- 1Division of Neurology, Department of Medicine, University of Toronto, Toronto, ON, Canada
- 2Grey Bruce Health Services, Owen Sound, ON, Canada
- 3Hurvitz Brain Sciences Program, Neurology Quality and Innovation Lab, Division of Neurology, Department of Medicine, Sunnybrook Health Sciences Center, University of Toronto, Toronto, ON, Canada
New-onset refractory status epilepticus (NORSE) is a clinical presentation where an individual develops refractory status epilepticus without active epilepsy, or related neurological conditions. A subset of these individuals has a preceding fever and would be diagnosed with febrile infection-related epilepsy syndrome (FIRES). The underlying etiology of this condition varies and includes autoimmune and viral encephalitides. These conditions require multiple specialized health care teams working collaboratively and specific resources for investigation of the underlying etiology and management to provide optimal patient care. In this paper, we provide: (1) recommendations upon early recognition of NORSE and FIRES, (2) guidance on the resources needed to optimally provide care, and (3) guidance on considerations to initiate transfer of patients to a more specialized medical center. Additional recommendations for resource-austere centers without the ability to transfer such patients are also discussed. These recommendations are only for adult patients with NORSE as pediatric patients may require additional special considerations.
1. Introduction
New-onset refractory status epilepticus (NORSE) can be defined as a clinical presentation in a patient without active epilepsy or other existing relevant neurological disorder, with new onset of refractory status epilepticus in the absence of a clear acute or active structural, metabolic, or toxic cause. Refractory status epilepticus (RSE) is a condition where continuous or recurrent seizures do not stop with standard anti-epileptic medications (1). The duration of seizure activity required to diagnose status epilepticus varies by type of seizure. Generalized convulsive status epilepticus involves at least 5 min of continuous seizure activity or repeated seizures without return to baseline in-between lasting at least 5 min. The timepoint at which this prolonged seizure activity may result in long term consequences is believed to be at 30 min. Focal status epilepticus is defined by 10 min or more of focal seizure activity with impaired awareness, with the possibility for long term consequences to arise after 60 min. Nonconvulsive status epilepticus occurs when seizure activity is present for 10 or more minutes lacking prominent motor symptoms (2). Status epilepticus is considered refractory if “persisting despite administration of at least 2 appropriately selected and dosed parenteral medications including a benzodiazepine. There is no specific seizure duration required” (1). NORSE has a subset of cases meeting the definition for febrile infection-related epilepsy syndrome (FIRES), where a febrile illness precedes the onset of refractory status epilepticus by 24 h to 2 weeks (1).
Although the prevalence of NORSE has not been studied and identified, the annual incidence of refractory status epilepticus is estimated to be 3.0–7.2 per 100,000 adults per year (3, 4). One study showed 20% of cases of refractory status epilepticus did not have a clear etiology after initial investigations (5), thereby making NORSE a rare condition. Despite its incidence, there is significant associated morbidity and mortality (5), and thus early recognition, identification, and transfer to an appropriate care-setting are paramount.
2. Early recognition
A prodromal period can precede the onset NORSE by a couple of weeks and often includes non-specific symptoms such as confusion, fever, fatigue, headache, gastrointestinal, or respiratory symptoms. It is estimated that this prodromal period is present in ~60% of cases (5). Individuals may then develop infrequent seizures which evolve into status epilepticus (6).
NORSE should be a diagnostic consideration in individuals presenting with new onset recurrent seizures evolving into status epilepticus with no known history of epilepsy and no clear identifiable etiology after initial blood work, CSF studies, and brain imaging has been completed.
There are several identified predictors of prolonged refractory status epilepticus. These include the presence of acute brain lesions, increased severity of status epilepticus (measured using the status epilepticus severity score [STESS] (7)), non-convulsive status epilepticus with coma, and increased serum albumin levels at onset of status epilepticus (8). STESS alone was found to be predictive of outcome and includes age, history of seizures, seizure type, and degree of impaired consciousness (7). The presence of these predictors may serve as a flag for clinicians, as each day of status epilepticus is associated with increased risk of mortality (8). As these predictive markers were identified in a more general population of individuals with status epilepticus, is unclear if they hold similar predictive value in the subset of those with NORSE and FIRES. It is plausible that considering NORSE top-of-mind in the differential diagnosis of new status epilepticus may aid in early recognition and clinical considerations for transfer, especially in resource-austere settings.
3. Investigations and treatment requirements
While it is of prime importance to provide airway and cardiovascular/blood pressure support and to halt seizures as soon as possible to prevent further neurologic injury, further consideration must be given to other aspects, including monitoring for breakthrough or nonconvulsive seizures and searching for an underlying etiology; especially one that can be treated. Once the patient is reasonably stabilized, consideration should be given to transferring the patient to a tertiary care center where more specialized investigations and care can be implemented.
An important aspect of a higher-level of care includes the multidisciplinary team, and ability to case conference about such patients with actionable diagnostic and treatment strategies. Centers with neurocritical care expertise are also uniquely qualified to monitor and treat these complex patients. Consultant teams are essential for the co-management of these cases. These services include Neurology with expertise in epilepsy and Internal Medicine and its subspecialties, who may be needed to help manage the multi-system effects of prolonged seizure activity and complications of antiseizure treatments including anesthetics (9). Individuals who continue to have seizures refractory to available therapies or sustain significant complications benefit from early involvement of palliative care for symptom management, bereavement support for the patients’ family, and possibly end of life care (10–12).
Furthermore, specialized neuro-focused centers play an important role in the recovery phase where multidisciplinary team members such as physiotherapy, occupational therapy, speech language pathology, and rehabilitation medicine can collaboratively address the ongoing needs of patients who survive the acute phase of this illness. The burden of critical illness on NORSE patients is an important consideration with individuals exhibiting prolonged hospital stays, with a median ICU stay of 26 days (13, 14), often with neurological sequalae including altered cognition and development of epilepsy (12, 15, 16).
From an investigation standpoint, readily available access to continuous scalp EEG monitoring with video and MR imaging are important aspects of care. Having access to specialized diagnostic tests including autoimmune, paraneoplastic antibody testing, viral PCR testing may aid in early diagnosis (or lack thereof) of underlying etiology. In a significant proportion of cases, no etiology is identified, rendering their classification as cryptogenic (5), although with increasing recognition of various autoimmune etiologies the cryptogenic category is diminishing. In addition to standard treatment, some patients with NORSE may benefit from immunomodulatory therapies, such as corticosteroids, intravenous immunoglobulins, or plasma exchange, particularly if the underlying cause is thought to be autoimmune or inflammatory. The provision of some of these services (e.g., plasma exchange) is a challenge in austere settings.
In resource-austere settings where transfer to a comprehensive center is not possible, substitution of modalities of investigation and/or virtual care may be considered. Critical care settings without subspecialized expertise, CT imaging instead of MRI to rule out gross structural lesions, and serial routine EEGs instead of continuous monitoring can be considered (Table 1).
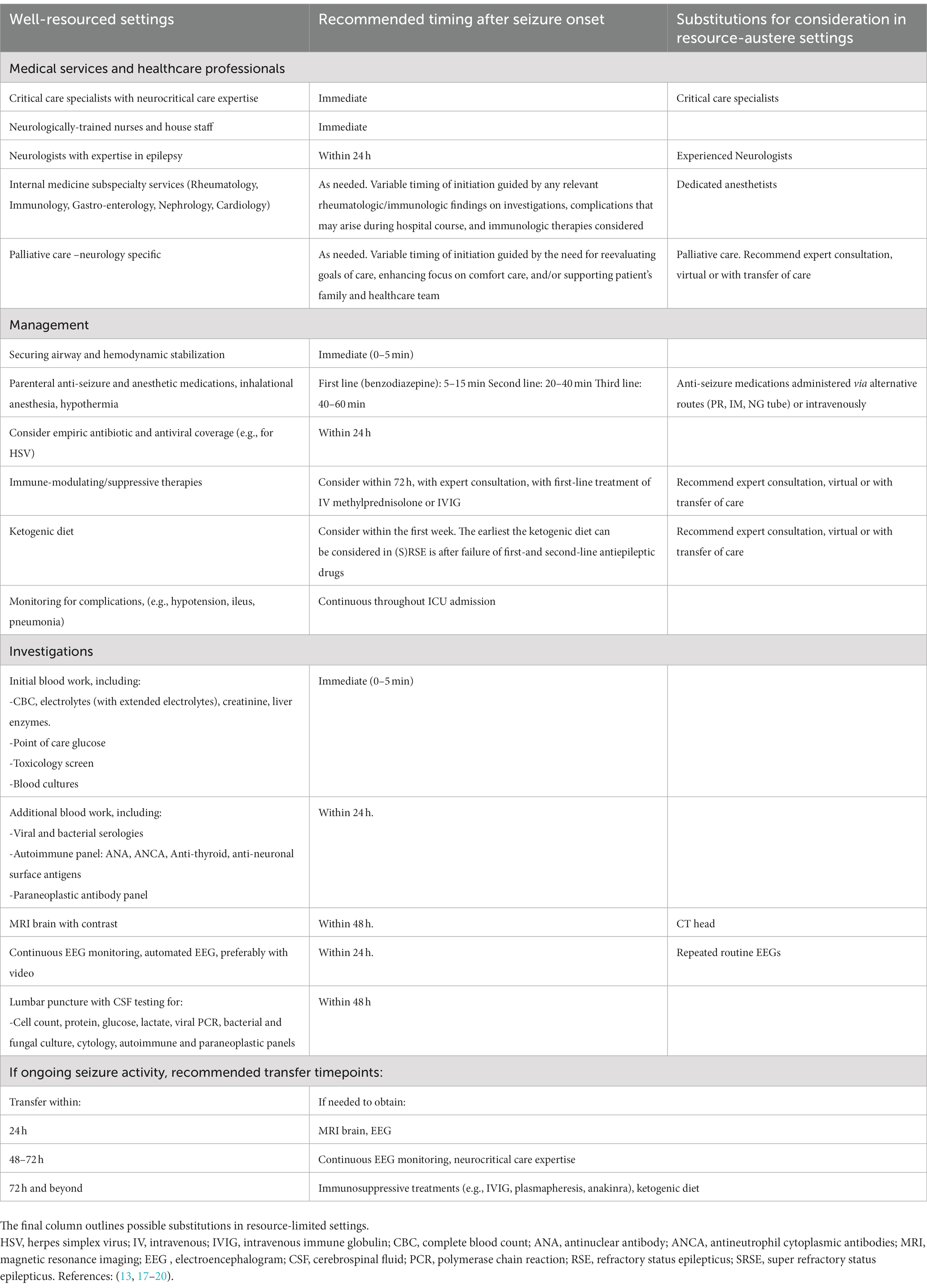
Table 1. Resources needed to provide optimal care for NORSE patients in the acute phase of their illness.
4. Proposed algorithm for recognition and transfer
When a patient is identified as having ongoing seizure activity, beyond the timepoints required for meeting criteria of status epilepticus (2), and after administration of an appropriately dosed parenteral benzodiazepine and another appropriate medication for treating status epilepticus (1) a diagnosis of refractory epilepticus is made. Specialized critical care services are crucial for providing optimal care to patients with NORSE, as this condition requires prompt and aggressive treatment in an ICU setting. Early transfer is also important because the critical care management of NORSE patients has potentially life-threatening complications that can arise such as respiratory failure (severe acute respiratory distress syndrome [ARDS]), cardiac complications (from seizure or anesthetics), gastro-intestinal complications, and metabolic disturbances.
When transferring a patient with NORSE to a specialized critical care facility, special considerations with attention to airway patency, adequate circulatory support, and provision of seizure-stabilizing medications and equipment for transport are necessary. A trained medical team with expertise in critical care and neurology should oversee the transfer, with appropriate monitoring and interventions in place to manage any potential complications that may arise during transport.
Early transfer should be facilitated, when possible, especially in cases where a transfer would enable access to essential tests (e.g., MRI, cEEG, neurocritical care, use of volatile anesthetics in the ICU for sedation or seizure suppression), and neuromodulatory treatment options (IVIG, plasma exchange, biologic treatments). Early transfer is especially important when nonconvulsive status epilepticus is suspected or there is lack of access to routine and serial EEG given the morbidity and mortality associated with prolonged status epilepticus (8). See Figure 1 for a proposed algorithm for identification and early transfer (13, 17).
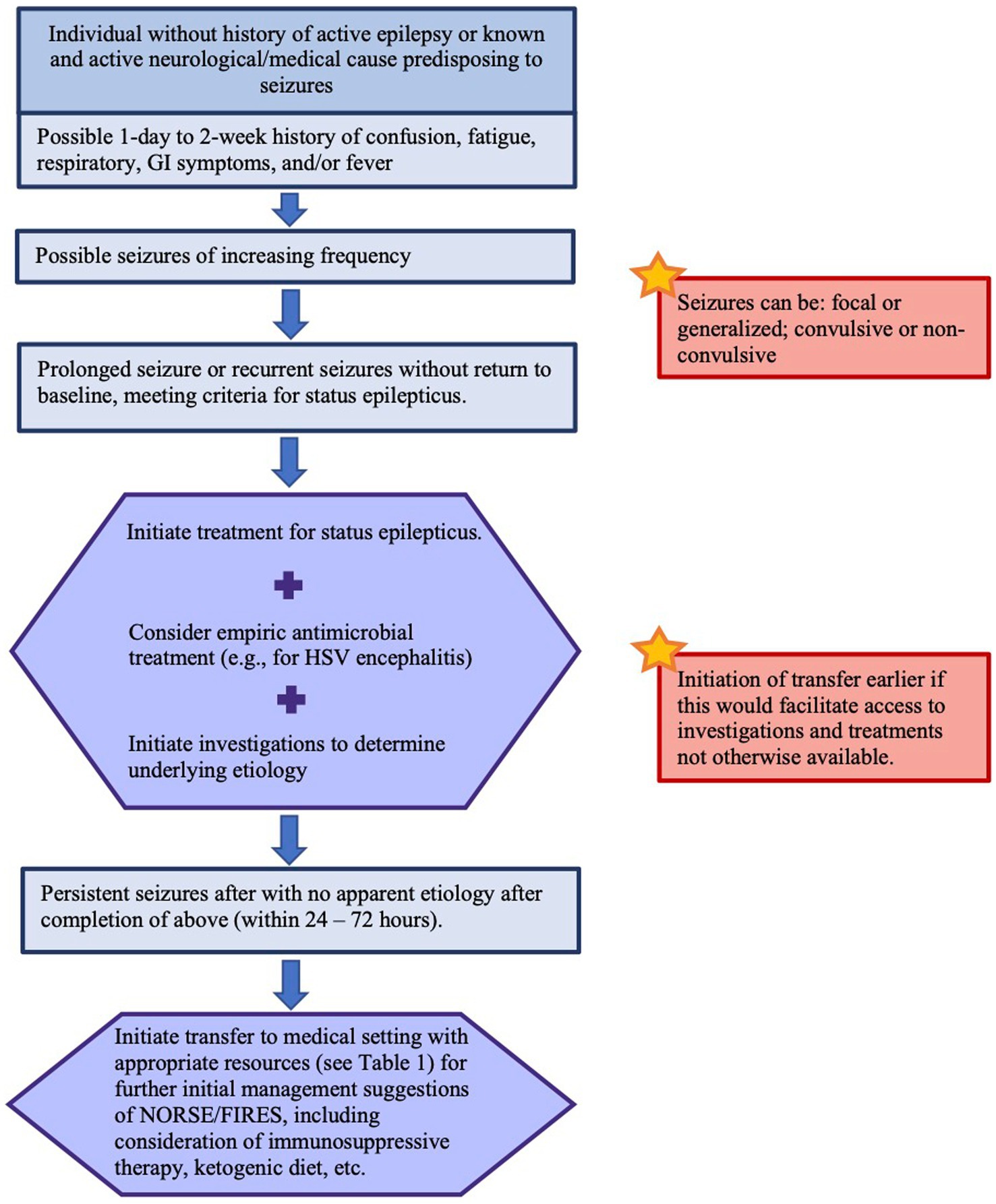
Figure 1. Proposed algorithm for recognition of NORSE/FIRES and transfer to a medical setting with appropriate resources. Please refer to reference (13) for details on recommended management of status epilepticus. Please refer to references (17, 20) for detailed recommendations on investigations and management of NORSE/FIRES.
5. Conclusion
Overall, early identification of NORSE and associated conditions such as FIRES is essential to initiate appropriate investigations and management. Optimal patient care involves a multidisciplinary approach and numerous investigations and treatments. We advocate for early transfer to a specialized center with these resources with the aim of mitigating the known risks and downstream complications of NORSE. These recommendations pertain to adult patients as pediatric patients may require additional special considerations.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
HK conceived this manuscript and oversaw direction and planning. SV wrote the first draft of this manuscript in consultation with HK and GY. All authors contributed to the content of this manuscript and were involved in editing this work.
Funding
This work was supported by the University of Toronto.
Acknowledgments
We acknowledge support of the NORSE Institute for raising awareness and developing resources for families and healthcare providers.
Conflict of interest
The authors declare that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hirsch, LJ, Gaspard, N, van Baalen, A, Nabbout, R, Demeret, S, Loddenkemper, T, et al. Proposed consensus definitions for new-onset refractory status epilepticus (NORSE), febrile infection-related epilepsy syndrome (FIRES), and related conditions. Epilepsia. (2018) 59:739–44. doi: 10.1111/epi.14016
2. Trinka, E, Cock, H, Hesdorffer, D, Rossetti, AO, Scheffer, IE, Shinnar, S, et al. A definition and classification of status epilepticus -report of the ILAE task force on classification of status epilepticus. Epilepsia. (2015) 56:1515–23. doi: 10.1111/epi.13121
3. Kantanen, A, Reinikainen, M, Parviainen, I, and Kälviäinen, R. Long-term outcome of refractory status epilepticus in adults: a retrospective population-based study. Epilepsy Res. (2017) 133:13–21. doi: 10.1016/j.eplepsyres.2017.03.009
4. Leitinger, M, Trinka, E, Giovannini, G, Zimmermann, G, Florea, C, Rohracher, A, et al. Epidemiology of status epilepticus in adults: a population-based study on incidence, causes, and outcomes. Epilepsia. (2019) 60:53–62. doi: 10.1111/epi.14607
5. Gaspard, N, Foreman, BP, Alvarez, V, Kang, CC, Probasco, JC, Jongeling, AC, et al. New-onset refractory status epilepticus: etiology, clinical features, and outcome. Neurology. (2015) 85:1604–13. doi: 10.1212/WNL.0000000000001940
6. Gaspard, N, Hirsch, LJ, Sculier, C, Loddenkemper, T, van Baalen, A, Lancrenon, J, et al. New-onset refractory status epilepticus (NORSE) and febrile infection–related epilepsy syndrome (FIRES): state of the art and perspectives. Epilepsia. (2018) 59:745–52. doi: 10.1111/epi.14022
7. Rossetti, AO, Logroscino, G, Milligan, TA, Michaelides, C, Ruffieux, C, and Bromfield, EB. Status epilepticus severity score (STESS). J Neurol. (2008) 255:1561–6. doi: 10.1007/s00415-008-0989-1
8. Sutter, R, Semmlack, S, Kaplan, PW, Opić, P, Marsch, S, and Rüegg, S. Prolonged status epilepticus: early recognition and prediction of full recovery in a 12-year cohort. Epilepsia. (2019) 60:42–52. doi: 10.1111/epi.14603
9. Hawkes, MA, and Hocker, SE. Systemic complications following status epilepticus. Curr Neurol Neurosci Rep. (2018) 18:1–9. doi: 10.1007/s11910-018-0815-9
10. Gofton, TE, Gaspard, N, Hocker, SE, Loddenkemper, T, and Hirsch, LJ. New onset refractory status epilepticus research: what is on the horizon? Neurology. (2019) 92:802–10. doi: 10.1212/WNL.0000000000007322
11. Wong, NW. The role of Hope, compassion, and uncertainty in Physicians' reluctance to initiate palliative care. AMA J Ethics. (2018) 20:E782–6. doi: 10.1001/amajethics.2018.782
12. Gofton, TE, Wong, N, Hirsch, LJ, and Hocker, SE. Communication Challenges: A Spotlight On New-onset Refractory Status Epilepticus. Mayo Clinic Proceedings: Elsevier (2019).
13. Glauser, T, Shinnar, S, Gloss, D, Alldredge, B, Arya, R, Bainbridge, J, et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the guideline Committee of the American Epilepsy Society. Epilepsy currents. (2016) 16:48–61. doi: 10.5698/1535-7597-16.1.48
14. Neligan, A, Kerin, B, Walker, MC, and Rajakulendran, S. New-onset refractory status epilepticus (NORSE): the Queen square neuro-ICU experience. Epilepsy Behav. (2021) 125:108387. doi: 10.1016/j.yebeh.2021.108387
15. Alvarez, V, and Drislane, FW. Is favorable outcome possible after prolonged refractory status epilepticus? J Clin Neurophysiol. (2016) 33:32–41. doi: 10.1097/WNP.0000000000000223
16. Kilbride, RD, Reynolds, AS, Szaflarski, JP, and Hirsch, LJ. Clinical outcomes following prolonged refractory status epilepticus (PRSE). Neurocrit Care. (2013) 18:374–85. doi: 10.1007/s12028-013-9823-4
17. Sculier, C, and Gaspard, N. New onset refractory status epilepticus (NORSE). Seizure. (2019) 68:72–8. doi: 10.1016/j.seizure.2018.09.018
18. Brophy, GM, Bell, R, Claassen, J, Alldredge, B, Bleck, TP, Glauser, T, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. (2012) 17:3–23. doi: 10.1007/s12028-012-9695-z
19. Gaspard, N, Sculier, C, Hirsch, LJ, Hocker, S, Sheikh, Z, Ghoshal, S, et al. NORSE (including FIRES) diagnostic evaluation. (2020) Available at: norseinstitute.org.
20. Wickstrom, R, Taraschenko, O, Dilena, R, Payne, ET, Specchio, N, Nabbout, R, et al. International consensus recommendations for management of new onset refractory status epilepticus (NORSE) including febrile infection-related epilepsy syndrome (FIRES): summary and clinical tools. Epilepsia. (2022) 63:2827–39. doi: 10.1111/epi.17391
Keywords: NORSE, FIRES, status epilepticus, epilepsy, neurocritical care
Citation: Vinette SA, Young GB and Khosravani H (2023) Early identification of NORSE and transfer to care setting with appropriate supports: A proposed algorithm. Front. Neurol. 14:1072020. doi: 10.3389/fneur.2023.1072020
Edited by:
Aljoscha Thomschewski, University Hospital Salzburg, AustriaReviewed by:
Ruzica Kravljanac, The Institute for Health Protection of Mother and Child Serbia, SerbiaCopyright © 2023 Vinette, Young and Khosravani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Houman Khosravani, aC5raG9zcmF2YW5pQHV0b3JvbnRvLmNh
 Sarah A. Vinette
Sarah A. Vinette Gordon Bryan Young2
Gordon Bryan Young2 Houman Khosravani
Houman Khosravani