- 1Department of Pharmacy Practice, University of Connecticut School of Pharmacy, Storrs, CT, United States
- 2Evidence-Based Practice Center, Hartford Hospital, Hartford, CT, United States
- 3Department of Neurology, Sarasota Memorial Hospital, Sarasota, FL, United States
- 4Alexion, AstraZeneca Rare Disease, Boston, MA, United States
- 5Guy's and St. Thomas' Hospitals, King's College London, London, United Kingdom
Objective: To develop a composite score for predicting functional outcome post–intracerebral hemorrhage (ICeH) using proxy measures that can be assessed retrospectively.
Methods: Data from the observational ERICH study were used to derive a composite score (SAVED2) to predict an unfavorable 90-day modified Rankin scale (mRS) score. Independent predictors of unfavorable mRS were identified via multivariable logistic regression and assigned score weights based on effect size. Area under the curve (AUC) was used to measure the score's discriminative ability. External validation was performed in the randomized ATACH-2 trial.
Results: There were 2,449 patients from ERICH with valid mRS data who survived to hospital discharge. Predictors associated with unfavorable 90-day mRS score and their corresponding point values were: age ≥70 years (odds ratio [OR], 3.8; 1-point); prior stroke (OR, 2.8; 1-point); need for ventilation (OR, 2.7; 1-point); extended hospital stay (OR, 2.7; 1-point); and non-home discharge location (OR, 5.3; 2-points). Incidence of unfavorable 90-day mRS increased with higher SAVED2 scores (P < 0.001); AUC in ERICH was 0.82 (95% CI, 0.80–0.84). External validation in ATACH-2 (n = 904) found an AUC of 0.74 (95% CI, 0.70–0.77).
Conclusions: Using data collected at hospital discharge, the SAVED2 score predicted unfavorable mRS in patients with ICeH.
Introduction
Functional outcome following stroke is clinically meaningful and of major relevance to patients. Tools, such as the modified Rankin scale (mRS), have been developed for the accurate assessment of post-stroke functional outcome (1–3). However, functional outcome data are often unavailable or difficult to collect from real-world sources, such as electronic health records and administrative claims databases.
When long-term functional outcome data are not available, surrogate or proxy measures provide alternative methods to assess post-stroke functional outcome. Proxy measures have included discharge destination (4) and home-time calculations (5), both of which strongly correlate with functional outcome measures between 3 and 12 months post-stroke (6). For instance, in a systematic literature review, Costa et al. found that being discharged to a location other than home was associated with an unfavorable mRS score among the 2 studies that assessed this relationship and that increased home-time post-stroke was associated with improved functional outcomes (6). The majority of proxy measure evaluations have been performed in ischemic stroke populations, while proxy measures in hemorrhagic stroke have not been well characterized.
Composite risk models/scores are used to combine various known risk factors and translate them into a more easily interpretable risk assessment of an individual experiencing a particular outcome (7). Here, we sought to develop a composite scoring system to predict post-intracerebral hemorrhage (ICeH) functional outcome using various proxy measures and risk factors that can be assessed retrospectively with ease and accuracy. By developing a score to predict functional outcomes, we hope to support researchers in better characterizing outcomes post-ICeH among large populations where long-term measures of functional status may not be available.
Materials and methods
Study population
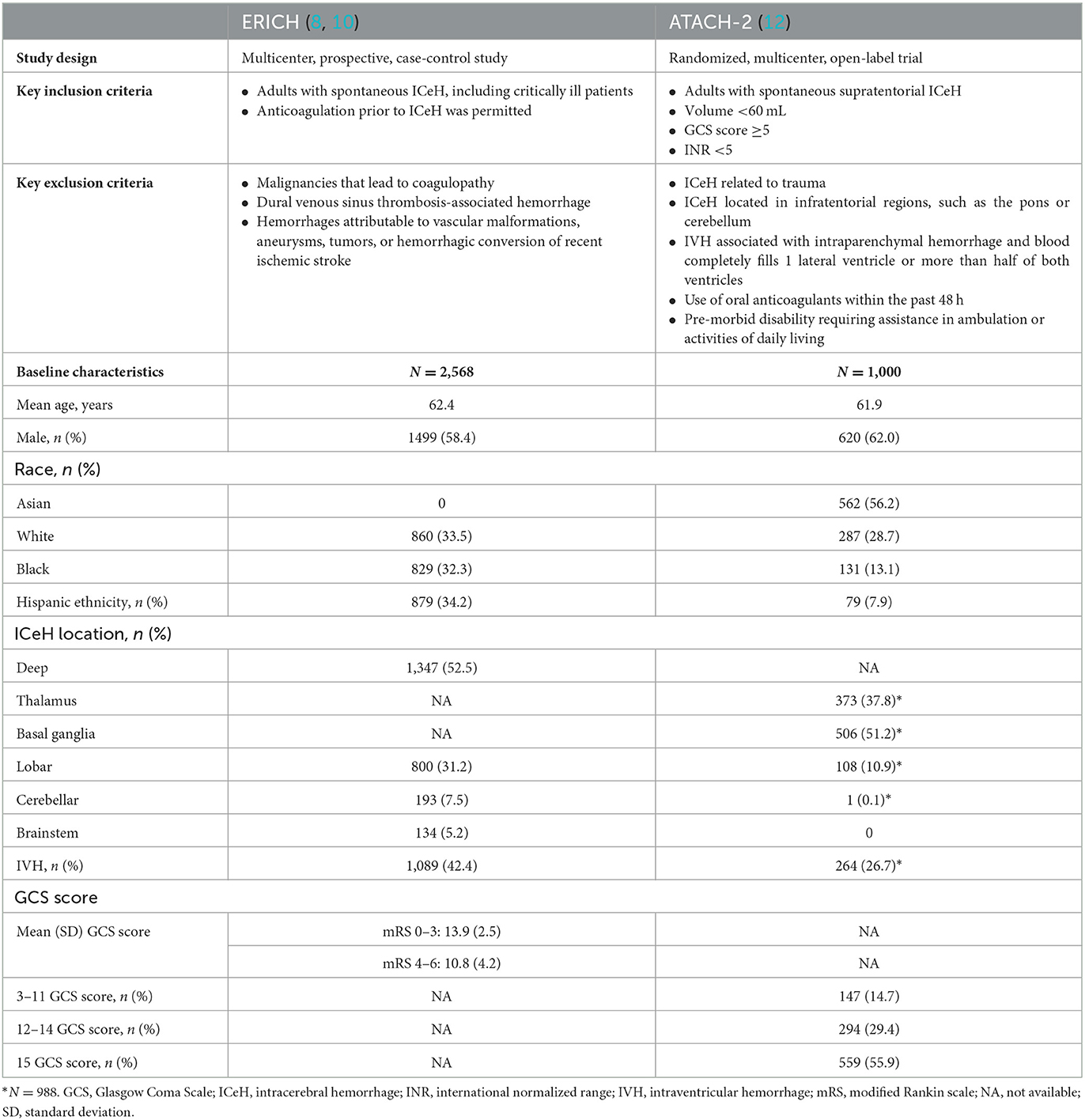
We analyzed individual patient-level data from 2 distinct, prospective clinical studies funded by the National Institute of Neurological Disorders and Stroke (Table 1).
The Ethnic/Racial Variations of Intracerebral Hemorrhage (ERICH) study was a multicenter, prospective, case-control study designed to recruit 1,000 non-Hispanic White, 1,000 non-Hispanic Black, and 1,000 Hispanic patients with spontaneous ICeH to identify risk factors among different races and ethnicities (8). The ERICH study allowed the inclusion of critically ill patients with ICeH, including those with Glasgow Coma Scale (GCS) score < 5, intraventricular bleeding, and infratentorial bleeds (8–10). ERICH also included patients who had received anticoagulation prior to ICeH, and they comprised 13.9% of the White, 7.2% of the Hispanic, and 4.7% of the Black cohorts (11).
The Antihypertensive Treatment of Acute Cerebral Hemorrhage-2 (ATACH-2) multicenter, randomized, open-label trial evaluated the efficacy of early, intensive, antihypertensive intravenous nicardipine treatment in 1,000 patients with spontaneous ICeH (12). The study excluded patients with hemorrhage ≥60 mL, GCS score < 5 at emergency department arrival, infratentorial bleeding (e.g., pons or cerebellum) and intraventricular extension, international normalized range (INR) >1.5, use of dabigatran or other oral anticoagulants, or pre-morbid disability requiring assistance in ambulation or activities of daily living (ADL). The primary outcome was death or disability (mRS score of 4–6, on a scale ranging from 0 [no symptoms] to 6 [death]) at 3 months after randomization. Details of the study design, patient populations, and methods, including those used to determine ICeH location and volume, have been previously described for both the ERICH (8) and ATACH-2 (12) studies.
Both ERICH (8) and ATACH-2 (12) reported mRS score at time points ranging from 1 month to ≥6 months post–hemorrhagic stroke. All patients in ERICH and ATACH-2 were eligible for inclusion in the current study if they survived to discharge and had a total hospital length of stay (LOS) < 90 days. Patients were excluded if discharge destination data, age, mRS score, need for intubation/ventilation, hospital LOS, or prior stroke history were missing or recorded as “unknown.” Attrition diagrams for ERICH and ATACH-2 are shown in Figure 1.
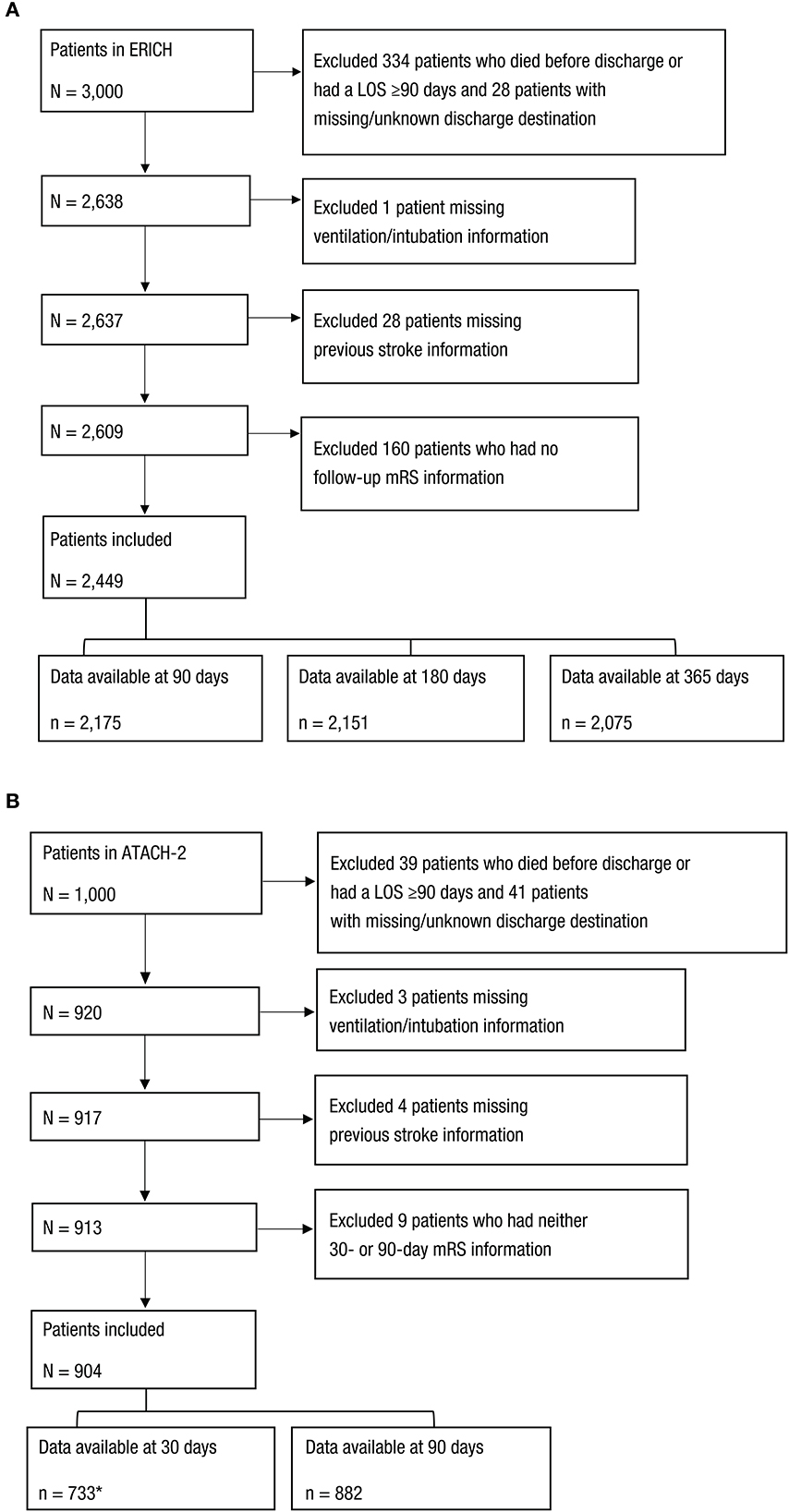
Figure 1. Selection of Patients From the (A) ERICH and (B) ATACH-2 Studies. *Excluded patients with a LOS ≥30 days. LOS, length of stay; mRS, modified Rankin scale.
Outcomes
Based on proxy measures identified in a prior systematic literature review (6) and available ERICH and ATACH-2 data, potential proxy measures of functional status assessed in this study included discharge destination to home (including home healthcare or relative's/friend's home) vs. non-home locations; extended hospital LOS (defined as hospital LOS ≥8 days); and need for endotracheal intubation and ventilation. Functional outcome status was assessed using mRS at 30, 90, and 180 days after ICeH.
Statistical analysis
The association between proxy measures and unfavorable outcome classification (defined as a mRS score of 3–6) was assessed. The discriminative ability (sensitivity, specificity, positive predictive value [PPV], negative predictive value [NPV], and area under the curve [AUC]) of each proxy measure with unfavorable functional outcome was evaluated.
To derive a composite score to predict 90-day mRS score, we used proxy measures available at hospital discharge (i.e., need for intubation/ventilation, extended LOS, and discharge destination) from the ERICH study. Selected proxy measures were augmented with variables—advanced age (≥70 years) and prior stroke history—as they are included in well-known clinical risk prediction tools for patients with ICeH (i.e., the Intracranial Hemorrhage [ICH] and Functional Outcome in Patients With Primary ICeH [FUNC] scores) (13) and they are also available in real-world datasets.
We used multivariable logistic regression to identify independent predictors of unfavorable mRS score. Based on the effect size, score weights were assigned to significant proxies/covariates to create the prior Stroke history per chart history, Age ≥70 years, need for Ventilation, Extended hospital LOS ≥8 days, Discharge to locations other than home (SAVED) score. A simplified score (SAVED2) was also derived by assigning points to each covariate based on the relative weight of each predictor's beta-coefficient to make interpretation easier for clinicians at the bedside. Discriminative ability of SAVED2 was assessed using AUC. Internal validation of the SAVED2 score was performed using data from the ERICH trial and external validation conducted using data from the ATACH-2 trial. All analyses were conducted with IBM SPSS, version 27 (IBM Corp., Armonk, NY).
Results
Derivation population (ERICH cohort)
Of the 3,000 patients with ICeH in the ERICH study, 2,449 patients were included in ≥1 of the analyses at 90, 180, or 365 days (Figure 1A). Of the 2,175 patients who survived to discharge and who had valid mRS data at 90 days after ICeH, 2,151 patients had data available at 180 days and 2,075 patients had data available at 365 days.
Nearly one-third of the patients were aged ≥70 years (30%), the median GCS score was 15 (range, 3–15), and 17% had a prior history of stroke (Table 2). Between 53.4 and 58.1% of patients had an unfavorable mRS score (3–6) at Days 30 through 365. Just over two-thirds of patients (68%) were discharged to a location other than home (Table 2). Using discharge destination as a proxy for unfavorable functional outcome yielded high sensitivity (86%), PPV (range, 67–73%), and NPV (range, 74–76%) at 90, 180, and 365 days (Table 3). More than half of the patients (53%) had an extended hospital LOS (Table 2). Extended LOS was modestly discriminative for predicting unfavorable functional outcome, ranging from 66 to 68% for sensitivity, 60 to 65% for specificity, 66 to 73% for PPV, and 59 to 61% for NPV across the different time points (Table 3). Twenty-eight percent of patients were ventilated/intubated during hospitalization for ICeH (Table 2). Using ventilation/intubation as a proxy for unfavorable functional outcome yielded high specificity (range, 86–87%) and PPV (77–82%), and lower NPV (range, 51–56%) and sensitivity (range, 41–42%) at 90, 180, and 365 days (Table 3).
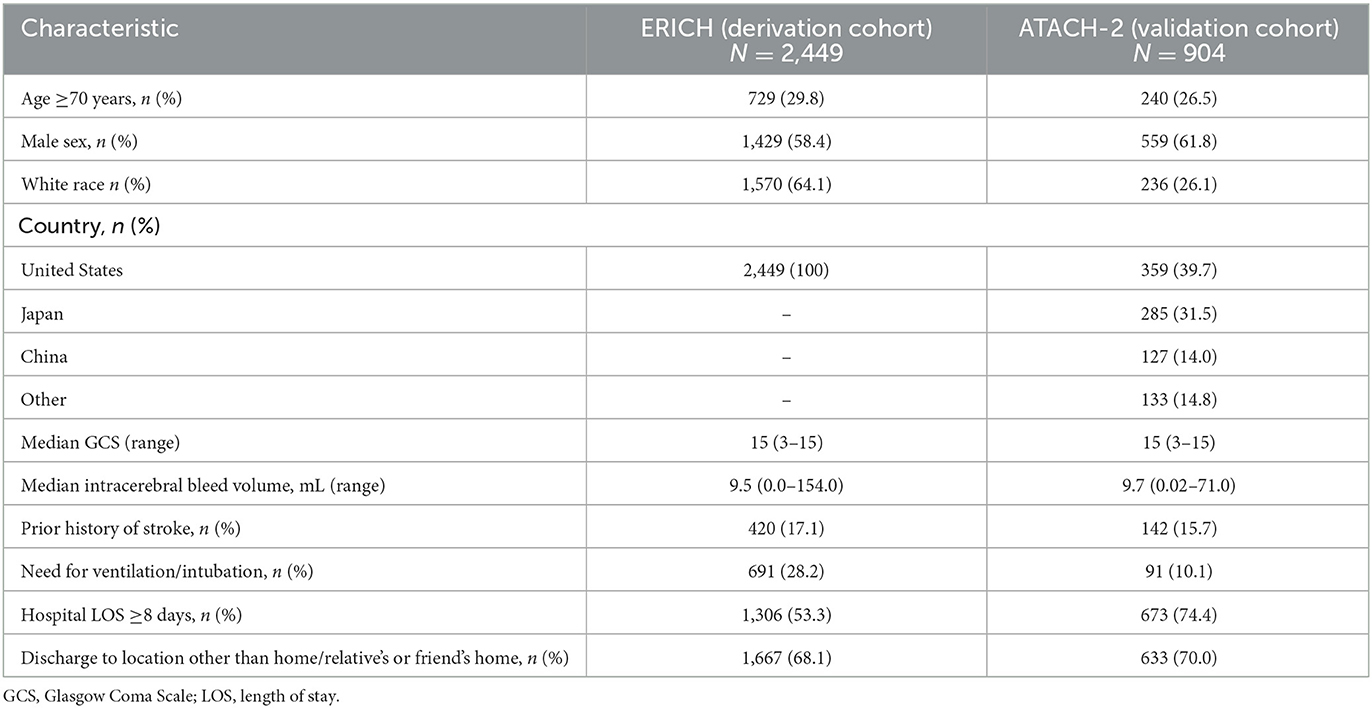
Table 2. Demographics and clinical characteristics of the ERICH and ATACH-2 study populations included in the analysis.
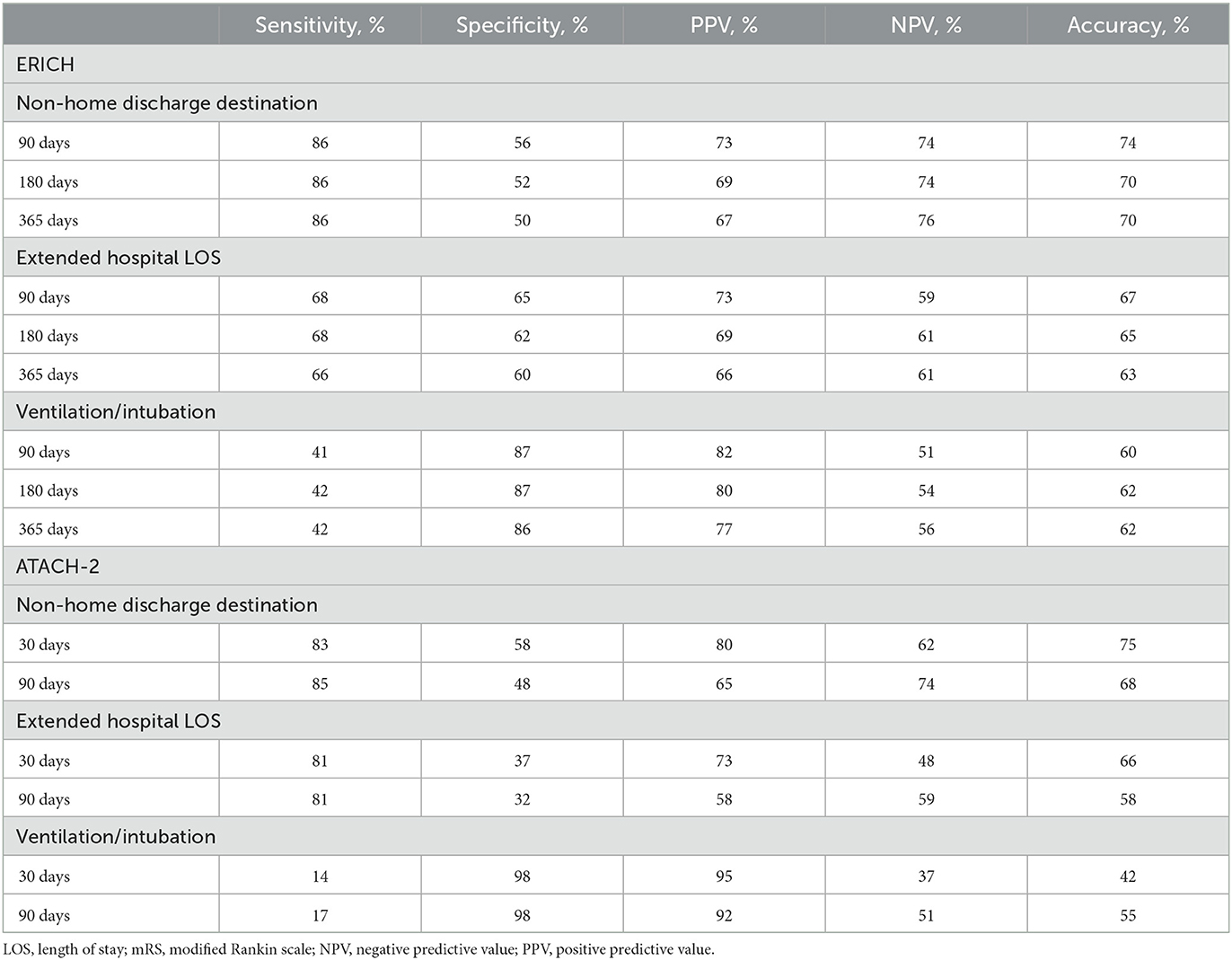
Table 3. Discriminative ability of proxy measures for unfavorable functional outcome (mRS Score 3–6) in ERICH and ATACH-2.
Derivation of SAVED2
To make a tool that clinicians can use at the patient bedside, we next derived a composite risk score to predict unfavorable outcome at 90 days for patients with ICeH who survived to discharge. Utilizing the ERICH population as the training database, we identified characteristics independently associated with unfavorable 90-day mRS score (3–6) and assigned points to each covariate based on the relative weight of each predictor's beta-coefficient using multivariable logistic regression. Among the 2,175 ERICH patients with available data, predictors independently associated with unfavorable 90-day mRS scores and their corresponding point values included: prior stroke history (odds ratio [OR], 2.8; 1 point), age ≥70 years (OR, 3.8; 1 point), need for ventilation (OR, 2.7; 1 point), extended hospital LOS ≥8 days (OR, 2.7; 1 point), and discharge to a location other than home (OR, 5.3; 2 points) (Table 4). The use of anticoagulation was also evaluated in the logistic regression model but was not found to be significantly associated with unfavorable mRS score (OR, 1.10; 95% confidence interval [CI], 0.77–1.56), potentially due to low utilization of anticoagulants (< 10%) in the ERICH population.
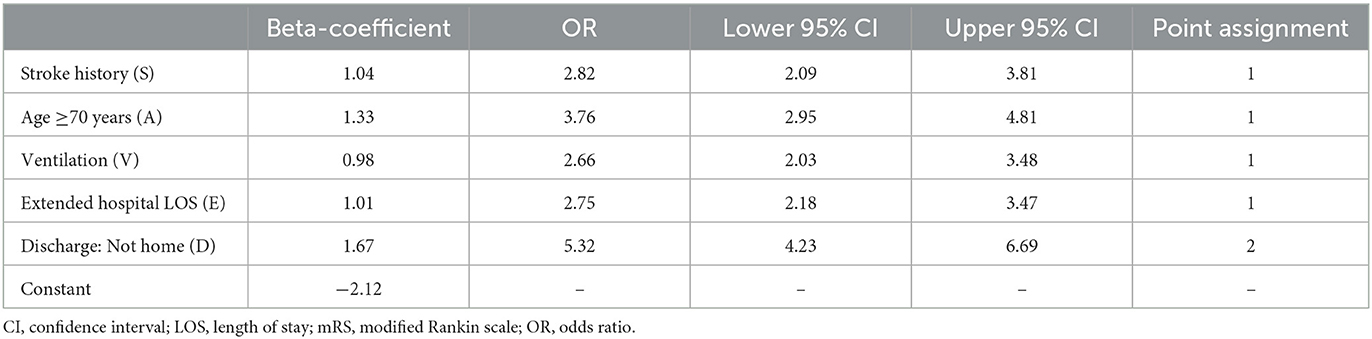
Table 4. Derivation of SAVED2 in ERICH: association of covariates with unfavorable mRS score (3–6) upon multivariable logistic regression and corresponding point assignment in SAVED2.
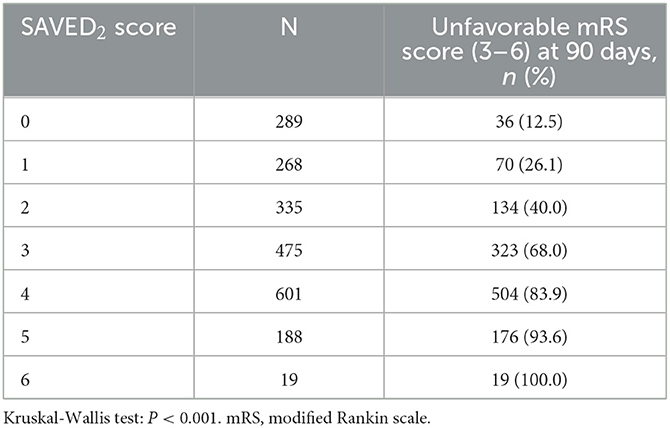
The incidence of unfavorable 90-day mRS scores increased across neighboring and worsening SAVED2 scores (P < 0.001) (Table 5). Unfavorable mRS scores at 90 days were seen in 36 of 289 patients (12.5%) with a SAVED2 score of 0 and in 195 of 207 patients (94.2%) with a SAVED2 score of 5 to 6. In the ERICH cohort, SAVED2 had an excellent ability to discriminate between patients likely to have an unfavorable (3–6) vs. favorable (0–2) mRS score at 90 days (AUC, 0.82; 95% CI, 0.80–0.84; Table 6). A SAVED2 score ≥3 predicted an unfavorable mRS score at 90 days with 81% sensitivity, 71% specificity, 80% PPV, 73% NPV, and 77% overall accuracy.
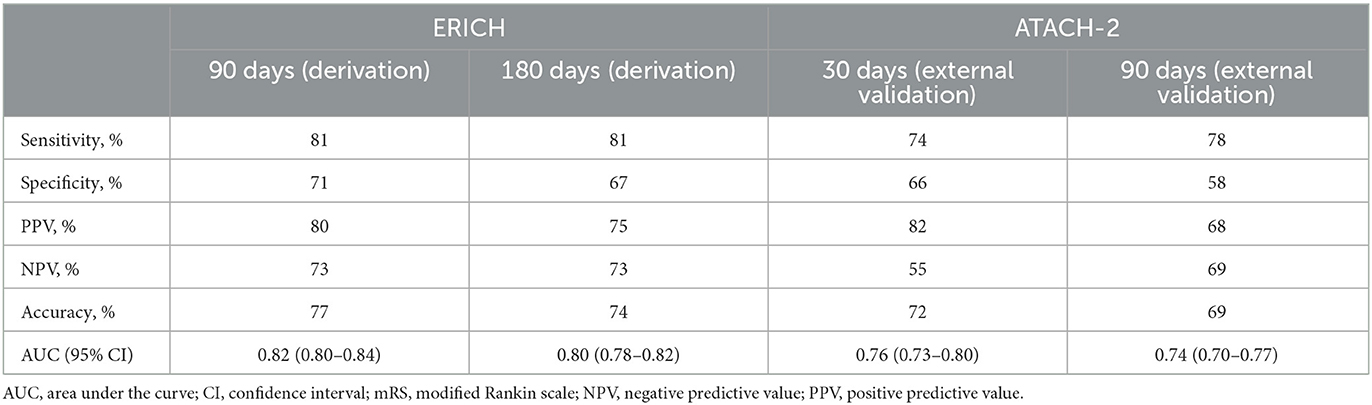
Table 6. Discriminative ability of SAVED2 score ≥3 to predict unfavorable outcome (mRS 3–6) in the ERICH (derivation) and ATACH-2 (external validation) cohorts.
External validation population (ATACH-2 cohort)
Of 1,000 patients with ICeH in ATACH-2, 904 patients were included in this analysis (Figure 1B). There were 733 patients with mRS data available at 30 days and 882 patients with mRS data available at 90 days.
About one-quarter of the patients were aged ≥70 years (27%), the median GCS score was 15 (range, 3–15), and 16% had a prior history of stroke (Table 2). Unfavorable mRS scores of 3 to 6 were seen in 67% of patients at Day 30 and 54% of patients at Day 90. Most patients (70%) were discharged to a location other than home (Table 2). When using non-home discharge destination as a proxy for unfavorable mRS, sensitivity (83 and 85%) and PPV (80 and 65%) were high, and specificity (58 and 48%) was lower at 30 and 90 days, respectively (Table 3). Nearly three-quarters of patients (74.4%) had an extended hospital LOS (Table 2). Using extended LOS as a proxy for unfavorable mRS yielded a high sensitivity (81%) and low specificity (37 and 32%) at 30 and 90 days, respectively (Table 3). Ten percent of patients were ventilated/intubated during the study (Table 2). When using ventilation/intubation as a proxy for unfavorable mRS, specificity (98 and 98%) and PPV (95 and 92%) were high, whereas sensitivity was low (14 and 17%) at 30 and 90 days, respectively (Table 3).
External validation of SAVED2
External validation in 882 eligible patients from ATACH-2 suggested that SAVED2 maintained good discriminative ability at 90 days (AUC, 0.74; 95% CI, 0.70–0.77; Table 6) within a dataset including patients with different baseline characteristics and bleed severity from the derivation dataset. At shorter (30-day) and longer (180-day) follow-up periods of functional outcome assessment, SAVED2 appeared to maintain its discriminative ability as evidenced by AUCs remaining in the clinically useful range, which is defined as ≥0.75 (Table 6).
Discussion
In this study, we identified proxy measures for assessing functional outcomes post-stroke and developed a novel scoring tool to predict 90-day functional outcomes based on data points that can be captured retrospectively. Our analysis confirmed that selected proxy measures, including discharge destination, extended hospital LOS, and need for mechanical ventilation, previously identified in the acute ischemic stroke literature (4, 14–16) may be useful in predicting functional outcome status in patients following ICeH. Discharge destination was highly sensitive but not as specific, whereas the need for mechanical ventilation had high specificity but lower sensitivity, suggesting that a composite measure including several of these proxy measures could create a stronger overall measure that accounts for the limited sensitivity or specificity of any given measure. We demonstrated that the use of these identified proxy measures as part of a composite risk score (SAVED2) had a good-to-excellent ability to discriminate between patients likely to have an unfavorable (3–6) compared to favorable (0–2) mRS score at 90 days.
These findings are important as accurate assessment of post-ICeH functional outcome is essential for both clinical and real-world evidence studies. SAVED2 has the potential to serve as a tool to approximate functional outcome post-ICeH when standard outcome measures, such as mRS, are unavailable. The score could also be used to look at how factors, such as the hospital level, treatment patterns, and personal characteristics, relate to functional outcomes. In a clinical setting, SAVED2 could be used to predict longer-term, 90-day outcomes at the time of hospital discharge.
While SAVED2 appeared to have good discriminative ability at 30 days, there is additional need to confirm whether 1-month mRS score alone can be a dependable and more efficient outcome measure in clinical trials. Additional analysis of ATACH-2 trial data—including evaluation of agreement, weighted kappa, and assessment of utility-weighted mRS at 30- and 90-days after adjustment for potential confounding—could help address this question, as could developing a model to predict 90-day mRS based on 30-day mRS scores and potential covariates included in the SAVED2 components.
This study is the first, to our knowledge, to report on the development and validation of a tool to assess functional outcomes among patients with ICeH using variables that can be assessed retrospectively. Unlike many studies that use split validation or just internal validation, we derived the SAVED2 score using a large, diverse multiethnic cohort and validated it in a separate cohort, strengthening its generalizability to other external cohorts and populations. However, it is possible that differences in the ERICH and ATACH-2 study populations, such as the broader inclusion criteria used in ERICH to include critically ill patients, may have contributed to the slight discrepancy in AUCs observed between the 2 studies. Another limitation of our study is that the data were derived from and validated in populations with spontaneous ICeH and may not be applicable to patients with ischemic stroke or non-ICeH. Although we excluded patients with missing data on any of the key variables, data completion was high for these fields and few patients had missing data. Another limitation is that we derived SAVED2 in the context of patients experiencing spontaneous ICeH in a pre–direct oral anticoagulant (DOAC) era, with fewer than 10% being on oral anticoagulants at the time of the bleed. Also, patients taking anticoagulants were excluded from the ATACH-2 validation cohort. It is unknown how anticoagulant use might impact results, as patients with anticoagulant-related ICeH may experience poorer prognoses compared with patients not on anticoagulants at the time of ICeH (17).
Outcomes for patients with ICeH are very poor. Although it has been decreasing, the mortality burden post-ICeH remains high with a US National Inpatient Sample analysis reporting a 24% inpatient mortality rate (18). Anticoagulant use increases the risk of morbidity and mortality (17). Furthermore, patients who survive the ICeH have a high comorbidity burden. For example, in a German study in 61 patients with DOAC-related ICeH, 28 of 43 survivors (65%) had an unfavorable outcome of mRS 3 to 5, indicating moderate-to-severe disability at 3-month follow-up (19).
Functional outcomes are key for supporting ADL among patients, and we hope that this score can be used to better assess these outcomes among large population-based databases where these data were previously unavailable. To improve outcomes among patients, particularly among those taking anticoagulants, further research is needed to assess the relationship between ICeH and long-term functional outcomes. Utilizing proxy measures such as the SAVED2 composite score may enable real-world studies of the long-term functional status associated with ICeH.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Boards/Ethics Committees at the participating sites. The patients/participants provided their informed consent to participate in those studies.
Author contributions
Contributed to the design, conceptualization of the study, and interpretation of data: CC, MCo, BK, BL, MCh, and AC. Statistical analysis: CC. All authors participated in drafting and revising the manuscript for intellectual content and approved the final manuscript.
Funding
This study was funded by Alexion, AstraZeneca Rare Disease. This post-hoc analysis utilized data from ERICH (NCT01202864), which was funded by the National Institutes of Health (R01NS069763-01) and ATACH-2 (NCT01176565), funded by the National Institutes of Health (U01NS062091; U01NS061861; U01NS059041; U01NS056975) and the Intramural Research Fund for Cardiovascular Diseases of the National Cerebral and Cardiovascular Center, Japan (H23-4-3).
Acknowledgments
We would like to thank Monica Nicosia, PhD, of Lumanity Scientific Inc., who provided writing and editorial assistance, which was funded by Alexion, AstraZeneca Rare Disease.
Conflict of interest
CC has received research funding from Alexion, AstraZeneca Rare Disease, Bayer AG, Global Blood Therapeutics, and Janssen; has received consulting fees from Alexion, AstraZeneca Rare Disease, and Global Blood Therapeutics; and has received honoraria from Medscape. MCo has received consulting fees from Alexion, AstraZeneca Rare Disease; and has received consulting fees from and served on the speakers' bureau for Portola Pharmaceuticals. BK and MCh are employees of Alexion, AstraZeneca Rare Disease. BL is a former employee of Alexion, AstraZeneca Rare Disease. AC has received research funding, consulting fees, and honoraria from Alexion, AstraZeneca Rare Disease, Bayer AG, and Bristol Myers Squibb/Pfizer. The authors declare that this study received funding from Alexion, AstraZeneca Rare Disease. The funder had the following involvement in the study: Bruce Koch, Belinda Lovelace and Mary J. Christoph are/were employees of Alexion, AstraZeneca Rare Disease and served as co-investigators for the study. They were involved in the study design, collection, analysis, interpretation of data, the writing of this article, and/or the decision to submit it for publication.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Duncan PW, Jorgensen HS, Wade DT. Outcome measures in acute stroke trials: a systematic review and some recommendations to improve practice. Stroke. (2000) 31:1429–38. doi: 10.1161/01.STR.31.6.1429
2. Dromerick AW, Edwards DF, Diringer MN. Sensitivity to changes in disability after stroke: a comparison of four scales useful in clinical trials. J Rehabil Res Dev. (2003) 40:1–8. doi: 10.1682/JRRD.2003.01.0001
3. Wilson JT, Hareendran A, Hendry A, Potter J, Bone I, Muir KW. Reliability of the modified Rankin scale across multiple raters: benefits of a structured interview. Stroke. (2005) 36:777–81. doi: 10.1161/01.STR.0000157596.13234.95
4. Qureshi AI, Chaudhry SA, Sapkota BL, Rodriguez GJ, Suri MF. Discharge destination as a surrogate for modified Rankin scale defined outcomes at 3- and 12-months poststroke among stroke survivors. Arch Phys Med Rehabil. (2012) 93:1408–13.e1. doi: 10.1016/j.apmr.2012.02.032
5. Quinn TJ, Dawson J, Lees JS, Chang TP, Walters MR, Lees KR, et al. Time spent at home poststroke: “home-time” a meaningful and robust outcome measure for stroke trials. Stroke. (2008) 39:231–3. doi: 10.1161/STROKEAHA.107.493320
6. Costa OS, Alberts MJ, Christoph MJ, Lovelace B, Rocco J, Coleman CI. Systematic review to identify proxy measures to assess post-stroke functional outcomes. Health Sci Rev. (2022) 5:100057. doi: 10.1016/j.hsr.2022.100057
7. Mechanick JI, Kushner RF. Lifestyle Medicine: A Manual for Clinical Practice. Cham: Springer. (2016). doi: 10.1007/978-3-319-24687-1
8. Woo D, Rosand J, Kidwell C, McCauley JL, Osborne J, Brown MW, et al. The Ethnic/Racial Variations of Intracerebral Hemorrhage (ERICH) study protocol. Stroke. (2013) 44:e120–5. doi: 10.1161/STROKEAHA.113.002332
9. Koch S, Elkind MS, Testai FD, Brown WM, Martini S, Sheth KN, et al. Racial-ethnic disparities in acute blood pressure after intracerebral hemorrhage. Neurology. (2016) 87:786–91. doi: 10.1212/WNL.0000000000002962
10. Woo D, Comeau ME, Venema SU, Anderson CD, Flaherty M, Testai F, et al. Risk factors associated with mortality and neurologic disability after intracerebral hemorrhage in a racially and ethnically diverse cohort. JAMA Netw Open. (2022) 5:e221103. doi: 10.1001/jamanetworkopen.2022.1103
11. Walsh KB, Woo D, Sekar P, Osborne J, Moomaw CJ, Langefeld CD, et al. Untreated hypertension: a powerful risk factor for lobar and nonlobar intracerebral hemorrhage in Whites, Blacks, and Hispanics. Circulation. (2016) 134:1444–52. doi: 10.1161/CIRCULATIONAHA.116.024073
12. Qureshi AI, Palesch YY, Barsan WG, Hanley DF, Hsu CY, Martin RL, et al. Intensive blood-pressure lowering in patients with acute cerebral hemorrhage. N Engl J Med. (2016) 375:1033–43. doi: 10.1056/NEJMoa1603460
13. Garrett JS, Zarghouni M, Layton KF, Graybeal D, Daoud YA. Validation of clinical prediction scores in patients with primary intracerebral hemorrhage. Neurocrit Care. (2013) 19:329–35. doi: 10.1007/s12028-013-9926-y
14. Zhang Q, Yang Y, Saver JL. Discharge destination after acute hospitalization strongly predicts three month disability outcome in ischemic stroke. Restor Neurol Neurosci. (2015) 33:771–5. doi: 10.3233/RNN-150531
15. Alonso A, Ebert AD, Kern R, Rapp S, Hennerici MG, Fatar M. Outcome predictors of acute stroke patients in need of intensive care treatment. Cerebrovasc Dis. (2015) 40:10–7. doi: 10.1159/000430871
16. ElHabr AK, Katz JM, Wang J, Bastani M, Martinez G, Gribko M, et al. Predicting 90-day modified Rankin scale score with discharge information in acute ischaemic stroke patients following treatment. BMJ Neurol Open. (2021) 3:e000177. doi: 10.1136/bmjno-2021-000177
17. Xian Y, Zhang S, Inohara T, Grau-Sepulveda M, Matsouaka RA, Peterson ED, et al. Clinical characteristics and outcomes associated with oral anticoagulant use among patients hospitalized with intracerebral hemorrhage. JAMA Netw Open. (2021) 4:e2037438. doi: 10.1001/jamanetworkopen.2020.37438
18. Javalkar V, Kuybu O, Davis D, Kelley RE. Factors associated with inpatient mortality after intracerebral hemorrhage: updated information from the United States Nationwide Inpatient Sample. J Stroke Cerebrovasc Dis. (2020) 29:104583. doi: 10.1016/j.jstrokecerebrovasdis.2019.104583
Keywords: cerebral hemorrhage, risk prediction, modified Rankin scale score, SAVED2 score, hemorrhagic stroke
Citation: Coleman CI, Concha M, Koch B, Lovelace B, Christoph MJ and Cohen AT (2023) Derivation and validation of a composite scoring system (SAVED2) for prediction of unfavorable modified Rankin scale score following intracerebral hemorrhage. Front. Neurol. 14:1112723. doi: 10.3389/fneur.2023.1112723
Received: 30 November 2022; Accepted: 30 January 2023;
Published: 22 February 2023.
Edited by:
Heling Chu, Shanghai Jiao Tong University, ChinaReviewed by:
Vivek Yedavalli, Johns Hopkins Medicine, United StatesYUkai Liu, Nanjing No. 1 Hospital, China
Copyright © 2023 Coleman, Concha, Koch, Lovelace, Christoph and Cohen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Craig I. Coleman,  Y3JhaWcuY29sZW1hbkBoaGNoZWFsdGgub3Jn
Y3JhaWcuY29sZW1hbkBoaGNoZWFsdGgub3Jn
†Present address: Belinda Lovelace, Health Economics and Outcomes Research, F2G Inc., Princeton, NJ, United States
 Craig I. Coleman
Craig I. Coleman Mauricio Concha3
Mauricio Concha3