). The average time from stroke onset to PFO occlusion was 50 days.
The inclusion criteria were as follows: age of 18–80 years, high clinical suspicion of RLS, voluntary participation, and good image quality in ultrasonic tests. The exclusion criteria were congenital heart diseases, such as atrial and ventricular septal defects, and the inability to perform the Valsalva maneuver (VM).
Activated saline contrast consisted of 8 mL of saline solution, 1 mL of air, and 1 mL of patient’s blood. The resulting fluid was vigorously mixed with two 20 mL syringes using a three-way pipe at least 20 times. We administered an intravenous bolus injection of activated saline contrast into the antecubital vein (11) using an 18-gauge needle to allow the bolus to reach the right atrium. Activated saline contrast injection was performed once at rest and twice during the VM.
The patients were trained to perform VM before the tests. The activated saline contrast was injected 5 s before the start of the VM. The patients were instructed to blow into a small soft plastic tube connector to a manometer. They were then required to maintain a minimum pressure of 40 mmHg for 5 s. The effective VM was identified by a peak Doppler flow velocity that decreased by at least 25% in the middle cerebral artery (11).
The cTCD test was performed using a TCD machine (DWL Doppler-Box; Germany) with a probe frequency of 2 MHz. For this test, participants were requested to lay in a comfortable left lateral position. We performed a single-channel TCD and double-depth monitoring, and the middle cerebral artery was observed through a temporal window. If the temporal window sound transmission was poor, a suboccipital window was selected to monitor the vertebral arteries. The first injection of activated saline contrast was conducted during rest and subsequently with the VM. The test was repeated after the first VM, and Doppler spectra were recorded for 25 s. We defined the cTCD outcome as positive for RLS when the TCD detected more than one microbubble within 25 s after the injection of activated saline (5). The test with the largest number of microbubbles was used to determine the RLS grade. The shunt grades (19) in the cTCD were as follows: grade 0 TCD (negative) = no microbubbles, grade I TCD = small shunt (1–10 microbubbles), grade II TCD = moderate shunt (10–30 microbubbles but no curtain), and grade III TCD = large shunt (more than 30 microbubbles, including the curtain pattern; Figure 1).
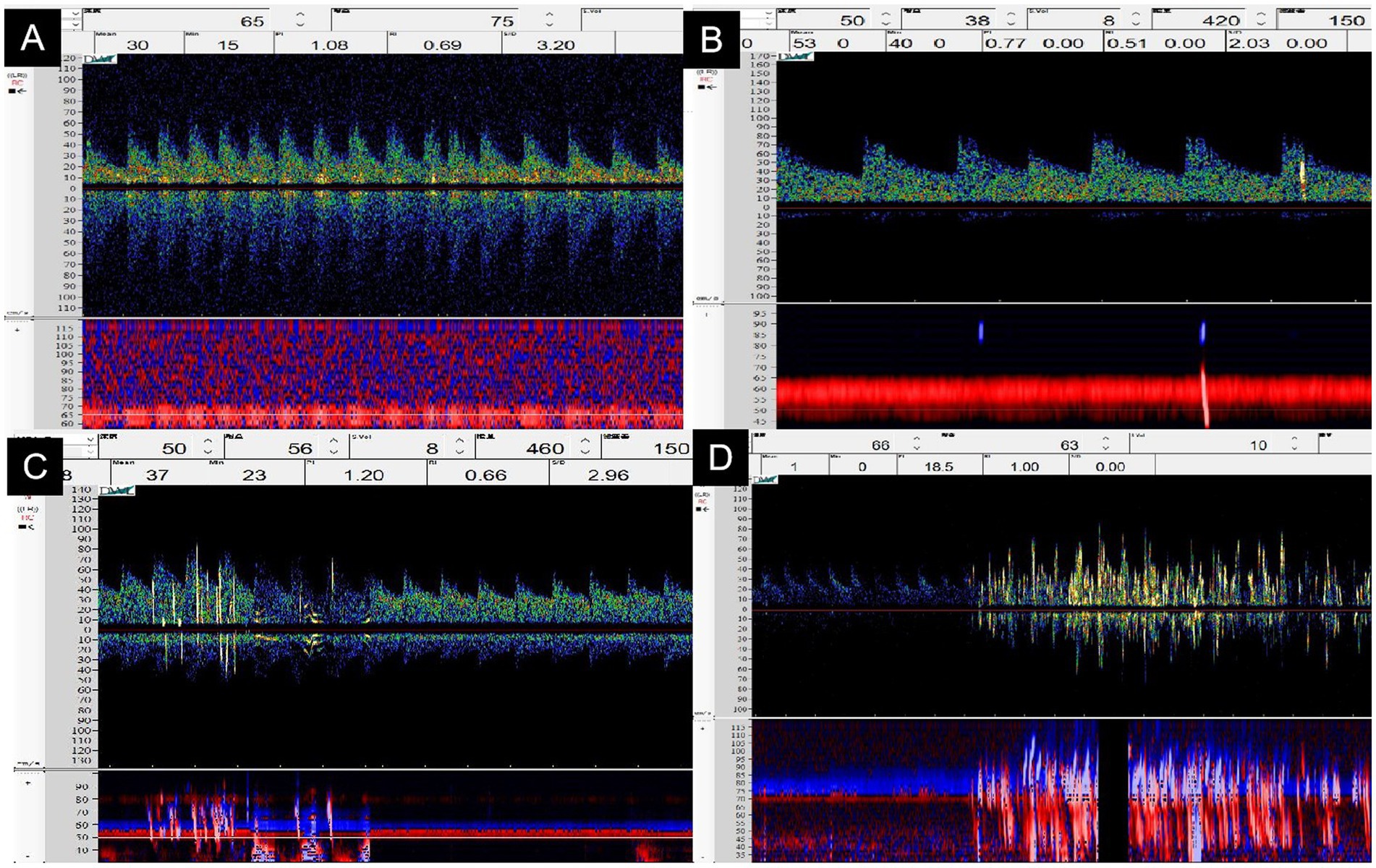
Figure 1. The grading classification of right-to-left shunts in contrast transcranial Doppler ultrasonography. (A) Grade 0TCD = no microbubbles. (B) Grade ITCD = 1–10 microbubbles (arrow). (C) Grade IITCD = 10–30 microbubbles but no curtain (arrow). (D) Grade IIITCD = curtain-like microbubbles (arrow).
cTTE was performed with an EPIQ 7C Color Doppler Ultrasound instrument (Philips, the Netherlands), with an X5-1 probe and a frequency of 1.0–5.0 MHz. We focused the ultrasound probe on the atrial septum and observed whether an interruption of echo continuity in the atrial septum and color blood flow through the interrupted site of the atrial septum were present. We recorded continuously during the contrast injections using the apical four-chamber view. When the TTE detected microbubbles in the left atrium within 5–7 cardiac cycles, the cTTE results were considered positive. The test in which the most microbubbles appeared in the left atrium was considered for the final result. The degree of shunt severity in cTTE based on the detected microbubbles in the left atrium was quantified as follows (6): grade 0 TTE (negative) = no microbubbles, grade I TTE = 1–10 microbubbles, grade II TTE = 11–30 microbubbles, and grade III TTE = more than 30 microbubbles (the left atrium is nearly filled with microbubbles or left atrial opacity is present; Figure 2).
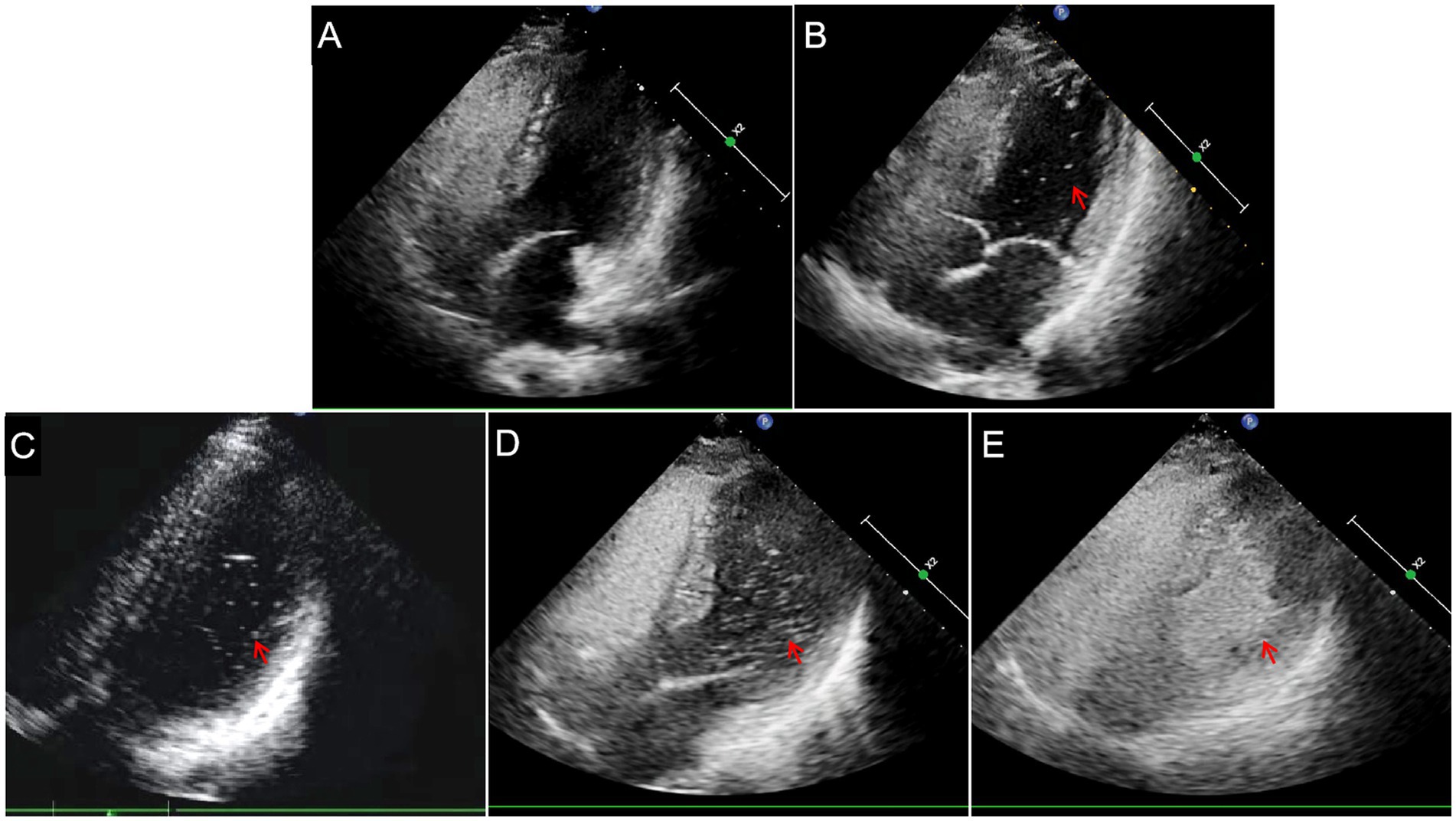
Figure 2. Semi-quantitative grading of right-to-left shunts in contrast transthoracic echocardiography. (A) Grade 0TTE = negative. (B) Grade ITTE = 1–10 microbubbles (arrow). (C) Grade IITTE = 11–30 microbubbles (arrow). (D) Grade IIITTE = >30 microbubbles (arrow) or (E) the left atrium is nearly filled with microbubbles (arrow).
cTEE was performed using a Philips EPIQ-7C instrument equipped with an X7-2t multiplane probe. All patients were fasting, and they were positioned in the left lateral decubitus position and received premedication with pharyngeal anesthesia using tetracaine. Blood pressure and electrocardiography findings were also monitored. Comprehensive two-dimensional color and spectral Doppler TEE were performed after the insertion of the probe. By observing the degree of involution of the foramen ovale valve under resting conditions, the presence of fissures between the septum primum and septum secundum, and the presence of color shunts observed by color Doppler (20), we confirmed the diagnosis of PFO when microbubbles (Supplementary Video 1) or color Doppler flow signals crossed from the foramen ovale (Supplementary Video 2). During the VM, the operator asked the patients to expand their abdomen and/or cough. An activated saline injection was performed posterior to the VM. We maintained continuous recording once during the basal condition and twice during the VM. The observations with the most microbubbles in the left atrium were regarded as the final results (13).
Two experienced ultrasound technicians performed synchronous detection of cTTE and cTCD in 173 patients. Each technician was blinded to the results obtained by the other technician during the inspection process. Both tests were performed using the same activated saline, posture, and VM. A fixed examiner instructed the patients to perform the VM. The result of the cTTE or cTCD with the most microbubbles was regarded as the final RLS grade in synchronous testing.
All statistical analyses were performed using SPSS (version 22.0; SPSS Inc., Chicago, IL, United States). The measured data showed a normal distribution and were expressed as the mean ± standard deviation.
The independent-sample t-test was used for between-group comparisons for age. Categorical variables are summarized as counts, and the differences between the two groups were analyzed using the chi-squared test. Risk factors for stroke recurrence were analyzed using binary logistic regression analysis. Statistical significance threshold was set at p < 0.05.
Table 1 presents the comparison of RLS manifestations between the synchronous multimode ultrasound and cTCD alone groups. The baseline data of the two groups were generally comparable (p > 0.05). However, the rate of grade II shunts (22.0%:10.0%) and total positive shunt rate (82.1%:74.8%) were significantly higher in the synchronous multimode ultrasound group than in the cTCD alone group (p = 0.001 and p = 0.048, respectively; Table 1).
Table 2 shows the comparison of RLS grades detected by cTCD with those detected by cTTE in patients from the synchronous multimode ultrasound group. Among the patients ultimately diagnosed with RLS grade I, 23 patients had RLS grade I in cTCD but grade 0 in synchronous cTTE, whereas four patients had RLS grade 0 in cTCD but grade I in synchronous cTTE. Among patients diagnosed with RLS grade II, 28 patients had RLS grade I in cTCD but RLS grade II in synchronous cTTE. Among patients diagnosed with RLS grade III, four patients had RLS grade I in cTCD but RLS grade III in synchronous cTTE.
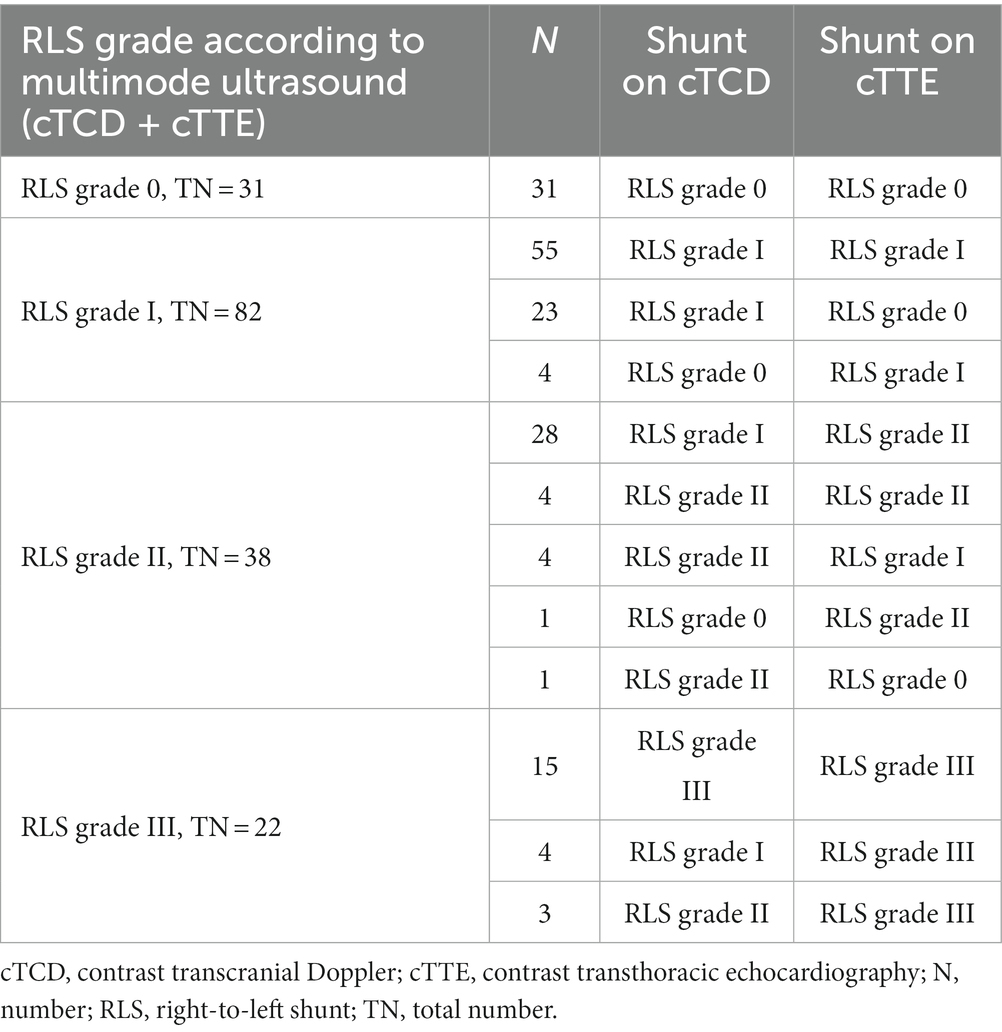
Table 2. Comparison of RLS grades detected by cTCD with those detected by cTTE in the synchronous multimode ultrasound group.
Table 3 shows the effectiveness of synchronous multimode ultrasound for the diagnosis of RLS/PFO when compared to that afforded by cTEE as the gold standard. Synchronous multimode ultrasound had a sensitivity of 87.5% and a specificity of 60.6%.
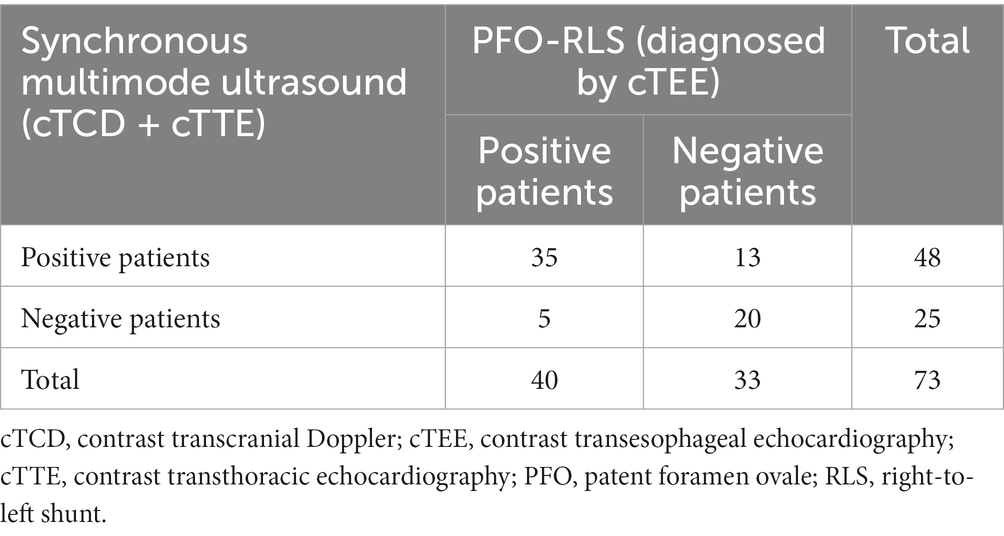
Table 3. Diagnostic effectiveness of synchronous multimode ultrasound for the diagnosis of PFO-RLS using cTEE as the gold standard.
Table 4 presents the comparison of RLS diagnoses in patients with cryptogenic stroke from the synchronous multimode ultrasound and cTCD alone groups. The total positivity rate (82.9%) was significantly higher as judged by the synchronous multimode ultrasound investigation than that reported by cTEE/TEE (61.4%, p = 0.005). RLS at all levels detected by multimode ultrasound was significantly different from that indicated by cTEE/TEE (p = 0.016).
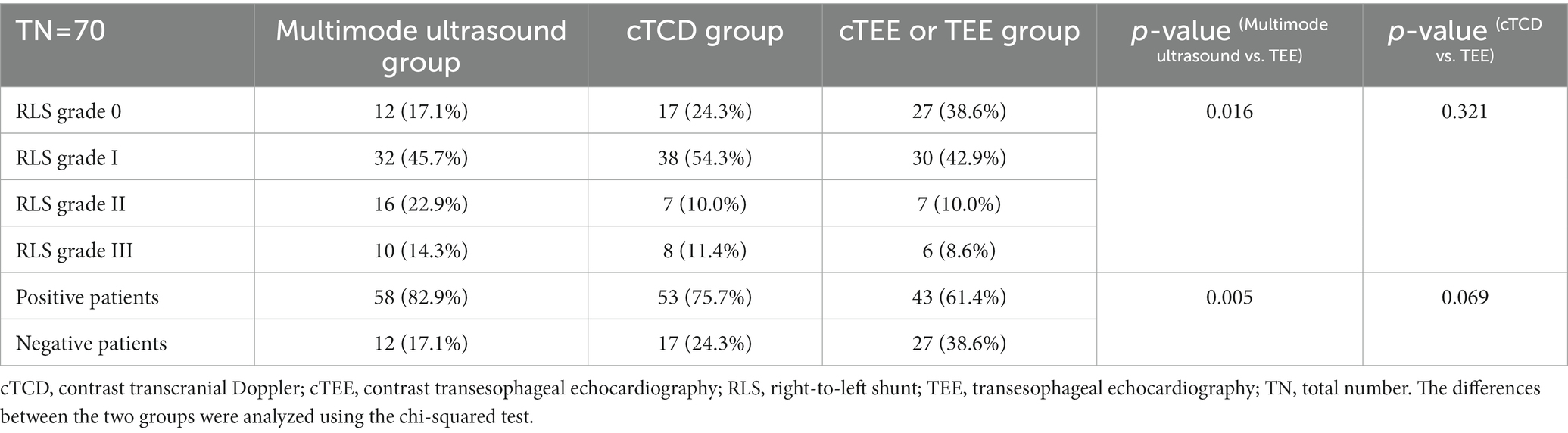
Table 4. Comparison of effectiveness of TCD alone and multimode ultrasound in patients with cryptogenic stroke.
Table 5 presents the comparison of clinical characteristics and stroke recurrence in patients with cryptogenic stroke that were diagnosed with RLS grade III and RLS grade < III. The rate of stroke recurrence was significantly different between these two groups (p = 0.013), and the RLS grade III group had a significantly higher number of patients with a RoPE score ≥ 7 (p = 0.001). The fractions of patients with cryptogenic stroke that had PFO closure and stroke recurrence are shown in Figure 3.
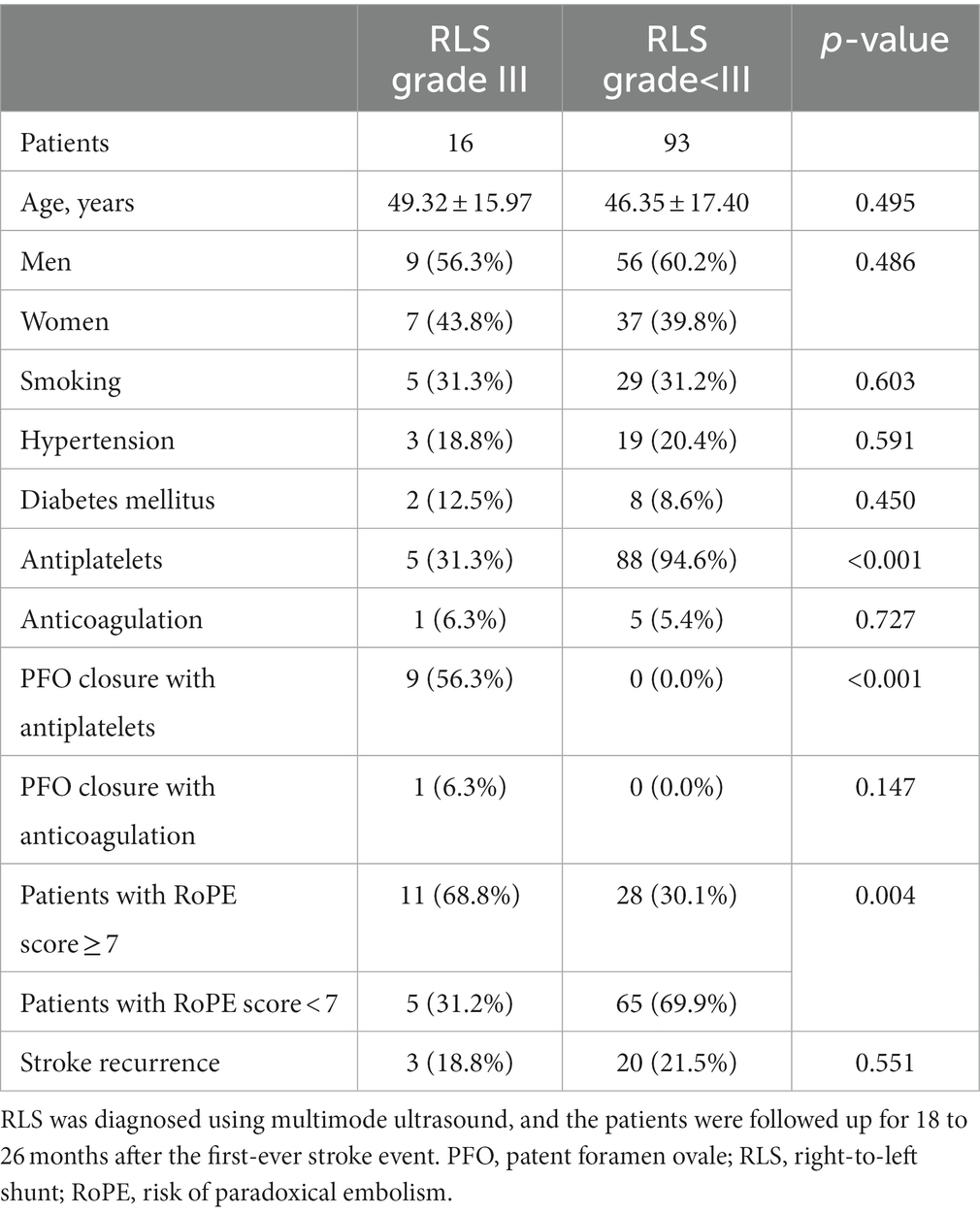
Table 5. Comparison of clinical characteristics between cryptogenic stroke patients with RLS grade III and those with RLS grade < III.
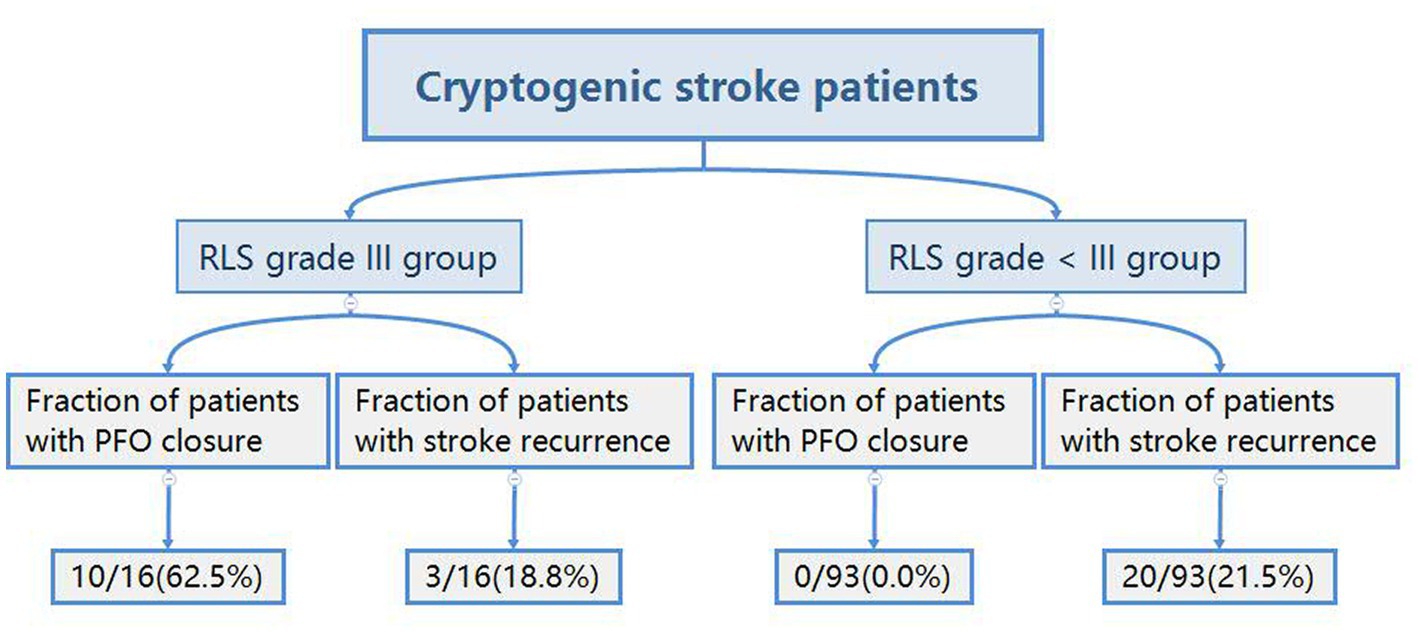
Figure 3. Flowchart of the state of patent foramen ovale closure and recurrence in patients with cryptogenic stroke. PFO, patent foramen ovale; RLS, right-to-left shunt.
Table 6 presents the results of binary logistic regression analyses of stroke recurrence. Age (odds ratio [OR] = 1.041) and RoPE score ≥ 7 (OR = 7.798) were risk factors for stroke recurrence, whereas therapy with antiplatelet drugs (OR = 0.590) and PFO closure combined with antiplatelet therapy (OR = 0.109) were protective factors against stroke recurrence.
We did not observe any complications during the synchronous multimode ultrasound.
In this study, the rate of RLS detection by the simultaneous multimodal ultrasound (cTTE and cTCD) was higher than that by cTCD alone, especially for RLS grades II and III. We showed that synchronous multimode ultrasound imaging significantly improved the detection rate of RLS and provided a more accurate classification of this condition. These advantages can help to diagnose stroke or migraine and assist with treatment decision-making.
Our study showed that TCD alone cannot reliably inform about the actual RLS grade and that using cTTE or cTCD for RLS/PFO screening is not completely interchangeable, as shown by the significant differences in the individual outcomes of simultaneous tests in the same patient (Table 2). Therefore, it is necessary to combine the results of both tests for the analysis. The synchronous test can significantly improve the total positive rate and detection rate of moderate/large RLS compared with the performance of the individual tests (Table 3).
Multimodal ultrasound imaging improved the sensitivity of RLS/PFO diagnosis for the following reasons: (1) Synchronous cTCD and cTTE combine the advantages of the two individual tests and avoid or reduce their shortcomings. This synergy increases the PFO detection rate. (2) The examiners need to count the number of microbubbles during cTTE. However, some microbubbles at certain levels, especially in small amounts, are not detected by the ultrasonic probe (21), and a single microbubble may be missed. (3) Obesity, pulmonary emphysema, other diseases, or VM affect the image quality of TTE (13), all of which can be avoided using cTCD. In cases of poor temporal bone windows or suspicious microbubble signals during cTCD (9), cTTE may be used to perform the test. (4) cTTE detects cardiac RLS directly in the heart, whereas cTCD detects only intracranial shunts, which are a subset of RLS (22). Therefore, the observed RLS values were not consistent. (5) Operators can mutually verify the examination results after the synchronous test of cTCD and cTTE, which helps gain additional experience.
Synchronous multimodal ultrasound can also improve the specificity of PFO diagnosis. cTCD neither displays an intracardiac structure nor identifies the source (e.g., pulmonary or cardiac) of RLS (13, 23). Furthermore, the atrial septum and intracardiac structures as well as the cardiac cycle in which the microbubbles appear can all be conveniently observed using cTTE, which helps determine whether there is a cardiogenic RLS. Most sonographers define a positive intracardiac RLS as comprising the passage of ≥1 microbubble into the left atrium within three cardiac cycles (10). It has been shown that the sensitivity and specificity for detecting PFO are higher within five cardiac cycles using cTTE (12). In addition, cTCD is a useful alternative for detecting PFO, especially for grades ≥ III (12). Therefore, a combination of cTCD and cTTE improves the specificity of PFO diagnosis.
Multimode ultrasound imaging can yield false-positive or false-negative results. False-positive results may be due to the mischaracterization of intrapulmonary shunts as intracardiac shunts. False-negative results are typically due to respiratory-phasic variation, inadequate VM, or inadequate use of agitated saline (4). Multimode ultrasound can also increase the testing costs for patients with negative results compared with those associated with cTCD or cTTE alone.
In a previous study, the detection rates of RLS grade II for cTTE and cTCD were 9.2 and 8.9%, respectively, whereas those of RLS grade III were 15.0 and 12.1%, respectively (21), which is consistent with our study findings. The detection rates of RLS grades II and III in the synchronous multimode ultrasound test were higher than those afforded by cTCD alone (Table 1).
Diagnosis of PFO using TCD has high sensitivity (95%) and specificity (92%). Therefore, TCD should be recommended as the first choice for PFO screening (24). cTTE can detect the majority of RLSs with better specificity than that of cTCD (25). Many experts believe that both cTCD and cTTE should be used as initial screening tests for PFO (6). A previous study (5) showed that the specificity was significantly higher, and the misdiagnosis rate was lower when cTTE was combined with cTCD to diagnose PFO.
In our experience, synchronous multimode ultrasound imaging can save patients’ time, make the test process more efficient, reduce the risk of the test, workload, and medical cost, and increase patient compliance. Most hospitals use asynchronous testing (13), which consists of cTCD first, followed by cTTE, or vice versa. To complete these tests sequentially rather than simultaneously, patients need to undergo two contrast echocardiography procedures, which extend the duration of work, decreases test efficiency, and increases the cost. Moreover, cTCD and cTTE can be completed by different operators in different locations, which may impede joint discussion and communication. Synchronous cTCD and cTTE tests can address these shortcomings. This approach is non-invasive and can be simultaneously completed with only one intravenous contrast-enhanced ultrasound, improving patient compliance. Sonographers and neurologists should coordinate the test time and place and collaboratively assess the test results. A better multi-disciplinary cooperation is critically important because the shunt grading by cTCD and cTTE indicates the size of the PFO and the next course of treatment (26).
A previous study (27) reported that the rate of RLS detection by cTCD in patients with cryptogenic stroke was 58.5%. In our study, we found a higher number of patients positive for RLS. There could be several possible reasons for this discrepancy. First, the participants in our study were patients with cryptogenic stroke or migraine, were at high risk of RLS, and were of younger age. Second, we adopted a standardized and quantifiable VM procedure, and the participants were fully trained before the test. Third, the procedures carried out by our specially-trained nurses may have produced more effective contrast enhancement with activated saline injection. Fourth, when the right atrium was filled with microbubbles and became blurry during the cTTE test, the participants were asked to relax, which facilitated detection of RLS at that time point.
Our study showed age and RoPE score ≥ 7 were risk factors for stroke recurrence. Age was shown to be a risk factor for ischemic stroke recurrence in patients with intracranial hemorrhage (28). In addition, older age is an independent predictor of atrial fibrillation after embolic stroke of undetermined source (ESUS) (29), and atrial fibrillation is a well-known risk factor for embolic stroke recurrence. The RoPE score positively correlates with the risk of stroke and is helpful in differentiating patients with ESUS and pathogenic PFO from those with incidental PFO (30).
Our study revealed that the use of antiplatelet treatment alone and PFO closure combined with antiplatelet treatment were protective factors against stroke recurrence. The subjects in this study received antiplatelet drugs more frequently than anticoagulants. Aspirin significantly reduced ischemic stroke recurrence (31). Anticoagulation therapy may reduce the risk of recurrent stroke more than antiplatelet therapy in patients with ESUS (32); however, there are also findings inconsistent with this notion (33). PFO closure in patients with cryptogenic stroke is superior to antithrombotic treatment in prevention of recurrence (34). PFO closure can be considered for the prevention of recurrent cryptogenic stroke in patients aged ≤60 years after a thorough evaluation, and PFO closure with medical therapy is more cost-effective than medical therapy alone (35).
The limitation of this study is that although we included a large number of patients, it was performed at a single center, and the results are only applicable to the selected population group. Larger multicenter studies evaluating more patients are needed to confirm our findings. Cooperating with cardiologists can help improve the methods and techniques for PFO detection.
We showed that screening for RLS/PFO using cTTE or cTCD was not completely interchangeable, and both cTCD and cTTE are necessary and complementary for detecting RLS/PFO. Synchronous multimode ultrasound (cTCD and cTTE) can significantly improve the detection rate and quantification of RLS, increase the test process efficiency, and reduce facility risks and medical costs. This test requires multi-disciplinary cooperation. We conclude that synchronous multimode ultrasound has great potential for clinical applications and deserves further investigation.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Ethics Review Board of the First Affiliated Hospital of Shenzhen University (No. 20220413006). The patients/participants provided their written informed consent to participate in this study.
LC and HX conceived the study, critically revised the manuscript, and obtained funding. QY conceived the study and wrote the first draft. DZ and SR provided constructive discussions and translated the manuscript. XZ, YZ, SH, and JW collected the data. WQ provided constructive discussions. All authors have read and approved the final manuscript.
This study was supported by the Shenzhen Second People’s Hospital Clinical Research Fund of the Guangdong Province High-level Hospital Construction Project (nos. 20223357021 and 20213357016), Guangdong Natural Science Funds (no. 2020B1515120061), and Department of Shenzhen Local Science and Technology Development (no. 2021Szvup052).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1148846/full#supplementary-material
SUPPLEMENTARY VIDEOS S1, S2 | The presence of a patent foramen ovale was confirmed when microbubbles (Video 1) or color Doppler flow signals (Video 2) crossed the foramen ovale.
cTCD, contrast transcranial Doppler; cTTE, contrast transthoracic echocardiography; ESUS, embolic stroke of undetermined source; OR, odds ratio; PFO, patent foramen ovale; RLS, Right-to-left shunt; RoPE, risk of paradoxical embolism; VM, Valsalva maneuver.
1. Romano, V, Gallinoro, CM, Mottola, R, Serio, A, Di Meglio, F, Castaldo, C, et al. Patent foramen ovale-a not so innocuous septal atrial defect in adults. J Cardiovasc Dev Dis. (2021) 8:60. doi: 10.3390/jcdd8060060
2. Kumar, P, Kijima, Y, West, BH, and Tobis, JM. The connection between patent foramen ovale and migraine. Neuroimaging Clin N Am. (2019) 29:261–09. doi: 10.1016/j.nic.2019.01.006
3. Giblett, JP, Abdul-Samad, O, Shapiro, LM, Rana, BS, and Calvert, PA. Patent foramen ovale closure in 2019. Interv Cardiol. (2019) 14:34–41. doi: 10.15420/icr.2018.33.2
4. Montrief, T, Alerhand, S, Denault, A, and Scott, J. Point-of-care echocardiography for the evaluation of right-to-left cardiopulmonary shunts: a narrative review. Can J Anaesth. (2020) 67:1824–38. doi: 10.1007/s12630-020-01813-2
5. Caputi, L, Carriero, MR, Falcone, C, Parati, E, Piotti, P, Materazzo, C, et al. Transcranial Doppler and transesophageal echocardiography: comparison of both techniques and prospective clinical relevance of transcranial Doppler in patent foramen ovale detection. J Stroke Cerebrovasc Dis. (2009) 18:343–8. doi: 10.1016/j.jstrokecerebrovasdis.2008.12.001
6. Zhao, E, Wei, Y, Zhang, Y, Zhai, N, Zhao, P, and Liu, B. A comparison of transthroracic echocardiograpy and transcranial doppler with contrast agent for detection of patent foramen ovale with or without the valsalva maneuver. Medicine (Baltimore). (2015) 94:e1937. doi: 10.1097/MD.0000000000001937
7. Wessler, BS, Kent, DM, Thaler, DE, Ruthazer, R, Lutz, JS, and Serena, J. The RoPE score and right-to-left shunt severity by transcranial doppler in the CODICIA study. Cerebrovasc Dis. (2015) 40:52–8. doi: 10.1159/000430998
8. Maillet, A, Pavero, A, Salaun, P, Pibourdin, A, Skopinski, S, Thambo, JB, et al. Transcranial doppler to detect right to left communication: evaluation versus transesophageal echocardiography in real life. Angiology. (2018) 69:79–82. doi: 10.1177/0003319717712356
9. Katsanos, AH, Psaltopoulou, T, Sergentanis, TN, Frogoudaki, A, Vrettou, AR, Ikonomidis, I, et al. Transcranial Doppler versus transthoracic echocardiography for the detection of patent foramen ovale in patients with cryptogenic cerebral ischemia: a systematic review and diagnostic test accuracy meta-analysis. Ann Neurol. (2016) 79:625–5. doi: 10.1002/ana.24609
10. Mahmoud, AN, Elgendy, IY, Agarwal, N, Tobis, JM, and Mojadidi, MK. Identification and quantification of patent foramen ovale-mediated shunts: echocardiography and transcranial doppler. Interv Cardiol Clin. (2017) 6:495–4. doi: 10.1016/j.iccl.2017.05.002
11. González-Alujas, T, Evangelista, A, Santamarina, E, Rubiera, M, Gómez-Bosch, Z, Rodríguez-Palomares, JF, et al. Diagnosis and quantification of patent foramen ovale. Which is the reference technique? Simultaneous study with transcranial Doppler, transthoracic and transesophageal echocardiography. Rev Esp Cardiol. (2011) 64:133–9. doi: 10.1016/j.recesp.2010.10.009
12. Yang, J, Zhang, H, Wang, Y, Zhang, S, Lan, T, Zhang, M, et al. The efficacy of contrast transthoracic echocardiography and contrast transcranial doppler for the detection of patent foramen ovale related to cryptogenic stroke. Biomed Res Int. (2020) 2020:1513409. doi: 10.1155/2020/1513409
13. Yang, X, Wang, H, Wei, Y, Zhai, N, Liu, B, and Li, X. Diagnosis of patent foramen ovale: the combination of contrast transcranial doppler, contrast transthoracic echocardiography, and contrast transesophageal echocardiography. Biomed Res Int. (2020) 2020:8701759. doi: 10.1155/2020/8701759
14. Adams, HP, Bendixen, BH, Kappelle, LJ, Biller, J, Love, BB, Gordon, DL, et al. Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial. TOAST. Trial of org 10172 in acute stroke treatment. Stroke. (1993) 24:35–41. doi: 10.1161/01.STR.24.1.35
15. Wang, W. New aspect of the 2010 China hypertension guideline. Chin Commun Physici-Ans. (2011) 24:21. Chinese
16. Society of Diabetes, Chinese Medical Association. China prevention and cure guidelines (2017) of type 2 diabetes. Chin J Diabetes (2018) 10:4–67. Chinese. doi: 10.3760/cma.j.issn.1674-5809.2018.01.003
17. Yu, S. New classification and diagnosis of cephalagra. Chin J Postgrad Med. (2005) 7:3–5. doi: 10.3760/cma.j.issn.1673-4904.2005.07.001
18. Cardiovascular Internal Medicine Branch of Chinese Medical Association, Cardiovascular Internal Medicine Branch of Chinese Medical Doctor Association. Chinese expert consensus on preventive closure of patent foramen ovale. Chin Circ. J. (2017) 32:209–4. Chinese. doi: 10.3969/j.issn.1000-3614.2017.03.001
19. Maffè, S, Dellavesa, P, Zenone, F, Paino, AM, Paffoni, P, Perucca, A, et al. Transthoracic second harmonic two- and three-dimensional echocardiography for detection of patent foramen ovale. Eur J Echocardiogr. (2010) 11:57–63. doi: 10.1093/ejechocard/jep165
20. Zhao, Q, Liu, R, Zhou, J, Dong, Z, and Chen, Y. Prevalence and grade of RLS in migraine: a prospective study of 251 migraineurs by synchronous test of c-TTE and c-TCD. Medicine (Baltimore). (2021) 100:e24175. doi: 10.1097/MD.0000000000024175
21. Duan, Z, Yang, Z, Song, B, Wang, Y, Shang, D, and Du, Y. Combined application of c-TTE and c-TCD in detecting PFO-RLS. Chin J Practical Nerv Dis. (2019) 22:183–6. doi: 10.12083/SYSJ.2019.02.035
22. Cao, L, Huang, X, and Wang, H. Relevance of small right-to-left shunt in contrast-enhanced transcranial Doppler in young and middle-aged patients with cryptogenic stroke: a report of two cases and literature review. Int J Neurosci. (2021) 132:1118–22. doi: 10.1080/00207454.2020.1865345
23. Droste, DW, Schmidt-Rimpler, C, Wichter, T, Dittrich, R, Ritter, M, Stypmann, J, et al. Right-to-left-shunts detected by transesophageal echocardiography and transcranial Doppler sonography. Cerebrovasc Dis. (2004) 17:191–6. doi: 10.1159/000075790
24. Komar, M, Olszowska, M, Przewłocki, T, Podolec, J, Stępniewski, J, Sobień, B, et al. Transcranial Doppler ultrasonography should it be the first choice for persistent foramen ovale screening? Cardiovasc Ultrasound. (2014) 12:16. doi: 10.1186/1476-7120-12-16
25. Zito, C, Dattilo, G, Oreto, G, Di Bella, G, Lamari, A, Iudicello, R, et al. Patent foramen ovale: comparison among diagnostic strategies in cryptogenic stroke and migraine. Echocardiography. (2009) 26:495–3. doi: 10.1111/j.1540-8175.2008.00852.x
26. Chen, J, Chen, L, Hu, W, Ni, X, Zhang, Z, Feng, X, et al. A comparison of contrast transthoracic echocardiography and contrast transcranial Doppler in cryptogenic stroke patients with patent foramen ovale. Brain Behav. (2019) 9:e01283. doi: 10.1002/brb3.1283
27. Xie, J, Wang, Y, Peng, W, Huang, S, and Lai, X. Comparison of contrast-transesophageal echocardiography with contrast-TCD in detection of right-to-left shunt in patients with cryptogenic stroke. J Clin Neurol. (2018) 31:341–3. doi: 10.3969/j.issn.1004-1648.2018.05.007
28. Wong, YS, Tsai, CF, and Ong, CT. Risk factors for stroke recurrence in patients with hemorrhagic stroke. Sci Rep. (2022) 12:17151. doi: 10.1038/s41598-022-22090-7
29. Bahit, MC, Sacco, RL, Easton, JD, Meyerhoff, J, Cronin, L, Kleine, E, et al. Predictors of atrial fibrillation development in patients with embolic stroke of undetermined source: an analysis of the RE-SPECT ESUS trial. Circulation. (2021) 144:1738–46. doi: 10.1161/CIRCULATIONAHA.121.055176
30. Strambo, D, Sirimarco, G, Nannoni, S, Perlepe, K, Ntaios, G, Vemmos, K, et al. Embolic stroke of undetermined source and patent foramen ovale: risk of paradoxical embolism score validation and atrial fibrillation prediction. Stroke. (2021) 52:1643–52. doi: 10.1161/STROKEAHA.120.032453
31. Kong, T, Chen, J, Sun, K, Zhang, W, Wang, J, Song, L, et al. Aspirin reduced recurrent stroke risk in patients with lacunar stroke. Acta Neurol Scand. (2019) 140:78–83. doi: 10.1111/ane.13105
32. Sato, N, Matsuo, R, Kiyuna, F, Nakamura, K, Hata, J, Wakisaka, Y, et al. Anticoagulation and risk of stroke recurrence in patients with embolic stroke of undetermined source having no potential source of embolism. Cerebrovasc Dis. (2020) 49:601–8. doi: 10.1159/000510773
33. Uchiyama, S, Toyoda, K, Lee, BC, Liou, CW, Wong, LKS, Grauer, C, et al. Dabigatran or aspirin in east asian patients with embolic stroke of undetermined source: RE-SPECT ESUS subgroup analysis. Stroke. (2021) 52:1069–73. doi: 10.1161/STROKEAHA.120.031891
34. Hviid, CVB, Simonsen, CZ, and Hvas, AM. Recurrence risk in patients with cryptogenic stroke, patent foramen ovale, and thrombophilia: a systematic review and meta-analysis. Thromb Haemost. (2019) 119:1839–48. doi: 10.1055/s-0039-1693739
Keywords: synchronous test, multimode ultrasound, contrast-transthoracic echocardiography, contrast-transcranial Doppler, right-to-left shunt, test effect
Citation: Yao Q, Xiong H, Zhang D, Ren S, Qi W, Zou X, Zhao Y, Huang S, Wang J and Cao L (2023) Synchronous multimode ultrasound for assessing right-to-left shunt: a prospective clinical study. Front. Neurol. 14:1148846. doi: 10.3389/fneur.2023.1148846
Received: 02 February 2023; Accepted: 31 May 2023;
Published: 20 June 2023.
Edited by:
Theodoros Karapanayiotides, Aristotle University of Thessaloniki, GreeceReviewed by:
Jesus Juega, Vall d’Hebron University Hospital, SpainCopyright © 2023 Yao, Xiong, Zhang, Ren, Qi, Zou, Zhao, Huang, Wang and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liming Cao, Y2FvbG0tMjAwN0AxNjMuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.