- 1School of Clinical Medicine, Beijing University of Chinese Medicine, Beijing, China
- 2Department of Acupuncture and Moxibustion, Beijing Hospital of Traditional Chinese Medicine, Capital Medical University, Beijing Key Laboratory of Acupuncture Neuromodulation, Beijing, China
- 3Department of Radiology, Dong Zhimen Hospital Beijing University of Chinese Medicine, Beijing, China
- 4Department of Psychology, University of Chinese Academy of Sciences, Beijing, China
- 5Peking University Third Hospital, Research Centre of Clinical Epidemiology, Beijing, China
Introduction: Acupuncture is an effective treatment in migraine without aura (MWoA), but the neurological mechanism has not been investigated using multimodal magnetic resonance imaging (MRI). This trial will combine functional MRI, structural MRI, and diffusion tensor imaging to explore the potential neural mechanism of acupuncture on MWoA, and will use machine learning approach to predict acupuncture treatment effects.
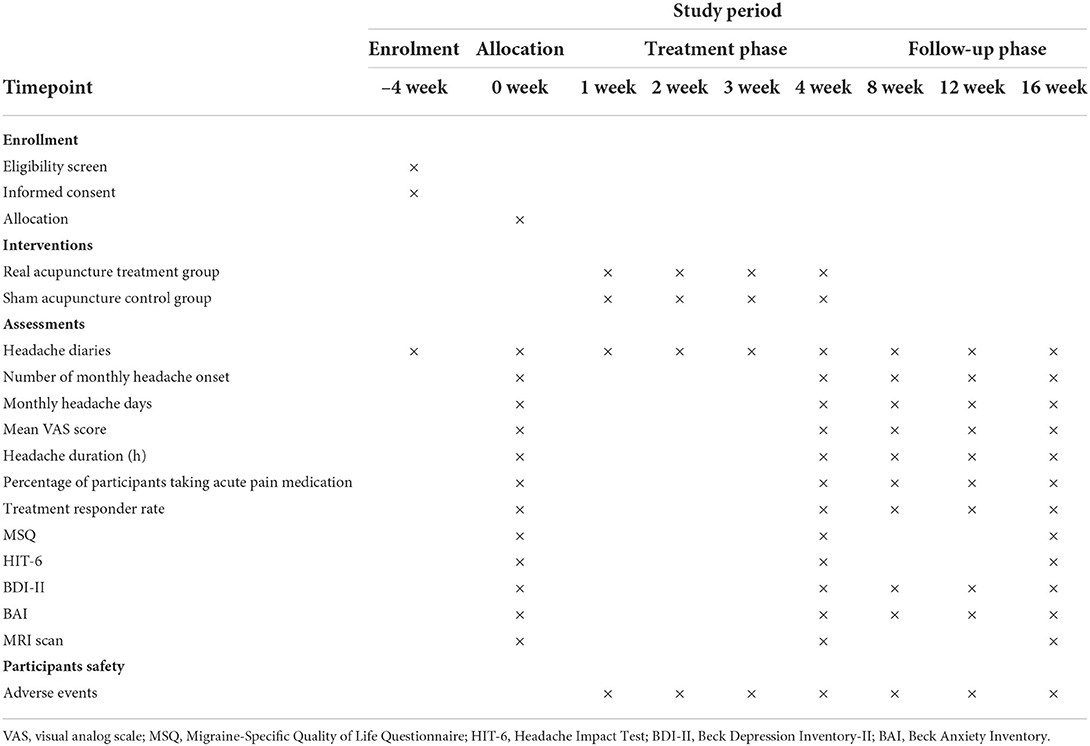
Methods: In this multimodal neuroimaging randomized controlled trial, a total of 60 MWoA participants will be randomly allocated to two groups: the real acupuncture treatment group and the sham acupuncture control group. This trial will include a 4-week baseline phase, a 4-week treatment phase, and a 12-week follow-up phase. Participants will undergo 12 acupuncture or sham acupuncture sessions during the treatment phase. The Headache Diary, Migraine-Specific Quality of Life Questionnaire, Headache Impact Test, Beck Depression Inventory-II, and Beck Anxiety Inventory will be utilized to evaluate the clinical efficacy. Multimodal MRI scans will be employed to investigate the mechanism of acupuncture at baseline, at the end of treatment, and after follow-up. Multimodal MRI data will be used to predict acupuncture treatment effects using machine learning technology.
Discussion: This study hypothesized that acupuncture therapy may treat MWoA by restoring the neuropathological alterations in brain activity. Our finding should provide valuable scientific proof for the effects of acupuncture and demonstrate the usefulness of acupuncture in the treatment of MWoA. Moreover, acupuncture response prediction might decrease healthcare expenses and time lags for patients.
Trial registration number: [ChiCTR2100044251].
Introduction
Migraine is a debilitating condition characterized by episodic or chronic headaches and physiological and emotional stressors (1, 2) that represents an important healthcare and social problem (3, 4). Migraine is a recurrent brain function disorder that affects approximately one billion individuals worldwide, from all geographies, ethnicities, and socio-economic backgrounds (5, 6). The 1-year prevalence of migraine is reported to be 15% globally, being the greatest in Southeast Asia (25–35%), and the lowest in China (9%) (7, 8).
The current armamentarium of treatment options includes acute, preventive, and non-pharmacological therapies. Acupuncture is traditionally used as a non-pharmacological therapy to treat various symptoms and diseases. Acupuncture is widely used for its analgesic benefits due to its effectiveness and safety (9). There is moderate evidence for acupuncture being at least non-inferior to conventional drug therapy (e.g., flunarizine, metoprolol) for episodic migraine prevention (10, 11). A recent study compared acupuncture with the most appropriate medication for each patient, which came out a conclusion that for migraine prophylaxis, acupuncture is just as successful as the suitable pharmaceutical therapy (12). However, acupuncture's clinical effects have been challenged on the basis that some of its effects may relate to psychological or ‘placebo’ mechanisms. Fortunately, plenty clinical evidence suggests that real acupuncture is superior to sham acupuncture in migraine, reflected by a higher total effective rate and decreased recurrence rate (13). Two previous meta-analyses recommended acupuncture for the prevention of episodic migraine (10, 14). Acupuncture is also recommended by guidelines in many countries for the management and therapy of migraine (15–21).
Due to the wide applications, growing attention has been paid to discovering rational explanations for the complicated neurophysiological mechanisms of acupuncture. Acupuncture has been proven in several studies to change a number of neurophysiological factors related to analgesia, which are considered to reduce or modulate pain perception and physiological processes (10). In addition, acupuncture has been proved to participate in the development of peripheral and central sensitization through modulation of the release of related mediators and serotonin system activation (22–24). Neuroimaging studies also have indicated that acupuncture could alter the abnormal functional activity and connectivity of the descending pain modulatory system, default mode network, and several related subcortical areas (25–27). Nevertheless, the complicated neurophysiological mechanisms of acupuncture for migraine prevention should be investigated independently (28). Moreover, no research have been conducted to investigate the mechanism underlying acupuncture's efficacy on migraine without aura (MWoA) using multimodal magnetic resonance imaging (MRI), which combines functional MRI (fMRI), structural MRI (sMRI), and diffusion tensor imaging (DTI).
Although acupuncture is used to treat migraine across many countries (9, 10, 29–34), approximately 50% of the migraineurs do not obtain significant relief following acupuncture (33, 34). The capacity to predict the effects of acupuncture could save the non-responders from having to suffer extended periods of ineffective therapy. Our group's most recent study used baseline brain gray matter volume as a predictor of acupuncture outcomes in migraine treatment (35). The machine learning classification approach is increasingly being implemented to identify patient subgroups or to predict responders and non-responders with certain therapies (36–38), giving a new paradigm for personalized therapeutic strategies.
Hence, we designed this multimodal brain imaging trial with three aims: (1) to re-evaluate the efficacy of acupuncture treatment for MWoA by comparing real acupuncture with sham acupuncture, (2) to investigate the promising neural mechanism of acupuncture for MWoA by integrating multimodal MRI, and (3) to apply machine learning approach to predict the effects of acupuncture on MWoA.
Methods
Study design
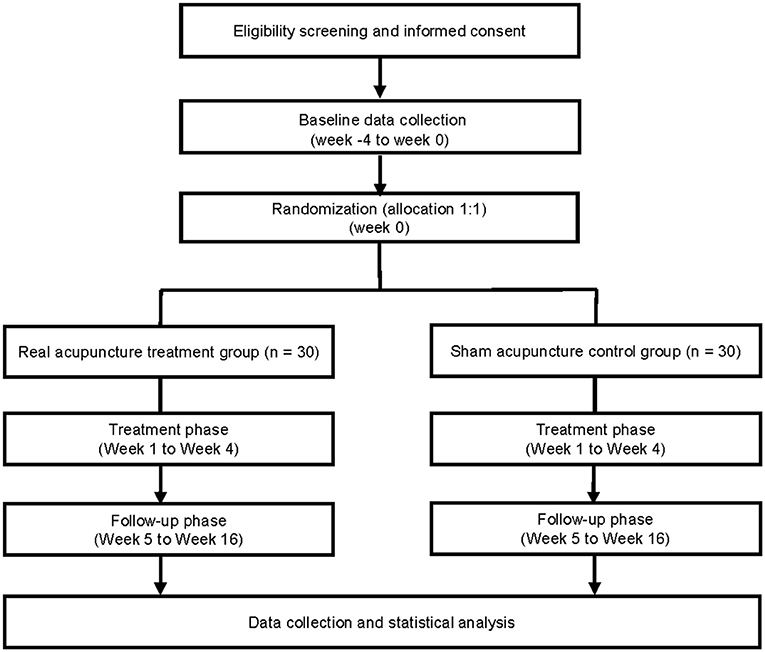
This trial was designed to evaluate the treatment effect and neurological mechanism of acupuncture in MWoA. Our study will be conducted as a 1:1 randomized, single-blinded, and sham-controlled study. Sixty participants diagnosed with MWoA will be considered eligible. They will be randomly assigned to two groups with 30 participants each. The real acupuncture treatment group will receive real acupuncture, whereas the sham acupuncture control group will undergo sham acupuncture. Pain, neuropsychological questionnaires, and multimodal MRI evaluation will be performed at baseline, after the treatment, and during the follow-up phase. This study will consist of three phases: (i) a 4-week screening phase (week−4 to week 0); (ii) a 4-week treatment phase (weeks 1–4), and (iii) a 12-week follow-up phase (weeks 5–16). At baseline, participants will be assessed via headache diaries, the Migraine-Specific Quality of Life Questionnaire (MSQ), Headache Impact Test (HIT-6), Beck Depression Inventory-II (BDI-II), Beck Anxiety Inventory (BAI), and multimodal MRI scans. The enrollment schedules, interventions, and assessments are summarized in Table 1, and a study flowchart is presented in Figure 1.
This trial will be reported following the Standard Protocol Items: Recommendations for Intervention Trials (SPIRIT) guidelines (39) (Supplementary material) and will follow the Consolidated Standards of Reporting Trials (CONSORT) (40) and the Standards for Reporting Interventions in Clinical Trials of Acupuncture principles (STRICTA) (41).
Recruitment
The researchers will recruit trial participants with MWoA from outpatient clinics at the Acupuncture and Moxibustion Department of the Beijing Hospital of Traditional Chinese Medicine, Capital Medical University. A certified neurologist (LL) will perform the diagnosis of MWoA and exclude other types of headaches or diseases based on syndromes and accessory examinations. To promote recruitment, advertisements will be posted in the hospital. The recruitment advertisement for the study will also be posted in the public account of WeChat of our hospital. For comparison with the MRI data analysis, 30 age- and sex-matched healthy controls will be recruited to receive a multimodal MRI scan. Researchers who are not involved in the treatment process will conduct the entire recruitment procedure.
Participants will be explained the purpose and nature of the study protocol. Written informed consent will be obtained from all the participants. Each participant will be informed of the random allocation of real acupuncture or sham acupuncture, and the potential benefits and risks. They will voluntarily sign an informed consent form prior to enrollment. Participants will be able to withdraw from this research at any time, without penalty or loss of benefits, and without having to give a reason. Meanwhile, we will endeavor to record the reason for withdrawal.
Participants
Inclusion criteria for patients with MWoA
The inclusion criteria will be as follows: (1) patients that fulfill the diagnostic criteria of the International Classification of Headache Disorders, 3rd edition for MWoA (33); (2) a migraine history of at least 1 year before study entry; (3) having experienced at least two migraine attacks in the preceding 4 weeks; (4) aged between 18 and 65 years, right-handed; (5) not having received treatments like acupuncture or pharmacological medicine (e.g., paracetamol, triptans, amitriptyline, beta-blockers, topiramate, valproic acid, or anti-GCRP monoclonal antibodies) in the 3 months before enrollment; (6) able to complete a headache diary.
Exclusion criteria for patients with MWoA
We will exclude patients with (1) chronic migraine, tension-type headache, cluster headache, or other primary headaches; (2) secondary headache caused by otorhinolaryngological diseases or intracranial pathological changes; (3) relatively severe systemic diseases (e.g., angiocardiopathy, cerebrovascular disease, hepatopathy, nephropathy, acute infectious disease, hematopathy, endocrinopathy, allergy, or methysis); (4) pregnancy, lactation, or insufficient contraception; (5) psychiatric or neurological disorders (e.g., major depressive disorder, schizophrenia, bipolar disorder, traumatic brain injury, stroke, Parkinson's disease); or (6) MRI contraindications (e.g., claustrophobia, cardiac pacemaker, or other metallic objects implanted in the body).
Inclusion criteria for healthy controls
The group of healthy controls will consist of participants (1) aged 18 to 65 years, right-handed; (2) with no personal or familial history of migraine, and (3) who agree to participate in this study voluntarily and to sign an informed consent form.
Exclusion criteria for healthy controls
(1) Relatively severe systemic diseases (e.g., angiocardiopathy, cerebrovascular disease, hepatopathy, nephropathy, acute infectious disease, hematopathy, endocrinopathy, allergy, or methysis) (2) pregnancy, lactation, or insufficient contraception (3) psychiatric or neurological disorders (e.g., major depressive disorder, schizophrenia, bipolar disorder, traumatic brain injury, stroke, Parkinson's disease), or (4) MRI contraindications (e.g., claustrophobia, cardiac pacemaker, or other metallic objects implanted in the body).
Randomization and allocation concealment
Block randomization will be employed to achieve a balance between the two groups, with a block size of four. Predetermined, sequentially numbered, opaque, and sealed envelopes will be produced by a third-party professional statistician (LZe) from the Epidemiology Research Center of Peking University Third Hospital using the PROC PLAN of Statistical Analysis System (SAS) 9.4 software (SAS Institute Inc., Cary, NC, USA) to avoid subjective bias from the researchers. Each sealed envelope will be numbered sequentially and kept secure until the trial is finished.
An independent assistant will separate and unseal each envelope from the strain in the sequence corresponding to the participant's screening order and will then assign eligible participants to the real acupuncture treatment group or the sham acupuncture control group. The assistant will not be involved in the baseline or outcome assessments. The treatment allocation results will be forwarded to the acupuncturist by this assistant. With the exception of the acupuncturist and the assistant who unsealed the envelopes, neither the participants nor the other researchers will be aware of group allocation.
Blinding
During the trial, participants will not be told which treatment they will receive: real acupuncture or sham acupuncture. To eliminate meaningful communication between the two groups during treatment, participants will receive acupuncture therapy in consulting rooms with compartments. Therefore, participants will be blinded to the treatment allocation. The acupuncturist will not be blinded to the group allocation; they will be unable to disclose the type of treatment.
Furthermore, outcome assessors, MRI scanners, and statisticians will be blinded to the treatment allocation of the participants throughout the trial. To avoid outcome assessors and statisticians from identifying that how participants are allocated, the labels of the real acupuncture treatment group and the sham acupuncture control group will be substituted with non-sensical letter combinations. Unblinding will be performed only after the trial finishes except if the participant has an adverse event suspected to be related to the acupuncture treatment (42).
The credibility of the blinding will be assessed at the end of the treatment phase (week 4). An investigator who is not engaged in the participant allocation or the therapy administration will examine the credibility of the participants' blinding.
Intervention
Real acupuncture treatment group
Participants in this group will obtain manual acupuncture at eight real acupoints (bilateral Fengchi [GB20], Fengfu [GV16], Baihui [GV20], bilateral Taiyang [EX-HN5], and bilateral Hegu [LI4]) (Figure 2) (Supplementary material) with disposable single-use sterile needles (0.25 × 25 mm, Ande Medical Instrument Co., Ltd., China). According to records in ancient and modern books, real acupoints have been proven effective and crucial, the suggestion of consensus meetings with clinical experts, and the results of our previous research on acupuncture treatment for MWoA (34). The positioning of acupoints will be determined according to the standards issued by the World Health Organization in 2010 (43). Needles will be inserted into acupoints at a depth of 10–15 mm following skin disinfecting with alcohol; the acupuncturist will twist the needles by 90–180°, lifting and thrusting needles with an amplitude of 3–5 mm to generate a deqi sensation. After achieving deqi sensation, the needles will be held at the acupoints for 30 min. The foregoing procedures will be manipulated for 10–15 s every 10 min to sustain the deqi sensation. Participants will obtain a total of 12 sessions of acupuncture treatment for 4 weeks, with three sessions per week.
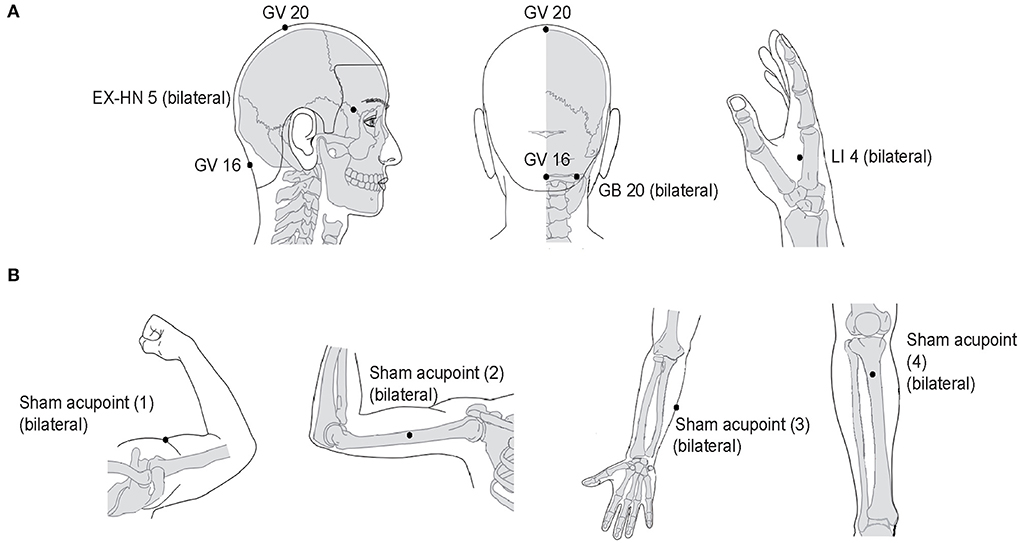
Figure 2. Location of real acupoints and sham acupoints. (A) Real acupoints. (B) Sham acupoints. EX-HN, Extrachannel points; GB, Gallbladder Meridian; GV, Governor Vessel; LI, Large Intestine Meridian.
Sham acupuncture control group
This group will obtain superficial skin penetration at eight sham acupoints. To minimize physiological effects, these sham acupoints do not correspond to any known meridian and are not conventional acupoints according to previous studies (44, 45). The sham acupoint locations are shown in Figure 2 (Supplementary material). Superficial skin penetration at sham acupoints, without needle manipulation for deqi sensation, is a common sham acupuncture control applied in many randomized controlled trials (46). Participants in sham group will receive an acupuncture procedure similar to that received by the participants in the real acupuncture treatment group. Additionally, the number and size of sterile steel needles for each treatment session will be the same as in the real acupuncture treatment group.
The same acupuncturist will perform therapy to minimize the bias caused by the different personal practices of the acupuncturists. The acupuncturist is a practicing physician licensed by the Ministry of Health of the People's Republic of China. The acupuncturist has more than five years of clinical experience. Before the commencement of the study, the acupuncturist will undergo specific training on the trial's purpose and standardized procedures, therapeutic interventions, and quality management.
The participants' weekly acupuncture times and compliance will be recorded in detail in case report forms (CRFs). Moreover, the number of acupuncture treatments received by each participant will be counted to monitor patient adherence.
Concomitant medication
Patients will be instructed to avoid taking medications as much as possible during the trial. According to principles of medical ethics, if the participants' migraine symptoms do not improve considerably, and they are unable to endure migraine attack, ibuprofen may be temporarily prescribed. Ibuprofen (300 mg per capsule with sustained release) will be recommended to all participants as their first option for acute medication. Except for ibuprofen, no drugs will be taken in this study. Researchers will record the name, dose, and time of the drugs taken in headache diaries and CRFs.
Multimodal data acquisition
All participants will receive an MRI scan in the Department of Radiology, Dong Zhimen Hospital Beijing University of Chinese Medicine, after providing their informed consent. MRI data will be obtained with a 3.0 Tesla superconductor (Siemens Magnetom Verio, Erlangen, Germany). Participants in both the real acupuncture treatment group and sham acupuncture control group will be scanned before randomization, at the end of treatment, and after the follow-up phase. In contrast, healthy controls will be scanned after recruitment. Given the possibility of variations associated with the menstrual cycle, female participants will be assessed outside the premenstrual or menstrual phases. All participants will undergo the MRI during the headache-free interval (not within 48 h after the last migraine attack). During scanning, the participants will be required to lie on their backs in the scanner. A headrest will be used to hold the head to prevent head movements from affecting the image, and a 16-channel head coil will be fixed on both sides of the headrest. They will be instructed to stay awake, relax, and not think of anything during the entire brain scan, with their ears plugged to attenuate the gradient noise. During fMRI scanning, participants will be instructed to view a centrally placed fixation cross (+), and during T1 and DTI scanning, they will be allowed to close their eyes and relax. Furthermore, the MRI scan will be conducted by the same technician (YZhu) using the same machine, and a professional staff member (ZT) will review the images for quality and procedure compliance after each scan. Both of them are highly qualified radiologists skilled in MRI.
First, the scanning procedure produces a T1-weighted structural image (repetition time (TR)/echo time (TE) = 2,000/3.51 ms, slice thickness = 1.00 mm, slice number =192, field of view (FOV) = 256 × 256 mm, flip angle = 8°, matrix size = 256 × 256) for standard space co-registration. Second, a T2*-weighted gradient-echo (GE) blood oxygenation level-dependent (BOLD) sequence will be recorded (TR/TE = 2,420/30 ms, slice thickness = 3.0 mm, slice number = 44, FOV = 192 × 192 mm, flip angle = 90°, matrix size = 64 × 64) to obtain fMRI data. Third, a DTI sequence (TR/TE, 12,700/91 ms; slice thickness = 2.0 mm, slice number = 64, FOV = 192 × 192 mm; matrix size = 96 × 96) will be used to collect connectivity information (Supplementary material). Scanning will be terminated if the participant complains of discomfort. A professional staff member (ZT) will check the images qualitatively to detect for any brain lesions or structural abnormalities.
Outcome measures
Primary outcome measure
The primary outcome is the change in the number of monthly headache onsets from week 0 to week 4.
Secondary outcome measures
The secondary outcome measures are as follows: (1) change in the number of monthly headache onsets from week 0 to week 16; (2) change in monthly headache days (MMDs); (3) change in visual analog scale (VAS) score of headache attack intensity; (4) change in headache duration (h); (5) percentage of participants taking acute pain medication; (6) treatment responder rate (the proportion of participants with ≥50% reduction in the number of monthly headache onsets); (7) change in MSQ (8, 39), change in HIT-6 (9, 40), change in BDI-II (10, 41), and change in BAI (47). These outcome measures will be repeatedly assessed at weeks 0, 4, and 16 by a researcher who is blinded to participant allocation. Additionally, the BDI-II and BAI will be repeatedly assessed at weeks 8 and 12. Neuropsychological and others assessment scales will be conducted by the researcher in a quiet room. To guarantee consistency, the same researcher will perform all the outcome assessments.
Headache diaries
A headache diary was verified in a previous study (48). In the headache diary, the participants will document each headache onset in detail, including attack frequency, migraine duration, migraine days, pain characteristics, pain intensity, location, inductions of headaches, concomitant symptoms (nausea, vomiting, photophobia, and phonophobia), aggravation by/causing avoidance of routine physical activity (walking or climbing stairs), precipitating factors, and acute medications. Pain intensity will be evaluated using a VAS (0 to 10).
HIT-6
HIT-6 assesses six headache-related domains affected, including pain, social functioning, role functioning, vitality, cognitive functioning, and psychological stress, and is designed to offer a global evaluation of the negative impact of headaches (49, 50). The six questions are assigned a point value of 6, 8, 10, 11, or 13 based on five questionnaire items that indicate how frequently headaches disrupt with daily activities or induce stress (never, rarely, sometimes, very often, or always). The total score ranges from 36 to 78, with higher scores indicating higher levels of headache impact. A previous study confirmed that HIT-6 is a robust and accurate measure for differentiating headache impact between episodic and chronic migraines (51).
MSQ
The 14-item MSQ is a patient-reported outcome instrument that assesses the impact of migraine across three domains (52, 53): the role restrictive (MSQ-RR), the role preventive (MSQ-RP), and the emotional functioning (MSQ-EF). Items are assigned scores of one to six (none of the time, a little bit of the time, some of the time, a good bit of the time, most of the time, and all of the time). Raw domain scores are calculated as a sum of 14-item and rescaled from a 0 to 100-point scale, with higher scores indicating better quality of life. The MSQ is a reliable and accurate assessment that could distinguish between the functional effect of chronic and episodic migraine in the chronic migraine population (54).
BDI-II
The BDI-II is a 21-item self-report scale that evaluates the depression severity (55–57). Its contents is compatible with the diagnostic criteria for major depressive disorder (MDD) in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (58). Items are graded on a four-point Likert scale ranging from zero to three, and the total score ranges from 0 to 63, with higher scores indicating higher levels of depression. The scale's features include its sufficient internal consistency, content reliability and worldwide dissemination (59).
BAI
The BAI is a 21 item self-report scale used to evaluate anxiety severity. This inventory was published in the USA by Beck in 1988 and is an anxiety assessment which has been carefully constructed to minimize misunderstanding with depression (60). The BAI examines affective, cognitive, and somatic components of anxiety. Items are rated from zero (not at all) to three (severely) depending on the severity of anxiety symptoms. The maximum total score is 63, with higher scores indicating greater anxiety. The BAI could be used as an effective assessment approach to determine between people who have and do not have panic disorder (61).
MRI outcome measures
This trial will concentrate on the following MRI indicators (week 0, week 4, and week 16): (1) fMRI: amplitude of low-frequency fluctuation (ALFF), regional homogeneity (ReHo), independent component analysis (ICA)-based functional connectivity (FC), seed-based FC, degree centrality (DC), (2) sMRI: voxel-based whole-brain voxel-mirrored homotopic connectivity (VMHC), cortical thickness, gray matter volume (GMV), white matter volume (WMV), total brain volume (TBV), (3) DTI: mean diffusivity (MD), radial diffusivity (RD), axial diffusivity (AD), and fractional anisotropy (FA).
Safety assessments
Adverse events (AEs) are unintentional injuries or complications following intervention. At each visit, participants will be asked to disclose any aberrant responses or uncomfortable feelings experienced to the researchers. To evaluate the risks associated with acupuncture, any AEs will be tracked and documented in the CRFs. Needle-related AEs include needle sticking, bleeding, hematoma, subcutaneous hemorrhage, serious pain, dizziness, local infection, neurological symptoms, and fainting (62). All unexpected AEs will be recorded in detail in the CRFs, including the time of occurrence (transient or persistent), severity of AEs (mild, moderate, or serious), and possible causes (needle-related or non-needle-related) by participants and outcome assessors. All AEs will be systematically collected via semi-structured and open-ended questionnaires and categorized by acupuncturists and neurologists within 24 h (63). Different types of AEs occurring in one participant will be classified as independent AEs. One type of AE with multiple occurrences in each participant will be classified as one AE. Disagreements will be resolved through discussion and consensus.
Participants experiencing mild to moderate AEs will be treated immediately and constantly monitored by the attending acupuncturist. In the case of serious AEs, the research team will immediately provide medical advice to the participant within 48 h. Serious AEs shall be presented within 24 h to the principal investigator and the research ethics committee. AEs will be tracked until they are properly resolved. The research ethics committee will decide whether the trial should be terminated.
Data management and monitoring
Clinical information from participants will be recorded using a CRF and headache diaries, which will be labeled with a specific number identification and documented by a researcher. A research assistant will check the clinical information for completeness, reliability, and consistency. Clinical information from the CRF and headache diaries will be entered into the EpiData database. Double data entry and validation will be performed by two investigators for reducing data input errors, and value pairs will be reviewed for discrepancies by referring to the paper-based source.
All CRFs and original paper-based data will be safely stored in locked filing cabinet. Electronic files will be saved in a password lock computer with restricted assessed to our study team members. Essential documents will be stored for a minimum of 5 years after the last publication. Additionally, the Center for Advancing Quality in Clinical Research of Beijing Hospital of Traditional Chinese Medicine will monitor the trial to assure enrollment rate, data accurateness and reliability.
Sample size calculation
There is no acknowledged standard for estimating sample size in neuroimaging research. According to the demands of neuroimaging research (64, 65) and similar previous research (66, 67), a sample size of 12–26 persons in each group is an appropriate sample size for data processing. Desmond et al. found that a sample of 25 participants in each group are required to keep 80% power after multiple comparisons, and this power calculations were performed through the simulation-based method for group-level fMRI studies (68). In sum, a sample of 30 participants in each group is deemed acceptable to account for 10–20% participants dropout and incorrect images owing to head movements in this study.
Retention strategies for participant engagement
The dropout is a critical determinant of results in acupuncture clinical trials, due to its time costing, more complicated procedure and even fear of needling (69). To avoid high dropout rate, we applied a flexible treatment timetable and personally illustration of acupuncture needle and effect from our senior investigator (70). However, participants will still be able to withdraw from this research at any time, and with or without any reason.
Statistical analysis
Clinical data analysis
The analyses will be completed using Statistical Package for Social Science (SPSS) for Windows (version 22.0) by statisticians blinded to the group allocation and treatment procedure. The statisticians involved in the study are affiliated to the Research Center of Clinical Epidemiology, Peking University Third Hospital. All statistical analyses will be based on the intention-to-treat principle. The ITT principle in this trial will be comprised of all allocated participants who receive at least one treatment and have a complete baseline assessment. The last observation carried forward approach will be used to fill the missing data from participants who drop out. Next, the per-protocol principle will be used for sensitivity analyses, including all randomized participants who complete all the treatment and have MRI scans. The histograms, normal probability plots and a Shapiro-Wilk test will be conducted to evaluate the normality of the data. Standard deviations, and 95% confidence intervals will be calculated using the distributed data. All hypothesis tests will be two-tailed analyses with statistical significance defined as p-value <0.05.
The study will report the median (interquartile range) or mean ± standard deviation for continuous variables, and numbers (percentages) for categorical variables. The chi-square and Fisher exact tests will be performed to compare dichotomous variables. The independent two-sample t-test or Wilcoxon rank-sum test will be performed for normally or non-normally distributed continuous variables. A linear mixed-effects model will also evaluate multivariate-adjusted treatment effects across groups. Furthermore, we will take sex, age, and baseline migraine days as covariates and conduct a mixed-effects model to avoid the influence of these factors on the results.
MRI data analysis
An independent MRI analyst (LZha), who is not involved in the enrollment or assessment of participants, will perform the MRI data analysis. First, the fMRI data will be preprocessed and analyzed using FMRIB Software Library (FSL; http://fsl.fmrib.ox.ac.uk/fsl), Analysis of Functional NeuroImages (AFNI; http://afni.nimh.nih.gov/afni), and FreeSurfer (http://surfer.nmr.mgh.harvard.edu/). The sMRI data will then be analyzed using the voxel-based morphometry (VBM) toolbox within Statistical Parametric Mapping 12 (SPM12; http://www.fil.ion.ucl.ac.uk/spm), and the DTI data will be processed using FSL. Pearson's correlation between the changes in brain activity and improvement in clinical outcomes will be calculated in each group.
Brain connectivity analyses
T2*-weighted BOLD images will be preprocessed, including cardiorespiratory artifact correction (AFNI, RETRO-ICOR), head motion correction (FSL, MCFLIRT), and brain extraction (FSL, BET). Cortical surface reconstruction will be completed to improve structural-functional co-registration using boundary-based registration (FreeSurfer, bbregister). Functional data will then be registered to the MNI (Montreal Neurological Institute) space (FSL, FNIRT). Spatial smoothing and high-pass temporal filtering will also be applied. After the preprocessing procedure, different analytical methods will be used to examine the neural response, including ALFF, ReHo, seed-based FC, and ICA-based FC. These are the most common analysis indicators in fMRI that reflect the functional activity of the brain (71, 72).
VBM analysis
T1-weighted structural MRI data will be used in the SPM-based VBM analysis. Non-uniformity correction, tissue classification, and image registration will be incorporated in a generative model. The Diffeomorphic Anatomical Registration Through Exponentiated Lie Algebra (DARTEL) toolbox will be performed to generate normalized images, and then brain tissue will be segmented into gray matter, white matter (73). The normalized data will be smoothed and registered to the MNI space. Different analytical methods will be used in the trial, including DC, VMHC, cortical thickness, GMV, WMV, and TBV, to measure differences in the brain structure of participants (74).
DTI analysis
The Brain Extraction Tool (BET) in FSL will be conducted for brain extraction. Then, the eddy current distortion and head motion will be rectify using FMRIB's Diffusion Toolbox (FDT). FA, MD and L1, L2, and L3 eigenvalue maps will be calculated by fitting a tensor model using FDT. These FA images will be non-linearly registered to the FMRIB58-FA standard-space template and aligned to the MNI space. Different analytical methods will be used in the trial, including AD, FA, MD, and RD. These indices could be used to assess the cerebral structure's integrity and connection (75).
Predict treatment response from baseline MRI
Our study will analyze neuroimaging data utilizing a training-validation-testing approach with a nested cross-validation and feature selection routine to categorize MWoA patients into acupuncture responders and non-responders. The proportion of responders, defined as participants with a reduction in monthly headache onsets by at least 50% will be determined (33). We will concatenate all the brain features (including white matter, gray matter, cortical thickness, and resting FC) to produce a joint feature vector to feed into the subsequent analysis process. Machine learning approaches including linear support vector machine (LSVM), k-nearest neighbors (k-NN), and random forests (RF) will be used to select the features with the highest discriminative power for the classifier. To avoid the risk of overfitting, we will use a leave-one-out cross-validation strategy to evaluate the performance of the classifiers and feature ranking. The performance of each classifier will be estimated and compared by accuracy, sensitivity, and specificity. Sensitivity and specificity indicate the proportion of correctly classified responders and non-responders, respectively. Then the best classifier will be chosen.
Patient and public involvement
The participants and the general public have no involvement in the study's design or implementation, and they will not be requested to provide feedback on reporting or to disseminate the finding. Participants will be able to view the study results via social media.
Ethics and dissemination
The trial protocol adheres the principles of the Declaration of Helsinki and was approved by the Research Ethical Committee of Beijing Hospital of Traditional Chinese Medicine, Capital Medical University (Ethics Reference Number: 2020BL02-053-01) (Supplementary material). This trial was registered with the Chinese Clinical Trial Registry (ID: ChiCTR2100044251).
If any modifications or decisions are made, the ethics committee will review and approve amendments, and new protocols will be uploaded to www.chictr.org.cn. The authors will retain full control of the manuscript content. The study results will be published in a peer-reviewed academic journal and disseminated electronically via conference presentations.
Discussion
The possibility of acupuncture to modulate abnormal cerebral activity to treat MWoA
Brain imaging has recently been widely employed in acupuncture research as a promising approach for investigating the neural mechanism of acupuncture (76). In latest years, studies have focused more on the interactions between the FC networks of brain regions to determine the neural circuitry underlying the therapeutic benefits of acupuncture, rather than the alterations in a specific brain region during acupuncture (28).
However, the exact pathophysiology of migraine remains unclear, and there is an abundance of imaging research indicating extensive structural and functional changes in brain regions and networks. They might influence migraine pain experience and multisensory integration (77, 78). Therefore, utilizing these brain imaging approaches, rigorous design and implementation might facilitate research of acupuncture mechanisms in migraineurs.
After acupuncture therapy, research showed enhanced ReHo/ALFF/brain metabolites in brain regions involved in pain processing, such as the affective-emotional processing of pain [e.g., the insula (79, 80), cerebellum (79), and brainstem (79)], cognitive pain processing [e.g., the orbitofrontal cortex (80–82)], and the descending pain modulation system (DPMS) [e.g., the rostral ventromedial medulla/trigeminocervical complex (81)]. Meanwhile, research showed lower levels of ReHo/ALFF/brain metabolites in brain regions implicated in cognitive pain processing [e.g., the hippocampus (79, 80)] and in the resting-state network, such as the default mode network (DMN) [e.g., the posterior cingulate cortex (79, 80), precuneus (79), and inferior parietal lobule (79)], and frontal parietal network (FPN) [e.g., the postcentral gyrus (79, 80)].
After long-term acupuncture therapy, enhanced FC has been identified in the DMN (27, 83) and FPN [e.g., the superior frontal gyrus and medial frontal gyrus (83)]. Moreover, it has been reported that there is an enhanced FC between the right FPN (RFPN), the left FPN [e.g., the left precentral gyrus and left postcentral gyrus (84)] and DMN [e.g., the left inferior parietal lobule (84) and posterior cingulate cortex (85)]. After acupuncture treatment, a group of researchers (85) found a reduction in FC between the RFPN and DMN (right precuneus). Furthermore, they applied seed-based analysis (SBA) by using the right precuneus as a seed to investigate the involvement of the right precuneus during acupuncture. They revealed the enhanced right precuneus FC with the DMN, DPMS, RFPN, and the reward system. The right ventrolateral periaqueductal gray was selected as the seed in another research (84), the authors discovered greater FC of the ventrolateral periaqueductal gray with the limbic systems and the DPMS.
Multimodal MRI as a promising approach to investigate the neural mechanism of acupuncture
A combination of two or more MRI scans is referred to as multimodal MRI. It has a high spatial-temporal resolution as well as broad anatomical and emotional sensitivity (86). Three of the most commonly employed neuroimaging modalities in acupuncture research are fMRI, sMRI, and DTI (87). Multimodal MRI may yield longitudinal approach to analyze the central mechanisms underpinning acupuncture's effects on MWoA. We aim to explore the neuropathological changes in patients with MWoA from the perspective of brain structure and function. sMRI and DTI may identify structural alterations in brain regions, while fMRI may investigate alterations in functional connectivity between brain regions.
The application of multimodal MRI and multidimensional analytic methodologies will be used to elucidate on the neural mechanisms of acupuncture from distinct brain regions and functional networks. Finally, cross-validation of fMRI, sMRI, and DTI data strengthens the results' accuracy and reproducibility.
Neuroimaging predictor of acupuncture outcome in the treatment of MWoA
Treatment personalization is an important trend in medicine. Imaging data is widely being used to support in disease diagnosis for oncology (88) and psychology (36–38). Nevertheless, limited studies have applied imaging to predict acupuncture effect. Our previous research employed a machine learning classification approach to develop a prediction model of acupuncture effectiveness in migraineurs based on pretreatment gray matter (GM) structure. The model was 83% accurate in differentiating between acupuncture responders and non-responders (35). Our findings present an objective biomarker for acupuncture therapy response, as well as a novel strategy for developing personalized medication for migraine.
Differences between individuals in the effectiveness of acupuncture are a prevalent issue. A recent study showed that only approximately 50% of patients had considerable relief of symptoms after 1 month of acupuncture therapy (35). As a result, predicting acupuncture response might lower medical expenses for those classified as non-responders. ADDIN EN.CITE. This study will use multiple non-parametric-regression-based machines learning approaches to discriminate between responders and non-responders. These packages of techniques are self-acting in learning patterns from data and no assumptions are demanded of the structure of the data. These techniques capture non-linear relationships in the data, and the interrelationship between predictors. Machine learning approaches are increasingly used for class prediction issues, which can help to avoid the pitfalls flaw of parametric regression models (ignoring non-linear influences of independent variables on the outcome, or ignoring interactions between independent variables) (89). LSVM, k-NN, and RF are commonly used approaches in machine learning, many researches have verified their promising performance for diseases prediction (90–93). We compare various methods to obtain a classification model with better accuracy, sensitivity, and specificity.
The present study has several limitations. First, sham acupuncture, designed as a minimally invasive needle on non-acupoints in our study, might have produced certain physiological effects. Minimally invasive needles are required to minimize the non-specific effects of sham acupuncture. However, in several previous studies, sham acupuncture produced non-specific effects in the control group. In the future, we will use a placebo needle in the sham group. However, patients may identify the placebo needle because real acupuncture is widely used in China. Moreover, placebo needles might cause a multitude of peripheral, segmental, and cerebral reactions to an unexpected extent (94–96). Our further studies should compare acupuncture with standard therapies rather than comparing it only to sham acupuncture. Second, this present study only included a single center; therefore, the reproducibility of this study cannot be confirmed. Subsequently, more centers will need to evaluate the reproducibility and robustness of our predictive model. Third, a standard prescription will be used to assess the effectiveness of acupuncture in this study. To minimize performance bias, this study will not employ personalized prescription based on the acupuncturist's experience (46). Fourth, we will not apply magnetic resonance spectroscopy (MRS) to investigate brain metabolites due to budget constraints (97). Therefore, we plan to add MRS to our investigations in the future.
To summarize, our study aims to evaluate the efficacy of acupuncture for MWoA. We hope to present solid evidence for the mechanisms of acupuncture therapy on MWoA using multimodal MRI data on brain structure and function. Moreover, machine learning technology will be used to predict the acupuncture responders for MWoA.
Ethics statement
The studies involving human participants were reviewed and approved by Research Ethical Committee of Beijing Hospital of Traditional Chinese Medicine, Capital Medical University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LL is a principal investigator of the study and is responsible for making final decisions on the trial design and manuscript preparation and conducted the study. JH and LL drafted the protocol. LL and YK participated in the design of the study and contributed to the revising the protocol manuscript. LZe was responsible for the statistical design of the study. YZ was responsible for MRI data acquisition. LZha and ZT provided MRI advice and made critical revisions. JS, YC, QC, YL, LZhu, and BL participated in data collection and were in charge of recruitment. LL is a principal investigator of the study and is responsible for making final decisions on the trial design and manuscript preparation. All authors contributed to the article and approved the submitted version.
Funding
This work will be supported by the following funding sources: the Capital Health Development Scientific Research Project Excellent Young Talents (Capital Development 2020-4-2236), the Beijing Municipal Education Commission Science and Technology Plan General Project (KM202110025005), the China National Natural Science Foundation (82074179), the China Association for Science and Technology Young Talent Lifting Project (2019-2021ZGZJXH-QNRC001), the National Key Research and Development Plan (2019YFC1709703), and the National Administration of Traditional Chinese Medicine: 2019 Project of Building Evidence-Practice Capacity for TCM (No. 2019XZZX-ZJ002).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.981752/full#supplementary-material
Abbreviations
MWoA, migraine without aura; MRI, magnetic resonance imaging; fMRI, functional magnetic resonance imaging; sMRI, structural magnetic resonance imaging; DTI, diffusion tensor imaging; MSQ, Migraine-Specific Quality of Life Questionnaire; HIT-6, Headache Impact Test; BDI-II, Beck Depression Inventory; BAI, Beck Anxiety Inventory; NSAIDs, non-steroidal anti-inflammatory drugs; EAN, European Academy of Neurology; AAN, American Academy of Neurology; the UK, the United Kingdom; the USA, the United States of America; SPIRIT, Standard Protocol Items, Recommendations for Intervention Trials; CONSORT, the Consolidated Standards of Reporting Trials; STRICTA, Standards for Reporting Interventions in Clinical Trials of Acupuncture principles; HCs, healthy controls; ICHD-III, The International Classification of Headache Disorders, 3rd edition; SAS, Statistical Analysis System; RA, real acupoints; WHO, World Health Organization; SA, sham acupoints; CRFs, Case Report Forms; TR, repeat time; TE, echo time; FOV, field of view; BOLD, blood oxygenation level-dependent; ALFF, amplitude of low-frequency fluctuation; ReHo, regional homogeneity; ICA, independent component analyses; FC, functional connectivity; DC, degree centrality; VMHC, voxel-mirrored homotopic connectivity; GMV, gray matter volume; WMV, white matter volume; TBV, total brain volume; MD, mean diffusivity; RD, radial diffusivity; AD, axial diffusivity; FA, fractional anisotropy; MMDs, monthly headache days; VAS, Visual Analog Scale; RFR, the role function-restrictive domain; RFP, the role function-preventive domain; EF, the emotional functioning domain; MDD, major depressive disorder; DSM-IV, the fourth edition of Diagnostic and Statistical Manual of Mental Disorders; AEs, adverse events; SPSS, Statistical Package for Social Science; ITT, intention-to-treat; LOCF, last observation carried forward method; PP, per-protocol; SDs, Standard deviations; CIs, confidence intervals; SPM, Statistical Parametric Mapping; DPARSF, Data Processing Assistant for Resting-State fMRI; VBM, voxel-based morphometry; FSL, fMRI of the brain Software Library; AFNI, Analysis of Functional NeuroImages; DARTEL, the Diffeomorphic Anatomical Registration using Exponentiated Lie algebra; MNI, Montreal Neurological Institute; FDT, FSL's Diffusion Toolbox; LSVM, linear support vector machine; k-NN, k-nearest neighbors; RF, random forests; DPMS, descending pain modulation system; DMN, default mode network; FPN, frontal parietal network; RFPN, right FPN; SBA, seed-based analysis; GM, gray matter; MRS, magnetic resonance spectroscopy.
References
1. Manack AN, Buse DC, Lipton RB. Chronic migraine: epidemiology and disease burden. Curr Pain Headache Rep. (2011) 15:70–8. doi: 10.1007/s11916-010-0157-z
2. Sprenger T, Borsook D. Migraine changes the brain: neuroimaging makes its mark. Curr Opin Neurol. (2012) 25:252–62. doi: 10.1097/WCO.0b013e3283532ca3
3. Borsook D, Maleki N, Becerra L, McEwen B. Understanding migraine through the lens of maladaptive stress responses: a model disease of allostatic load. Neuron. (2012) 73:219–34. doi: 10.1016/j.neuron.2012.01.001
4. Liu J, Lan L, Mu J, Zhao L, Yuan K, Zhang Y, et al. Genetic contribution of catechol-O-methyltransferase in hippocampal structural and functional changes of female migraine sufferers. Hum Brain Mapp. (2015) 36:1782–95. doi: 10.1002/hbm.22737
5. Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1211–59.
7. Saylor D, Steiner TJ. The Global Burden of Headache. Semin Neurol. (2018) 38:182–90. doi: 10.1055/s-0038-1646946
8. Collaborators GBDH. Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. (2018) 17:954−76. doi: 10.1016/S1474-4422(18)30322-3
9. Xu J, Zhang FQ, Pei J, Ji J. Acupuncture for migraine without aura: a systematic review and meta-analysis. J Integr Med. (2018) 16:312–21. doi: 10.1016/j.joim.2018.06.002
10. Linde K, Allais G, Brinkhaus B, Fei Y, Mehring M, Vertosick EA, et al. Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev. (2016) 2016:Cd001218. doi: 10.1002/14651858.CD001218.pub3
11. Li YX, Xiao XL, Zhong DL, Luo LJ, Yang H, Zhou J, et al. Effectiveness and safety of acupuncture for migraine: an overview of systematic reviews. Pain Res Manag. (2020) 2020:3825617. doi: 10.1155/2020/3825617
12. Giannini G, Favoni V, Merli E, Nicodemo M, Torelli P, Matra A, et al. Randomized clinical trial on acupuncture versus best medical therapy in episodic migraine prophylaxis: the ACUMIGRAN study. Front Neurol. (2020) 11:570335. doi: 10.21203/rs.3.rs-32721/v1
13. Yang Y, Que Q, Ye X, Zheng G. Verum vs. sham manual acupuncture for migraine: a systematic review of randomized controlled trials. Acupunct Med. (2016) 34:76–83. doi: 10.1136/acupmed-2015-010903
14. Vickers AJ, Vertosick EA, Lewith G, MacPherson H, Foster NE, Sherman KJ, et al. Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. (2018) 19:455–74. doi: 10.1016/j.jpain.2017.11.005
15. Li SW Li YS, Liu RZ, Qiao XY, Wan Q, Yang XS Yu SY Yu TM., Zou J. Guidelines for the diagnosis and treatment of migraine in China. Zhongguo Teng Tong Yi Xue Za Zhi. (2011) 17:65–86.
16. NIfHaC E. Headaches in Over 12s: Diagnosis and Management. London UK: National Institute for Health and Care Excellence (2012). p. 30.
17. Lanteri-Minet M, Valade D, Géraud G, Lucas C, Donnet A. [Guidelines for the diagnosis and management of migraine in adults and children]. Rev Neurol. (2012) 169:14-29. doi: 10.1016/j.neurol.2012.07.022
18. British Association for the Study of Headache. National Headache Management System for Adults 2019. (2019).
19. Eigenbrodt AK, Ashina H, Khan S, Diener HC, Mitsikostas DD, Sinclair AJ, et al. Diagnosis and management of migraine in ten steps. Nat Rev Neurol. (2021) 17:501–14. doi: 10.1038/s41582-021-00509-5
20. Becker WJ, Findlay T, Moga C, Scott NA, Harstall C, Taenzer P. Guideline for primary care management of headache in adults. Can Fam Physician. (2015) 61:670-9.
21. Acupuncture Services. Clinical Guidelines for Medical Necessity Review of Acupuncture Services. Clinical Guidelines. Bluffton: eviCore (2018).
22. Kursun O, Yemisci M, van den Maagdenberg A, Karatas H. Migraine and neuroinflammation: the inflammasome perspective. J Headache Pain. (2021) 22:55. doi: 10.1186/s10194-021-01271-1
23. Xu X, Liu L, Zhao L, Li B, Jing X, Qu Z, et al. Effect of electroacupuncture on hyperalgesia and vasoactive neurotransmitters in a rat model of conscious recurrent migraine. Evid Based Complement Alternat Med. (2019):9512875. doi: 10.1155/2019/9512875
24. Liu L, Pei P, Zhao LP, Qu ZY, Zhu YP, Wang LP. Electroacupuncture pretreatment at GB20 exerts antinociceptive effects via peripheral and central serotonin mechanism in conscious migraine rats. Evid Based Complement Alternat Med. (2016) 1846296. doi: 10.1155/2016/1846296
25. Akerman S, Holland PR, Goadsby PJ. Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci. (2011) 12:570–84. doi: 10.1038/nrn3057
26. Xue T, Yuan K, Zhao L, Yu D, Zhao L, Dong T, et al. Intrinsic brain network abnormalities in migraines without aura revealed in resting-state fMRI. PLoS ONE. (2012) 7:e52927. doi: 10.1371/journal.pone.0052927
27. Zou Y, Tang W, Li X, Xu M, Li J. Acupuncture Reversible Effects on Altered Default Mode Network of Chronic Migraine Accompanied with Clinical Symptom Relief. Neural Plast. (2019) 2019:5047463. doi: 10.1155/2019/5047463
28. Chang CM, Yang CP, Yang CC, Shih PH, Wang SJ. Evidence of potential mechanisms of acupuncture from functional mri data for migraine prophylaxis. Curr Pain Headache Rep. (2021) 25:49. doi: 10.1007/s11916-021-00961-4
29. Kristoffersen ES, Grande RB, Aaseth K, Lundqvist C, Russell MB. Management of primary chronic headache in the general population: the Akershus study of chronic headache. J Headache Pain. (2012) 13:113–20. doi: 10.1007/s10194-011-0391-8
30. Wells RE, Bertisch SM, Buettner C, Phillips RS, McCarthy EP. Complementary and alternative medicine use among adults with migraines/severe headaches. Headache. (2011) 51:1087–97. doi: 10.1111/j.1526-4610.2011.01917.x
31. Chessman AW. Review: acupuncture reduces migraine frequency more than usual care, sham acupuncture, or prophylactic drugs. Ann Intern Med. (2016) 165:JC44. doi: 10.7326/ACPJC-2016-165-8-044
32. Pokladnikova J, Maresova P, Dolejs J, Park AL, Wang B, Guan X, et al. Economic analysis of acupuncture for migraine prophylaxis. Neuropsychiatr Dis Treat. (2018) 14:3053–61. doi: 10.2147/NDT.S174870
33. Diener HC, Kronfeld K, Boewing G, Lungenhausen M, Maier C, Molsberger A, et al. Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomized controlled clinical trial. Lancet Neurol. (2006) 5:310–6. doi: 10.1016/S1474-4422(06)70382-9
34. Wang LP, Zhang XZ, Guo J, Liu HL, Zhang Y, Liu CZ, et al. Efficacy of acupuncture for migraine prophylaxis: a single-blinded, double-dummy, randomized controlled trial. Pain. (2011) 152:1864–71. doi: 10.1016/j.pain.2011.04.006
35. Yang XJ, Liu L, Xu ZL, Zhang YJ, Liu DP, Fishers M, et al. Baseline brain gray matter volume as a predictor of acupuncture outcome in treating migraine. Front Neurol. (2020) 11:111. doi: 10.3389/fneur.2020.00111
36. Redlich R, Opel N, Grotegerd D, Dohm K, Zaremba D, Burger C, et al. Prediction of individual response to electroconvulsive therapy via machine learning on structural magnetic resonance imaging data. JAMA Psychiatry. (2016) 73:557–64. doi: 10.1001/jamapsychiatry.2016.0316
37. Du Y, Fu Z, Calhoun VD. Classification and prediction of brain disorders using functional connectivity: promising but challenging. Front Neurosci. (2018) 12:525. doi: 10.3389/fnins.2018.00525
38. Grotegerd D, Stuhrmann A, Kugel H, Schmidt S, Redlich R, Zwanzger P, et al. Amygdala excitability to subliminally presented emotional faces distinguishes unipolar and bipolar depression: an fMRI and pattern classification study. Hum Brain Mapp. (2014) 35:2995–3007. doi: 10.1002/hbm.22380
39. Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gotzsche PC, Krleza-Jeric K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. (2013) 158:200–7. doi: 10.7326/0003-4819-158-3-201302050-00583
40. Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P, Group C. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med. (2008) 148:295–309. doi: 10.7326/0003-4819-148-4-200802190-00008
41. MacPherson H, Altman DG, Hammerschlag R, Li Y, Wu T, White A, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. Acupunct Med. (2010) 28:83–93. doi: 10.1111/j.1756-5391.2010.01086.x
42. Tfelt-Hansen P, Pascual J, Ramadan N, Dahlöf C, D'Amico D, Diener HC, et al. Guidelines for controlled trials of drugs in migraine: third edition. A guide for investigators Cephalalgia. (2012) 32:6–38. doi: 10.1177/0333102411417901
43. Qiu T, Li L. [Discussion on the Chinese edition of the WHO standard acupuncture point locations in the western Pacific Region]. Zhongguo Zhen Jiu. (2011) 31:827–30.
44. Li Y, Liang F, Yang X, Tian X, Yan J, Sun G, et al. Acupuncture for treating acute attacks of migraine: a randomized controlled trial. Headache. (2009) 49:805–16. doi: 10.1111/j.1526-4610.2009.01424.x
45. Li Y, Zheng H, Witt CM, Roll S, Yu SG, Yan J, et al. Acupuncture for migraine prophylaxis: a randomized controlled trial. CMAJ. (2012) 184:401–10. doi: 10.1503/cmaj.110551
46. Zhao L, Chen J, Li Y, Sun X, Chang X, Zheng H, et al. The long-term effect of acupuncture for migraine prophylaxis: a randomized clinical trial. JAMA Intern Med. (2017) 177:508–15. doi: 10.1001/jamainternmed.2016.9378
47. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. (2011) 63 Suppl 11:S467–72. doi: 10.1002/acr.20561
48. Russell MB, Rasmussen BK, Brennum J, Iversen HK, Jensen RA, Olesen J. Presentation of a new instrument: the diagnostic headache diary. Cephalalgia. (1992) 12:369–74. doi: 10.1111/j.1468-2982.1992.00369.x
49. Dowson AJ. Assessing the impact of migraine. Curr Med Res Opin. (2001) 17:298–309. doi: 10.1185/030079901753403207
50. Kosinski M, Bayliss MS, Bjorner JB, Ware JE. Jr., Garber WH, Batenhorst A, et al. A six-item short-form survey for measuring headache impact: the HIT-6 Qual Life Res. (2003) 12:963–74. doi: 10.1023/A:1026119331193
51. Yang M, Rendas-Baum R, Varon SF, Kosinski M. Validation of the Headache Impact Test (HIT-6) across episodic and chronic migraine. Cephalalgia. (2011) 31:357–67. doi: 10.1177/0333102410379890
52. Jhingran P, Davis SM, LaVange LM, Miller DW, Helms RW. Migraine-specific quality-of-life questionnaire. Further investigation of the factor structure. Pharmacoeconomics. (1998) 13:707–17. doi: 10.2165/00019053-199813060-00007
53. Jhingran P, Osterhaus JT, Miller DW, Lee JT, Kirchdoerfer L. Development and validation of the migraine-specific quality of life questionnaire. Headache. (1998) 38:295–302. doi: 10.1046/j.1526-4610.1998.3804295.x
54. Bagley CL, Rendas-Baum R, Maglinte GA, Yang M, Varon SF, Lee J. Kosinski M. Validating migraine-specific quality of life questionnaire v21 in episodic and chronic migraine. Headache. (2012) 52:409–21. doi: 10.1111/j.1526-4610.2011.01997.x
55. Beck AT, Steer RA, Brown GK. Beck Depression Inventory-II. San Antonio: Psychological Corporation. (1996). doi: 10.1037/t00742-000
56. Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. (1996) 67:588–97. doi: 10.1207/s15327752jpa6703_13
57. Steer RA, Ball R, Ranieri WF, Beck AT. Dimensions of the Beck depression inventory-II in clinically depressed outpatients. J Clin Psychol. (1999) 55:117–28.3.0.CO;2-A“ target=”_blank“>https://doi.org/10.1002/(SICI)1097-4679(199901)55:1<117::AID-JCLP12>3.0.CO;2-A
59. Richter P, Werner J, Heerlein A, Kraus A, Sauer H. On the validity of the Beck Depression Inventory. A review. Psychopathology. (1998) 31:160–8. doi: 10.1159/000066239
60. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol. (1988) 56:893–7. doi: 10.1037/0022-006X.56.6.893
61. Leyfer OT, Ruberg JL, Woodruff-Borden J. Examination of the utility of the Beck Anxiety Inventory and its factors as a screener for anxiety disorders. J Anxiety Disord. (2006) 20:444–58. doi: 10.1016/j.janxdis.2005.05.004
62. Zhang J, Shang H, Gao X, Ernst E. Acupuncture-related adverse events: a systematic review of the Chinese literature. Bull World Health Organ. (2010) 88:915–21C. doi: 10.2471/BLT.10.076737
63. Sun Y, Liu Y, Liu B, Zhou K, Yue Z, Zhang W, et al. Efficacy of acupuncture for chronic prostatitis/chronic pelvic pain syndrome: a randomized trial. Ann Intern Med. (2021) 174:1357–66. doi: 10.7326/M21-1814
64. Hanspach J, Nagel AM, Hensel B, Uder M, Koros L, Laun FB. Sample size estimation: Current practice and considerations for original investigations in MRI technical development studies. Magn Reson Med. (2021) 85:2109–16. doi: 10.1002/mrm.28550
65. McLaren CE, Chen WP, O'Sullivan TD, Gillen DL, Su MY, Chen JH, et al. Sample size and power determination when limited preliminary information is available. BMC Med Res Methodol. (2017) 17:1–8. doi: 10.1186/s12874-017-0329-1
66. Yeo S, Choe IH, van den Noort M, Bosch P, Jahng GH, Rosen B, et al. Acupuncture on GB34 activates the precentral gyrus and prefrontal cortex in Parkinson's disease. BMC Complement Altern Med. (2014) 14:336. doi: 10.1186/1472-6882-14-336
67. Yan CQ, Wang X, Huo JW, Zhou P, Li JL, Wang ZY, et al. Abnormal global brain functional connectivity in primary insomnia patients: a resting-state functional MRI study. Front Neurol. (2018) 9:856. doi: 10.3389/fneur.2018.00856
68. Desmond JE, Glover GH. Estimating sample size in functional MRI (fMRI) neuroimaging studies: statistical power analyses. J Neurosci Methods. (2002) 118:115–28. doi: 10.1016/S0165-0270(02)00121-8
69. Jeon SR, Nam D, Kim TH. Dropouts in randomized clinical trials of Korean medicine interventions: a systematic review and meta-analysis. Trials. (2021) 22:176. doi: 10.1186/s13063-021-05114-x
70. Wong CA, Song WB, Jiao M, O'Brien E, Ubel P, Wang G, et al. Strategies for research participant engagement: a synthetic review and conceptual framework. Clin Trials. (2021) 18:457–65. doi: 10.1177/17407745211011068
71. Zhou F, Huang S, Zhuang Y, Gao L, Gong H. Frequency-dependent changes in local intrinsic oscillations in chronic primary insomnia: A study of the amplitude of low-frequency fluctuations in the resting state. Neuroimage Clin. (2017) 15:458–65. doi: 10.1016/j.nicl.2016.05.011
72. Vargas C, Lopez-Jaramillo C, Vieta E, A. systematic literature review of resting state network-functional MRI in bipolar disorder. J Affect Disorders. (2013) 150:727–35. doi: 10.1016/j.jad.2013.05.083
73. Ashburner J. fast diffeomorphic image registration algorithm. Neuroimage. (2007) 38:95–113. doi: 10.1016/j.neuroimage.2007.07.007
74. Matsuda H, MRI. morphometry in Alzheimer's disease. Aging Res Rev. (2016) 30:17–24. doi: 10.1016/j.arr.2016.01.003
75. Aoki Y, Yoncheva YN, Chen B, Nath T, Sharp D, Lazar M, et al. Association of white matter structure with autism spectrum disorder and attention-deficit/hyperactivity disorder. JAMA Psychiatry. (2017) 74:1120–8. doi: 10.1001/jamapsychiatry.2017.2573
76. Cai RL, Shen GM, Wang H, Guan YY. Brain functional connectivity network studies of acupuncture: a systematic review on resting-state fMRI. J Integr Med. (2018) 16:26–33. doi: 10.1016/j.joim.2017.12.002
77. Maleki N, Gollub RL. What have we learned from brain functional connectivity studies in migraine headache? Headache. (2016) 56:453–61. doi: 10.1111/head.12756
78. Chong CD, Gaw N, Fu Y, Li J, Wu T, Schwedt TJ. Migraine classification using magnetic resonance imaging resting-state functional connectivity data. Cephalalgia. (2017) 37:828–44. doi: 10.1177/0333102416652091
79. Zhao L, Liu J, Zhang F, Dong X, Peng Y, Qin W, et al. Effects of long-term acupuncture treatment on resting-state brain activity in migraine patients: a randomized controlled trial on active acupoints and inactive acupoints. PLoS ONE. (2014) 9:e99538. doi: 10.1371/journal.pone.0099538
80. Qin XL, Wang WY, Wang JZ, Xie WY, Zhang YM, Gao YQ. [Analysis on regional homogeneity of resting brain during balance acupuncture-induced analgesic effect in migraine patients without aura]. Zhen Ci Yan Jiu. (2019) 44:446–50.
81. Li Z, Zeng F, Yin T, Lan L, Makris N, Jorgenson K, et al. Acupuncture modulates the abnormal brainstem activity in migraine without aura patients. Neuroimage Clin. (2017) 15:367–75. doi: 10.1016/j.nicl.2017.05.013
82. Gu T, Lin L, Jiang Y, Chen J, D'Arcy RC, Chen M, et al. Acupuncture therapy in treating migraine: results of a magnetic resonance spectroscopy imaging study. J Pain Res. (2018) 11:889–900. doi: 10.2147/JPR.S162696
83. Zhang Y, Li KS, Liu HW, Fu CH, Chen S, Tan ZJ, et al. Acupuncture treatment modulates the resting-state functional connectivity of brain regions in migraine patients without aura. Chin J Integr Med. (2016) 22:293–301. doi: 10.1007/s11655-015-2042-4
84. Li KS, Zhang Y, Ning YZ, Zhang H, Liu HW, Fu CH, Ren Y, Zou YH. The effects of acupuncture treatment on the right frontoparietal network in migraine without aura patients. J Headache Pain. (2015) 16. doi: 10.1186/s10194-015-0518-4
85. Li Z, Lan L, Zeng F, Makris N, Hwang J, Guo T, et al. The altered right frontoparietal network functional connectivity in migraine and the modulation effect of treatment. Cephalalgia. (2017) 37:161–76. doi: 10.1177/0333102416641665
86. Uludag K, Roebroeck A. General overview on the merits of multimodal neuroimaging data fusion. Neuroimage. 2014 102 (Pt 1):3-10. doi: 10.1016/j.neuroimage.2014.05.018
87. Qiu K, Jing M, Sun R, Yang J, Liu X, He Z, et al. The status of the quality control in acupuncture-neuroimaging studies. Evid Based Complement Alternat Med. (2016) 2016:3685785. doi: 10.1155/2016/3685785
88. Bi WL, Hosny A, Schabath MB, Giger ML, Birkbak NJ, Mehrtash A, et al. Artificial intelligence in cancer imaging: Clinical challenges and applications. CA Cancer J Clin. (2019) 69:127–57. doi: 10.3322/caac.21552
89. Kruppa J, Liu Y, Biau G, Kohler M, Konig IR, Malley JD, et al. Probability estimation with machine learning methods for dichotomous and multicategory outcome: theory. Biom J. (2014) 56:534–63. doi: 10.1002/bimj.201300068
90. Weng SF, Reps J, Kai J, Garibaldi JM, Qureshi N. Can machine-learning improve cardiovascular risk prediction using routine clinical data? PLoS ONE. (2017) 12:e0174944. doi: 10.1371/journal.pone.0174944
91. Senders JT, Staples PC, Karhade AV, Zaki MM, Gormley WB, Broekman MLD, et al. Machine learning and neurosurgical outcome prediction: a systematic review. World Neurosurg. (2018) 109:476-86 e1. doi: 10.1016/j.wneu.2017.09.149
92. Churpek MM, Yuen TC, Winslow C, Meltzer DO, Kattan MW, Edelson DP. Multicenter Comparison of machine learning methods and conventional regression for predicting clinical deterioration on the wards. Crit Care Med. (2016) 44:368–74. doi: 10.1097/CCM.0000000000001571
93. Goldstein BA, Navar AM, Carter RE. Moving beyond regression techniques in cardiovascular risk prediction: applying machine learning to address analytic challenges. Eur Heart J. (2017) 38:1805–14. doi: 10.1093/eurheartj/ehw302
94. Tsukayama H, Yamashita H, Kimura T, Otsuki K. Factors that influence the applicability of sham needle in acupuncture trials - Two randomized, single-blind, crossover trials with acupuncture-experienced subjects. Clin J Pain. (2006) 22:346–9. doi: 10.1097/01.ajp.0000176359.94644.mL
95. Lund I, Naslund J, Lundeberg T. Minimal acupuncture is not a valid placebo control in randomized controlled trials of acupuncture: a physiologist's perspective. Chin Med. (2009) 4:1. doi: 10.1186/1749-8546-4-1
96. Dincer F, Linde K. Sham interventions in randomized clinical trials of acupuncture–a review. Complement Ther Med. (2003) 11:235–42. doi: 10.1016/S0965-2299(03)00124-9
Keywords: acupuncture, clinical trial, migraine without aura, multimodal magnetic resonance imaging, neurological mechanism, protocol, treatment effects prediction
Citation: Hong J, Sun J, Zhang L, Tan Z, Chen Y, Chen Q, Zhu Y, Liu Y, Zhu L, Zeng L, Kong Y, Li B and Liu L (2022) Neurological mechanism and treatment effects prediction of acupuncture on migraine without aura: Study protocol for a randomized controlled trial. Front. Neurol. 13:981752. doi: 10.3389/fneur.2022.981752
Received: 29 June 2022; Accepted: 22 August 2022;
Published: 08 September 2022.
Edited by:
Faisal Mohammad Amin, University of Copenhagen, DenmarkCopyright © 2022 Hong, Sun, Zhang, Tan, Chen, Chen, Zhu, Liu, Zhu, Zeng, Kong, Li and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lu Liu, bHVsdWxhbGF2aWN0b3IxOTg1QDEyNi5jb20=
 Jiahui Hong
Jiahui Hong Jingqing Sun2
Jingqing Sun2 Lin Zeng
Lin Zeng Yazhuo Kong
Yazhuo Kong Lu Liu
Lu Liu