
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurol., 14 June 2023
Sec. Neurotrauma
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1110539
 Nathan E. Cook1,2,3*
Nathan E. Cook1,2,3* Charles E. Gaudet1,2,3
Charles E. Gaudet1,2,3 Alicia Kissinger-Knox1,2,3
Alicia Kissinger-Knox1,2,3 Brian C. Liu2,3
Brian C. Liu2,3 Amy A. Hunter4,5
Amy A. Hunter4,5 Marc A. Norman6
Marc A. Norman6 Altaf Saadi7,8
Altaf Saadi7,8 Grant L. Iverson1,2,3,9
Grant L. Iverson1,2,3,9Introduction: This systematic review examined whether race or ethnicity are associated with clinical outcomes (e.g., time to return to school/sports, symptom duration, vestibular deficits, and neurocognitive functioning) following sport-related concussion among child, adolescent, or college-aged student athletes. Additionally, this review assessed whether the existing literature on this topic incorporated or included broader coverage of social determinants of health.
Methods: The online databases PubMed, MEDLINE®, PsycINFO®, CINAHL, Cochrane Library, EMBASE, SPORTDiscus, Scopus, and Web of Science were searched.
Results: A total of 5,118 abstracts were screened and 12 studies met inclusion criteria, including 2,887 youth and young adults. Among the included articles, only 3 studies (25%) examined whether race and ethnicity were associated with outcomes following concussion as a primary objective. None of the studies assessed the association between social determinants of health and outcomes following concussion as a primary objective, although 5 studies (41.7%) addressed a social determinant of health or closely related topic as a secondary objective.
Discussion: Overall, the literature to date is extremely limited and insufficient for drawing conclusions about whether race or ethnicity are categorically associated with outcomes from sport-related concussion, or more specifically, whether there are socioeconomic, structural, or cultural differences or disparities that might be associated with clinical outcome.
Systematic review registration: identifier: PROSPERO, CRD42016041479, CRD42019128300.
Health disparities associated with race and ethnicity are well established (1). A systematic review and technical report from the American Academy of Pediatrics characterized racial and ethnic child health disparities as “extensive, pervasive, and persistent” (2). There is evidence that disparities relating to both physical and mental health persist into college age (3–5). Disparities have been documented across the full spectrum of health and health care, including prevention, access to care, care utilization, and quality of care (2). Within the literature, race and ethnicity are sometimes used interchangeably, and these are not biological constructs. It is recognized that these terms serve as proxies of structural factors like racism, thereby encompassing a large range of social determinants of health. Social determinants of health are non-medical conditions in people's environments that affect their health, including the social constructs of race and ethnicity as well as other factors such as socioeconomic status, education, neighborhood environment, among others.
Racial and ethnic disparities are relevant to the evaluation, treatment, and rehabilitation of children, adolescents, and young adults following sport-related concussion. These disparities have been reported with regard to access and utilization of health care services for concussion (6–8), receipt of academic accommodations following concussion (9), and awareness of concussion signs and symptoms (10). Results from two emergency department (ED) surveillance datasets reporting on ED visits throughout the United States indicated that black youth were less likely to visit the emergency department for a head injury or concussion compared to non-Hispanic white youth (6, 8). Further, among youth presenting to the ED for a sport-related concussion, non-white youth were more likely to leave without being seen by a healthcare provider (11). Disparities have also been reported in terms of specialty care access, such that Hispanic youth were less likely to be seen for subspeciality concussion care, compared to subspecialty care for fractures (7). Following an ED visit for concussion, Hispanic children were significantly less likely to receive academic support compared to children who are not Hispanic (9). Taken together, these studies raise numerous concerns and questions about how social determinants may influence possible differences in access to health care services, service delivery, and in clinical outcomes.
The extent to which there are differences in clinical outcomes following sport-related concussion between individuals of various racial and ethnic identities is not well-understood. Clinical outcomes are diverse, such as the duration of symptoms, severity of neurocognitive deficits, time to return to school without accommodations, and time to return to sports. Identifying factors that are associated with worse, or better, clinical outcome following concussion, and quantifying the magnitude of those effects, is necessary to determine whether or the degree to which social determinants, health history, or injury characteristics should be included in prognostic risk models that could be used to guide medical management, treatment, and rehabilitation of injured student athletes as well as to identify potential foci for system-level change to reduce health disparities. A systematic review examining a broad array of potential factors that may be associated with clinical outcome following concussion was conducted in advance of the Concussion in Sport Group meeting in 2016 held in Berlin (12). This review identified 7 studies that analyzed whether clinical outcomes differed by race or ethnicity. Five of those studies reported null results and two studies reported an association (12). Given that the focus of this prior systematic review was extremely broad (i.e., investigating any potential predictor of concussion outcome and ultimately identifying 21 predictors), no individual potential risk factor was analyzed in depth, including race and ethnicity. Moreover, the literature search for this systematic review was conducted in June 2016 and many additional studies on concussion outcome have been published since that time. Therefore, an updated systematic review focused specifically on whether clinical outcomes (e.g., time to return to school/sports, symptom duration, vestibular deficits, neurocognitive functioning) following sport-related concussion differ in association with race or ethnicity is warranted. The objectives of this systematic review were to (i) determine if race or ethnicity are associated with clinical outcome following sport-related concussion among child, adolescent, or college-aged student athletes; (ii) examine whether the existing literature on this topic incorporates or includes broader coverage of social determinants of health; and (iii) identify knowledge gaps and directions for future research.
Articles were identified through online database searching, hand-searching reference lists (i.e., pearl growing), and performing cited reference searches (see Figure 1). Databases included PubMed, MEDLINE®, PsycINFO®, CINAHL, Cochrane Library, EMBASE, SPORTDiscus, Scopus, and Web of Science. Articles published in English from database inception to May 15, 2021 were included in our searches (Registration: PROSPERO CRD42016041479, CRD42019128300).
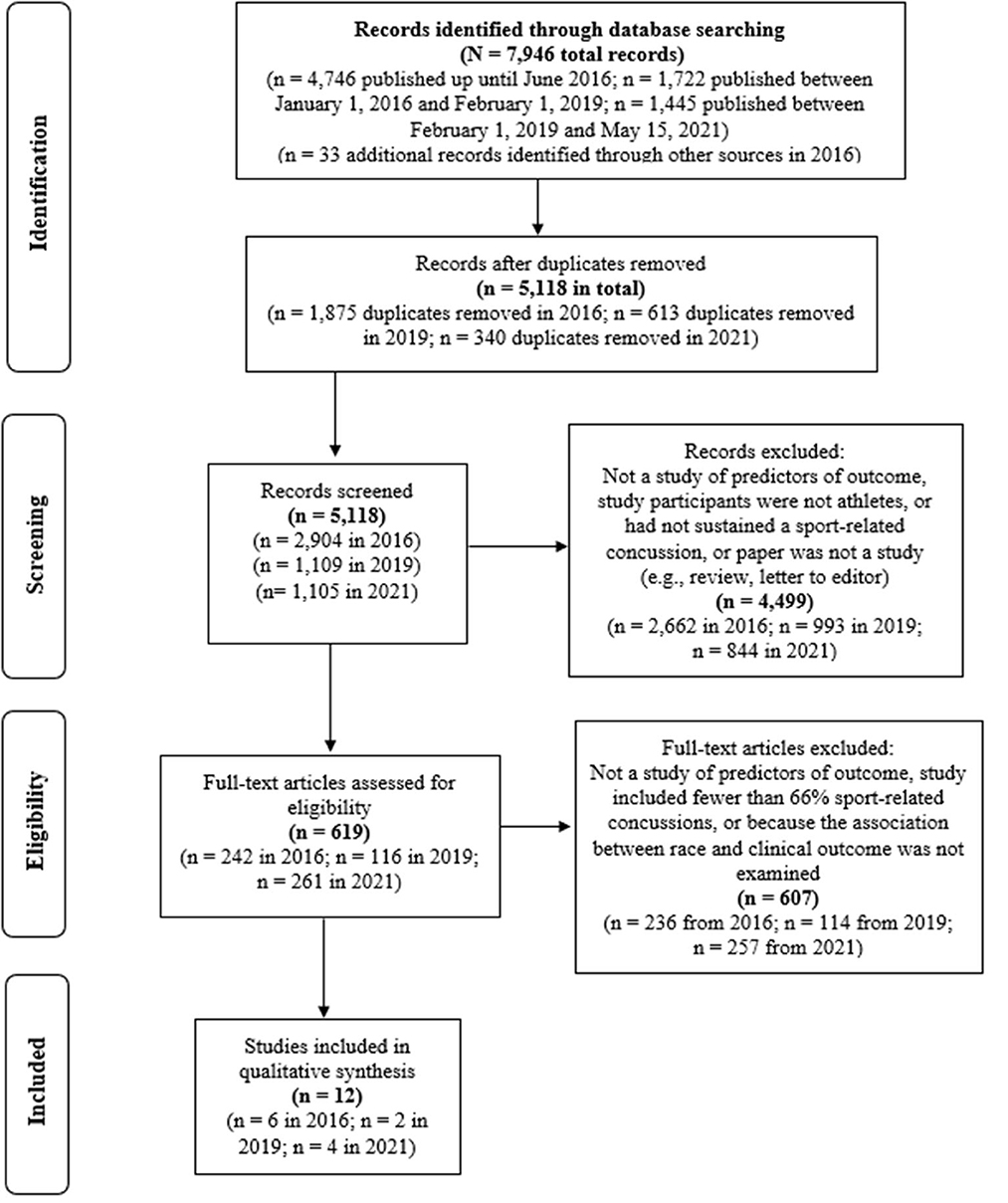
Figure 1. Systematic literature search (PRISMA). There was a mistake in the reporting of the number of records identified in the original search from 2016, as published by Iverson et al. (12). The initial search in 2016 yielded 4,746 records, as noted in this figure.
Two general categories relating to (i) sport and athlete-related terms, and (ii) brain concussion related terms were used as the key search terms, as follows: sport, sports [MeSH], athletic, athlete, player AND craniocerebral trauma, brain injuries, brain concussion, sports concussion, athletic injuries, mild traumatic brain injury, mTBI, traumatic brain injury, TBI, brain concussion, concussion, multiple concussions, repeated concussion, repetitive concussion, cumulative concussions, concussion history, brain damage, prognosis, outcome, recovery, risk factor, injury incidence, sex differences, gender, genetics, ApoE, BDNF, S100B, GFAP, severity, loss of consciousness, LOC, post-traumatic amnesia, PTA, amnesia, retrograde amnesia, seizure, seizures, learning disorder, ADHD, level of education, migraine, mental health, sleep disorders, medications, cervical injury, vestibular injury, psychological reactions, anxiety, depression, headaches, intractable headaches, magnetic resonance imaging, MRI, computer tomography, and CT. This extraordinarily broad set of search terms was used to replicate the terms used in our prior systematic reviews (12–16) because many articles examine multiple predictors, and race/ethnicity might simply be included as a secondary or demographic variable, and thus, a more focused search would likely miss articles that did in fact examine race/ethnicity as one of many predictors or variables analyzed.
To be included, clinical outcomes needed to be measured one or more weeks following injury. We did not study acute clinical outcome. Outcome and clinical recovery were defined broadly to include self-reported resolution of concussion symptoms, improvement in neuropsychological functioning, improvement in vestibular deficits, and time to medical clearance and return to play and/or participation in normal activities, such as school.
Three authors (AKK, CG, and BL) completed the extraction of information from the articles [i.e., first author, year of publication, the PubMed identification number, number of participants, proportion of female participants, age, setting, time since injury, characteristics of the index concussion (e.g., proportion experiencing loss of consciousness, posttraumatic amnesia), study design, outcome examined, and the period for assessing the clinical outcome]. Authors extracted details regarding the association between race and outcome from the index concussion, including results of statistical significance testing, direction of effects, and any quantitative metrics reported in the study (e.g., recovery times, parameter estimates from statistical modeling, effect sizes). Discrepancies were resolved by discussion.
For the included studies, three authors (AKK, CG, and BL) coded whether social determinants of health (SDoH) and associated subcategories were reflected. A coding sheet was developed by the study team to identify SDoH and associated subcategories derived from both the Healthy People 2020 (https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health) and the Healthy People 2030 websites (https://health.gov/healthypeople/objectives-and-data/social-determinants-health). The five SDoH domains identified by Healthy People were included: Economic Stability, Education Assess and Quality, Health Care Access and Quality, Neighborhood and Built Environment, and Social and Community Context. Healthy People 2020 provided a list of several key issues and underlying factors associated with each of the five domains. For example, an important issue included under Economic Stability is “poverty.” All the key issues and underlying factors were included as separate variables to code, and the list was cross-referenced with material on the Healthy People 2030 website, where a separate webpage is available for each SDoH domain. Three co-authors (NC, AKK, and BL) read the text descriptions and identified other key issues or underlying factors that were not included in the Healthy People 2020 bulleted list.
The same three authors (AKK, CG, and BL) also collected information about the sample size, average age, age range, gender, racial composition, and ethnic composition of the sample. The extent to which the studies analyzed or provided information about key health equity variables (e.g., culture/acculturation, socioeconomic status, and language) was characterized as follows: the study (i) provided no mention of the variable, (ii) included the variable as a demographic category only, or (iii) examined the variable in depth (e.g., the health equity variable was a primary variable of interest in the study, or outcome or prognostic results were stratified and reported across levels of the variable). We also coded race and ethnicity in this manner. The content analysis coding sheet is included in the Supplementary material.
Risk of bias for each article was rated by three authors (NC, AKK, and CG) using the Newcastle-Ottawa Scale, a risk of bias assessment system designed for observational studies (17). Differences in risk of bias ratings were resolved by discussion. The scale includes nine items assessing specific study features relating to Sample Selection, Comparability between Research Groups, and Outcome (for Cohort studies) or Exposure (for Case Control studies). For each of the nine items, credit is assigned for stronger, higher quality design features based on criteria presented on the scoring sheets and in the coding manual (17). This scale has been reported to be suitable for systematic reviews (18). For the current review, when rating the Newcastle-Ottawa Scale, we considered race or ethnicity as the “exposure” and prolonged recovery or worse clinical outcome (e.g., symptom duration ≥28 days, worse neurocognitive test performance, longer duration of return to play) from the index concussion as the “outcome.” Additionally, the level of evidence for each article was rated by the same three authors (NC, AKK, and CG) using the Oxford Classification for Evidence-Based Medicine. Differences in the level of evidence ratings were resolved by discussion.
Substantial heterogeneity in the participant populations, comparators, clinical outcomes, and recovery time periods precluded quantitative synthesis and analyses. We performed a narrative synthesis and descriptively summarized the study samples and methodologies. We summarized the results of statistical significance testing (using each study authors' definition of significance, most often was p < 0.05) regarding whether clinical outcome from concussion was or was not associated with race or ethnicity, including the direction of effects. We reported the results of our content analysis descriptively.
A total of 5,118 abstracts were screened, 619 full-text articles were evaluated for inclusion, and 12 studies met inclusion criteria (19–30). Four studies (25%) reported concussion outcome among children or adolescents (maximum sample age ≤ 19 years) (19–22). Eight studies (75%) reported outcome among college-age samples (i.e., the mean sample age >18, they included participants age ≥ 20 years, or they indicated the sample consisted exclusively of college athletes) (23–30). Characteristics for the study populations are summarized in Table 1. There were 2,887 participants (mean age = 17.8 years, SD = 2.04, median = 18.9 years among the eight studies that reported sample age). Two studies involved overlapping samples (19, 20)—the number of non-overlapping participants was 2,769. Ten (83.3%) of the studies were published since 2015, and 5 (41.7%) were published since 2018. One study was published in 2010 and one study was published in 2004. Studies included a median of 26.0% girls (range 0%-50.8%). The racial and ethnic compositions of the included studies are summarized in Table 2. Two-thirds of the studies (66.7%) were prospective designs and one-third (33.3%) were retrospective. Studies in this review examined the following outcomes: recovery time/symptom duration (k = 6) (21, 22, 24–26, 30), time to return to sports (k = 5) (19, 20, 26, 27, 30), mental health problems (k = 2) (28, 29), and neuropsychological functioning and symptom severity (k = 1) (23) following concussion [several studies reported multiple outcomes, so the number of studies sums to greater than 12].
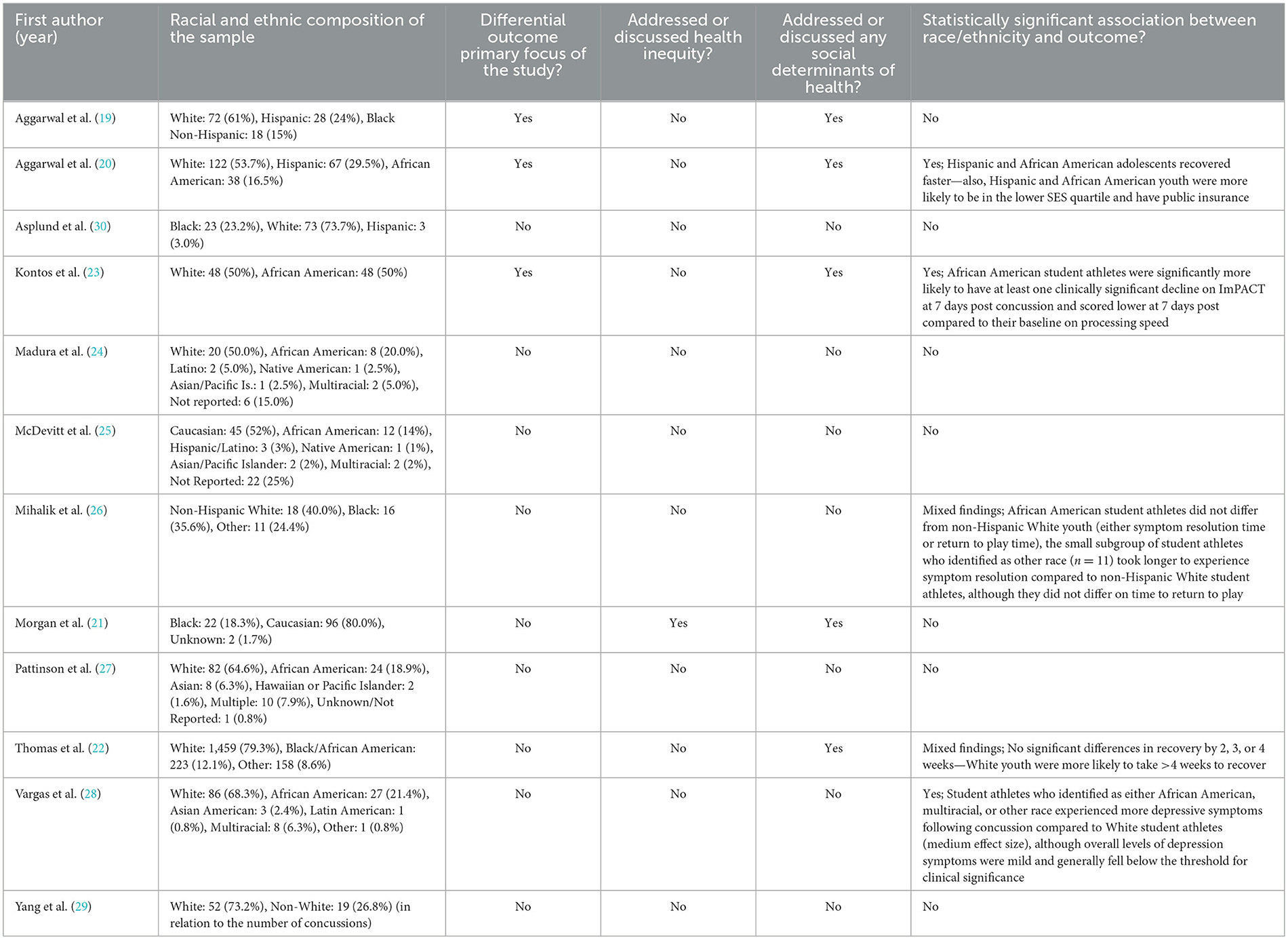
Table 2. Summary of review findings regarding race, ethnicity, and outcome from concussion (studies listed alphabetically).
Level of Evidence and Newcastle-Ottawa Scale ratings are summarized in Table 3. The mean level of evidence was 3.3 (SD = 0.5). Nine studies (75%) were rated as level 3 (i.e., cohort studies) (19, 20, 22, 24–27, 29, 30) and 3 studies (25%) as level 4 (i.e., case-control studies or lower-quality prognostic cohort studies) (21, 23, 28). Studies received credit for between three to eight Newcastle-Ottawa Scale items (mean = 5.7, SD = 1.3).
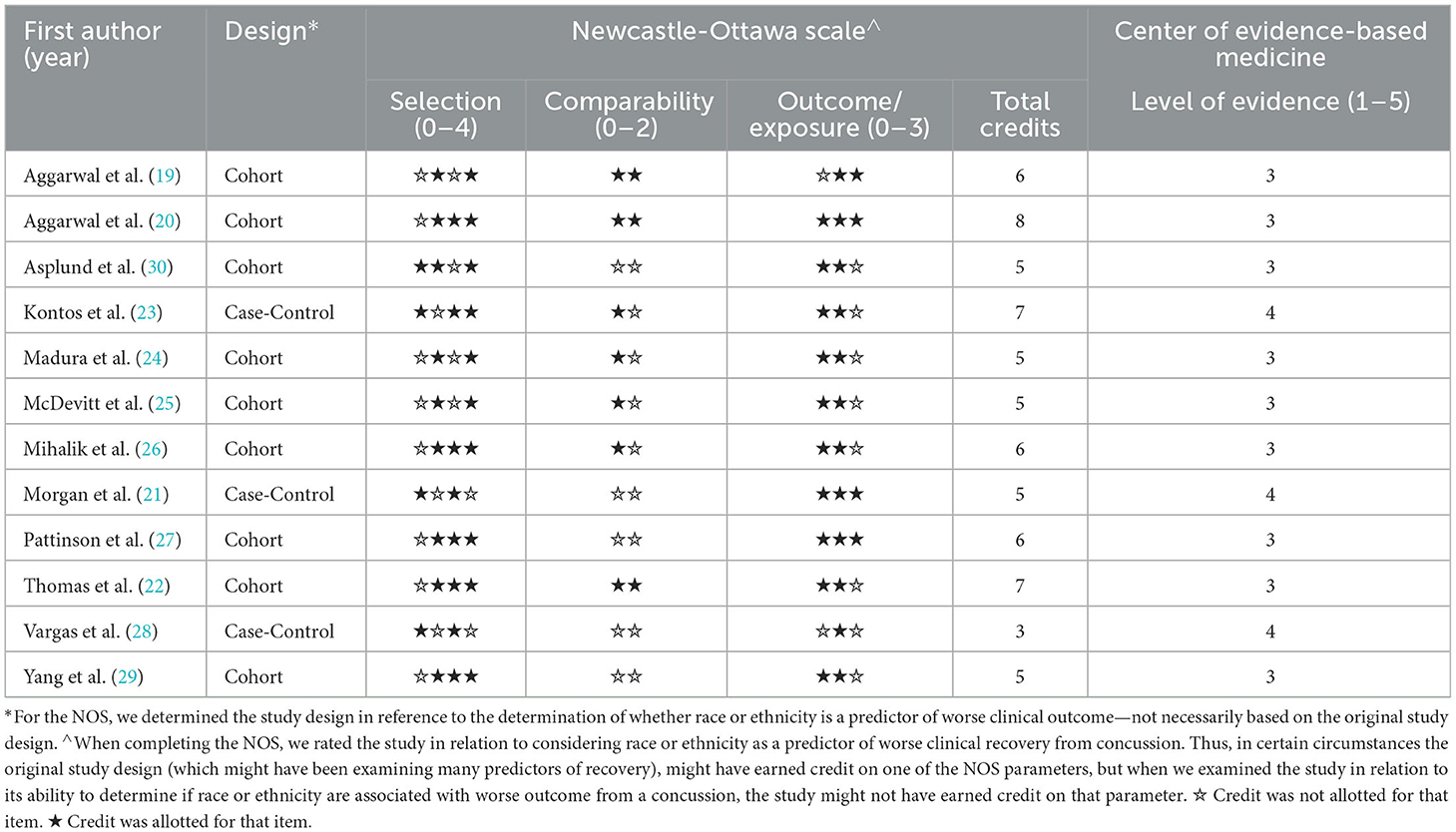
Table 3. The Newcastle-Ottawa Quality Assessment Scale scores and the level of evidence of the included studies (listed alphabetically).
Across all studies and outcomes, the most frequent finding was that clinical outcomes did not differ based on race or ethnicity. Most studies (58.3%) did not find a statistically significant association between race or ethnicity and outcome from concussion. Three studies (25.0%) reported a statistically significant result (20, 23, 28) and the remaining two studies (16.7%) reported predominantly null results with an isolated statistically significant finding (22, 26). Of note, among these studies with at least one statistically significant result, two (40%) reported that racial and ethnic minority youth had better outcomes (i.e., faster recovery times, less likely to take >4 weeks to recover) (20, 22). The remaining three studies reported that racial and ethnic minority youth had worse outcomes (i.e., worse subacute neurocognitive test performance, higher levels of depressive symptoms, and longer symptom resolution time) (23, 26, 28). Among the included articles, only three studies (25%) were specifically designed and carried out to examine whether race and ethnicity were associated with clinical outcomes following concussion (19, 20, 23), and two of these studies reported statistically significant results (20, 23) while the other study reported a null result. However, there are major caveats and considerable nuance to appreciate and consider when interpreting results from these studies. Further detail about the individual studies and their findings are provided in sections below.
Four studies were identified that examined the potential association between race and outcome from a sport-related concussion in children and adolescents (19–22), and two of those studies reported on a partially overlapping sample (19, 20). Thus, there were three independent samples totaling 2,080 youth studied. All three pediatric samples were recruited from specialty concussion clinics.
The clinical outcome in all four studies was recovery time. This included days to recovery for two studies (19, 20), recovery within several time periods for one study (i.e., within 2 weeks, 3 weeks, 4 weeks, or >4 weeks) (22), and persistent symptoms lasting >3 months following an injury in the fourth study (21). Two studies with partially overlapping samples reported mixed results. An initial study of 118 youth noted a 4 day difference in median recovery time between youth identified as White race (n = 72, median 17 days) compared to youth identified as “Minority” race (n = 46, median 13 days), and this difference was not statistically significant in either univariate (p = 0.06) or multivariate (p = 0.50) analyses (19). The investigators added 109 additional youth to the sample and replicated the analyses. With the larger sample (N = 227), the authors noted an eight day difference in median recovery time between youth identified as White race (n = 122, median 19 days) compared to youth identified as a combined Hispanic/African American group (n = 105, median 11 days), and this difference was statistically significant in univariate analyses (p < 0.001) (20). In multivariate models, the authors further stratified their racial and ethnic analyses by gender. Compared to girls who identified as White race (the reference group in these analyses), neither girls who identified as Hispanic or African American (combined; p = 0.91) nor boys who identified as White (p = 0.08) differed in recovery time, though boys who identified as Hispanic or African American (combined) recovered significantly sooner following injury (p = 0.003) (20).
A large study of 1,733 patients (79.3% White) found that youth identified as White were more likely to have prolonged recovery (symptom resolution >4 weeks post injury), compared to youth identified as Black/African American (12.1% of the sample) or Other race (8.6% of the sample; further detail about the racial identities of these youth was not reported) (22). Of note, this study also reported null findings; the racial groups did not differ in terms of proportions of youth recovered within 2 weeks, 3 weeks, or 4 weeks (22). A retrospective case-control study from a specialty concussion clinic compared 40 youth diagnosed with “post-concussion syndrome” (i.e., symptoms lasting >3 months following injury) to matched controls (matched on age and sex) who recovered within 3 weeks (21). The prolonged recovery group included 90% White and 10% Black youth, and the controls included 75.0% White and 22.5% Black youth as well as 2.5% with “unknown” race; these differences were not statistically significant (p = 0.13) (21). Of note, the prolonged recovery group contained only four youth identified as Black.
Eight studies were identified that examined the potential association between race and ethnicity and outcome from sport-related concussion among college-aged individuals (23–30). Across the eight studies there were a total of 689 young adults studied. Study settings included primary care sports medicine clinics, an outpatient hospital-based concussion program, and multiple National Collegiate Athletics Association (NCAA) institutions.
Of the five studies that examined return to play time for college-aged individuals (24–27, 30), none revealed a statistically significant difference in time to return to sport times associated with race or ethnicity. Specifically, in a study of 101 collegiate athletes, researchers reported no statistically significant difference in time to return to play following concussion between student athletes identifying as Black, White, or Hispanic (30). Notably, return to play was assessed as a binary outcome, with prolonged recovery defined as more than seven days to return to play (30). In a case series of 87 athletes (age: M = 19.47, SD = 6.02) return to play time (prolonged return to play defined as more than 60 days) did not differ between racial groups (25). Similarly, in a study of 40 student athletes (age: M = 19.96, SD = 6.28), there were no differences in prolonged return to play (taking >20 days to obtain clearance for full return) associated with race (24). A study of 127 collegiate athletes did not show an association between race and time to return to sports (prolonged recovery was defined as requiring 14 days or more to return to sport) (27). Furthermore, return to play times, assessed as a continuous variable, did not differ by race among 45 collegiate athletes following concussion (26).
One study of 45 collegiate athletes examined symptom severity and duration. Univariate analyses revealed those whose race or ethnicity was classified as “other” experienced longer symptom resolution time as compared to Non-Hispanic White athletes. However, there were no differences in symptom duration between Non-Hispanic White and Black athletes, as well as no association between race and symptom severity (26).
There were mixed findings regarding neurocognitive functioning. Results of a case-control study that matched 48 African American and 48 White high school and collegiate athletes (age, years: M = 19.33, SD = 2.08) revealed that African American athletes were more likely to have clinically significant declines on computerized neurocognitive testing, relative to preinjury baseline performance, at seven days post-injury compared to White participants (p = 0.03). Additionally, relative to preinjury baseline, African American athletes showed greater declines in processing speed than White athletes at seven days post injury (p = 0.01) (23). In contrast, a study of 45 collegiate athletes that compared neurocognitive functioning between Non-Hispanic White, Black, and athletes grouped as “other,” did not reveal an association between race and neurocognitive performance, as measured using the Standardized Assessment of Concussion at multiple time points following injury (26).
In a prospective cohort study of 45 collegiate athletes (51 total concussions), athletes whose race or ethnicity was categorized as “other” performed worse on balance testing compared to White athletes, as measured by the Balance Error Scoring System in an unadjusted negative binomial regression model. However, there were no differences in balance testing performance between Non-Hispanic White and Black athletes (26).
In a study of 84 collegiate athletes, athletes who did not identify as White reported greater levels of depressive symptoms following injury (p = 0.01) but did not differ in baseline depressive symptoms (p = 0.16) or change in depressive symptoms (p = 0.29), as measured by the 7-item Beck Depression Inventory-Fast Screen. Notably, when history of psychiatric treatment was controlled for, race was not associated with depressive symptoms following injury (p = 0.38) (28). Similarly, race was not associated with symptoms of depression or anxiety at 1 week following injury in a study of 67 collegiate athletes, as measured by the Center for Epidemiological Studies Depression Scale and State Trait Anxiety Inventory. Athletes with a pre-existing history of depression were more likely to experience depressive symptoms and state anxiety following concussion (29).
Among the studies included in this review, none were designed and carried out considering social determinants of health (SDoH) as a guiding framework. Further, no study specifically referenced or discussed social determinants of health. With that said, results of our content analysis revealed that five studies (41.7%) addressed a SDoH or closely related topic in some form or fashion (19–23). One study addressed three SDoH domains (21), one study addressed two domains (19), and the remaining three studies addressed one domain (20, 22, 23). The most commonly addressed domain was Healthcare Access and Quality (k = 3) (19, 21, 22). Two studies addressed Economic Stability (19, 20). Two other studies addressed Education Access and Quality (21, 23). One study addressed Social and Community (21). No studies addressed the Neighborhood and Built Environment domain.
No studies directly examined or studied health equity. Only one study referenced or discussed the topic of health equity. Specifically, in their discussion section, Morgan and colleagues position their findings in the context of considerable literature demonstrating childhood health disparities associated with race (21).
Four studies (33.3%) excluded participants based on demographic or health factors (19, 20, 23, 28). They were not excluded based on race. Participants were most commonly excluded for learning disabilities (23), psychiatric disorders (19, 20, 23), or a history of inpatient treatment (28), or substance use disorders (23, 28).
Five studies (41.7%) discussed future directions and research needs that implicated or were related in some form or fashion to social determinants or health equity (19, 20, 23, 26, 28). In terms of SDoH domains, social and community (19, 20, 23, 26, 28), economic stability (19, 23), and education access and quality (19, 23) were most commonly implicated in the context of future clinical and research directions.
Race and ethnicity are social constructs, not biological attributes (31–33). We identified 12 published studies that examined whether there was an association between race or ethnicity and worse clinical outcome from sport-related concussion. We sought to determine whether there is a general association between race or ethnicity and outcome from this injury, and the extent to which other sociodemographic factors or social determinants of health might be associated with any such identified differences. Importantly, of those 12 studies, only three were designed specifically to examine race, ethnicity, or both as a primary variable of interest. In the studies reviewed, the association between race and outcome, broadly, has not been well-characterized, when race was included, it was generally considered a demographic variable of possible interest, and it sometimes was combined (or conflated) with ethnicity. Moreover, the sample sizes associated with self-identified race or ethnicity were often too small to have reasonably powered analyses. Overall, the literature to date is extremely limited and insufficient for drawing conclusions about whether race or ethnicity are categorically associated with outcome from this injury, or more specifically, whether or which social determinants of health might be associated with clinical outcome.
Some of the studies in this review used samples from specialty clinics. In a recent specialty concussion care study, there were no racial disparities in how injured youth athletes were initially medically managed or how they ultimately presented to the specialty clinic despite racial differences in school type and insurance coverage (34). Specialty clinic visits for concussion care during the pandemic were substantially less, however, than prior to the pandemic, and patients tended to present considerably later following injury (i.e., a delayed presentation for specialty care) (35). There is evidence that youth who present for specialty care for concussion earlier have better clinical outcomes, as measured by faster clinical recovery or being less likely to have prolonged symptoms (36–38). Therefore, given disparities in access to specialty care, those disparities could partially underlie differential clinical outcomes.
Even when individuals may have access to healthcare, perceptions and racial inequalities within the healthcare setting may make minoritized populations less likely to seek out healthcare providers. In many cases, the providers are not demographically similar to the patients they serve, and this can create, for example, barriers of understanding and willingness to work collaboratively. Consequently, this may adversely impact healthcare outcomes. Future researchers using specialty clinic samples are encouraged, if possible, to contextualize who is seen in the clinic relative to the local population. For example, if the proportion of the local population is 45% Black but the clinic sample is only 5% Black, reporting this discrepancy will help contextualize possible insurance-related or other access-related issues and barriers to specialty care. Of course, researchers are encouraged to directly study social determinants of health like socioeconomic factors, health literacy, and community-level factors that might be associated with recruitment bias, access to care, and outcome from injury.
There are some studies illustrating differences associated with race on some clinical measures used to assess the effects of, and monitor recovery from, concussion (20, 39). There are many possible reasons underlying some of these differences, including quality of education (40), socioeconomic status (39–41), and stereotype threat (42). Stereotype threat refers to “being at risk of confirming, as self-characteristic, a negative stereotype about one's group” [(42), p. 797]. Stereotype threat, contextual variables, and perceived discrimination are associated with lower scores on neuropsychological testing in some studies (43–46). Moreover, it is possible that stereotype threat can be a social barrier in a health care clinical encounter that can contribute to greater patient anxiety and possible disparities in health care utilization (47). More research designed to deconstruct and quantify the associations between a broad range of contextual and interpersonal factors that might influence reporting or performance on clinical outcome measures, or how they are interpreted, will likely lead to more refined and personalized use of these measures.
Some research has identified differences and disparities associated with race or ethnicity with regard to awareness of concussion signs and symptoms (10), utilization of health care services for concussion (6–8), and receiving academic accommodations following concussion (9). Awareness of concussion signs and symptoms facilitates immediate removal from play following concussion and is associated with better clinical outcome in college students (48). College students who continue to participate in sports following concussion, in contrast to immediate removal from play, are more likely to have greater symptoms, longer recovery times, and greater time away from sports (49, 50). Therefore, when athletes, athletic trainers, and coaches have less knowledge and awareness about concussion signs and symptoms, injured athletes might be less likely to be removed from play following an injury—thus increasing their risk for prolonged recovery. Health care service utilization is also associated with outcome.
Future concussion researchers are encouraged to discuss differences associated with race contextualized within a social ecological model, and it is important to appreciate that racism and other social determinants of health, not race per se, are risk factors for different health outcomes. Racism is a social determinant of health that operates at the intrapersonal, interpersonal, institutional, and structural levels contributing to health inequities and worse health outcomes for children and adolescents (51). Race is therefore sometimes used as a proxy for vulnerability to institutional and structural racism, socioeconomic disparities, and health inequities. There is excellent guidance for researchers on reporting race and ethnicity in medical and science journals that is designed to promote fairness, equity, consistency, and clarity (31).
Researchers and healthcare providers are encouraged to address systemic inequities in research and training. Myths and miseducation appear persistent in medical training. For example, 25% of surveyed residents believed that black skin is thicker than white, and there were misbeliefs that Black people experience pain differently than whites (52). This has led to racial biases in pain management, as well as more systemic inequalities in medical treatment (53–55). Such racial biases have been identified among counseling and clinical psychology trainees as well. For example, given identical symptomatology, graduate students rated a hypothetical Black client as less symptomatic compared to a hypothetical White client (56). Moreover, those from minoritized populations may not feel understood by providers, and their concerns may be dismissed by misperceptions, racial biases, and language barriers.
There are also important considerations regarding family structures. For example, some parents may have limited ability to take time off from work and thus to attend numerous healthcare appointments, perhaps especially those located some distance or time from their home or work. Other youth may be in the care of grandparents, and thus attention to caregiver demographics and family-specific factors potentially impacting healthcare may be the key.
Telehealth is a strategy for improving access and quality of pediatric healthcare (57). Telehealth is possible for youth sport-related concussions (58, 59), and in pediatric neurology more broadly (60). In a pilot study comparing in-person to telehealth concussion care, therapeutic alliance scores for parents and caregivers were significantly higher for the in-person condition than for the telehealth condition—but not for the patients themselves. Both telehealth and in-person care were associated with high satisfaction scores (61). However, in a large pediatric neurology study, there were racial and ethnic disparities between youth who used telephone encounters vs. telemedicine (audio and video) encounters (60). In some cases, families do not have the technology (e.g., smart phones) or the technological literacy to participate in telemedicine. More research is also needed in regard to disparities and outcomes associated with telehealth concussion care.
Based on the present review, it is not known the extent to which there are differences in clinical outcome from sport-related concussion associated with race or ethnicity—or the possible underlying reasons for any such differences. Identifying and quantifying factors that are associated with worse, or better, clinical outcome following concussion will help inform future multivariable prognostic risk models that could be used to guide medical management and inform personalized and precision treatment and rehabilitation for injured student athletes. Moreover, identifying these factors might help guide efforts to improve health literacy, enhance equitable access to health care, and reduce disparities in health outcomes.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
NC helped conceptualize the review, drafted sections of the manuscript, extracted data from all studies in the review, rated risk of bias and level of evidence for all studies in the review, assisted with the literature review, edited the manuscript, and approved the final manuscript. CG, AK-K, and BL extracted data from studies in the review, rated risk of bias and level of evidence for studies in the review, edited the manuscript, and approved the final manuscript. AH and AS reviewed the articles included in the review for conceptual and methodological issues and edited the manuscript. MN critically reviewed and edited the manuscript. GI helped conceptualize the review, conducted article screening prior to the full text reviews, drafted sections of the manuscript, and edited drafts of the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
GI acknowledges unrestricted philanthropic support from ImPACT Applications, Inc., the Mooney-Reed Charitable Foundation, Boston Bolts, the National Rugby League, and the Schoen Adams Research Institute at Spaulding Rehabilitation. None of the above entities were involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
AS has received research funding from the American Academy of Neurology, National Institute of Health, National Science Foundation, and the Russel Sage Foundation. GI serves as a scientific advisor for NanoDX®, Sway Operations, LLC, and Highmark, Inc. He has a clinical and consulting practice in forensic neuropsychology, including expert testimony, involving individuals who have sustained mild TBIs (including former athletes). He has received research funding from several test publishing companies, including ImPACT Applications, Inc., CNS Vital Signs, and Psychological Assessment Resources (PAR, Inc.). He has received research funding as a principal investigator from the National Football League and subcontract grant funding as a collaborator from the Harvard Integrated Program to Protect and Improve the Health of National Football League Players Association Members.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1110539/full#supplementary-material
1. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C.: The National Academic Press (2003).
2. Flores G, Committee On Pediatric R. Technical report—Racial and ethnic disparities in the health and health care of children. Pediatrics. (2010) 125:e979–e1020. doi: 10.1542/peds.2010-0188
3. Dzierzewski JM, Ravyts SG, Dautovich ND, Perez E, Schreiber D, Rybarczyk BD. Mental health and sleep disparities in an urban college sample: a longitudinal examination of White and Black students. J Clin Psychol. (2020) 76:1972–83. doi: 10.1002/jclp.22974
4. Kodish T, Lau AS, Gong-Guy E, Congdon E, Arnaudova I, Schmidt M, et al. Enhancing racial/ethnic equity in college student mental health through innovative screening and treatment. Adm Policy Ment Health. (2022) 49:267–82. doi: 10.1007/s10488-021-01163-1
5. McEligot AJ, Mitra S, Beam W. The association between fitness and obesity in diverse multi-ethnic college students. J Am Coll Health. (2021) 69:290–7. doi: 10.1080/07448481.2019.1665054
6. Lyons TW, Miller KA, Miller AF, Mannix R. Racial and ethnic differences in emergency department utilization and diagnosis for sports-related head injuries. Front Neurol. (2019) 10:690. doi: 10.3389/fneur.2019.00690
7. Copley M, Jimenez N, Kroshus E, Chrisman SPD. Disparities in use of subspecialty concussion care based on ethnicity. J Racial Ethn Health Disparities. (2020) 7:571–6. doi: 10.1007/s40615-019-00686-6
8. Wallace JS, Mannix RC. Racial disparities in diagnosis of concussion and minor head trauma and mechanism of injury in pediatric patients visiting the emergency department. J Pediatr. (2021) 233:249–54. doi: 10.1016/j.jpeds.2021.01.057
9. Snedden TR, Pierpoint LA, Currie DW, Comstock RD, Grubenhoff JA. Postconcussion academic support in children who attend a primary care provider follow-up visit after presenting to the emergency department. J Pediatr. (2019) 209:168–75. doi: 10.1016/j.jpeds.2019.01.041
10. Wallace J, Covassin T, Moran R. Racial disparities in concussion knowledge and symptom recognition in american adolescent athletes. J Racial Ethn Health Disparities. (2018) 5:221–8. doi: 10.1007/s40615-017-0361-1
11. Deichman JJ, Graves JM, Klein TA, Mackelprang JL. Characteristics of youth who leave the emergency department without being seen following sports-related concussion. Concussion. (2019) 4:CNC68. doi: 10.2217/cnc-2019-0010
12. Iverson GL, Gardner AJ, Terry DP, Ponsford JL, Sills AK, Broshek DK, et al. Predictors of clinical recovery from concussion: a systematic review. Br J Sports Med. (2017) 51:941. doi: 10.1136/bjsports-2017-097729
13. Cook NE, Gaudet Iii CE, Van Patten R, Kissinger-Knox AM, Iverson G. Clinical outcome following sport-related concussion among children and adolescents with a history of prior concussion: a systematic review. J Neurotrauma. (2022) 3:6. doi: 10.1186/s40798-022-00528-6
14. Iverson GL, Williams MW, Gardner AJ, Terry DP. Systematic review of preinjury mental health problems as a vulnerability factor for worse outcome after sport-related concussion. Orthop J Sports Med. (2020) 8:2325967120950682. doi: 10.1177/2325967120950682
15. Cook NE, Iaccarino MA, Karr JE, Iverson GL. Attention-deficit/hyperactivity disorder and outcome after concussion: a systematic review. J Dev Behav Pediatr. (2020) 41:571–82. doi: 10.1097/DBP.0000000000000808
16. Terry DP, Buttner F, Huebschmann NA, Gardner AJ, Cook NE, Iverson GL. Systematic review of pre-injury migraines as a vulnerability factor for worse outcome following sport-related concussion. Front Neurol. (2022) 13:915357. doi: 10.3389/fneur.2022.915357
17. Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-Randomised Studies in Meta-Analyses. Ottawa, ON: Ottawa Hospital Research Institute.
18. Deeks JJ, Dinnes J, D'Amico R, Sowden AJ, Sakarovitch C, Song F, et al. Evaluating non-randomised intervention studies. Health Technol Assess. (2003) 7:1–173. doi: 10.3310/hta7270
19. Aggarwal SS, Ott SD, Padhye NS, Meininger JC, Armstrong TS. Clinical and demographic predictors of concussion resolution in adolescents: a retrospective study. Appl Neuropsychol Child. (2019) 8:50–60. doi: 10.1080/21622965.2017.1381099
20. Aggarwal SS, Ott SD, Padhye NS, Schulz PE. Sex, race, ADHD, and prior concussions as predictors of concussion recovery in adolescents. Brain Inj. (2020) 34:809–17. doi: 10.1080/02699052.2020.1740942
21. Morgan CD, Zuckerman SL, Lee YM, King L, Beaird S, Sills AK, et al. Predictors of postconcussion syndrome after sports-related concussion in young athletes: a matched case-control study. J Neurosurg Pediat. (2015) 15:589. doi: 10.3171/2014.10.PEDS14356
22. Thomas DJ, Coxe K, Li H, Pommering TL, Young JA, Smith GA, et al. Length of recovery from sports-related concussions in pediatric patients treated at concussion clinics. Clin J Sport Med. (2018) 28:56–63. doi: 10.1097/JSM.0000000000000413
23. Kontos AP, Elbin RJ III, Covassin T, Larson E. Exploring differences in computerized neurocognitive concussion testing between African American and White athletes. Arch Clin Neuropsychol. (2010) 25:734–44. doi: 10.1093/arclin/acq068
24. Madura SA, McDevitt JK, Tierney RT, Mansell JL, Hayes DJ, Gaughan JP, et al. Genetic variation in SLC17A7 promoter associated with response to sport-related concussions. Brain Inj. (2016) 30:908–13. doi: 10.3109/02699052.2016.1146958
25. McDevitt J, Tierney RT, Phillips J, Gaughan JP, Torg JS, Krynetskiy E. Association between GRIN2A promoter polymorphism and recovery from concussion. Brain Inj. (2015) 29:1674–81. doi: 10.3109/02699052.2015.1075252
26. Mihalik JP, Chandran A, Powell JR, Roby PR, Guskiewicz KM, Stemper BD, et al. Do head injury biomechanics predict concussion clinical recovery in college american football players? Annals Biomed Eng. (2020) 3:2555–65. doi: 10.1007/s10439-020-02658-y
27. Pattinson CL, Meier TB, Guedes VA, Lai C, Devoto C, Haight T, et al. Plasma biomarker concentrations associated with return to sport following sport-related concussion in collegiate athletes-a concussion assessment, research, and education (CARE) consortium study. JAMA Network Open. (2020) 3:1–11. doi: 10.1001/jamanetworkopen.2020.13191
28. Vargas G, Rabinowitz A, Meyer J, Arnett PA. Predictors and prevalence of postconcussion depression symptoms in collegiate athletes. J Athl Train. (2015) 50:250–5. doi: 10.4085/1062-6050-50.3.02
29. Yang J, Peek-Asa C, Covassin T, Torner JC. Post-concussion symptoms of depression and anxiety in division I collegiate athletes. Dev Neuropsychol. (2015) 40:18–23. doi: 10.1080/87565641.2014.973499
30. Asplund CA, McKeag DB, Olsen CH. Sport-related concussion: factors associated with prolonged return to play. Clin J Sport Med. (2004) 14:339–43. doi: 10.1097/00042752-200411000-00003
31. Flanagin A, Frey T, Christiansen SL. Committee AMAMoS. Updated guidance on the reporting of race and ethnicity in medical and science. J JAMA. (2021) 326:621–7. doi: 10.1001/jama.2021.13304
32. Brasel KJ, Coimbra R. Toward improved reporting and use of race, ethnicity, sex, and gender: an editorial. J Trauma Acute Care Surg. (2022) 92:629–30. doi: 10.1097/TA.0000000000003503
33. Smedley A, Smedley BD. Race as biology is fiction, racism as a social problem is real: Anthropological and historical perspectives on the social construction of race. Am Psychol. (2005) 60:16–26. doi: 10.1037/0003-066X.60.1.16
34. Wallace J, Hou BQ, Hajdu K, Tang AR, Grusky AZ, Lee T, et al. Health care navigation of black and white adolescents after sport-related concussion: a path toward health equity. J Athl Train. (2022) 57:352–9. doi: 10.4085/1062-6050-0330.21
35. Kontos AP, Eagle SR, Holland CL, Thomas D, Hickey R, Santucci C, et al. Effects of the COVID-19 pandemic on patients with concussion presenting to a specialty clinic. J Neurotrauma. (2021) 38:2918–22. doi: 10.1089/neu.2021.0203
36. Kontos AP, Jorgensen-Wagers K, Trbovich AM, Ernst N, Emami K, Gillie B, et al. Association of time since injury to the first clinic visit with recovery following concussion. JAMA Neurol. (2020) 77:435–40. doi: 10.1001/jamaneurol.2019.4552
37. Eagle SR, Puligilla A, Fazio-Sumrok V, Kegel N, Collins MW, Kontos AP. Association of time to initial clinic visit with prolonged recovery in pediatric patients with concussion. J Neurosurg Pediatr. (2020) 26:165–70. doi: 10.3171/2020.2.PEDS2025
38. Barnhart M, Bay RC, Valovich McLeod TC. The influence of timing of reporting and clinic presentation on concussion recovery outcomes: a systematic review and meta-analysis. Sports Med. (2021) 51:1491–508. doi: 10.1007/s40279-021-01444-7
39. Houck Z, Asken B, Clugston J, Perlstein W, Bauer R. Socioeconomic status and race outperform concussion history and sport participation in predicting collegiate athlete baseline neurocognitive scores. J Int Neuropsychol Soc. (2018) 24:1–10. doi: 10.1017/S1355617717000716
40. Houck ZM, Asken BM, Bauer RM, Caccese JB, Buckley TA, McCrea MA, et al. Academic aptitude mediates the relationship between socioeconomic status and race in predicting ImPACT scores in college athletes. Clin Neuropsychol. (2020) 34:561–79. doi: 10.1080/13854046.2019.1666923
41. Wallace J, Karr JE, Schatz P, Worts P, Covassin T, Iverson GL. The frequency of low scores on impact in adolescent student-athletes: stratification by race and socioeconomic status using multivariate base rates. Dev Neuropsychol. (2022) 47:125–35. doi: 10.1080/87565641.2022.2034827
42. Steele CM, Aronson J. Stereotype threat and the intellectual test performance of African Americans. J Pers Soc Psychol. (1995) 69:797–811. doi: 10.1037/0022-3514.69.5.797
43. Nguyen HH, Ryan AM. Does stereotype threat affect test performance of minorities and women? A meta-analysis of experimental evidence. J Appl Psychol. (2008) 93:1314–34. doi: 10.1037/a0012702
44. Brown RP, Day EA. The difference isn't black and white: stereotype threat and the race gap on Raven's advanced progressive matrices. J Appl Psychol. (2006) 91:979–85. doi: 10.1037/0021-9010.91.4.979
45. VanLandingham H, Ellison RL, Laique A, Cladek A, Khan H, Gonzalez C, et al. A scoping review of stereotype threat for BIPOC: cognitive effects and intervention strategies for the field of neuropsychology. Clin Neuropsychol. (2022) 36:503–22. doi: 10.1080/13854046.2021.1947388
46. Thames AD, Hinkin CH, Byrd DA, Bilder RM, Duff KJ, Mindt MR, et al. Effects of stereotype threat, perceived discrimination, and examiner race on neuropsychological performance: simple as black and white? J Int Neuropsychol Soc. (2013) 19:583–93. doi: 10.1017/S1355617713000076
47. Abdou CM, Fingerhut AW. Stereotype threat among black and white women in health care settings. Cultur Divers Ethnic Minor Psychol. (2014) 20:316–23. doi: 10.1037/a0036946
48. Asken BM, Bauer RM, Guskiewicz KM, McCrea MA, Schmidt JD, Giza CC, et al. Immediate removal from activity after sport-related concussion is associated with shorter clinical recovery and less severe symptoms in collegiate student-athletes. Am J Sports Med. (2018) 46:1465–74. doi: 10.1177/0363546518757984
49. Asken BM, McCrea MA, Clugston JR, Snyder AR, Houck ZM, Bauer RM. “Playing through it”: delayed reporting and removal from athletic activity after concussion predicts prolonged recovery. J Athl Train. (2016) 51:329–35. doi: 10.4085/1062-6050-51.5.02
50. Eagle SR, Asken B, Trbovich A, Houck ZM, Bauer RM, Clugston JR, et al. Estimated duration of continued sport participation following concussions and its association with recovery outcomes in collegiate athletes: findings from the NCAA/DoD care consortium. Sports Med. (2022) 52:1991–2001. doi: 10.1007/s40279-022-01668-1
51. Fanta M, Ladzekpo D, Unaka N. Racism and pediatric health outcomes. Curr Probl Pediatr Adolesc Health Care. (2021) 51:101087. doi: 10.1016/j.cppeds.2021.101087
52. Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci USA. (2016) 113:4296–301. doi: 10.1073/pnas.1516047113
53. Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J Public Health. (2012) 102:988–95. doi: 10.2105/AJPH.2011.300621
54. Goyal MK, Kuppermann N, Cleary SD, Teach SJ, Chamberlain JM. Racial disparities in pain management of children with appendicitis in emergency departments. JAMA Pediatr. (2015) 169:996–1002. doi: 10.1001/jamapediatrics.2015.1915
55. Meghani SH, Byun E, Gallagher RM. Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med. (2012) 13:150–74. doi: 10.1111/j.1526-4637.2011.01310.x
56. Gushue GV. Race, color-blind racial attitudes, and judgments about mental health: a shifting standards perspective. J Couns Psychol. (2004) 51:398–407. doi: 10.1037/0022-0167.51.4.398
57. Curfman AL, Hackell JM, Herendeen NE, Alexander JJ, Marcin JP, Moskowitz WB, et al. Telehealth: improving access to and quality of pediatric health care. Pediatrics. (2021) 148:129. doi: 10.1542/peds.2021-053129
58. McPherson JI, Saleem GT, Haider MN, Leddy JJ, Torres D, Willer BS. Development of a telehealth examination for sport-related concussion in the outpatient setting. Neurology. (2022) 98:S8–9. doi: 10.1212/01.wnl.0000801808.74733.1d
59. Womble MN, Reynolds E, Kissinger-Knox A, Collins MW, Kontos AP, West RV, et al. The emerging role of telehealth for concussion clinical care during the coronavirus (COVID-19) pandemic. J Head Trauma Rehabil. (2022) 37:E49–54. doi: 10.1097/HTR.0000000000000713
60. Rametta SC, Fridinger SE, Gonzalez AK, Xian J, Galer PD, Kaufman M, et al. Analyzing 2,589 child neurology telehealth encounters necessitated by the COVID-19 pandemic. Neurology. (2020) 95:e1257–e66. doi: 10.1212/WNL.0000000000010010
Keywords: concussion, clinical recovery, race, ethnicity, mild traumatic brain injury, social determinants of health (SDOH)
Citation: Cook NE, Gaudet CE, Kissinger-Knox A, Liu BC, Hunter AA, Norman MA, Saadi A and Iverson GL (2023) Race, ethnicity, and clinical outcome following sport-related concussion: a systematic review. Front. Neurol. 14:1110539. doi: 10.3389/fneur.2023.1110539
Received: 28 November 2022; Accepted: 10 April 2023;
Published: 14 June 2023.
Edited by:
Ramon Diaz-Arrastia, University of Pennsylvania, United StatesReviewed by:
Maria Isabel Chamorro Muñoz, Andusian Health Service, SpainCopyright © 2023 Cook, Gaudet, Kissinger-Knox, Liu, Hunter, Norman, Saadi and Iverson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nathan E. Cook, bmVjb29rQG1naC5oYXJ2YXJkLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.