
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 24 March 2023
Sec. Multiple Sclerosis and Neuroimmunology
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1135392
This article is part of the Research Topic New Cerebrospinal Fluid Research to Uncover Mechanisms Driving Neurological and Psychiatric Diseases - Volume II View all 6 articles
Background: Neurosarcodosis is one of the most frequent differential diagnoses of multiple sclerosis (MS) and requires central nervous system (CNS) biopsy to establish definite diagnosis according to the latest consensus diagnostic criteria. We here analyzed diagnostic values of basic cerebrospinal fluid (CSF) parameters to distinguish neurosarcoidosis from MS without CNS biopsy.
Methods: We retrospectively assessed clinical, radiological and laboratory data of 27 patients with neurosarcoidosis treated at our center and compared following CSF parameters with those of 138 patients with relapsing-remitting MS: CSF white cell count (WCC), CSF/serum albumin quotient (Qalb), intrathecal production of immunoglobulins including oligoclonal bands (OCB), MRZ reaction, defined as a polyspecific intrathecal production of IgG reactive against ≥2 of 3 the viruses measles (M), rubella (R), and zoster (Z) virus, and CSF lactate levels. Additional inflammatory biomarkers in serum and/or CSF such as neopterin, soluble interleukin-2 receptor (sIL-2R) and C-reactive protein (CRP) were assessed.
Results: There was no significant difference in the frequency of CSF pleocytosis, but a CSF WCC > 30/μl was more frequent in patients with neurosarcoidosis. Compared to MS, patients with neurosarcoidosis showed more frequently an increased Qalb and CSF lactate levels as well as increased serum and CSF levels of sIL-2R, but a lower frequency of intrathecal IgG synthesis and positive MRZ reaction. Positive likelihood ratio (PLR) of single CSF parameters indicating neurosarcoidosis was highest, if (a) CSF WCC was >30/μl (PLR 7.2), (b) Qalb was >10 × 10−3 (PLR 66.4), (c) CSF-specific OCB were absent (PLR 11.5), (d) CSF lactate was elevated (PLR 23.0) or (e) sIL-2R was elevated (PLR>8.0). The combination of (a) one of three following basic CSF parameters, i.e., (a.1.) CSF WCC >30/ul, or (a.2.) QAlb >10 × 10−3, or (a.3.) absence of CSF-specific OCB, and (b) absence of positive MRZ reaction showed the best diagnostic accuracy (sensitivity and specificity each >92%; PLR 12.8 and NLR 0.08).
Conclusion: Combined evaluation of basic CSF parameters and MRZ reaction is powerful in differentiating neurosarcoidosis from MS, with moderate to severe pleocytosis and QAlb elevation and absence of intrathecal IgG synthesis as useful rule-in parameters and positive MRZ reaction as a rule-out parameter for neurosarcoidosis.
Sarcoidosis is an inflammatory granulomatous disease, affecting the central nervous system (CNS) in 5–15% of cases, then referred to as neurosarcoidosis. The prevalence of neurosarcoidosis (~3–4/100'000) is much lower than multiple sclerosis (MS), which is by far the most frequent inflammatory CNS disease (190/100'000 in Switzerland, global burden 44/100'000 with prevalence ranging from 4.8/100'000 in Western Pacific countries to 117/100'000 in Americas and 143/100'000 in European countries) and the most frequently evaluated differential diagnosis (1–5). However, neurosarcoidosis is most probably more frequent than other neuroimmunological diseases mimicking MS such as neuromyelitis optica spectrum disorder (NMOSD, prevalence ~1/100'000) or MOG antibody-associated disease (MOGAD, prevalence ~2/100'000) (6–10). While evidence of autoimmune pathomechanisms in sarcoidosis is accumulating, there is yet no consensus about its definition as an autoimmune disease and no clear understanding, if immunologic pathways of systemic sarcoidosis, e.g., pulmonary sarcoidosis, can be translated to neurosarcoidosis (11). A mixture of complex genetic patterns and different environmental exposures appear to contribute to the risk of disease development (12–16). Neurologic involvement is, among several other factors, associated with increased mortality in sarcoidosis, but establishing the diagnosis of neurosarcoidosis remains challenging (11, 17). Due to its diverse clinical phenotypes, differentiating neurosarcoidosis from other inflammatory CNS diseases, e.g., MS, can cause difficulties, but is important for the selection of effective treatment strategies. Furthermore, latest consensus diagnostic criteria stipulate that only CNS biopsy with histopathological evidence can establish the diagnosis of definite neurosarcoidosis (18, 19). However, it would be favorable in the future to develop a reliable combination of cerebrospinal fluid (CSF) parameters, radiological and clinical features that would obviate the need for an invasive biopsy.
Recent studies indicate absence of CSF-specific oligoclonal bands (OCB) as a good CSF marker to distinguish neurosarcoidosis from MS, which is the most frequently evaluated differential diagnosis (20). However, basic CSF diagnostics involving CSF white cell count and profiling, blood CSF barrier function, CSF lactate and serum/CSF glucose ratio appear to help distinguishing both disease entities, and data about positive and negative likelihood ratios (PLR and NLR) of single parameters or the combination thereof to help in diagnosing neurosarcoidosis is scarce. We here extended the analysis of basic CSF parameters in both diseases to the MRZ reaction, which is defined as a polyspecific intrathecal production of IgG reactive against ≥2 of 3 the viruses measles (M), rubella (R), and zoster (Z) virus and which is reported as a highly specific CSF biomarker of MS.
We retrospectively analyzed clinical, radiological and laboratory data from 27 patients with possible (n = 4), probable (n = 19), or definite (n = 4) neurosarcoidosis according to consensus diagnostic criteria (19) for predominant clinical phenotype, MRI, FDG-PET and CT findings, CNS or lymph node biopsy locations (Supplementary Table 1) and, if available, frequency of pathologic inflammatory serum and/or CSF markers (Tables 1, 2). In a second step, basic demographic and CSF data from neurosarcoidosis patients and 138 patients with untreated relapsing-remitting multiple sclerosis (MS) were compared for CSF white cell count (WCC), CSF/serum albumin ratio (QAlb), IgG, IgA and IgM CSF/serum ratios (QIgG, QIgA, QIgM), frequency of intrathecal synthesis of IgG, IgA, and IgM according to Reiber's diagram (21) and their intrathecal fraction (IgGIF, IgAIF, and IgMIF), frequency of CSF-specific OCB, intrathecal production of IgG reactive against measles, rubella and varicella zoster virus (MRZ reaction), CSF lactate levels and CSF/serum glucose ratio. 25/27 (92.6%) neurosarcoidosis patients were untreated at the time of lumbar puncture, 1 patient with possible neursarcoidosis was under treatment with mycophenolate mofetil, 1 patient with definite neurosarcoidosis was under treatment with methotrexate. Informed consent was obtained from all patients. Since data of all patients were anonymized for this study, the local Cantonal Ethics Committee stated that the research project does not fall within the scope of the Human Reseach Act (HRA) and therefore, an authorization from the ethics committee is not required (BASEC Nr. Req-2022-01134).
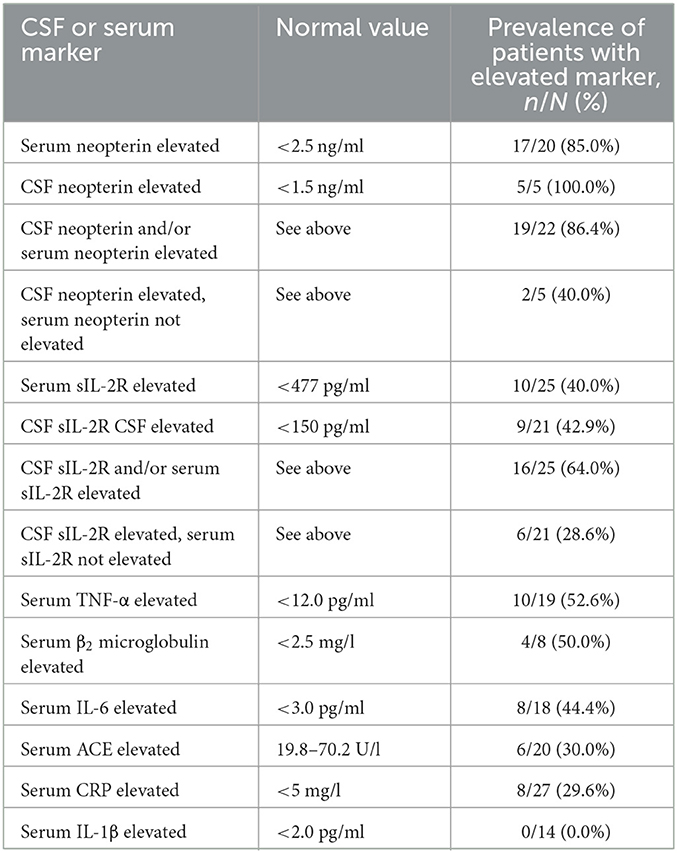
Table 2. Prevalence of pathological inflammatory serum and/or CSF markers in neurosarcoidosis patients.
Neurosarcoidosis patients were screened for data availability of serum neopterin (normal value <2.5 ng/ml, neopterin ELISA kit, IBL International), CSF neopterin [normal value <1.5 ng/ml according to Motta et al. (22)], serum soluble interleukin-2 receptor (sIL2-R, normal value <477 pg/ml, sIL-2R ELISA kit, R&D Biotech), CSF sIL2R [normal value <150 pg/ml according to Petereit et al. (23)], serum tumor necrosis factor alpha (TNF-α, normal value <12.0 pg/ml, TNF-alpha ELISA kit, IBL International), serum β2 microglobulin (normal value <2.5 mg/l, Beta-2 microglobulin Optilite Kit, Binding Site), serum interleukin 6 (IL-6, normal value <3.0 pg/ml, Interleukin-6 ELISA kit, IBL International), serum interleukin-1 beta (IL-1β, normal value <2.0 pg/ml, Interleukin-1beta ELISA kit, IBL international), serum angiotensin-converting enzyme [ACE, normal value 19.8–70.2 U/l according to Lopez-Sublet et al. (24)] and C-reactive peptide [CRP, normal value <5 mg/l according to Eda et al. (25)] and the frequencies of respective pathologic values were captured. Additionally, patients with neurosarcoidosis and MS were compared for prevalence of elevated serum sIL-2R, CSF sIL-2R and serum CRP.
A CSF white cell count >4/μl was classified as “increased,” representing pleocytosis. WCC was further grouped into (i) 0-−4/μl (no pleocytosis), (ii) 5–30/μl (mild pleocytosis) and (iii) >30/μl (moderate pleocytosis) as an assessment of pleocytosis severity. CSF lactate was considered pathologic if outside of range 1.7–2.6 mmol/l. CSF/blood ratio of glucose was calculated, a ratio <0.5 was considered pathologic.
Albumin levels and IgG, IgM and IgG levels in CSF and serum were quantified by immunonephelometry (Atellica NEPH 630 System, Siemens Healthineers, Switzerland) and respective CSF/serum ratios were calculated. Function of the blood-CSF barrier (BCSFB) was assessed using CSF/serum albumin quotient (QAlb), with QAlb = CSF albumin concentration / serum albumin concentration. The upper reference limit of QAlb was calculated as QAlb = [4+(age/15)] × 10−3 according to Reiber et al. (26), with age representing the patient's age in years. Elevated QAlb indicated disturbed BCSFB, with QAlb >10 × 10−3 defined as moderate BCSFB dysfunction and QAlb >20 × 10−3 defined as severe BCSFB disruption.
IgG index was calculated as QIgG/QAlb, with QIgG = CSF IgG concentration / serum IgG concentration. IgG index ≥0.7 indicated intrathecal synthesis of IgG. The relative intrathecal fraction of IgG, IgA, and IgM (IgGIF, IgAIF, and IgMIF) were, respectively calculated according to Reiber (21). IgGIF >0%, IgAIF >0% and/or IgMIF >0% indicated intrathecal synthesis of IgG, IgA, and/or IgM, respectively. OCB were detected by isoelectric focusing (IEF) on agarose gels and immunoblotting using IgG-specific antibodies in a semi-automated approach (Interlab G26, Interlab, Italy). OCB patterns were evaluated according to international consensus criteria (27): OCB pattern type 1 = no OCBs in CSF or Serum; OCB pattern type 2 = CSF-restricted OCBs (intrathecal IgG production); OCB pattern type 3 = identical bands in CSF and serum (i.e., systemic inflammation), and additional CSF-restricted OCBs (i.e., intrathecal IgG production); OCB pattern type 4 = identical OCBs in CSF and serum; and OCB pattern type 5 = monoclonal bands in CSF and serum. Intrathecal IgG synthesis was indicated only by IEF patterns 2 and 3. OCBs were considered CSF-restricted, if ≥2 additional bands were detected in CSF compared to serum.
Measles- (M), rubella- (R) and varicella zoster (Z) virus-specific IgG antibodies were measured in paired CSF and serum samples with commercial ELISA kits and fully automated ELISA processing. Serum (1:404 and 1:2,020 or 1:3,232 dilutions) and CSF (1:2 and 1:10, or 1:8, 1:16, 1:40, 1:80 dilutions) were analyzed using commercial ELISA kits (EI 2610-9601-L G; EI 2590-9601-LG; EI 2650-9601-L G) from Euroimmun AG (Switzerland) and fully automated ELISA processing (Analyzer I, Euroimmun AG, Switzerland).
The virus-specific CSF/serum antibody index (CAIspec) was calculated as previously described by Reiber (21). In short, CAIspec was assessed as CAIspec = Qspec/QIgG (if QLim (IgG) > QIgG), or CAIspec = Qspec/QLim (IgG), if QLim (IgG) < QIgG. The respective parameters were calculated as follows: Qspec = antigen-specific IgGCSF [AU]/antigen-specific IgGserum [AU]; QIgG = total IgGCSF [mg/l]/total IgGserum [mg/l]; QLim (IgG) = 0.93 × ( + 6 × 10−6)0.5 – 1.7 × 10−3; QLim (IgG) refers to the upper discrimination line of the hyperbolic reference range for the blood-derived IgG in CSF as absence of intrathecal IgG synthesis. CAIspec ≥1.5 indicated intrathecal synthesis of virus-specific antibodies. MRZ reaction (MRZR) was interpreted as positive, if polyclonal intrathecal production of antibodies against ≥2 of the 3 antigens measles (M)-, rubella (R)- and varicella zoster (Z) virus lysate, was detectable (28).
Differences in age and disease duration were compared with the Kruskal-Wallis test. Differences in frequency of female gender, pleocytosis, elevated QAlb, intrathecal immunoglobulin synthesis according to Reiber, CSF-specific OCB, elevated CSF lactate, pathologic CSF/serum glucose ratio, elevetad sIL-2R levels in serum or CSF, elevated CRP levels in serum and positive MRZ reaction were compared with Yates's chi-squared test. Differences in mean values of WCC, QAlb, immunoglobulin CSF/serum ratios, IgG index and intrathecal fraction of immunoglobulins were calculated using unpaired t-test. Sensitivity, specificity, positive likelihood ratio (PLR) and negative likelihood ratio (NLR) with 95%-confidence intervals (95%-CI) of single or combined basic CSF/serum parameters were analyzed to assess their value in distinguishing neurosarcoidosis from MS.
First clinical symptoms of neurosarcoidosis patients included optic neuritis (14.8%), sensory and/or motoric dysfunction (22.2%), myelitis (22.2%), extraocular movement impairment (9.1%), gait disturbance (11.1%), cerebellar syndrome (3.7%), vestibular syndrome (9.1%), and meningoencephalitis (11.1%), strongly mimicking MS-like CNS syndromes in 81.5% of cases (Table 1). 19/27 (70.4%) neurosarcoidosis patients had neurological manifestation before detection of systemic sarcoidosis (Table 1). 88.9% of neurosarcoidosis patients showed MRI abnormalities, mostly involving leptomeningeal enhancement (Table 1). Of those patients who received an FDG-PET scan, 93.4% showed sarcoidosis-typical systemic lesions and/or abnormalities (Table 1).
Analysis of inflammatory markers in serum and/or CSF of neurosarcoidosis patients showed elevated levels of neopterin in CSF or serum in 19/22 (86.4%) patients, elevated levels of sIL-2R in CSF or serum (16/25, 64.0%), elevated serum TNF-α (10/19, 52.6%), elevated serum β2 microglobulin (4/8, 50.0%), elevated serum IL-6 (8/18, 44.4%%), elevated serum ACE (6/20, 30.0%) and elevated serum CRP (8/27, 29.6%) in descending order, while no patient showed elevated levels of IL-1β (0/14, 0.0%) (Table 2). Elevated neopterin levels in serum were detected in 17/20 (85.0%) patients, and elevated neopterin levels in CSF in 5/5 (100.0%) patients, of whom 2/5 (40.0%) had only elevated CSF neopterin levels with normal serum neopterin levels. Elevated levels of sIL-2R in serum were detected in 10/25 (40.0%) patients, and elevated levels of sIL-2R in CSF in 9/21 (42.9%), of whom 6/21 (28.6%) had only elevated CSF sIL-2R, but normal sIL-2R levels in serum (Table 2).
Comparison of demographic features (Table 3) showed that patients with neurosarcoidosis (median age 43.5 years, interquartile range [IQR] 40–51.5) were significantly older at time of lumbar puncture than MS patients (median age 32 years, IQR 28-38; p < 0.001) and had a longer disease duration in months from first clinical presentation until lumbar puncture (6.0 months, IQR 0.0–15.8 vs. 0.0, IQR 0.0–2.0; p = 0.013). Furthermore, female sex was more frequent in MS than in neurosarcoidosis (67.4 vs. 44.4%; p = 0.041, Table 3).
There was no significant difference in the frequency of pleocytosis (63.8 vs. 55.6%; p = 0.42) between patients with neurosarcoidosis and patients with MS, but a CSF WCC >30/μl was more frequent in patients with neurosarcoidosis (22.2 vs. 3.6%; p < 0.001) and a CSF WCC >100/μl was present in neurosarcoidosis patients only (7.4 vs. 0.0%; p = 0.001) (Table 4). These findings corroborate previous reports from the current literature, where 31.8–62.7% of patients with definite or probable neurosarcodosis had CSF pleocytosis among studies involving more than 20 patients (Supplementary Table 2) (18, 20, 29, 30).
Elevated QAlb indicating BCSFB dysfunction showed a much stronger association with neurosarcoidosis than with MS (70.4 vs. 26.1%; p < 0.001) (Table 4). This association was even stronger with QAlb >10 × 10−3 (48.1 vs. 0.7%, p < 0.001). A severe elevation of QAlb >20 × 10−3 was again present in neurosarcoidosis patients only (25.9 vs. 0.0%, p < 0.001). This finding matches well with the current literature, which reports increased CSF protein levels as alternative measure of BCSFB dysfunction in 45.5–76.4% (Supplementary Table 2) (18, 20, 29, 30).
Intrathecal synthesis of IgG according to Reiber's diagram was more frequent in MS patients (52.2 vs. 7.7%, p < 0.001), whereas no significant difference in intrathecal synthesis of IgA or IgM, respectively, was detected (Table 4). Neurosarcoidosis patients showed higher values in CSF/serum IgG ratio (9.3 [SD 10.2] vs. 4.5 [SD 2.5], p = 0.024) and IgA ratio (8.9 [13.5%] vs. 1.8 [1.9], p = 0.014), but not IgM ratio (4.1 [9.9] vs. 0.7 [1.1], p = 0.093), than MS patients (Supplementary Table 3). However, these findings should be interpreted in line with the more frequent and more intense BCSFB dysfunction observed in neurosarcoidosis patients, since CSF/serum immunoglobulin ratios are biased by QAlb. Interestingly, if intrathecal synthesis of IgG, IgA or IgM was present, the intensity of production, described as relative intrathecal fraction IgIF according to Reiber (21), did not vary between neurosarcoidosis and MS (Supplementary Table 3). CSF-specific OCB were present in most of the MS patients (94.2%), but also in 33.3% of the neurosarcoidosis patients (p < 0.001) (Table 4). The latter finding is higher than in recent studies [2.9–4.5% in Arun et al. (20) and Kidd (30)], but in line with older studies [27.3–37.0% in Joseph and Scolding (29) and in Zajicek et al. (18)] (Supplementary Table 2).
Furthermore, patients with neurosarcoidosis were significant more likely to show pathological levels of CSF lactate (33.3 vs. 1.4%, p < 0.001) and pathological CSF/serum glucose ratio (26.9 vs. 0%, p < 0.001) (Table 4).
A positive MRZ reaction was present in 33.3% of MS patients, but only in a single patient with neurosarcoidosis (3.7%, p < 0.001) (Table 5). Significant differences in the prevalence of IgG synthesis reactive against measles virus antigens (3.7 vs. 30.4%, p = 0.004), rubella virus antigens (11.1 vs. 39.1%, p = 0.005) and varicella zoster virus antigens (7.4 vs. 50.7%, p < 0.001) were detected between neurosarcoidosis patients and MS patients (Table 5). Not only the single virus-specific antibody reactivity species (measles or rubella or zoster), but also most of the combinations thereof were significantly less frequent in neurosarcoidosis than in MS patients (Supplementary Table 4). The rubella- and zoster-specific CAI values, but not measles-specific CAI values, were significantly lower in neurosarcoidosis patients compared to MS patients (Supplementary Table 5). These results are in line with two previous studies, which reported a positive MRZ reaction in < 1–9.1% of patients (Supplementary Table 6) (31, 32). However, after including single cases reporting MRZ reaction in patients neurosarcoidosis, the overall frequency of positive MRZ reaction was 3/27 (11.1%) (Supplementary Table 6) (28, 33–35).
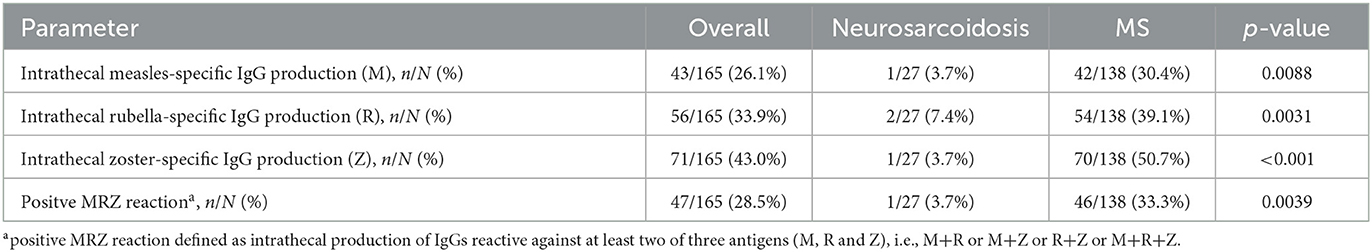
Table 5. Comparison of frequency of MRZ reaction in patients with neurosarcoidosis and patients with MS.
Elevated levels of sIL-2R in serum (40.0 vs. 5.0%, p = 0.007) and CSF (38.1 vs. 0.0%, p = 0.002) as well as elevated serum CRP (25.9 vs. 0.0%, 0.014) showed a strong association with neurosarcoidosis compared to MS (Table 6). Accordingly, serum sIL-2R levels (Figure 1), CSF sIL-2R levels (Figure 2) and serum CRP levels (Figure 3) were significantly higher in neurosarcoidosis than in MS patients.
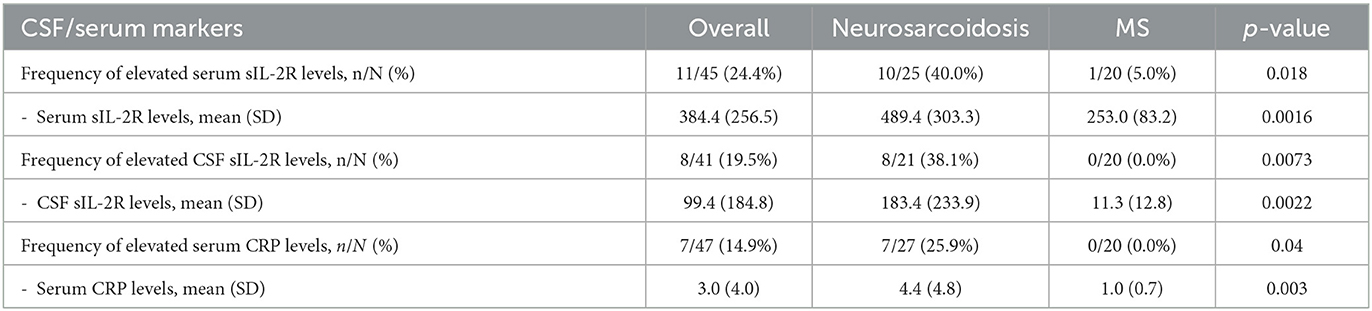
Table 6. Comparison of serum sIL-2R, CSF sIL-2R and serum CRP levels between patients with neurosarcoidosis and patients with MS.
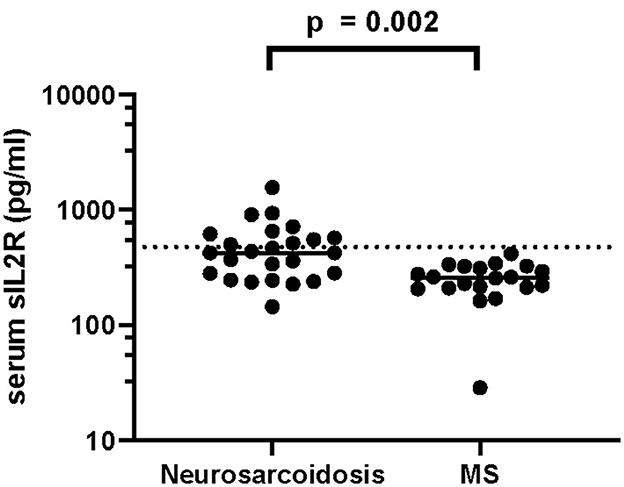
Figure 1. Serum sIL-2R levels in neurosarcoidosis and MS patients. The dashed line represents the cut-off for normal values.
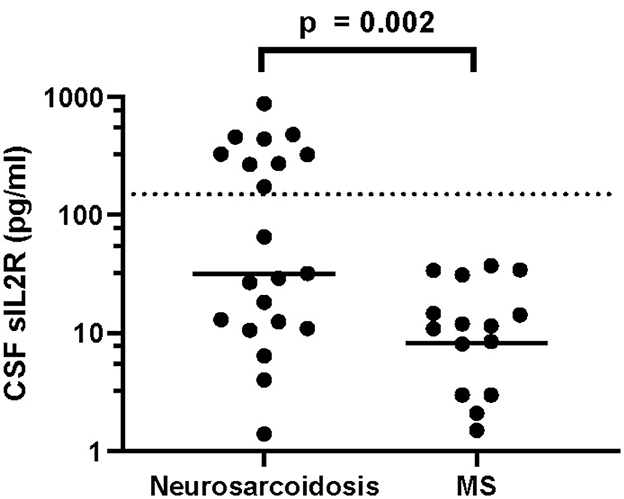
Figure 2. CSF sIL-2R levels in neurosarcoidosis and MS patients. The dashed line represents the cut-off for normal values.
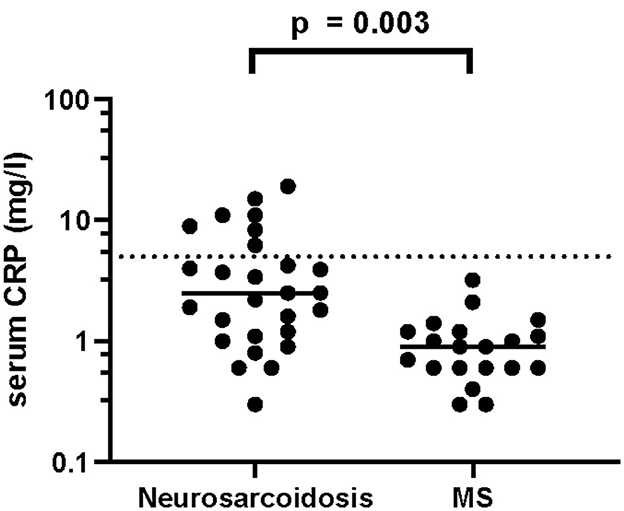
Figure 3. CSF CRP levels in neurosarcoidosis and MS patients. The dashed line represents the cut-off for normal values.
In order to distinguish neurosarcoidosis from MS by laboratory parameters, we further analyzed sensitivities and specificities, as well as positive and negative likelihood ratios (PLR and NLR) of single inflammatory markers and basic CSF parameters (Table 7) and the combinations thereof (Table 8). Diagnostic tests with a PLR of >10 and NLR < 0.1 are generally considered as useful (36, 37), since they are increasing the probability for a defined condition by ~45% (38).
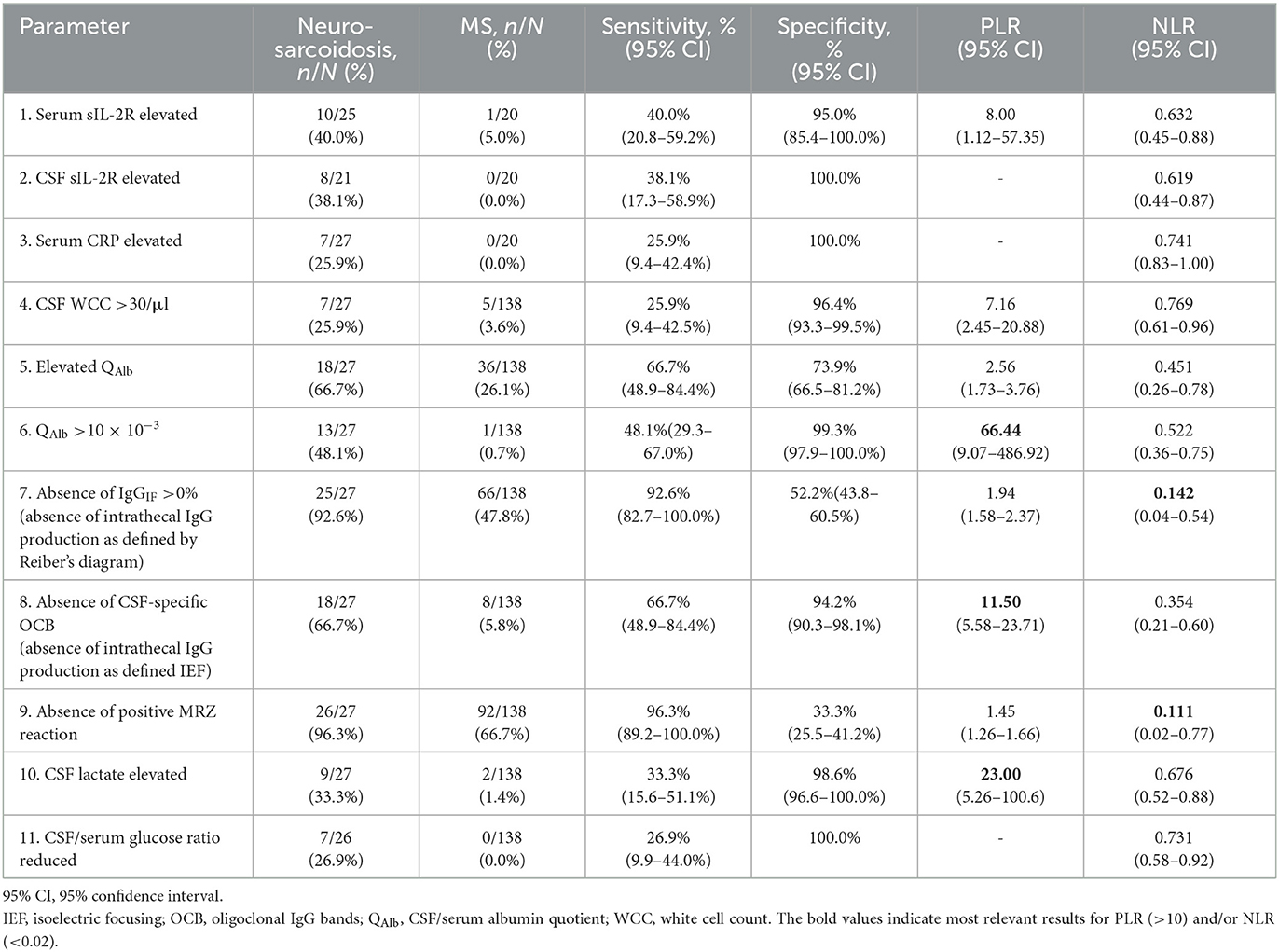
Table 7. Sensitivity, specificity, and likelihood ratios of single inflammatory markers and basic CSF parameters to distinguish neurosarcoidosis from MS.
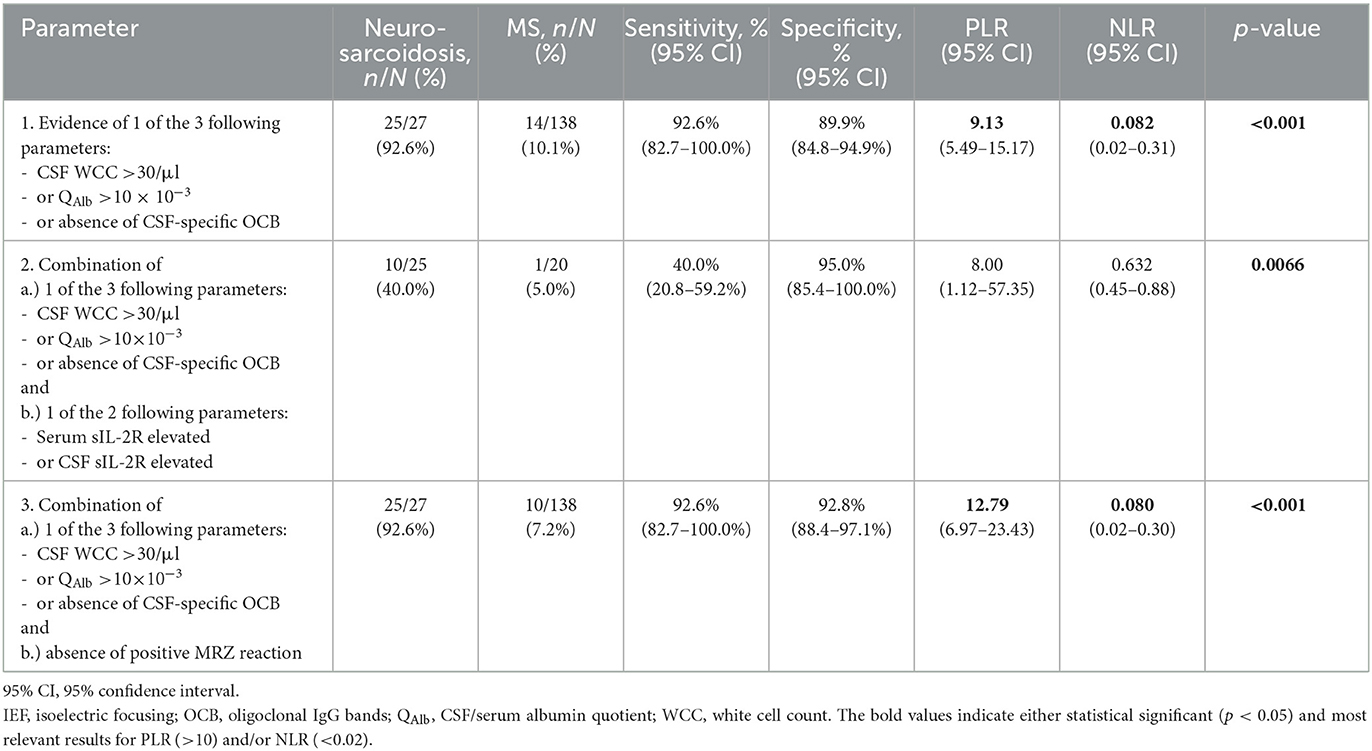
Table 8. Sensitivity, specificity and likelihood ratios of combinations of basic CSF parameters and/or inflammatory markers to distinguish neurosarcoidosis from MS.
Regarding the analysis of single parameters, most inflammatory CSF and serum markers showed high specificity (serum sIL-2R 95.0% [95%-CI 85.4–100.0%], CSF sIL-2R and serum CRP 100.0%), but low sensitivity (serum sIL-2R 40.0% [95%-CI 20.8–59.2%], CSF sIL-2R 38.1% [95%-CI 17.3–58.9%] and serum CRP 25.9% [95%-CI 9.4–42.4%]) and hence high values of respective NLRs (serum sIL-2R 0.63 [0.45–0.88], CSF sIL-2R 0.62 [0.44–0.87] and serum CRP 0.74 [0.83–1.00]) (Table 7). Regarding single basic CSF parameters, highest PLRs were found for QAlb >10 × 10−3 (PLR 66.44 [95%-CI 9.07–486.92]), elevated CSF lactate (PLR 23.00 [95%-CI 5.26-100.6]) and absence of CSF-specific OCB (11.50 [95%-CI 5.58–23.71]) (Table 7). Lowest NLRs were found for absence of positive MRZ reaction (0.11 [95%-CI 0.02–0.77]) and absence of intrathecal IgG synthesis according to Reiber's diagram (0.14 [95%-CI 0.04–0.54]).
In the combined analysis of multiple parameters, the combination of (1) CSF WCC >30/ul, or (2) QAlb >10 × 10−3, or (3) absence of CSF-specific OCB, showed more favorable values for sensitivity (92.6% [95%-CI 82.7–100.0%]), specificity (89.9% [95%-CI 84.8–94.9%]), PLR (9.13 [95%-CI 5.49–15.17]) and NLR (0.082 [95%-CI 0.02–0.31]) to distinguish neurosarcoidosis from MS (Table 8) than the analysis of single parameters (Table 7). When introducing elevated serum or CSF sIL-2R levels as an additional obligatory condition to the latter combination, sensitivity drastically dropped from 92.6% (95%-CI 82.7–100.0%) to 40.0% (95%-CI 20.8–59.2%) and therefore, NLR worsened from 0.082 (95%-CI 0.02–0.31) to 0.63 (95%-CI 0.45–0.88). However, adding absence of positive MRZ reaction (i.e., proof of negative MRZ reaction) as an obligatory condition to the set of basic CSF parameters (i.e., one of the three following parameters fulfilled, (1) CSF WCC >30/ul, or (2) QAlb >10 × 10−3, or (3) absence of CSF-specific OCB) led to an improvement in specificity from 89.9 to 92.8% (95%-CI 88.4–97.1%), in PLR from 9.13 to 12.79 (95%-CI 6.97–23.43) and in NLR from 0.082 to 0.080 (95%-CI 0.02–0.30) while high sensitivity of 92.6% (95%-CI 82.7–100.0) was preserved, marking the best available result regarding diagnostic accuracy in differentiating neurosarcoidosis from MS by CSF analysis.
This retrospective single-center study demonstrates the value of analyzing basic CSF parameters and MRZ reaction to differentiate neurosarcoidosis from MS, which is most commonly considered as a differential diagnosis in routine clinical practice. We show that a CSF WCC >30/μl, QAlb >10 × 10−3 and/or absence of CSF-specific OCB together with absence of positive MRZ reaction are significantly more likely to indicate neurosarcoidosis than MS. As neurosarcoidosis is a serious and often devastating disease that requires therapeutic interventions that differ significantly from those for MS patients, it is of great importance to reliably distuingish between these two diseases and to diagnose the respective disease early and correctly.
Early work on neurosarcoidosis reported that it is the most common disease that can closely mimic MS and is initially misdiagnosed as MS (39). In our cohort of patients with neurosarcoidosis, we also found a high frequency of MS-mimicking neurological syndromes, among them most frequently myelitis, optic neuritis, and sensory and/or motor dysfunction. This is partially in contrast to other reports which find higher frequencies of non-MS mimicking syndromes such as cranial neuropathy in 23–73% (with facial nerve paralysis being the most common) and headache or meningitis in 8–40% (11, 18, 20, 29, 40–47).
According to current literature, 38–69% of patients with neurosarcoidosis do not have a diagnosis of concomitant systemic sarcoidosis before the onset of neurologic symptoms or develop the neurological manifestations as the presenting syndrome of sarcoidosis (17, 20, 46), and 1–20% are reported to have isolated neurosarcoidosis, i.e., without identifiable signs of sarcoid manifestation in other organs (20, 44–51), making the diagnostic situation and differentiation from MS more complicated. The reasons for the large variability in the reported prevalences of neurological symptoms in neurosarcoidosis are probably mainly due to differences in local care and referral between medical specialties and facilities in different countries and centers (11). Another factor could be different fractions of cases with definite, possible, and probable neurosarcoidosis included into the studies and different diagnostic criteria used for inclusion or exclusion of patients. Most recent larger studies report data including 13–25% of reported cases having definite neurosarcoidosis, 59–86% with probable and 15–25% with possible neurosarcoidosis according to Zajicek et al. (18) criteria or Stern et al. (19) criteria (18, 20, 46, 47, 52). Our data included 15% with definite, 70% with probable and 15% with possible neurosarcoidosis and mirroor this typical distribution across recent studies. In addition, recent data suggest that the frequency of neurosarcoidosis among patients with systemic sarcoidosis may probably be higher (up to 34%) than the historically reported 5–15% (11, 47, 52). This finding could be due to heterogeneous awareness of the clinical spectrum of neurosarcoidosis and/or heterogeneous strategies and efforts to prove or disprove the diagnosis of neurosarcoidosis across centers and among different practitioners.
A very interesting and important observation in the routine clinical care of patients with relapsing or re-activated neurosarcoidosis is that neurological deficits often recur in the same way as in previous episodes of disease, due to re-inflammation of the same CNS structures that were previously affected, e.g., re-activation of the same myelitic lesion (11). In one study, disease recurred in 60% of neurosarcoidosis patients who discontinued immunomodulatory therapy with infliximab in the same neuroanatomic lesion (51). This feature of disease recurrence at the same individual neuroanatomical site is less common in MS, as new lesions in individual patients often occur at a wider range of predilection sites. In addition, concomitant involvement of central and peripheral nervous system is very rare in neurosarcoidosis (47), and each of these two manifestations of neurosarcoidosis is associated to different degrees with simultaneouss affections of other organs by sarcoidosis (47). More intensive systematic assessment of cases within neurosarcoidosis-specified registries will most likely enable to assess clearer data (47).
Regarding radiological findings, our cohort of neurosarcoidosis patients showed MRI abnormalities in 89% of cases, most commonly leptomeningeal enhancement (59%). This again reflects typical frequencies reported in literature (69–83% of cases with MRI changes), with the exception, that leptomeningeal enhancement is reported a slightly less frequent (35–46% with leptomeningeal enhancement) (20, 46, 48, 52). Although MRI findings in neurosarcoidosis are highly variable and both contrast-enhancing and non-enhancing lesions are frequently found across various areas of the central nervous system (18, 19), leptomeningeal enhancement is very rare in MS and useful as a rule-in parameter for neurosarcoidosis (53, 54). The frequency of MS-typical lesions found in neurosarcoidosis patients is reported between 5 and 24% (20, 47, 48, 54).
To add another layer of complexity, there is an open debate in the field about coexistence of MS and sarcoidosis in individual patients (54–56). A study analyzing a large epidemiological database found that patients with systemic sarcoidosis have a three times higher risk to additionally acquire the diagnosis of MS during the disease course (57). In one large MS center, retrospective chart review of all neurosarcoidosis patients revealed, that 8/50 cases had been diagnosed with definite or probable MS many years before the diagnosis was changed to neurosarcoidosis because of newly evolving, biopsy-proven systemic sarcoidosis (39). In this study, the misdiagnosis rate of MS instead of true neurosarcoidosis was estimated to be ~1 per 500 (0.2%) patients per decade (39). In contrast, another single-center study described 2/80 patients misdiagnosed with neurosarcoidosis before diagnosis was changed to MS in one case and necrotizing vasculitis in the other case, respectively, as proven by postmortem studies (20). The prevalence of cases with coexistent MS and sarcoidosis stands and falls with the degree of certainty, with which both diseases have been diagnosed. An important starting point would be the identification and documentation of cases with unequivocal histopathological confirmation of both MS and sarcoidosis (i.e., by biopsies of CNS as well as extra-CNS tissue) to better estimate such a prevalence. Until now, such histopathologically double proven cases have not been reported (56), and in all patients with systemic sarcoidosis who underwent brain biopsy for suspected CNS demyelinating disease and are reported in the literature, histopathological analysis revealed neurosarcoidosis (39, 56, 58). The question, whether neurosarcoidosis and MS may co-exist in an individual case, is even less clear, but seems to be much less likely (54, 55).
There have been only few studies assessing typical CSF profiles in neurosarcoidosis patients. Among studies involving more than 20 patients, 32–63% of cases with neurosarcoidosis had a CSF pleocytosis and 46–76% increased CSF protein levels (18, 20, 29, 30). A recent meta-analysis reported increased CSF WCC in 58% and elevated CSF protein in 63% (46). Our findings (64% with pleocytosis and 70.4% with increased QAlb or CSF protein) are in line with these studies. Conflicting results are reported regarding CSF-specific OCB as a sensitive measure of intrathecal production of IgG in neurosarcoidosis. Recent studies document a very low prevalence of CSF-specific OCB of 3–5% (20, 30), whereas older studies report 27–37% of cases to show CSF-specific OCB (18, 29). This variability is even higher (0–63%) in smaller studies involving < 20 patients (59, 60). In our cohort, 33% of neurosarcoidosis patients had CSF-specific OCB. Since the above-mentioned meta-analysis by Fritz et al. (46) found CSF-specific OCB in 42% of cases with neurosarcoidosis, we think, that a prevalence of 30–40% CSF-specific OCB in neurosarcoidosis is more realistic. Reasons for these differences could be the use of different neurosarcoidosis diagnostic criteria or any other selection bias regarding neurosarcoidosis cohorts over the years in the above-mentioned studies, as well as different IEF methods and reagents for the detection of OCB, resulting in different sensitivities.
Our study shows that these single parameters are not helpful to reliably distinguish neurosarcoidosis from MS, since either PLR was <10 or NLR was >0.1. Values of PLR >10 and NLR < 0.1 are usually regarded as useful (36, 37), as they are increasing the probability for a defined condition by nearly 50% (38). So far, all studies reported these individual parameters without likelihood ratios, and the differences in CSF laboratory findings between neurosarcoidosis and MS remained fuzzy (54). However, we found that combinations of basic CSF parameter, i.e., (1) CSF WCC >30/μl, (2) QAlb >10 × 10−3 or (3) absence of CSF-specific OCB, with or without additional parameters such as increased sIL-2R or negative MRZ reaction, yield PLR values near 10 or >10 and NLR values < 10. These sets of conditional combinations are therefore useful to differentiate between neurosarcoidosis and MS.
The MRZ reaction was first described in 1992 by Felgenhauer and Reiber. It is considered positive, if intrathecally produced IgG react against at least 2 out of 3 viral antigens, i.e., measles (M), rubella (R), and varicella zoster (Z) virus lysates. A positive MRZ reaction is found only in 63% of MS patients, but it is linked with a very high specificity for MS (98%) (61). Reports about the prevalence of positive MRZ reaction in neurosarcoidosis is scarce, and summarizing all cases from literature shows a prevalence of 3/27 (11%) (28, 31–35). Only one study included more than 20 cases with neurosarcoidosis and reported a positive MRZ reaction in 2/22 (9%) of cases (32). We found a lower rate of positive MRZ reaction in both neurosarcoidosis (4%) and MS (33%) than reported in the literature. Again, differences in the diagnostic criteria used and differences in the methodology and use of reagents to detect an MRZ reaction could explain these discrepant results. However, we confirm previous reports, that positive MRZ reaction is significantly higher prevalent in MS than in neurosarcoidosis.
We found a low sensitivity of increased sIL-2R levels in CSF and/or serum for neurosarcoidosis (38–40%). Other studies reported increased levels in more than 50% of patients (62). Although MS patients typically have normal CSF and serum levels of sIL-2R, it is not specific for neurosarcoidosis, as patients with neurotuberculosis, CNS lymphoma and bacterial meningitis (23, 62–64). However, we show that interpreting sIL-2R levels in the context of basic CSF parameters improves PLR and NLR values and therefore diagnostic accuracy in distinguishing neurosarcoidosis from MS. Our data show that additional parameters such as CRP in serum and lactate in CSF are also attractive candidates for inclusion in combined laboratory parameter sets to distinguish neurosarcoidosis from MS.
Since CSF neopterin levels were elevated in 5/5 (100%) of our neurosarcoidosis patients, this may be an additional marker of interest to evaluate in the future for specificity and sensitivity analysis as well as PLR and NLR to distinguish neurosarcoidosis from MS. Unfortunately, neopterin values in CSF were only available in 5 neurosarcoidosis patients and in none of our MS patients, so that a representative analysis of sensitivity and specificity for neurosarcoidosis was not possible. Interestingly, an increase in CSF neopterin has so far been described not only in neurosarcoidosis (65–67) but also in a proportion of MS patients (68). As the literature on neopterin in CSF is sparse in both diseases, this marker should first be systematically analyzed in larger cohorts of neurosarcoidosis and MS patients before being included in further testing for specificity and sensitivity analysis.
We have not analyzed CD4/CD8 T cell ratio in CSF, but an increase of CSF CD4/CD8 T cell ratio >5.0 has so far been found in 14–38% neurosarcoidosis patients and has been proposed as cut-off value to favor the diagnosis of neurosarcoidosis (69–72). Chazal et al. (71) reported that with a lower CSF CD4/CD8 T cell ratio cut-off value of 3.9, the sensitivity was 29% and the specificity 100% for neurosarcoidosis (n = 29) vs. MS (n = 12), and the sensitivity was 29% and the specificity 87% when comparing neurosarcoidosis with MS and other neuroinflammatory diseases (n = 29). Nordström et al. (72) reported that in a cohort of 11 neurosarcoidosis patients and 55 patients with other neurological disease including 6 with MS, an elevated CSF CD4/CD8 T cell ratio ≥5 alone was not adequate for diagnosing neurosarcoidosis (positive predictive value 40%, negative predictive value 88%). However, the combination of a CD4/CD8 T cell ratio ≥5 and elevated lymphocyte count in CSF increased the positive predictive value (57%) with a negative predictive value (88%) and a specificity of 95% for neurosarcoidosis (72). We think, that a more systematic analysis of CSF CD4/CD8 T cell ratio is needed in larger cohorts of neurosarcoidosis and MS patients, to sharpen the picture and to clearly determine the best cut-off value and the respective sensitivity, specificity, PLR and NLR for neurosarcoidosis vs. MS.
There is a dearth of data on PLRs and NLRs of diagnostic tests in general (37). Sensitivities and specificities are insufficient parameters to predict, whether a diagnostic test or a combination of diagnostic tests indicates reliably a certain disease. It is important to note, that PLRs and NLRs are considerably influenced by the prevalence of the respective disease and that they should be reported together with sensitivities and specificities including their respective confidence intervals. By reporting all these measures, diagnostic accuracy is more reliably assessed than by analyzing sensitivities and specificities alone (73). In clinical routine, pretest probabilities or even pretest-odds are often not only unavailable, but also neglected by treating medical team. However, the assessment of likelihood ratios of laboratory parameters and their combinations in relation to clinical and radiological parameters will be invaluable in assessing more accurately the probability that a suspected diagnosis is correct than by intuition or experience. Referencing to known likelihood ratios will most likely help to harmonize test interpretation and diagnostic accuracy between different centers.
It will be important to re-assess these CSF measures in other and larger cohorts. However, from the existing literature including this study a certain pattern of basic CSF parameters seems to emerge, which is typical for neurosarcoidosis, i.e., CSF WCC >30/μl, QAlb >10 × 10−3 and/or absence of CSF-specific OCB together with absence of positive MRZ reaction. If these findings are reproducible in larger cohorts, it should be evaluated whether they can be included in the diagnostic criteria for neurosarcoidosis to distinguish neurosarcoidosis from MS, as this is the most commonly considered differential diagnosis. This type of analysis should also be extended to other neuroinflammatory disease to enable more accurate differential diagnosis.
Furthermore, it would be interesting to combine the above discussed typical patterns of CSF laboratory findings with typical radiological findings such as FDG-PET-positive lymphadenopathy for the analysis of specificity and sensitivity as well as positive and negative likelihood ratios, since FDG-PET-positive lymphadenopathy was found with high prevalence, i.e., in 24/27 (88.9%) neurosarcoidosis patients, and stood out as a sensitive marker among extraneuronal manifestations in our patients with neurosarcoidosis. Unfortunately, we did not have a sufficient number of cases with MS and FDG-PET or CT scan in our cohort to enable us to compare this parameter between neurosarcoidosis and MS patients, as this analysis is not part of the routine assessment in clinical practice. We did not find any studies in the literature that systematically reported the prevalence of lymphadenopathy in untreated MS as identified by means of FDG-PET or CT scan. We found only one observational study assessing signs of lymphadenopathy in MS patients by means of ultrasound (74). This study found that the size and sonographic morphology of deep cervical lymph nodes in 22 drug-free MS patients is significantly different as compared to 20 healthy donors.
Limitations of this study are that the analysis was performed retrospectively and on a single-center level, that the overall number of patients with neurosarcoidosis was low, and that the minority of patients analyzed in this study had a histopathologically proven definite neurosarcoidosis. Analyzing the data retrospectively in principle depends on how accurately clinical, radiological, and laboratory findings are documented in the medical records. Strengths of this study are that we provide the community with robust likelihood ratios for combined sets of CSF parameters, which are useful for routine clinical practice.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
BV had a major role in the acquisition of the data, analyzed and interpreted the data, and drafted the manuscript for intellectual content. SN acquired, analyzed and interpreted the data, and revised the manuscript for intellectual content. MH analyzed and interpreted the data and revised the manuscript for intellectual content. MZ acquired and analyzed the data, and revised the manuscript for intellectual content. IJ designed and conceptualized the study, acquired, analyzed and interpreted the data, and drafted the manuscript for intellectual content. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1135392/full#supplementary-material
2. Joseph FG, Scolding NJ. Sarcoidosis of the nervous system. Pract Neurol. (2007) 7:234–44. doi: 10.1136/jnnp.2007.124263
3. Arkema EV, Grunewald J, Kullberg S, Eklund A, Askling J. Sarcoidosis incidence and prevalence: a nationwide register-based assessment in Sweden. Eur Respir J. (2016) 48:1690–9. doi: 10.1183/13993003.00477-2016
4. Blozik E, Rapold R, Eichler K, Reich O. Epidemiology and costs of multiple sclerosis in Switzerland: an analysis of health-care claims data, 2011–2015. Neuropsychiatr Dis Treat. (2017) 13:2737–45. doi: 10.2147/NDT.S143180
5. Walton C, King R, Rechtman L, Kaye W, Leray E, Marrie RA, et al. Rising prevalence of multiple sclerosis worldwide: insights from the Atlas of MS, third edition. Mult Scler. (2020) 26:1816–21. doi: 10.1177/1352458520970841
6. Street D, Halfpenny CA, Galea I. CNS inflammation other than multiple sclerosis: how likely is diagnosis? Neurology. (2014) 82:1187–9. doi: 10.1212/WNL.0000000000000273
7. Papp V, Illes Z, Magyari M, Koch-Henriksen N, Kant M, Pfleger CC, et al. Nationwide prevalence and incidence study of neuromyelitis optica spectrum disorder in Denmark. Neurology. (2018) 91:e2265–75. doi: 10.1212/WNL.0000000000006645
8. Boesen MS, Jensen PEH, Born AP, Magyari M, Nilsson AC, Hoei-Hansen C, et al. Incidence of pediatric neuromyelitis optica spectrum disorder and myelin oligodendrocyte glycoprotein antibody-associated disease in Denmark 2008–2018: a nationwide, population-based cohort study. Mult Scler Relat Disord. (2019) 33:162–7. doi: 10.1016/j.msard.2019.06.002
9. Hor JY, Asgari N, Nakashima I, Broadley SA, Leite MI, Kissani N, et al. Epidemiology of neuromyelitis optica spectrum disorder and its prevalence and incidence worldwide. Front Neurol. (2020) 11:501. doi: 10.3389/fneur.2020.00501
10. O'connell K, Hamilton-Shield A, Woodhall M, Messina S, Mariano R, Waters P, et al. Prevalence and incidence of neuromyelitis optica spectrum disorder, aquaporin-4 antibody-positive NMOSD and MOG antibody-positive disease in Oxfordshire, UK. J Neurol Neurosurg Psychiatry. (2020) 91:1126–8. doi: 10.1136/jnnp-2020-323158
11. Bradshaw MJ, Pawate S, Koth LL, Cho TA, Gelfand JM. Neurosarcoidosis: pathophysiology, diagnosis, and treatment. Neurol Neuroimmunol Neuroinflamm. (2021) 8. doi: 10.1212/NXI.0000000000001084
12. Judson MA, Hirst K, Iyengar SK, Rybicki BA, El-Ghormli L, Baughman RP, et al. Comparison of sarcoidosis phenotypes among affected African-American siblings. Chest. (2006) 130:855–62. doi: 10.1378/chest.130.3.855
13. Fischer A, Schmid B, Ellinghaus D, Nothnagel M, Gaede KI, Schurmann M, et al. A novel sarcoidosis risk locus for Europeans on chromosome 11q13.1. Am J Respir Crit Care Med. (2012) 186:877–885. doi: 10.1164/rccm.201204-0708OC
14. Van Moorsel CH, Christiani DC. Genetic susceptibility to sarcoidosis, a chronic inflammatory disorder. Am J Respir Crit Care Med. (2012) 186:816–8. doi: 10.1164/rccm.201209-1582ED
15. Fingerlin TE, Hamzeh N, Maier LA. Genetics of Sarcoidosis. Clin Chest Med. (2015) 36:569–84. doi: 10.1016/j.ccm.2015.08.002
16. Moller DR, Rybicki BA, Hamzeh NY, Montgomery CG, Chen ES, Drake W, et al. Genetic, immunologic, and environmental basis of sarcoidosis. Ann Am Thorac Soc. (2017) 14:S429–36. doi: 10.1513/AnnalsATS.201707-565OT
17. Ungprasert P, Crowson CS, Matteson EL. Characteristics and long-term outcome of neurosarcoidosis: a population-based study from 1976–2013. Neuroepidemiology. (2017) 48:87–94. doi: 10.1159/000477300
18. Zajicek JP, Scolding NJ, Foster O, Rovaris M, Evanson J, Moseley IF, et al. Central nervous system sarcoidosis-diagnosis and management. QJM. (1999) 92:103–17. doi: 10.1093/qjmed/92.2.103
19. Stern BJ, Royal W, Gelfand JM, Clifford DB, Tavee J, Pawate S, et al. Definition and consensus diagnostic criteria for neurosarcoidosis: from the neurosarcoidosis consortium consensus group. JAMA Neurol. (2018) 75:1546–53. doi: 10.1001/jamaneurol.2018.2295
20. Arun T, Pattison L, Palace J. Distinguishing neurosarcoidosis from multiple sclerosis based on CSF analysis: a retrospective study. Neurology. (2020) 94:e2545–54. doi: 10.1212/WNL.0000000000009491
21. Reiber H. Cerebrospinal fluid–physiology, analysis and interpretation of protein patterns for diagnosis of neurological diseases. Mult Scler. (1998) 4:99–107. doi: 10.1177/135245859800400302
22. Motta I, Allice T, Romito A, Ferrara M, Ecclesia S, Imperiale D, et al. Cerebrospinal fluid viral load and neopterin in HIV-positive patients with undetectable viraemia. Antivir Ther. (2017) 22:539–543. doi: 10.3851/IMP3140
23. Petereit HF, Reske D, Tumani H, Jarius S, Markus Leweke F, Woitalla D, et al. Soluble CSF interleukin 2 receptor as indicator of neurosarcoidosis. J Neurol. (2010) 257:1855–63. doi: 10.1007/s00415-010-5623-3
24. Lopez-Sublet M, Caratti Di Lanzacco L, Danser AHJ, Lambert M, Elourimi G, Persu A, et al. Focus on increased serum angiotensin-converting enzyme level: from granulomatous diseases to genetic mutations. Clin Biochem. (2018) 59:1–8. doi: 10.1016/j.clinbiochem.2018.06.010
25. Eda S, Kaufmann J, Roos W, Pohl S. Development of a new microparticle-enhanced turbidimetric assay for C-reactive protein with superior features in analytical sensitivity and dynamic range. J Clin Lab Anal. (1998) 12:137–44. doi: 10.1002/(SICI)1098-2825(1998)12:3<137::AID-JCLA2>3.0.CO;2-6
26. Reiber H, Otto M, Trendelenburg C, Wormek A. Reporting cerebrospinal fluid data: knowledge base and interpretation software. EJIFCC. (2004) 15:74–81. doi: 10.1515/CCLM.2001.051
27. Andersson M, Alvarez-Cermeno J, Bernardi G, Cogato I, Fredman P, Frederiksen J, et al. Cerebrospinal fluid in the diagnosis of multiple sclerosis: a consensus report. J Neurol Neurosurg Psychiatry. (1994) 57:897–902. doi: 10.1136/jnnp.57.8.897
28. Felgenhauer K, Reiber H. The diagnostic significance of antibody specificity indices in multiple sclerosis and herpes virus induced diseases of the nervous system. Clin Investig. (1992) 70:28–37. doi: 10.1007/BF00422934
29. Joseph FG, Scolding NJ. Neurosarcoidosis: a study of 30 new cases. J Neurol Neurosurg Psychiatry. (2009) 80:297–304. doi: 10.1136/jnnp.2008.151977
30. Kidd DP. Sarcoidosis of the central nervous system: clinical features, imaging, and CSF results. J Neurol. (2018) 265:1906–15. doi: 10.1007/s00415-018-8928-2
31. Reiber H, Ungefehr S, Jacobi C. The intrathecal, polyspecific and oligoclonal immune response in multiple sclerosis. Mult Scler. (1998) 4:111–7. doi: 10.1177/135245859800400304
32. Hottenrott T, Dersch R, Berger B, Rauer S, Eckenweiler M, Huzly D, et al. The intrathecal, polyspecific antiviral immune response in neurosarcoidosis, acute disseminated encephalomyelitis and autoimmune encephalitis compared to multiple sclerosis in a tertiary hospital cohort. Fluids Barriers CNS. (2015) 12:27. doi: 10.1186/s12987-015-0024-8
33. Graef IT, Henze T, Reiber H. [Polyspecific immune reaction in the central nervous system in autoimmune diseases with CNS involvement]. Z Arztl Fortbild (Jena). (1994) 88:587–91.
34. Brecht I, Weissbrich B, Braun J, Toyka KV, Weishaupt A, Buttmann M, et al. Intrathecal, polyspecific antiviral immune response in oligoclonal band negative multiple sclerosis. PLoS ONE. (2012) 7:e40431. doi: 10.1371/journal.pone.0040431
35. Endres D, Frye BC, Schlump A, Kuzior H, Feige B, Nickel K, et al. Sarcoidosis and obsessive-compulsive symptoms. J Neuroimmunol. (2022) 373:577989. doi: 10.1016/j.jneuroim.2022.577989
36. Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ. (2004) 329:168–9. doi: 10.1136/bmj.329.7458.168
37. Fierz W, Bossuyt X. Likelihood ratio approach and clinical interpretation of laboratory tests. Front Immunol. (2021) 12:655262. doi: 10.3389/fimmu.2021.655262
38. Mcgee S. Simplifying likelihood ratios. J Gen Intern Med. (2002) 17:646–9. doi: 10.1046/j.1525-1497.2002.10750.x
39. Scott TF, Yandora K, Kunschner LJ, Schramke C. Neurosarcoidosis mimicry of multiple sclerosis: clinical, laboratory, and imaging characteristics. Neurologist. (2010) 16:386–9. doi: 10.1097/NRL.0b013e3181b287df
40. Wiederholt WC, Siekert RG. Neurological manifestations of sarcoidosis. Neurology. (1965) 15:1147–54. doi: 10.1212/WNL.15.12.1147
41. Delaney P. Neurologic manifestations in sarcoidosis: review of the literature, with a report of 23 cases. Ann Intern Med. (1977) 87:336–45. doi: 10.7326/0003-4819-87-3-336
42. Stern BJ, Krumholz A, Johns C, Scott P, Nissim J. Sarcoidosis and its neurological manifestations. Arch Neurol. (1985) 42:909–17. doi: 10.1001/archneur.1985.04060080095022
43. Oksanen V, Gronhagen-Riska C, Tikanoja S, Somer H, Fyhrquist F. Cerebrospinal fluid lysozyme and beta 2-microglobulin in neurosarcoidosis. J Neurol Sci. (1986) 73:79–87. doi: 10.1016/0022-510X(86)90066-3
44. Chapelon C, Ziza JM, Piette JC, Levy Y, Raguin G, Wechsler B, et al. Neurosarcoidosis: signs, course and treatment in 35 confirmed cases. Medicine. (1990) 69:261–76. doi: 10.1097/00005792-199009000-00001
45. Pawate S, Moses H, Sriram S. Presentations and outcomes of neurosarcoidosis: a study of 54 cases. QJM. (2009) 102:449–60. doi: 10.1093/qjmed/hcp042
46. Fritz D, Van De Beek D, Brouwer MC. Clinical features, treatment and outcome in neurosarcoidosis: systematic review and meta-analysis. BMC Neurol. (2016) 16:220. doi: 10.1186/s12883-016-0741-x
47. Ramos-Casals M, Perez-Alvarez R, Kostov B, Gomez-De-La-Torre R, Feijoo-Masso C, Chara-Cervantes J, et al. Clinical characterization and outcomes of 85 patients with neurosarcoidosis. Sci Rep. (2021) 11:13735. doi: 10.1038/s41598-021-92967-6
48. Smith JK, Matheus MG, Castillo M. Imaging manifestations of neurosarcoidosis. AJR Am J Roentgenol. (2004) 182:289–95. doi: 10.2214/ajr.182.2.1820289
49. Scott TF, Yandora K, Valeri A, Chieffe C, Schramke C. Aggressive therapy for neurosarcoidosis: long-term follow-up of 48 treated patients. Arch Neurol. (2007) 64:691–6. doi: 10.1001/archneur.64.5.691
50. Carlson ML, White JRJr, Espahbodi M, Haynes DS, Driscoll CL, Aksamit AJ, et al. Cranial base manifestations of neurosarcoidosis: a review of 305 patients. Otol Neurotol. (2015) 36:156–66. doi: 10.1097/MAO.0000000000000501
51. Gelfand JM, Bradshaw MJ, Stern BJ, Clifford DB, Wang Y, Cho TA, et al. Infliximab for the treatment of CNS sarcoidosis: a multi-institutional series. Neurology. (2017) 89:2092–100. doi: 10.1212/WNL.0000000000004644
52. Joubert B, Chapelon-Abric C, Biard L, Saadoun D, Demeret S, Dormont D, et al. Association of prognostic factors and immunosuppressive treatment with long-term outcomes in neurosarcoidosis. JAMA Neurol. (2017) 74:1336–44. doi: 10.1001/jamaneurol.2017.2492
53. Wattjes MP, Ciccarelli O, Reich DS, Banwell B, De Stefano N, Enzinger C, et al. MAGNIMS-CMSC-NAIMS consensus recommendations on the use of MRI in patients with multiple sclerosis. Lancet Neurol. (2021) 20:653–70. doi: 10.1016/S1474-4422(21)00095-8
54. Chan F, Riminton DS, Ramanathan S, Reddel SW, Hardy TA. Distinguishing CNS neurosarcoidosis from multiple sclerosis and an approach to “overlap” cases. J Neuroimmunol. (2022) 369:577904. doi: 10.1016/j.jneuroim.2022.577904
55. Tyshkov C, Pawate S, Bradshaw MJ, Kimbrough DJ, Chitnis T, Gelfand JM, et al. Multiple sclerosis and sarcoidosis: a case for coexistence. Neurol Clin Pract. (2019) 9:218–27. doi: 10.1212/CPJ.0000000000000629
56. Scott TF. Neurosarcoidosis mimicry of MS: clues from cases with CNS tissue diagnosis. J Neurol Sci. (2021) 429:117621. doi: 10.1016/j.jns.2021.117621
57. Rajoriya N, Wotton CJ, Yeates DG, Travis SP, Goldacre MJ. Immune-mediated and chronic inflammatory disease in people with sarcoidosis: disease associations in a large UK database. Postgrad Med J. (2009) 85:233–7. doi: 10.1136/pgmj.2008.067769
58. Miller DH, Kendall BE, Barter S, Johnson G, Macmanus DG, Logsdail SJ, et al. Magnetic resonance imaging in central nervous system sarcoidosis. Neurology. (1988) 38:378–83. doi: 10.1212/WNL.38.3.378
59. Borucki SJ, Nguyen BV, Ladoulis CT, Mckendall RR. Cerebrospinal fluid immunoglobulin abnormalities in neurosarcoidosis. Arch Neurol. (1989) 46:270–3. doi: 10.1001/archneur.1989.00520390036012
60. Mclean BN, Mitchell DN, Thompson EJ. Local synthesis of specific IgG in the cerebrospinal fluid of patients with neurosarcoidosis detected by antigen immunoblotting using Kveim material. J Neurol Sci. (1990) 99:165–75. doi: 10.1016/0022-510X(90)90153-E
61. Jarius S, Eichhorn P, Franciotta D, Petereit HF, Akman-Demir G, Wick M, et al. The MRZ reaction as a highly specific marker of multiple sclerosis: re-evaluation and structured review of the literature. J Neurol. (2017) 264:453–66. doi: 10.1007/s00415-016-8360-4
62. Otto C, Wengert O, Unterwalder N, Meisel C, Ruprecht K. Analysis of soluble interleukin-2 receptor as CSF biomarker for neurosarcoidosis. Neurol Neuroimmunol Neuroinflamm. (2020) 7. doi: 10.1212/NXI.0000000000000725
63. Scheibe F, Flick H, Wengert O, Wittschieber D, Bohner G, Ruokonen P, et al. Diagnostic pitfalls: a case of neurosarcoidosis mimicking tuberculous meningitis. J Neurol. (2012) 259:1736–9. doi: 10.1007/s00415-012-6429-2
64. Ikeguchi R, Shimizu Y, Shimizu S, Kitagawa K. CSF and clinical data are useful in differentiating CNS inflammatory demyelinating disease from CNS lymphoma. Mult Scler. (2018) 24:1212–23. doi: 10.1177/1352458517717804
65. Furukawa Y, Nishi K, Kondo T, Tanabe K, Mizuno Y. Significance of CSF total neopterin and biopterin in inflammatory neurological diseases. J Neurol Sci. (1992) 111:65–72. doi: 10.1016/0022-510X(92)90113-Y
66. Uysal P, Durmus S, Sozer V, Gelisgen R, Seyhan EC, Erdenen F, et al. YKL-40, soluble IL-2 receptor, angiotensin converting enzyme and C-reactive protein: comparison of markers of sarcoidosis activity. Biomolecules. (2018) 8. doi: 10.3390/biom8030084
67. Kraaijvanger R, Janssen Bonas M, Vorselaars ADM, Veltkamp M. Biomarkers in the diagnosis and prognosis of sarcoidosis: current use and future prospects. Front Immunol. (2020) 11:1443. doi: 10.3389/fimmu.2020.01443
68. Shaw CE, Dunbar PR, Macaulay HA, Neale TJ. Measurement of immune markers in the serum and cerebrospinal fluid of multiple sclerosis patients during clinical remission. J Neurol. (1995) 242:53–8. doi: 10.1007/BF00887815
69. Stern BJ, Griffin DE, Luke RA, Krumholz A, Johns CJ. Neurosarcoidosis: cerebrospinal fluid lymphocyte subpopulations. Neurology. (1987) 37:878–81. doi: 10.1212/WNL.37.5.878
70. Marangoni S, Argentiero V, Tavolato B. Neurosarcoidosis. Clinical description of 7 cases with a proposal for a new diagnostic strategy. J Neurol. (2006) 253:488–95. doi: 10.1007/s00415-005-0043-5
71. Chazal T, Costopoulos M, Maillart E, Fleury C, Psimaras D, Legendre P, et al. The cerebrospinal fluid CD4/CD8 ratio and interleukin-6 and−10 levels in neurosarcoidosis: a multicenter, pragmatic, comparative study. Eur J Neurol. (2019) 26:1274–80. doi: 10.1111/ene.13975
72. Nordstrom S, Andersson B, Malmestrom C. Cerebrospinal fluid CD4(+) /CD8(+) ratio in diagnosing neurosarcoidosis. Acta Neurol Scand. (2020) 142:480–5. doi: 10.1111/ane.13297
73. Eusebi P. Diagnostic accuracy measures. Cerebrovasc Dis. (2013) 36:267–72. doi: 10.1159/000353863
Keywords: neurosarcoidosis, multiple sclerosis, cerebrospinal fluid, pleocytosis, blood-CSF barrier dysfunction, oligoclonal bands, MRZ reaction
Citation: Vlad B, Neidhart S, Hilty M, Ziegler M and Jelcic I (2023) Differentiating neurosarcoidosis from multiple sclerosis using combined analysis of basic CSF parameters and MRZ reaction. Front. Neurol. 14:1135392. doi: 10.3389/fneur.2023.1135392
Received: 09 January 2023; Accepted: 06 March 2023;
Published: 24 March 2023.
Edited by:
Luisa María Villar, Ramón y Cajal University Hospital, SpainReviewed by:
Mathias Fousse, Saarland University Medical School, GermanyCopyright © 2023 Vlad, Neidhart, Hilty, Ziegler and Jelcic. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ilijas Jelcic, aWxpamFzLmplbGNpY0B1c3ouY2g=
†ORCID: Ilijas Jelcic orcid.org/0000-0003-3090-7319
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.