- Department of Neurological Rehabilitation, Zhengzhou Central Hospital Affiliated to Zhengzhou University, Zhengzhou, China
Introduction: Postural balance is impaired in patients with chronic low back pain (CLBP). In addition, the swaying velocity can be affected by low back pain (LBP) dysfunction. However, the extent to which the dysfunction affects postural balance in CLBP patients remains unclear. Therefore, this study aimed to investigate the effect of LBP-related disability on postural balance among CLBP patients and determine factors associated with postural balance impairments.
Methods: Participants with CLBP were recruited and instructed to complete the one-leg stance and Y-balance test. Moreover, they were divided into two subgroups (i.e., low and medium to high LBP-related disability groups) to compare the difference in postural balance based on the degree of LBP-related disability measured by the Roland Morris Disability Questionnaire. The relationships between postural balance and negative emotions as well as LBP characteristics were determined using the Spearman correlations.
Results: A total of 49 participants with low LBP-related disabilities and 33 participants with medium to high LBP-related disabilities participated in the study. Compared to the medium to high LBP-related disability group, patients in the low LBP-related disability group performed better in one-leg stance on the left leg (z = -2.081, p = 0.037). For Y-balance test, patients in the low LBP-related disability group also had greater normalized values of left leg reach in posteromedial (t = 2.108, p = 0.038) direction and composite score (t = 2.261, p = 0.026) and of right leg reach in posteromedial (t = 2.185, p = 0.032), and posterolateral (t = 2.137, p = 0.036) directions as well as composite score (t = 2.258, p = 0.027). Factors associated with postural balance impairments were also revealed, such as anxiety, depression, and fear avoidance belief.
Discussion: The greater the dysfunction degree, the worse the CLBP patient’s postural balance impairment. Negative emotions could also be considered contributing factors for postural balance impairments.
1. Introduction
Low back pain (LBP) is one of the most frequently occurring musculoskeletal complaints with a lifetime prevalence of up to 80% (1, 2). Although in most cases, the disease is self-limited and naturally resolves within 6 weeks, approximately 20% of cases may progress to chronic low back pain (CLBP), thereby resulting in greater burdens on health and economy (3). However, CLBP is difficult to treat and is associated with various mechanical changes (4). After taking age into account as a major determinant of balance, LBP may still explain 9% of the variance in balance (5).
Postural balance is the ability to maintain or restore body balance under static or dynamic conditions (6), which requires stable central nervous system function and good sensory and motor system function. Postural balance in patients with CLBP may be impaired by central and/or peripheral mechanisms. Constant interaction between central and peripheral mechanisms is required to maintain balance. Peripheral mechanisms of balance include (1) somatosensory systems (e.g., receptors in joints, muscles, and ligaments) that provide input regarding joint position and force, (2) the visual system, which provides input about the environment, and (3) the vestibular system, which provides input regarding angular velocity and linear acceleration. The central nervous system integrates peripheral inputs and controls appropriate muscular responses to maintain balance. If any of these components are impaired, postural balance impairment may occur. The core basis of CLBP is a chronic injury to the muscles of the low back, accompanied by changes in the nervous system (7). For example, Henry et al. (8) reported that individuals with CLBP have abnormal automatic postural coordination, which indicates altered neuromuscular control (8). And Yu et al. (9) found that individuals with CLBP had lower cerebellar gray matter density which is essential for balance control (9).
Thus, optimal postural balance is necessary to perform normal activities of daily living. Although balance assessments have been performed with expensive laboratory equipment, such laboratory equipment is impractical in a clinical setting (10–12). One-leg stance (OLS) and Y-balance test (YBT) are available and inexpensive to measure static and dynamic balance, which have high intra- and inter-rater reliability and can be easily implemented in clinical practice (12, 13).
When compared to healthy controls, there is an impaired performance in OLS and YBT in those with CLBP, which may affect spinal stability (14). Impaired postural balance may increase the compression load on the spine, thereby resulting in the risk of future deterioration (15). In addition, CLBP patients might modify their motor control strategies in an attempt to prevent further pain (16, 17). Postural balance may be influenced by other factors, such as age, impaired proprioception, muscle strength, and coordination (16, 18). As there is a lack of evidence on the effect of negative emotions on postural balance in those with CLBP (16), their relationships remain to be determined.
Furthermore, functional disability may be a potential contributing factor to postural strategies adopted by CLBP patients (19). A Brazilian epidemiological study has shown that 27.7 and 22.7% of CLBP patients had LBP-related disabilities and changes in postural balance, respectively (20). Brech et al. (4) found that the degree of LBP-related disability is negatively correlated with the swaying velocity of OLS among women with CLBP (4), which means CLBP women with greater dysfunction have better postural balance. This unexpected result may be due to the subjects’ compensation and the number and type of subjects included (10 women). Thus, whether the effect of LBP-related disability on postural balance would have similar results in the general CLBP population remains unclear.
Assessment of balance is an important management aspect of CLBP, providing useful clinical information that could be incorporated into rehabilitation programs. Thus, this study aims to explore the effect of LBP-related disability on postural balance among patients with CLBP, and determine the factors (e.g., negative emotions and LBP characteristics) related to postural balance. The first hypothesis of this study is that participants with greater LBP-related disability would have worse balance performance in OLS and YBT. The second hypothesis is that negative emotions (e.g., anxiety, depression, and fear avoidance belief) and LBP characteristics would be negatively correlated with postural balance.
2. Materials and methods
2.1. Participants
CLBP subjects were recruited in a local community through posted advertisements. Inclusion criteria were pain in the lumbar and sacroiliac joint regions that had lasted more than 12 weeks before the test and an average pain intensity score of ≥2/10 on the numerical rating scale (NRS) in the past week. Alshehre et al. (12) found a moderate effect for the Y balance test in young adults with CLBP of NRS ≥ 2/10 (12). Meanwhile, exclusion criteria were patients who reported current pregnancy, signs of nerve root compression, serious spinal conditions (e.g., tumor, infection, or fracture), specific balance issues (e.g., vestibular apparatus problem or uncorrected visual disturbances), history of surgery to the lower extremity or spine, or pain in the joints of the lower extremities. In addition, none of the participants had been treated with CLBP in the past 12 weeks. This study was approved by the Ethics Committee of Zhengzhou Central Hospital Affiliated to Zhengzhou University (No.: 201966).
Once participants were determined to be eligible for the study, their demographic and clinical characteristics were collected, including age, sex, height, weight, and body mass index (BMI), as well as leg length (LL), duration, and location of LBP. LL is the distance between the anterior superior iliac spine and the ipsilateral medial malleolus at supine position (12, 21). Furthermore, participants rated their current pain and average pain intensity in the past week using the NRS. Participants also completed the Roland Morris Disability Questionnaire (RMDQ) to evaluate LBP-related disability, the Self-Rating Anxiety Scale (SAS) to evaluate anxiety in the last week, the Self-Rating Depression Scale (SDS) to evaluate depression in the last week, and the Fear-Avoidance Beliefs Questionnaire for physical activities (FABQp) and work activities (FABQw) to evaluate the fear-avoidance level.
As a widely employed scale with good validity and reliability, RMDQ can allow quantification and further classification of LBP by the extent of its impact on physical function (19). Although cutoff points of RMDQ have not been established clearly, Kimachi et al. (19) found that the level of dysfunction based on RMDQ was associated with an increased risk of falls in the elderly, and the incidence of any fall over the past year was 27.8% of those with low LBP-related disability (RMDQ = 1–5) and 37.6% of those with medium to high level of LBP-related disability (RMDQ = 6–24) (19). Thus, in the present study, participants were divided into two subgroups based on the degree of LBP-related disability measured by RMDQ to compare the difference in postural balance: low (RMDQ = 1–5) and medium to high LBP-related disability (RMDQ = 6–24).
2.2. Procedures
Herein, subjects were asked to perform the OLS to assess their static postural balance (22). During the test, subjects were asked to stand on one leg on a force platform with bare feet and eyes closed. The test ended when the non-standing foot touched the floor or the standing leg, and a timer was used to record the duration. The order of one-leg stance on the left (OLS-L) and right (OLS-R) legs was randomized with random numbers table to minimize the order effect. Subjects practiced thrice on each leg for familiarization. Then, they completed three trials for each leg with the mean value for analysis. There was a 30 s break between trials to avoid fatigue.
Afterward, subjects were instructed to complete YBT correctly to evaluate their dynamic balance (12). The test involves maximal reaching distances in anterior (AT), posterolateral (PL), and posteromedial (PM) directions from the central stance platform at an angle of 120° (Figure 1). During the test, participants were instructed to keep the standing leg on the central stance platform barefooted, and use another bare foot to slide and reach the indicators in three directions as far as possible, and then return to their initial standing position while maintaining their balance. Moreover, the testing orders of the reaching directions and legs were randomized with random numbers table to minimize the order effect. Subjects practiced thrice in each direction for familiarization. Then, they completed three trials in each direction with the mean value for analysis. There were 10 s breaks between trials and 30 s breaks between reach directions and between legs to minimize fatigue. The outcome measures of interest were the distances to be reached in the three directions, the composite score (CS), and the normalized reach. The composite score was calculated as [(AT ± PM ± PL)/(3 × LL)]. Normalized reach was calculated as [(reach distance/LL) × 100%] (12).
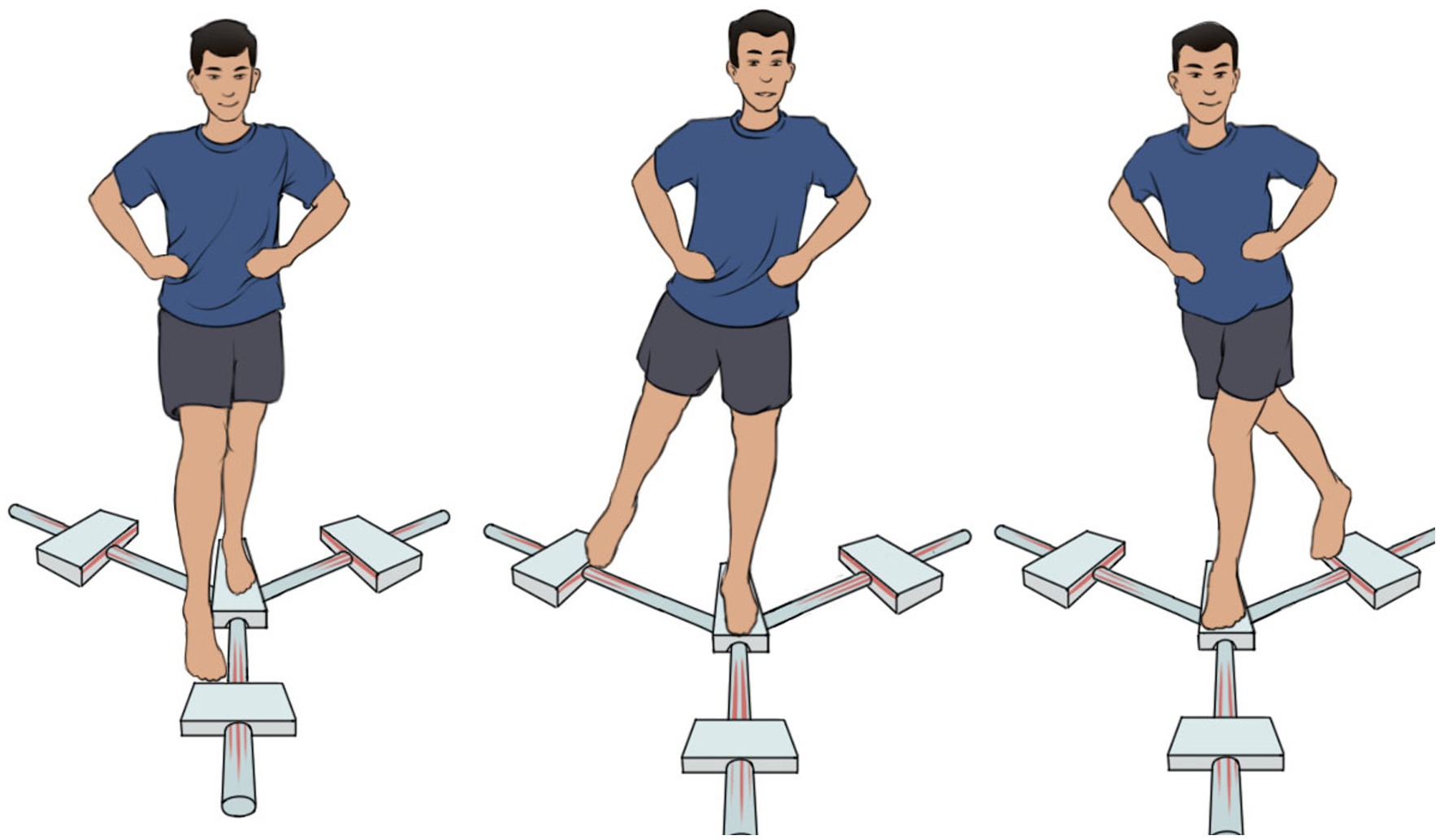
Figure 1. The Y balance test in the anterior (left part), posterolateral (middle part), and posteromedial (right part) reach directions. Here’s an example of the right leg reach.
2.3. Statistical analysis
According to Alshehre et al. (12), a calculation by G*Power software (v3.1) showed that at least 62 participants (31 per group) were required to detect a moderate effect of Y balance test (power = 0.80, α = 0.05) (12). All data were analyzed using the SPSS software (v23.0). The statistical significance level was set at p < 0.05. The Chi-square test was utilized to explore the significant differences in categorical variables between the groups. The Kolmogorov–Smirnov test was used to analyze whether or not the continuous variables were normally distributed. To test the first hypothesis, independent T-tests (for normally distributed variables) and Mann-Whiney U-tests (for non-normally distributed variables) were utilized to explore the balance performance between low and medium to high LBP-related disability groups. To address the second hypothesis, Spearman correlations were applied to describe the relationships between postural balance and its influencing factors.
3. Results
3.1. Participants’ characteristics
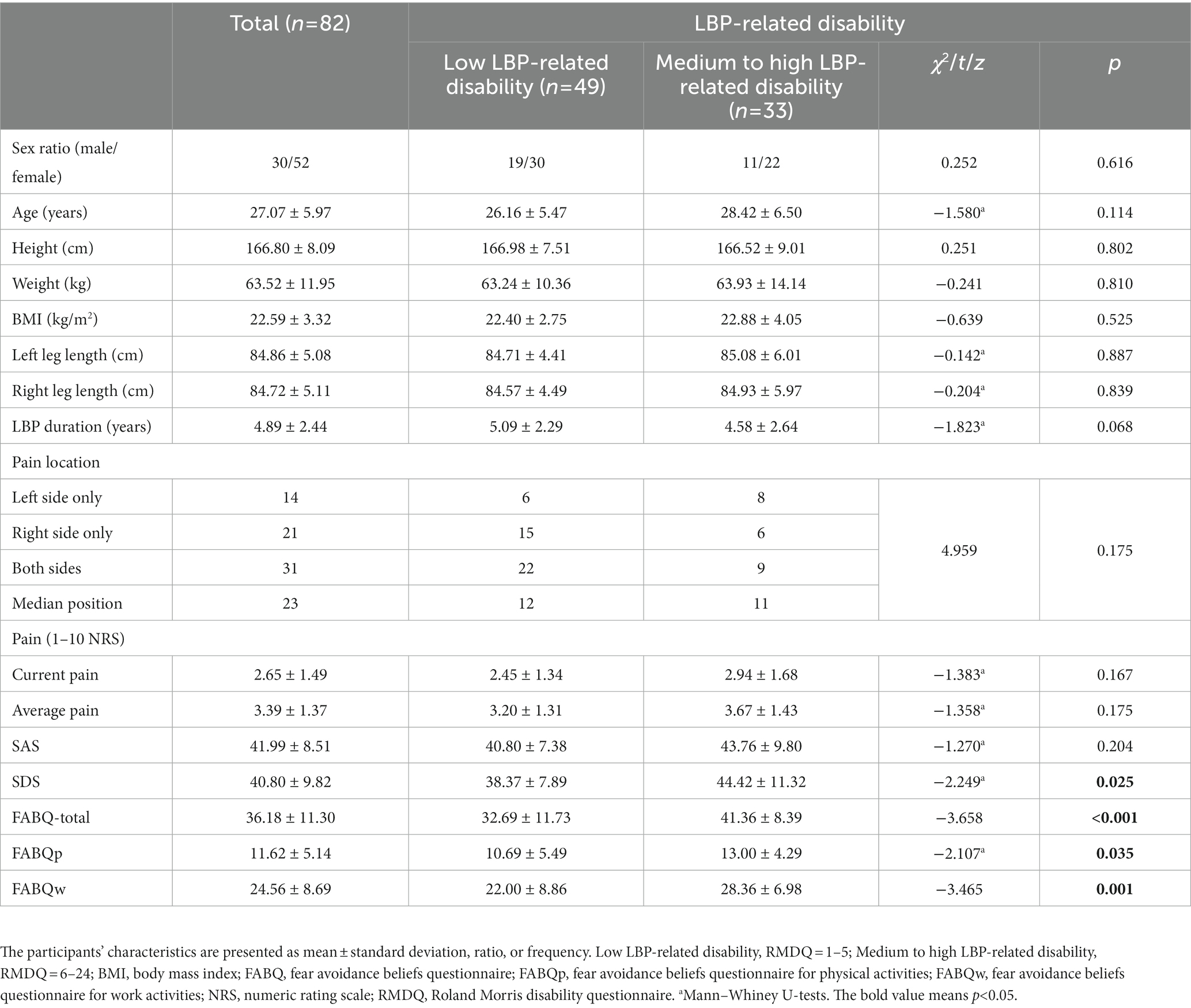
A total of 49 participants with low LBP-related disabilities and 33 participants with medium to high LBP-related disabilities participated in this study. Participants’ characteristics of both groups are summarized in Table 1. The low LBP-related disability group consisted of 19 men and 30 women with a mean age of 26.16 ± 5.47 years, whereas the medium to high LBP-related disability group consisted of 11 men and 22 women with a mean age of 28.42 ± 6.50 years. However, demographic characteristics of age, gender, height, weight, BMI, and LL were not significantly different between groups (p > 0.05). Moreover, no significant clinical differences were observed in LBP duration, pain location, pain intensity, and anxiety between groups (p > 0.05). However, significant differences were found in depression and fear-avoidance levels (including total score, FABQp, and FABQw), which were higher in the medium to high LBP-related disability group (p < 0.05).
3.2. Static balance
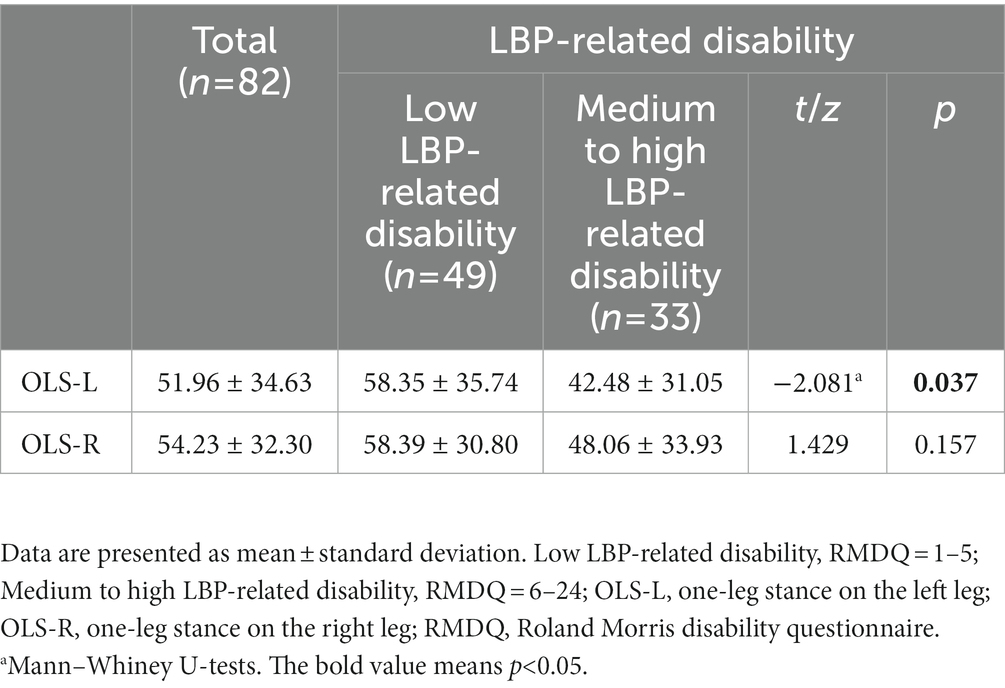
Table 2 displays the OLS scores for both groups. The OLS-L score was significantly higher in the low LBP-related disability group (z = −2.081, p = 0.037), whereas the OLS-R had no significant difference between groups (t = 1.429, p = 0.157).
3.3. Dynamic balance
Table 3 presents the YBT scores for both groups. No significant differences were found in the absolute reaching distances in all directions and composite scores between groups. However, concerning the normalized reach, the low LBP-related disability group had significant scores in PM (p = 0.038) and CS (p = 0.026) of the left leg reach, PM (p = 0.032), PL (p = 0.036), and CS (p = 0.027) of the right leg reach as compared to those of the medium to high LBP-related disability group.
3.4. Correlation analysis
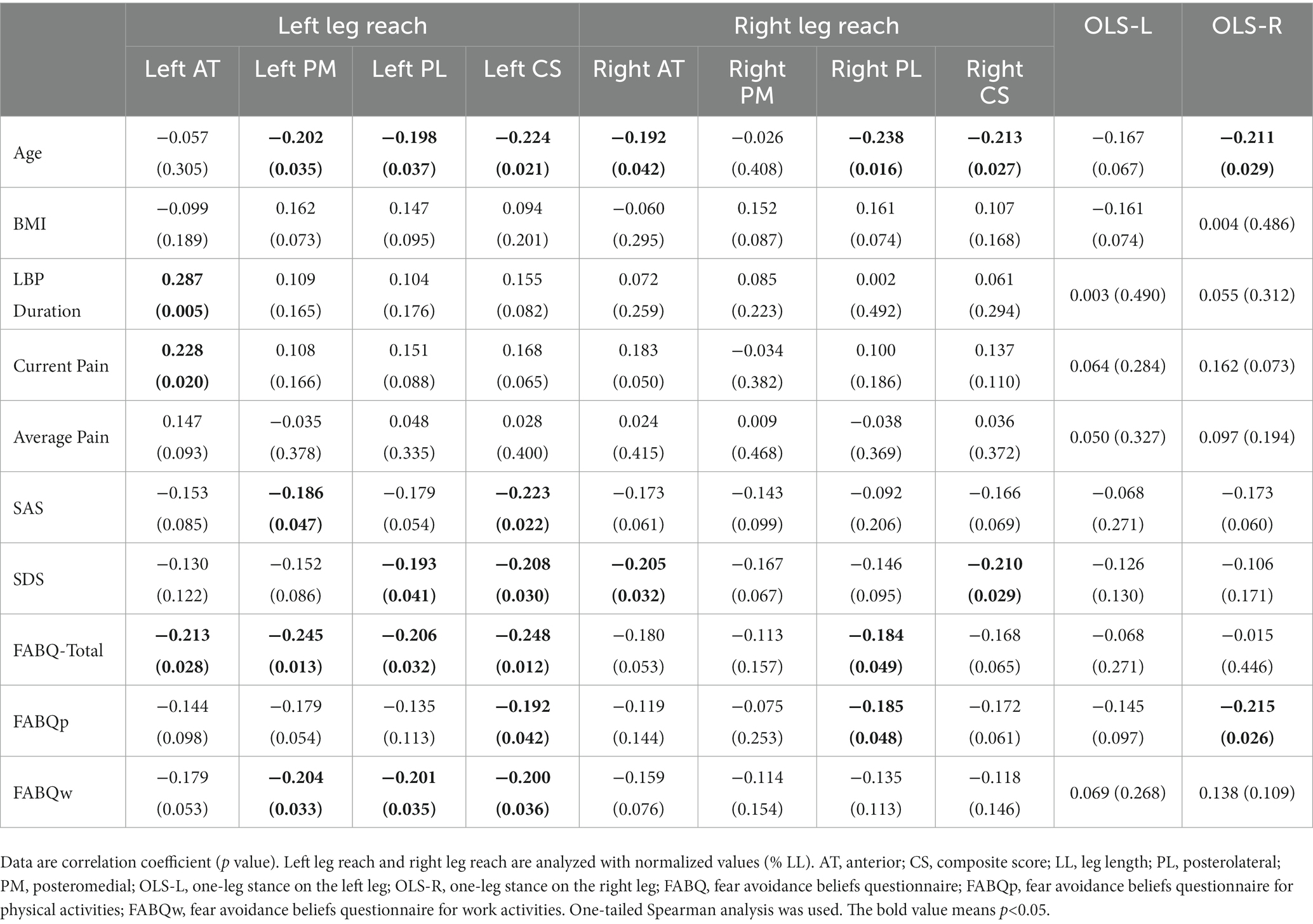
Table 4 shows the relationships between balance and demographic and clinical characteristics. The normalized values of left and right leg reach were selected for analysis. Age was negatively correlated with both legs’ reach in multiple directions and OLS-R score. Duration of LBP was positively correlated with left leg reach in the AT direction (r = 0.287, p = 0.005). As for the pain intensity, current pain is positively related to the left leg reach in the AT direction (r = 0.228, p = 0.020). SAS showed an inverse correlation with left leg reach in the PM direction (r = −0.186, p = 0.047) and CS (r = −0.223, p = 0.022), and SDS was negatively related to left leg reach in the PL direction (r = −0.193, p = 0.041) and CS (r = −0.208, p = 0.030), and right leg reach in the AT direction (r = −0.205, p = 0.032), and CS (r = −0.210, p = 0.029). Moreover, fear-avoidance levels (including total score, FABQp, and FABQw) were negatively correlated with both legs reaching in multiple directions, and FABQp presented an inverse correlation with the OLS-R score (r = −0.215, p = 0.026).
4. Discussion
This study evaluated the associations between disability and postural balance in patients with CLBP. We divided 82 patients into low and medium to high LBP-related disability groups. We found that patients in the low LBP-related disability group performed better in OLS and YBT than the medium to high LBP-related disability group. Factors that influence postural balance, such as age, LBP duration, pain intensity, and negative emotions were also revealed.
4.1. Effects of disability on postural balance
In our study, CLBP patients with medium to high dysfunctions were less likely to maintain their balance in OLS-L as compared to those with low dysfunctions, thereby demonstrating a different outcome to the findings of Tsigkanos et al. (23) which indicates that CLBP participants had worse performance in the OLS-R (23). It could be because of differences in the included subjects. Tsigkanos et al. (23) included patients with a higher mean age and no assessment of dysfunction. Thus, the finding of OLS partially supports the original hypothesis that the more severe the LBP-related disability, the worse the static balance.
Although no significant differences were observed in the absolute values of the YBT reaching distance between groups, the normalized reach distances in PM, PL, and CS were significantly higher in the low LBP-related disability group as compared to the medium to high LBP-related disability group. This may be because highly dysfunctional subjects may be accompanied by functional impairments in other body parts, such as lower limbs. For example, poor balance in the posterior direction predicted ankle sprains (24, 25). The YBT composite score showed that the CLBP participants’ ability to perform multiplanar motion decreased with the increase of the dysfunction (26). However, no differences were observed in the AT direction, which was similar to the findings of Hooper et al. (2016) (21). It may be due to the vision that compensates for any somatosensory and vestibular issues during the reaching in AT direction (21, 27). In PM and PL directions, the lower limbs are placed out of sight behind the body, thereby relying more on somatosensory and vestibular sense to complete the balance tasks. That is, the increase in difficulty may further expose deficiencies in dynamic balance in CLBP patients with higher dysfunction, again supporting our original hypothesis.
Perfect posture balance requires stable nervous system function. Normal nervous functions base on normal anatomical structures such as cerebellum, spinal cord, and peripheral nerves, which are essential for the processing of balance information and the timely and effective balance response. Although this paper cannot provide evidence of neural mechanisms, CLBP has been shown to cause neurological changes, such as cerebellar atrophy, white matter damage, and decreased sensory perception (9). And postural balance is related to functional parameters such as muscle strength, flexibility, muscle control, and proprioception (23). Thus, postural balance impairments in CLBP patients implicate not only abnormal lumbar muscle conditions but also underlying neurological changes leading to neural inefficiency, which can be further investigated by combining neuroimaging techniques such as functional near-infrared spectroscopy.
4.2. Other factors related to postural balance
Our findings of a significant negative correlation between age and performance of YBT and OLS are consistent with previous research (22, 23). Postural balance deteriorates with age possibly caused by biological changes (e.g., neuromusculoskeletal alterations, mobility issues, and sensory-motor deficits) (22, 28). Particularly, impaired postural balance increases the risk of falls in older CLBP patients (29). In addition, BMI is unlikely to affect postural balance, which is consistent with da Silva et al. (2019) (22). Interestingly, LBP duration and current pain intensity were found to be significantly positively correlated with the left leg reaching distance (normalized value) in AT direction. However, Brech et al. (4) found that the lumbar pain intensity and frequency were not correlated with postural balance in women with CLBP (4), which may be because the included participants were younger and their compensatory capacity was high (30). Moreover, we found that the scores of depression and fear avoidance belief (except for anxiety) were higher in the medium to high LBP-related disability group than in the low LBP-related disability group. Moreover, anxiety, depression, and fear avoidance belief were negatively related to YBT performance in multiple directions and only the FABQp score presented a significant inverse correlation with the OLS-R score. Recently, researchers have proposed that negative emotions could affect motor control. For example, anxiety and depression disrupt sensory integration and cognitive interaction (31, 32), requiring greater attention demands to maintain balance. However, although there is a lack of evidence on the effect of pain-related anxiety and depression on postural balance, it is theoretically possible that anxiety and depression could affect postural balance (16). Furthermore, CLBP patients with high fear-avoidance beliefs were not only vigilant but also significantly restricted their range of motion during lumbar flexion and extension (18). Fear may also disrupt the automaticity of neural control pathways, leading to deficits in trunk motor control and increased trunk variability during maintaining balance, which may also increase the risk of LBP (33). Dynamic balance is a more difficult condition than static balance, which makes it easier to reveal the relationship between negative emotions and dynamic balance ability in YBT (34).
4.3. Limitations
However, there are still some limitations despite the findings in this paper. First, we included only young subjects and did not include subjects from other age groups, such as elderly patients with CLBP. And we lack evidence from healthy controls, i.e., healthy young adults with no disabilities. Thus, future studies should study a wider age range of subjects and include healthy controls to enhance the applicability of the findings in this paper. Second, this is a cross-sectional study. Thus, longitudinal research can be further carried out to investigate the effects of LBP-related disability and other factors on postural balance. Furthermore, this paper is limited to behavioral results and lacks neuroimaging evidence, so neuroimaging techniques should be further used to explore the neural mechanism of the effect of LBP-related disability on balance impairments.
5. Conclusion
The greater the dysfunction degree, the worse the CLBP patient’s postural balance. In addition, age, and negative emotions (i.e., anxiety, depression, and fear avoidance belief) could be considered contributing factors for postural balance impairments. Given that postural balance is critical for CLBP patients’ daily living, it should be thoroughly evaluated and integrated into LBP management.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Zhengzhou Central Hospital Affiliated to Zhengzhou University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
PS, KL, XY, ZW, and YY conceptualized this study and contributed to revising and approving the final version of the manuscript. PS and KL contributed to collecting data. Analyzing the data and drafting the manuscript were by PS. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the General Project of Medical Science and Technology Project of Health Department of Henan Province (2018020808).
Acknowledgments
The authors thank all the CLBP patients who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hartvigsen, J, Hancock, MJ, Kongsted, A, Louw, Q, Ferreira, ML, Genevay, S, et al. What low back pain is and why we need to pay attention. Lancet. (2018) 391:2356–67. doi: 10.1016/S0140-6736(18)30480-X
2. Maher, C, Underwood, M, and Buchbinder, R. Non-specific low back pain. Lancet. (2017) 389:736–47. doi: 10.1016/S0140-6736(16)30970-9
3. Andersson, GB. Epidemiological features of chronic low-back pain. Lancet. (1999) 354:581–5. doi: 10.1016/S0140-6736(99)01312-4
4. Brech, GC, Andrusaitis, SF, Vitale, GF, and Greve, JM. Correlation of disability and pain with postural balance among women with chronic low back pain. Clinics. (2012) 67:959–62. doi: 10.6061/clinics/2012(08)17
5. Liu-Ambrose, T, Eng, JJ, Khan, KM, Mallinson, A, Carter, ND, and McKay, HA. The influence of back pain on balance and functional mobility in 65- to 75-year-old women with osteoporosis. Osteopor Int. (2002) 13:868–73. doi: 10.1007/s001980200119
6. Cavanaugh, JT, Guskiewicz, KM, and Stergiou, N. A nonlinear dynamic approach for evaluating postural control: new directions for the management of sport-related cerebral concussion. Sports Med. (2005) 35:935–50. doi: 10.2165/00007256-200535110-00002
7. Alexander, KM, and LaPier, TL. Differences in static balance and weight distribution between normal subjects and subjects with chronic unilateral low back pain. J Orthop Sports Phys Ther. (1998) 28:378–83. doi: 10.2519/jospt.1998.28.6.378
8. Henry, SM, Hitt, JR, Jones, SL, and Bunn, JY. Decreased limits of stability in response to postural perturbations in subjects with low back pain. Clin Biomech. (2006) 21:881–92. doi: 10.1016/j.clinbiomech.2006.04.016
9. Yu, GZ, Ly, M, Karim, HT, Muppidi, N, Aizenstein, HJ, and Ibinson, JW. Accelerated brain aging in chronic low back pain. Brain Res. (2021) 1755:147263. doi: 10.1016/j.brainres.2020.147263
10. Fullam, K, Caulfield, B, Coughlan, GF, and Delahunt, E. Kinematic analysis of selected reach directions of the Star Excursion balance test compared with the Y-balance test. J Sport Rehabil. (2014) 23:27–35. doi: 10.1123/JSR.2012-0114
11. Sell, TC. An examination, correlation, and comparison of static and dynamic measures of postural stability in healthy, physically active adults. Phys Ther Sport. (2012) 13:80–6. doi: 10.1016/j.ptsp.2011.06.006
12. Alshehre, Y, Alkhathami, K, Brizzolara, K, Weber, M, and Wang-Price, S. Reliability and validity of the Y-balance test in young adults with chronic low Back pain. Int J Sports Phys Ther. (2021) 16:628–35. doi: 10.26603/001c.23430
13. da Silva, RA, Vieira, ER, Carvalho, CE, Oliveira, MR, Amorim, CF, and Neto, EN. Age-related differences on low back pain and postural control during one-leg stance: a case-control study. European Spine J. (2016) 25:1251–7. doi: 10.1007/s00586-015-4255-9
14. Mazaheri, M, Coenen, P, Parnianpour, M, Kiers, H, and van Dieën, JH. Low back pain and postural sway during quiet standing with and without sensory manipulation: a systematic review. Gait Posture. (2013) 37:12–22. doi: 10.1016/j.gaitpost.2012.06.013
15. Hodges, P, van den Hoorn, W, Dawson, A, and Cholewicki, J. Changes in the mechanical properties of the trunk in low back pain may be associated with recurrence. J Biomech. (2009) 42:61–6. doi: 10.1016/j.jbiomech.2008.10.001
16. Shanbehzadeh, S, Salavati, M, Talebian, S, Khademi-Kalantari, K, and Tavahomi, M. Attention demands of postural control in non-specific chronic low back pain subjects with low and high pain-related anxiety. Exp Brain Res. (2018) 236:1927–38. doi: 10.1007/s00221-018-5267-6
17. Thomas, JS, France, CR, Sha, D, and Wiele, NV. The influence of pain-related fear on peak muscle activity and force generation during maximal isometric trunk exertions. Spine. (2008) 33:E342–8. doi: 10.1097/BRS.0b013e3181719264
18. Meinke, A, Maschio, C, Meier, ML, Karlen, W, and Swanenburg, J. The association of fear of movement and postural sway in people with low back pain. Front Psychol. (2022) 13:1006034. doi: 10.3389/fpsyg.2022.1006034
19. Kimachi, K, Kimachi, M, Takegami, M, Ono, R, Yamazaki, S, Goto, Y, et al. Level of low back pain-related disability is associated with risk of subsequent falls in an older population: locomotive syndrome and health outcomes in Aizu cohort study (LOHAS). Pain Med. (2019) 20:2377–84. doi: 10.1093/pm/pny313
20. Hlaing, SS, Puntumetakul, R, Wanpen, S, and Boucaut, R. Balance control in patients with subacute non-specific low back pain, with and without lumbar instability: a cross-sectional study. J Pain Res. (2020) 13:795–803. doi: 10.2147/JPR.S232080
21. Hooper, TL, James, CR, Brismée, JM, Rogers, TJ, Gilbert, KK, Browne, KL, et al. Dynamic balance as measured by the Y-balance test is reduced in individuals with low back pain: a cross-sectional comparative study. Phys Ther Sport. (2016) 22:29–34. doi: 10.1016/j.ptsp.2016.04.006
22. da Silva, RA, Vieira, ER, Léonard, G, Beaulieu, LD, Ngomo, S, Nowotny, AH, et al. Age- and low back pain-related differences in trunk muscle activation during one-legged stance balance task. Gait Posture. (2019) 69:25–30. doi: 10.1016/j.gaitpost.2019.01.016
23. Tsigkanos, C, Gaskell, L, Smirniotou, A, and Tsigkanos, G. Static and dynamic balance deficiencies in chronic low back pain. J Back Musculoskelet Rehabil. (2016) 29:887–93. doi: 10.3233/BMR-160721
24. van Lieshout, R, Reijneveld, EA, van den Berg, SM, Haerkens, GM, Koenders, NH, de Leeuw, AJ, et al. Reproducibility of the modified STAR EXCURSION balance test composite and specific reach direction scores. Int J Sports Phys Ther. (2016) 11:356–65.
25. Sung, PS, and Park, MS. Ankle reaction times with tray usage following a slip perturbation between subjects with and without chronic low back pain. Gait Posture. (2022) 97:196–202. doi: 10.1016/j.gaitpost.2022.07.260
26. Wilson, BR, Robertson, KE, Burnham, JM, Yonz, MC, Ireland, ML, and Noehren, B. The relationship between hip strength and the Y balance test. J Sport Rehabil. (2018) 27:445–50. doi: 10.1123/jsr.2016-0187
27. Mergner, T, Schweigart, G, Maurer, C, and Blümle, A. Human postural responses to motion of real and virtual visual environments under different support base conditions. Exp Brain Res. (2005) 167:535–56. doi: 10.1007/s00221-005-0065-3
28. Sakai, Y, Watanabe, T, Wakao, N, Matsui, H, Osada, N, Sugiura, T, et al. Proprioception and geriatric low back pain. Spine Surg Rel Res. (2022) 6:422–32. doi: 10.22603/ssrr.2021-0269
29. Melzer, I, Benjuya, N, and Kaplanski, J. Postural stability in the elderly: a comparison between fallers and non-fallers. Age Ageing. (2004) 33:602–7. doi: 10.1093/ageing/afh218
30. Zwierzchowska, A, Gawel, E, Celebanska, D, and Rosolek, B. Musculoskeletal pain as the effect of internal compensatory mechanisms on structural and functional changes in body build and posture in elite polish sitting volleyball players. BMC Sports Sci Med Rehabil. (2022) 14:49. doi: 10.1186/s13102-022-00439-9
31. Bolmont, B, Gangloff, P, Vouriot, A, and Perrin, PP. Mood states and anxiety influence abilities to maintain balance control in healthy human subjects. Neurosci Lett. (2002) 329:96–100. doi: 10.1016/S0304-3940(02)00578-5
32. Mingorance, JA, Montoya, P, Vivas Miranda, JG, and Riquelme, I. Differences in postural balance, pain sensitivity and depression between individuals with acute and chronic Back pain. J Clin Med. (2022) 11:2700. doi: 10.3390/jcm11102700
33. Nishi, Y, Shigetoh, H, Fujii, R, Osumi, M, and Morioka, S. Changes in trunk variability and stability of gait in patients with chronic low back pain: impact of laboratory versus daily-living environments. J Pain Res. (2021) 14:1675–86. doi: 10.2147/JPR.S310775
Keywords: functional disability, chronic low back pain, balance, age, emotion
Citation: Sun P, Li K, Yao X, Wu Z and Yang Y (2023) Association between functional disability with postural balance among patients with chronic low back pain. Front. Neurol. 14:1136137. doi: 10.3389/fneur.2023.1136137
Edited by:
Simona Bonavita, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Xin Li, Sun Yat-sen University, ChinaJianjun Sun, Peking University Third Hospital, China
Copyright © 2023 Sun, Li, Yao, Wu and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pingge Sun, eXVmZWlkeDM2OUAxNjMuY29t
 Pingge Sun
Pingge Sun Kunbin Li
Kunbin Li Zhiyuan Wu
Zhiyuan Wu