
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurol. , 15 September 2022
Sec. Stroke
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.971399
Objective: The effect of endovascular thrombectomy (EVT) in acute ischemic stroke patients with prestroke disability (modified Rankin Scale score, mRS) ≥2) has not been well-studied. This study aimed to assess the safety and benefit of EVT in patients with prestroke disability.
Methods: According to PRISMA guidelines, literature searching was performed using PubMed, Embase, and Cochrane databases, for a series of acute ischemic stroke patients with prestroke mRS ≥2 treated by EVT. Random-effects meta-analysis was used to pool the rate of return to prestroke mRS and mortality at 3-month follow-up.
Results: In total, 13 observational studies, with 2,625 patients, were analyzed. The rates of return to prestroke mRS in patients with prestroke mRS of 2–4 were 20% (120/588), 27% (218/827), and 31% (34/108), respectively. Patients with prestroke disability treated by EVT had a higher likelihood of return to prestroke mRS (relative risk, RR, 1.86; 95% CI 1.28–2.70) and a lower likelihood of mortality (RR 0.75; 95%CI 0.58–0.97) compared with patients with standard medical treatment. Successful recanalization (Thrombolysis in Cerebral Infarction grade 2b-3) after EVT gave a higher likelihood of return to prestroke mRS (RR 2.04; 95% CI 1.17–3.55) and lower mortality (RR 0.72; 95% CI 0.62–0.84) compared with unsuccessful reperfusion.
Conclusions: Acute ischemic stroke patients with prestroke disability may benefit from EVT. Withholding EVT on the sole ground of prestroke disabilities may not be justified.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/.
Current guidelines for acute ischemic stroke treatment unanimously recommend endovascular thrombectomy (EVT) for eligible patients with a prestroke modified Rankin Scale score (mRS) of 0–1 (1–3). The challenge of the available evidence from randomized clinical trials is partly due to the trial selection paradigms that exclude patients with prestroke mRS ≥2 (4). However, prestroke mRS ≥2 is relatively common among patients harboring acute ischemic stroke, with a reported frequency between 23.5 and 34.1% (4, 5). Furthermore, an international survey has reported that the EVT practice for patients with prestroke mRS ≥2 is heterogenous, and the EVT decision largely depends on clinician opinions (6). Therefore, selecting optimal treatments is necessary for these patients to obtain timely and successful revascularizations and improved clinical outcomes.
Beyond the previously published literature review, which has been limited to a broad overview of the current evidence (7), two systematic reviews of observational studies compare the outcome of EVT in patients with prestroke mRS ≥3 to those with mRS <3 (8, 9). Adamou et al. (8) have concluded that prestroke mRS ≥3 represents an independent predictor for unfavorable clinical outcomes. Bala et al. (9) have revealed that although patients with prestroke mRS ≥3 are related to an increased risk of death, higher proportions of patients reached their prestroke mRS. Because those systematic reviews categorize patients with prestroke mRS = 2 into the disability-free group, and only <15% of the patients in the analysis have prestroke mRS ≥3, concerns arise about selection bias and limited generalizability of the results. Moreover, no stratified analyses have been performed in the previous systematic reviews based on prestroke mRS categories (i.e., mRS 2, 3, and so on), and consequently, no effects of the disability degree on outcomes have been studied. In addition, the superiority of EVT and standard medical treatments (including intravenous thrombolysis, systematic anti-coagulation, antiplatelet medications, or combinations of these medical treatments) have not been well-evaluated. The benefit of successful reperfusion as a proxy for EVT is yet to be assessed.
The present systematic review and meta-analysis aim to (1) estimate the rate of differential outcomes of EVT in patients with prestroke disability, stratified by prestroke mRS; (2) assess the safety and efficacy of EVT in treating patients with prestroke disability, in comparison with standard medical treatment; and (3) evaluate the safety and benefit of successful recanalization achieved by EVT in patients with prestroke disability.
The study protocol was prospectively registered in the PROSPERO registry (Registration No.: CRD42022327983). This systematic review and meta-analysis was conducted in accordance with the PRISMA statement (10) and was reported in compliance with the MOOSE guidelines (11).
Types of studies: prospective or retrospective observational studies. Types of participants: acute ischemic stroke patients with prestroke mRS ≥2. Types of interventions: EVT and /or standard medical treatment. Types of outcome measures: outcomes included a return to prestroke mRS and mortality at a 3-month follow-up.
Systematic literature searching was conducted on Pubmed, Embase, and the Cochrane Library, from their inception to March 28, 2022, without any restrictions. Additional manual searching included the reference lists of all included studies and relevant review articles.
Complete searching keywords were as follows: ((“prestroke” OR “pre-stroke” OR (“stroke” AND (“premorbid” OR “pre-morbid” OR “preexisting” OR “pre-existing” OR “previous” OR “baseline”))) AND (“morbidity” OR “mobility impairment” OR “disability” OR “disabilities” OR “dependence” OR “dependent” OR “dependency”)) AND (“reperfusion therapies” OR “reperfusion treatments” OR “endovascular therapy” OR “endovascular treatment” OR “intra-arterial therapy” OR “intra-arterial treatment” OR “endovascular thrombectomy” OR “mechanical thrombectomy” OR “intra-arterial thrombectomy” OR “MT” OR “EVT” OR “IAT”). Our search was last updated on 3 June 2020 to ensure there were no new studies meeting the eligibility criteria.
The records obtained from electronic database searching were imported into the Zotero reference management software (www.zotero.org), and duplicates were removed. Two reviewers independently screened the titles and abstracts of the records for eligibility. Subsequently, all studies deemed eligible according to title and abstract screening were subjected to a full-text review by two independent reviewers. In the case of disagreements about the literature search results, the senior author (M-FY) was consulted to formulate a mutual consensus.
Two reviewers independently extracted the data using a standardized template adapted from the Cochrane Collaboration. Information was collected on study characteristics (first author, year of publication, study period, country of origin, study design, number of institutions, included population, and number of patients), patient characteristics (age, sex, National Institutes of Health Stroke Scale, NIHSS, and Alberta Stroke Program Early CT Score, ASPECTS), and clinical outcomes. When duplicate reports of the same study were found, data from the most complete data set was analyzed. Disagreements were adjudicated by the senior author (M-FY).
Two reviewers independently assessed the quality of observational studies included in this meta-analysis using the Newcastle-Ottawa Scale (NOS) (12). All these studies were reviewed and scored based on the following domains: selection of study groups (0–4 scores), comparability (0–2 scores), and assessment of outcomes (0–3 scores). A maximum number of nine scores could be awarded. Score ≥8 suggested a low risk of bias, 6–7 suggested a moderate risk of bias, and ≤5 suggested a high risk of bias. The potential disagreements were resolved through discussion with the senior author (M-FY).
Stratified by prestroke mRS (mRS 2, 3, 4, and 5), the cumulative percentage and 95% CI for each outcome in patients treated with EVT were evaluated from each cohort. In addition, the effect (risk ratio RR with associated 95% CI) of EVT on outcomes in patients with prestroke disability was studied by meta-analyzing the rates in studies reporting data in patients treated with EVT vs. standard medical treatment. Furthermore, the effect estimates of outcomes were computed by analyzing the event rates in studies reporting data in EVT patients with successful recanalization vs. those without. Random-effect models with the inverse-variance method were used to combine studies to yield the overall effect (13). Statistical significance was determined using the equivalent Z test, with a 2-tailed value of p < 0.05 considered as the significance threshold. Heterogeneity among studies was assessed by the Cochran Q test at a significance level of p < 0.1 and quantified by the I2 statistic. I2-value < 50, 50% ≤ I2-value ≤ 75%, and I2-value > 75% were considered to represent low, moderate, and significant heterogeneity (14). All statistical analyses were conducted with the Cochrane Collaboration's Review Manager Software Package (RevMan 5.3).
The initial search yielded 936 records, of which 291 records were repeats, and 612 records were excluded after reading the titles and abstracts. After reviewing the remaining 33 full-text articles, 12 articles (15–26) met the inclusion criteria. In addition, one relevant study (27) was identified from the updated search. Finally, 13 articles were included in this systematic review and meta-analysis. The screening process and reasons for exclusion are shown in Figure 1.
A total of 13 articles published between 2018 and 2022 were finally included for analysis. All these studies were retrospective observational studies based on prospective databases or prospective registries, and 10 of them were multi-centered. Overall, 2,271 patients underwent EVT, whereas 354 patients were treated with standard medical treatment. Eight studies reported the impact of EVT in a series of patients with prestroke disability stratified by prestroke mRS. Three studies compared the safety and efficacy of EVT and standard medical treatments for patients with pre-stroke disability. Five studies investigated whether successful recanalization would benefit patients treated with EVT. Age, sex, NIHSS, and ASPECTS were comparable for the intervention and control groups (p > 0.05). The characteristics of the included studies are summarized in Table 1.
The quality of all studies included in this systematic review and meta-analysis was considered reasonable. Of the 13 observational studies, six were rated as having a low risk of bias (good quality), and seven were rated as having a moderate risk of bias (fair quality). The results of the bias assessment are shown in Table 2.
Eight of the 13 studies, including 1,530 patients with prestroke disability treated with EVT, reported the distribution of mRS shifts and death at 3 months by prestroke mRS. The overall rate of return to prestroke mRS at 3 months was 20% (mRS = 2; 120/588, 95% CI 17 to 23%, I2 = 0%; Figure 2 and Table 3), 27% (mRS = 3; 218/827, 95% CI 21 to 33%, I2 = 73%; Figure 2 and Table 3), and 31% (mRS = 4; 34/108, 95% CI 22 to 40%, I2=0%; Figure 2 and Table 3), respectively, after EVT. There were only seven patients in the group with prestroke mRS of five, and the overall rate of return to prestroke mRS was 29%. The rate of mortality at 3 months after EVT was 36% (mRS = 2; 203/588, 95% CI 30 to 42%, I2 = 46%; Figure 2 and Table 3), 45% (mRS = 3; 378/827, 95% CI 40 to 49%, I2 = 43%; Figure 2 and Table 3), and 61% (mRS = 4; 66/108, 95% CI 52 to 70%, I2 = 0%; Figure 2 and Table 3), respectively.
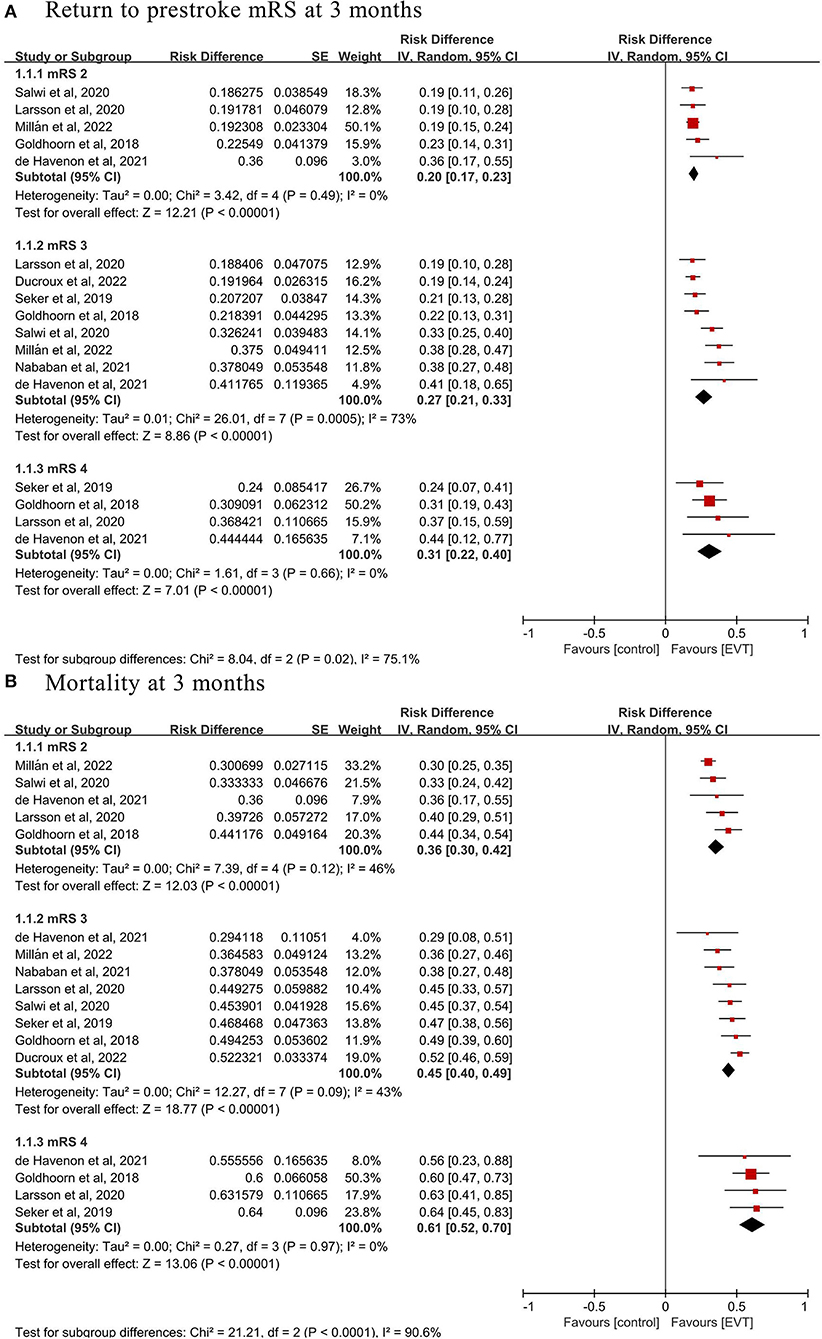
Figure 2. Pooled incidence of (A) return to prestroke modified Rankin Scale (mRS) and (B) mortality at 3 months in prestroke disability patients treated with endovascular thrombectomy (EVT).
Three of the 13 studies, involving 769 patients (415 EVT and 354 standard medical treatments), compared the safety and efficacy between EVT and standard medical treatments for patients with prestroke disability, which were selected for the comparative meta-analysis. The pooled analysis found that EVT was related to a higher likelihood of return to prestroke mRS at 3 months (three studies; RR 1.86, 95% CI 1.28–2.70, p = 0.001, I2 = 53%; Figure 3 and Table 3) and a lower likelihood of mortality at 3 months (three studies; RR 0.75, 95% CI 0.58–0.97, p = 0.03, I2 = 0%; Figure 3 and Table 3) compared with standard medical treatments.
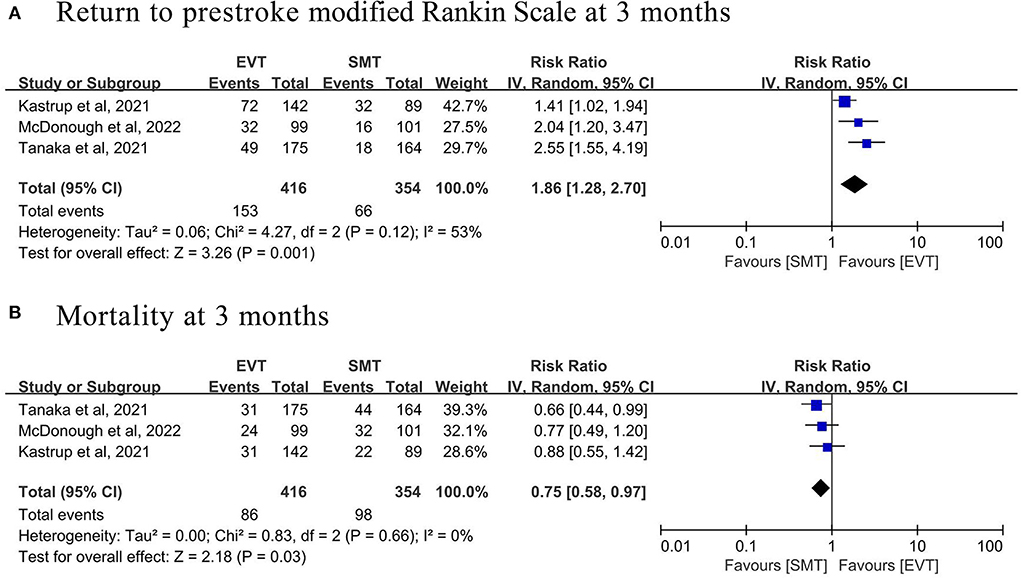
Figure 3. Forest plot of (A) return to prestroke modified Rankin Scale and (B) mortality at 3 months in prestroke disability patients treated with endovascular thrombectomy (EVT) vs. standard medical therapy (SMT).
Five of the 13 studies, involving 887 patients (616 with successful recanalization and 271 with no recanalization), analyzed whether successful recanalization benefited patients with prestroke disability undergoing EVT, which were selected for the comparative meta-analysis. The pooled analysis found that patients with successful recanalization achieved by EVT had a higher proportion of return to prestroke mRS at 3 months (four studies; RR 2.04, 95% CI 1.17–3.55, p = 0.01, I2 = 50%; Figure 4 and Table 3) and lower mortality at 3 months (three studies; RR 0.72, 95% CI 0.62–0.84, p < 0.001, I2 = 0%; Figure 4 and Table 3), compared with patients without successful recanalization.
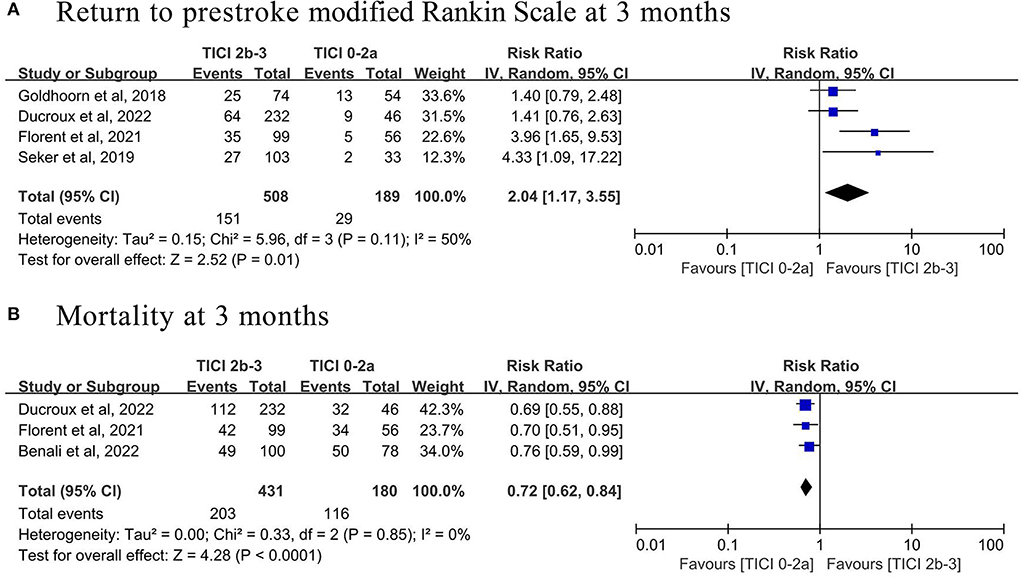
Figure 4. Forest plot of (A) return to prestroke modified Rankin Scale and (B) mortality at 3 months in prestroke disability patients with vs. without successful recanalization (Thrombolysis In Cerebral Ischemia (TICI) 2b-3) after endovascular thrombectomy.
Our meta-analysis of nearly 3,000 acute ischemic stroke patients with prestroke mRS ≥2 showed that (1) the chance of a return to prestroke mRS at 3 months was slightly increased with increasing prestroke mRS and significantly increased mortality was found at 3 months; (2) as compared with patients treated with standard medical treatments, EVT increased the rate of favorable clinical outcomes; and (3) patients with successful reperfusion after EVT had a higher likelihood of returning to prestroke mRS and lower risk of mortality compared with those having no reperfusion.
In general, clinicians do not always consider EVT for eligible ischemic stroke patients with prestroke disability due to the fact that they were more likely to die (6, 28). Our findings were in line with previous studies (28) that showed every point increase in prestroke mRS was associated with a higher risk of mortality (28). However, this association was not explained by the influence of prestroke disability on EVT. The higher mortality would probably be related to prestroke comorbidity and frailty and medical complexity (29, 30). Surprisingly, prestroke disability patients treated with EVT had a higher chance of returning to prestroke mRS with increasing prestroke mRS. Indeed, using typical dichotomy-based definitions of favorable outcomes (e.g., mRS, 0–1, or 0–2) did not show significance in patients with prestroke disability, as it set an unattainable and unjust bar of success. Thus, it may be reasonable for patients with prestroke disability to maintain their premorbid status to be considered favorable outcomes. Although the above results cannot be ascribed to the interaction of prestroke disability and the effects of EVT, there was no association between prestroke mRS and accumulated disability. These data supported a more inclusive EVT selection paradigm with regard to prestroke disability. More importantly, the results of this meta-analysis were in line with other series concerning patients with mRS of 0–1 treated endovascularly (31, 32), which showed that EVT for patients with prestroke disability gave a higher rate of return to prestroke mRS and lower mortality at 3-month follow-up compared with medical management. Our analyses also suggested that successful reperfusion after EVT resulted in a higher likelihood of return to prestroke mRS and a lower risk of mortality compared with those having no reperfusion, in line with evidence suggesting that patients with larger infarct cores may benefit from EVT (33). EVT should be recommended on the basis of evidence from comparative meta-analysis and be considered an effective treatment for acute ischemic stroke.
Current guidelines from the Chinese Stroke Association (1) and the American Heart Association/American Stroke Association (2) suggest that EVT may be reasonable for acute ischemic stroke patients with prestroke mRS ≥2 (class IIb, level of evidence B), whereas the European Stroke Organization (3) does not mention prestroke disability in their guidelines on EVT in acute ischemic stroke due to a lack of trial evidence. We hoped the presented data would prompt the guideline to add a statement that prestroke disability should not be regarded as an exclusion criterion for EVT treatment. Future randomized controlled trials are still needed to validate the efficacy and safety of EVT in stroke patients with prestroke disability. Further studies of deaths and health and social care costs in acute ischemic stroke patients with prestroke disability treated with EVT would also be meaningful, stratified by baseline mRS.
The outcome data, references, and subgroup analyses included in the present meta-analysis were more comprehensive and complete, containing a larger sample size, than those previously published meta-analyses. However, several irresolvable limitations of the present report need to be acknowledged. First, all of the studies included herein were observational, which were susceptible to biases, and limited the validity of our findings. Second, publication bias across individual studies was not evaluated because the recommended minimum of 10 studies per outcome was not met. Third, we could not draw valid conclusions about patients with a prestroke mRS of 5 because EVT was very uncommon in this population. Four, one (25) of the three studies that compared the outcomes between EVT and SMT involved some patients with mRS 1, also limiting the validity of our findings.
The present meta-analysis found that increased prestroke mRS in acute ischemic stroke patients had no association with accumulated disability, despite a higher probability of death. For eligible ischemic stroke patients with prestroke disability, EVT significantly improved clinical outcomes compared with standard medical treatments alone. Successful recanalization increased the probability of return to the prestroke level of disability and lower mortality. These findings show that prestroke disability should not be regarded as an exclusion criterion from EVT practice.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
J-CY and Q-JB: conception and design of the study, acquisition of data, analysis and interpretation of data, and drafting of the article. YG: acquisition of data, analysis and interpretation of data, and drafting of the article. S-JC and J-TZ: acquisition of data and analysis and interpretation of data. QZ and PZ: revising the manuscript critically for important intellectual content. M-FY: the conception and design of the study and revising the manuscript critically for important intellectual content. All authors have read and approved the final version of the manuscript.
This study was supported by the Science and Technology Department of Qinghai Province (No. 2020-ZJ-774).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Liu L, Chen W, Zhou H, Duan W, Li S, Huo X, et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of ischaemic cerebrovascular diseases. Stroke Vasc Neurol. (2020) 5:159–76. doi: 10.1136/svn-2020-000378
2. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. (2019) 50:e344–418. doi: 10.1161/STR.0000000000000211
3. Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, et al. European stroke organization (ESO)- European society for minimally invasive neurological therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg. (2019) 11:535–8. doi: 10.1136/neurintsurg-2018-014568
4. Ganesh A, Luengo-Fernandez R, Pendlebury ST, Rothwell PM. Long-term consequences of worsened post-stroke status in patients with premorbid disability. Stroke. (2018) 49:2430–6. doi: 10.1161/STROKEAHA.118.022416
5. Gumbinger C, Ringleb P, Ippen F, Ungerer M, Reuter B, Bruder I, et al. Outcomes of patients with stroke treated with thrombolysis according to pre-stroke Rankin scale scores. Neurology. (2019) 93:e1834–43. doi: 10.1212/WNL.0000000000008468
6. Salwi S, Niec JA, Hassan AE, Lindsell CJ, Khatri P, Mocco J, et al. Endovascular treatment for acute stroke patients with a pre-stroke disability: an international survey. Front Neurol. (2021) 12:714594. doi: 10.3389/fneur.2021.714594
7. Ganesh A, Fraser JF, Perue GLG, Amin-Hanjani S, Leslie-Mazwi TM, Greenberg SM, et al. Endovascular treatment and thrombolysis for acute ischemic stroke in patients with premorbid disability or dementia: a scientific statement from the American heart association/American stroke association. Stroke. (2022) 53:e204–17. doi: 10.1161/STR.0000000000000406
8. Adamou A, Gkana A, Mavrovounis G, Beltsios ET, Kastrup A, Papanagiotou P. Outcome of endovascular thrombectomy in pre-stroke dependent patients with acute ischemic stroke: a systematic review and meta-analysis. Front Neurol. (2022) 13:880046. doi: 10.3389/fneur.2022.880046
9. Bala F, Beland B, Mistry E, Almekhlafi MA, Goyal M, Ganesh A. Endovascular treatment of acute ischemic stroke in patients with pre-morbid disability: a meta-analysis. J Neurointerv Surg. (2022) 5:8573. doi: 10.1136/neurintsurg-2021-018573
10. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. (2009) 62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006
11. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
12. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
13. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR, A. basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. (2010) 1:97–111. doi: 10.1002/jrsm.12
14. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. (2011). Ailable online at: www.handbook.cochrane.org
15. Goldhoorn RJB, Verhagen M, Dippel DWJ, van der Lugt A, Lingsma HF, Roos YB, et al. Safety and outcome of endovascular treatment in pre-stroke-dependent patients. Stroke. (2018) 49:2406–14. doi: 10.1161/STROKEAHA.118.022352
16. Seker F, Pfaff J, Schönenberger S, Herweh C, Nagel S, Ringleb PA, et al. Clinical outcome after thrombectomy in patients with stroke with premorbid modified rankin scale scores of 3 and 4: a cohort study with 136 patients. AJNR Am J Neuroradiol. (2019) 40:283–6. doi: 10.3174/ajnr.A5920
17. Larsson A, Karlsson C, Rentzos A, Schumacher M, Abrahamson M, Allardt A, et al. Do patients with large vessel occlusion ischemic stroke harboring pre-stroke disability benefit from thrombectomy? J Neurol. (2020) 267:2667–74. doi: 10.1007/s00415-020-09882-5
18. Salwi S, Cutting S, Salgado AD, Espaillat K, Fusco MR, Froehler MT, et al. Mechanical thrombectomy in patients with ischemic stroke with pre-stroke disability. Stroke. (2020) 51:1539–45. doi: 10.1161/STROKEAHA.119.028246
19. de Havenon A, Castonguay A, Nogueira R, Nguyen TN, English J, Satti SR, et al. Pre-stroke disability and outcome after thrombectomy for emergent anterior circulation large vessel occlusion stroke. Neurology. (2021) 97:e1914–9. doi: 10.1212/WNL.0000000000012827
20. Florent EG, Barbara C, Marc F, Maeva K, Fouzi B, Lucie DS, et al. Clinical outcomes and safety of mechanical thrombectomy for acute ischaemic stroke in patients with pre-existing dependency. J Stroke Cerebrovasc Dis. (2021) 30:105848. doi: 10.1016/j.jstrokecerebrovasdis
21. Kastrup A, Roth C, Politi M, Alexandrou M, Hildebrandt H, Schröter A, et al. Endovascular Therapy vs. thrombolysis in pre-stroke dependent patients with large vessel occlusions within the anterior circulation. Front Neurol. (2021) 12:666596. doi: 10.3389/fneur.2021.666596
22. Nababan T, Phillips TJ, Hankey GJ, Crockett MT, Chiu AHY, Singh TP, et al. Mechanical thrombectomy is efficacious in patients with pre-stroke moderate disability. J Med Imaging Radiat Oncol. (2021) 65:858–63. doi: 10.1111/1754-9485.13260
23. Tanaka K, Yamagami H, Yoshimoto T, Uchida K, Morimoto T, Toyoda K, et al. Endovascular therapy for acute ischemic stroke in patients with pre-stroke disability. J Am Heart Assoc. (2021) 10:e020783. doi: 10.1161/JAHA.121.020783
24. Ducroux C, Derex L, Nourredine M, Haesebaert J, Buisson M, Alesefir W, et al. Successful thrombectomy is beneficial in patients with pre-stroke disability: results from an international multicenter cohort study. J Neuroradiol. (2022) 5:6. doi: 10.1016/j.neurad.2022.03.006
25. McDonough RV, Ospel JM, Majoie CBLM, Saver JL, White P, Dippel DWJ, et al. Clinical outcome of patients with mild pre-stroke morbidity following endovascular treatment: a HERMES substudy. J Neurointerv Surg. (2022) 35:8428. doi: 10.1136/neurintsurg-2021-018428
26. Millán M, Ramos-Pachón A, Dorado L, Bustamante A, Hernández-Pérez M, Rodríguez-Esparragoza L, et al. Predictors of functional outcome after thrombectomy in patients with pre-stroke disability in clinical practice. Stroke. (2022) 53:845–54. doi: 10.1161/STROKEAHA.121.034960
27. Benali F, Kappelhof M, Ospel J, Ganesh A, McDonough RV, Postma AA, et al. Benefit of successful reperfusion achieved by endovascular thrombectomy for patients with ischemic stroke and moderate pre-stroke disability (mRS 3): results from the MR CLEAN registry. J Neurointerv Surg. (2022) 25:8853. doi: 10.1136/neurintsurg-2022-018853
28. Quinn TJ, Taylor-Rowan M, Coyte A, Clark AB, Musgrave SD, Metcalf AK, et al. Pre-stroke modified rankin scale: evaluation of validity, prognostic accuracy, and association with treatment. Front Neurol. (2017) 8:275. doi: 10.3389/fneur.2017.00275
29. Fearon P, McArthur KS, Garrity K, Graham LJ, McGroarty G, Vincent S, et al. Pre-stroke modified rankin stroke scale has moderate interobserver reliability and validity in an acute stroke setting. Stroke. (2012) 43:3184–8. doi: 10.1161/STROKEAHA.112.670422
30. Han TS, Fry CH, Gulli G, Affley B, Robin J, Irvin-Sellers M, et al. Pre-stroke disability predicts adverse post-stroke outcome: a registry-based prospective cohort study of acute stroke. Stroke. (2020) 51:594–600. doi: 10.1161/STROKEAHA.119.027740
31. Goyal M, Menon BK, van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomized trials. Lancet. (2016) 387:1723–31. doi: 10.1016/S0140-6736(16)00163-X
32. Lin Y, Schulze V, Brockmeyer M, Parco C, Karathanos A, et al. Endovascular thrombectomy as a means to improve survival in acute ischemic stroke: a meta-analysis. JAMA Neurol. (2019) 76:850–4. doi: 10.1001/jamaneurol.2019.0525
Keywords: ischemic stroke, disability, thrombectomy, outcomes, meta-analysis
Citation: Yang J-C, Bao Q-J, Guo Y, Chen S-J, Zhang J-T, Zhang Q, Zhou P and Yang M-F (2022) Endovascular thrombectomy in acute ischemic stroke patients with prestroke disability (mRS ≥2): A systematic review and meta-analysis. Front. Neurol. 13:971399. doi: 10.3389/fneur.2022.971399
Received: 17 June 2022; Accepted: 19 August 2022;
Published: 15 September 2022.
Edited by:
Ana Catarina Fonseca, University of Lisbon, PortugalReviewed by:
Luis Rafael Moscote-Salazar, Latinamerican Council of Neurocritical Care (CLaNi), ColombiaCopyright © 2022 Yang, Bao, Guo, Chen, Zhang, Zhang, Zhou and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ming-Fei Yang, aWxvdmV5b3VjbXVAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.