
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 11 August 2022
Sec. Stroke
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.946172
Aim: The aim of this study was to assess the relationship of circadian syndrome and stroke.
Methods: We performed a cross-sectional analysis of 11,855 participants from the National Health and Nutrition Examination Survey (NHANES) database between 2005 and 2018, and collected the baseline characteristics. Multivariate logistic regression models were developed to explore the association between circadian syndrome and stroke. Simultaneously, subgroup analyses based on the difference of gender, race, and components associated with circadian syndrome also were performed. The odds ratio (OR) and 95% CI were calculated in this study.
Results: All the participants were divided into the non-stroke group and the stroke group. There were approximately 3.48% patients exclusively with stroke and 19.03% patients exclusively with circadian syndrome in our study. The results suggested that the risk of stroke in patients with circadian syndrome was higher than that in patients without circadian syndrome (OR = 1.322, 95 CI%: 1.020–1.713). Similar associations were found in women with circadian syndrome (OR = 1.515, 95 CI%: 1.086–2.114), non-Hispanic whites with circadian syndrome (OR = 1.544, 95 CI%: 1.124–2.122), participants with circadian syndrome who had elevated waist circumference (OR = 1.395, 95 CI%: 1.070–1.819) or short sleep (OR = 1.763, 95 CI%: 1.033–3.009).
Conclusion: Circadian syndrome was associated with the risk of stroke. Particularly, we should pay more close attention to the risk of stroke in those populations who were female, non-Hispanic whites, had the symptoms of elevated waist circumference or short sleep.
Stroke is the leading cause of mortality and serious long-term disability worldwide and has been considered one of the most prevalent and devastating diseases affecting humanity today (1, 2). According to the report of the Global Burden of Disease, the number of patients who were diagnosed with stroke has continued to increase in recent years, resulting in a significant economic burden (3). Existing evidence suggested the risk factors related to stroke, such as arterial hypertension, dyslipidemia, diabetes mellitus, obesity, sleep disorders (4, 5). A better understanding of the contribution of risk factors to stroke burden is important for effective prevention strategies.
The circadian system plays an important role in human health and metabolism (6). Some poor lifestyles, including sleep disturbances, the use of artificial light, and shift work, have been reported to cause the circadian rhythm disturbances, which have adverse effects on human health (7). Recently, a growing number of studies have focused on the relationship between the circadian system and chronic diseases (8–10). Circadian dysfunction has been proposed and defined as the presence of any four of the following seven traits, including elevated waist circumference, elevated triglycerides, reduced high-density lipoprotein (HDL)-cholesterol, elevated blood pressure, elevated fasting glucose, short sleep duration (<6 h/day), and the depression symptom (7). Shi et al. (11) assessed the association between circadian syndrome and cardiovascular disease (CVD), and the result also suggested that the circadian syndrome was a strong predictor for CVD occurrence. However, to the best of our knowledge, there has been no study that examined the association between circadian syndrome and stroke so far.
Herein, the aim of this study was to explore the correlation between circadian syndrome and the occurrence of stroke, and focusing on the number of symptoms in circadian syndrome. In addition, we performed subgroup analyses based on gender, race, and components associated with circadian syndrome.
All data in this study were derived from the National Health and Nutrition Examination Survey (NHANES) database between 2005 and 2018. NHANES, as a major program of the National Center for Health Statistics (NCHS), aims to evaluate the health and nutrition of adults and children in the United States (12, 13). The survey adopts a complex multistage sampling method every year to extract nationally representative data of ~5,000 people (14). The data collection process in NHANES contained two parts, an in-person interview (including demographic, socioeconomic, dietary, and health-related questions) and a physical examination (including medical, dental, and physiological measurements, as well as laboratory tests) performed in the Mobile Examination Center (MEC) (14, 15). https://www.cdc.gov/nchs/nhanes/about_nhanes.htm.
Our cross-sectional study included 12,826 participants whose surveys included information on stroke history and characteristics of circadian syndrome. Meanwhile, the exclusion criteria were as follows: (1) subjects without the information of height, weight, marital status, the educational level, household income, smoking, and sleep disorders (n = 518); (2) the participants had missing information on heart failure, coronary heart disease (CHD), hypertension, and diabetes mellitus (n = 453). All the participants provided written consent to participate in the NHANES survey, and data collection was approved by the NCHS Research Ethics Review Committee.
We collected the following information in the current study: age (years), gender, body mass index (BMI, kg/m2), race, marital status, the educational level, household income, smoking, sleep disorders, type of dietary intake [dietary fiber, fat, protein, fruit, vegetables, vitamin A (mcg), vitamin C (mg), vitamin D (mg), vitamin E (mg)], the history of diseases [heart failure, CHD, angina, heart disease, hypertension, high cholesterol, diabetes mellitus], biomarkers [total cholesterol (TC, mg/dL), glycosylated hemoglobin (HbA1c, %), LDL (mg/dL), C-reactive protein (CRP, mg/dL)], and circadian syndrome. Sleep duration was assessed by the question, “How much sleep do you usually get at night on weekdays or workdays?” (16). Sleep disorders were identified by the question “Have you ever been told by a doctor or other health professional that you have a sleep disorder?”. The participants who answered “yes” were asked to say the type of sleep disorder (sleep apnea, insomnia, restless legs, and others) (17, 18). Hypertension was defined as systolic blood pressure of ≥140 mmHg and/or diastolic blood pressure of ≥90 mmHg or the using of antihypertensive medications (19).
Having ≥ 4 of the following components was defined as having circadian syndrome (11): elevated waist circumference (≥102 cm in men, ≥88 cm in women), elevated triglycerides (≥150 mg/dL) or the using of lipid-lowering medication, reduced high-density lipoprotein (HDL)-cholesterol (<40 mg/dL in men and <50 mg/dL in women) or the using of lipid-lowering medication, elevated blood pressure (systolic ≥ 130 and/or diastolic ≥85 mmHg) or the using of an anti-hypertensive drug, elevated fasting glucose (≥100 mg/dL) or the using of anti-diabetic medication, short sleep (<6 h/day), depression symptoms [the patient health status questionnaire-9 (PHQ-9) score ≥ 10] (20, 21).
To estimate the association between the symptoms of circadian syndrome and stroke, we defined the circadian syndrome exposure numbers based on the number of components each participant experienced (elevated waist circumference, elevated triglycerides, reduced HDL cholesterol, elevated blood pressure, elevated fasting glucose, short sleep, and depression symptoms): 4 indicated that an exposure of circadian syndrome was composed of four components; 5 indicated circadian syndrome consists of five components; ≥6 represented circadian syndrome had more than six factors. Noteworthily, <4 means that the participants were not defined as circadian syndrome.
The primary outcome of our study was the occurrence of stroke. Stroke was defined as through the question: “Has a doctor or other health professional ever told you that you had a stroke?”. The participant was considered as a stroke victim when the response was “yes” of the question (5, 22).
After weighted analysis, all measurement data were approximately normal distribution. The measurement data were shown by mean ± standard error (Mean ± SE), and the independent-samples t-test was used for the comparison between two groups. The enumeration data were described as the number of cases and the composition ratio [n (%)], comparison between groups adopted χ2 or the Fisher's exact test. Additionally, we also interpolated the missing value by multiple Imputation (R: mice), and the sensitivity analysis after interpolation is shown in Supplementary Table 1.
First of all, we performed the univariate difference analysis in the study. Then, variables with statistical significance in univariate difference analysis were included as covariables in the multivariate logistic regression model to explore the correlation between circadian syndrome and stroke, and assess the association between the number of symptoms of circadian syndrome and stroke. Three models were introduced: Model 1 was the coarse model; Model 2 adjusted age and BMI; Model 3 adjusted age, BMI, race, marital status, the educational level, household income, sleep disorders, heart failure, CHD, angina, heart disease, hypertension, high cholesterol, diabetes mellitus, smoking, the intake of dietary fiber, the intake of protein, the intake of fat, the intake of vitamin D, the intake of vitamin E, the intake of fruits, TC, HbA1c, and LDL. Simultaneously, we also conducted subgroup analyses based on the difference of gender, race, and components associated with circadian syndrome. The odds ratio (OR) and 95% confidence interval (CI) were calculated. SAS (version 9.4) software was used for statistical analyses. All statistical tests were conducted by using bilateral tests. p < 0.05 was considered as statistically significant difference.
After excluding some participants who had the missing information (n = 971), a total of 11,855 eligible participants were enrolled eventually, and they were divided into the non-stroke group (n = 11,443) and the stroke group (n = 412). The incidence of stroke approximately was 3.48% in our study. Baseline characteristics of all the subjects were displayed in Table 1. Overall, the average age was 47.45 ± 0.29 years. Approximately, 2,473 participants were identified as having circadian syndrome, of which 1,614 participants with circadian syndrome were identified by four features, and 711 participants were identified by five features. Moreover, Table 1 also reveals that some variables had statistical significance between the non-stroke group and the stroke group (p < 0.05).
As illustrated in Table 2, the results suggested that the risk of stroke in the patients with circadian syndrome was higher than that in the patients without circadian syndrome (Model 1: OR = 2.050, 95 CI%: 1.587–2.648). After adjusting some covariates, the results of Model 2 (OR = 1.539, 95 CI%: 1.186–1.996) and Model 3 (OR = 1.322, 95 CI%: 1.020–1.713) were similar to those of Model 1. In addition, we also found when the patients with circadian syndrome composed of more than six components, the risk of stroke was 2.591-times higher than the patients with circadian syndrome composed of four components (OR = 3.591, 95 CI%: 1.972–6.538).
Figure 1 indicates the result of subgroup analysis based on the gender. After adjusting covariates, we found that the risk of stroke in the female patients with circadian syndrome was 1.515 times higher than the patients without circadian syndrome (Model 3: OR = 1.515, 95 CI%: 1.086–2.114, p < 0.05). Nevertheless, there was not a statistical significance between male patients with circadian syndrome and stroke (Model 3, p > 0.05). Similarly, from the results of the racial subgroup analysis (Figure 2), the patients with circadian syndrome had a higher risk of stroke than those without circadian syndrome only for non-Hispanic whites (Model 3: OR = 1.544, 95 CI%: 1.124–2.122, p < 0.05). It is worth noting that we also investigated the correlation between stroke and components associated with circadian syndrome. As shown in Figure 3, the results illustrated that the patients with circadian syndrome with the characteristic of elevated waist circumference had higher risk of stroke compared to the normal waist circumference (Model 3: OR = 1.395, 95 CI%: 1.070–1.819, p < 0.05); the patients with circadian syndrome with the characteristic of having short sleep were associated with the higher risk of stroke than those without short sleep (Model 3: OR = 1.763, 95 CI%: 1.033–3.009, p < 0.05).
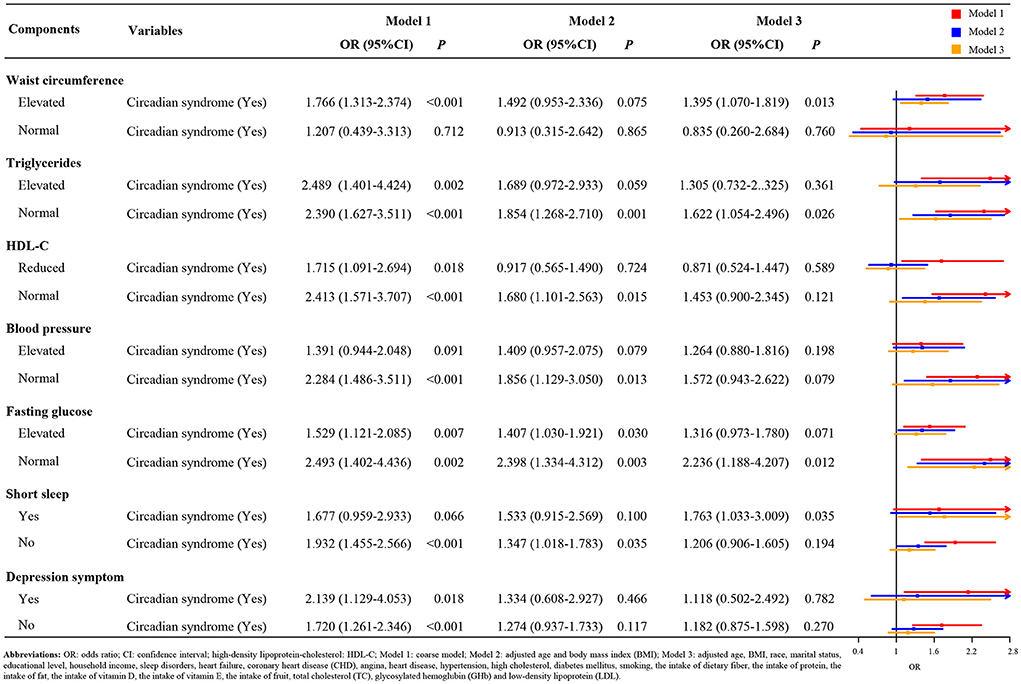
Figure 3. The association of circadian syndrome and stroke based on the components associated with circadian syndrome.
Stroke is recognized as one of the most devastating diseases affecting human civilization, which produced a high effect on the health and quality of life for humans (23). At present, the concept of circadian syndrome has been proposed, which might bring some risk for diseases. However, there were few studies to investigate the association of circadian syndrome and the risk of stroke to date. In this cross-sectional study, the findings showed that circadian syndrome might be associated with the incidence of stroke, especially for female patients with circadian syndrome, non-Hispanic white patients with circadian syndrome, patients with circadian syndrome, who had the characteristic of elevated waist circumference or having short sleep.
To the best of our knowledge, this is the first study conducted to explore the association of circadian syndrome and stroke. Previous studies have only focused on the impact of metabolic syndrome on the risk of stroke (24, 25). However, compared to metabolic syndrome, the circadian syndrome included two components of short sleep and depression symptom. Several reports have illustrated that short sleep and depression symptom could increase the risk of stroke (26, 27). As expected, circadian syndrome was related to the risk of stroke in our study. Because circadian syndrome was defined as meeting at least four characteristics, we discussed the association between the number of characteristics and stroke risk. Interestingly, our study results displayed who patients with circadian syndrome composed of more than six components had a higher risk of stroke compared to the patients with circadian syndrome composed of four components (OR = 3.591, 95 CI%: 1.972–6.538). Although we obtained no significant correlation between patients with circadian syndrome composed of five components and the prevalence of stroke (p > 0.05), the OR suggested that stroke risk in patients with circadian syndrome composed of five components may be higher than the circadian syndrome of four components, lower than the circadian syndrome of six components. This suggests that there might be a positive correlation between the number of components each participant with circadian syndrome and stroke experienced. In other words, the greater the number of matching characteristics in patients with circadian syndrome, the higher the risk of stroke may be. However, more prospective studies are still needed to confirm this positive association.
Additionally, the gender and race differences in the association between circadian syndrome and the risk of stroke were observed in this study. The result indicated that the association was more significant in female patients with circadian syndrome. This may be related to gender differences in arterial structure and function (28). In a stratified analysis of the seven features composed the circadian syndrome, we found that not all factors were associated with the risk of stroke; we guessed that the reason may be related to our sample size. It is important to note that patients with circadian syndrome who had the characteristic of elevated waist circumference or short sleep seem to have higher risk on the occurrence of stroke. These findings indicated that future stroke prevention for patients with circadian syndrome may benefit from improving the sleep duration and shrinking the waist circumference, such as increase physical activity, adhere to a regular schedule, reduce the intake of high-calorie foods, and reduce sedentary time.
This study has some advantages. Firstly, our study included a relatively large sample size, which was sufficient to support our conclusion. Also, gender, race, and components were selected for subgroup analysis to provide a more detailed analysis of the impact of different populations diagnosed with circadian syndrome on the risk of stroke. However, our study has some limitations. Firstly, since this was a cross-sectional study, the causal relationship between circadian syndrome and the risk of stroke cannot be determined in this study. Secondly, we excluded some participants who had the missing information; we are not sure whether these missing cases affected the result of this study. Thirdly, the assessment of sleep duration and stroke relied on the participants' self-reported, which might cause an information bias. Lastly, although our study has a relatively large sample size, it does not support the conclusion which factors constitute a stronger association between circadian syndrome and the risk of stroke. Thus, future studies should investigate the causal relationship between circadian syndrome and the risk of stroke in a large-scale population-based cohort study.
In short, circadian syndrome was associated with the risk of stroke. Of note, we should pay more close attention to the risk of stroke in those populations who are female patients with circadian syndrome, non-Hispanic white patients with circadian syndrome, and patients with circadian syndrome who had the characteristic of elevated waist circumference or having short sleep.
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes/index.htm.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
YW and JL: designed the study. YW: wrote the manuscript. LY and YZ: collected, analyzed, and interpreted the data. JL: critically reviewed, edited, and approved the manuscript. All authors read and approved the final manuscript.
This research was supported by the Hebei Provincial Health Commission (No. 20150716).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.946172/full#supplementary-material
1. Iadecola C, Buckwalter MS, Anrather J. Immune responses to stroke: mechanisms, modulation, and therapeutic potential. J Clin Invest. (2020) 130:2777–88. doi: 10.1172/jci135530
2. Titova OE, Michaëlsson K, Larsson SC. Sleep Duration and stroke: prospective cohort study and mendelian randomization analysis. Stroke. (2020) 51:3279–85. doi: 10.1161/strokeaha.120.029902
3. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. (2020) 76:2982–3021. doi: 10.1016/j.jacc.2020.11.010
4. Li J, Li L, Lv Y, Kang Y, Zhu M, Wang W. Effect of the interaction between depression and sleep disorders on the stroke occurrence: an analysis based on national health and nutritional examination survey. Behav Neurol. (2021) 2021:6333618. doi: 10.1155/2021/6333618
5. Mai X, Liang X. Risk factors for stroke based on the national health and nutrition examination survey. J Nutr Health Aging. (2020) 24:791–5. doi: 10.1007/s12603-020-1430-4
6. Thosar SS, Butler MP, Shea SA. Role of the circadian system in cardiovascular disease. J Clin Invest. (2018) 128:2157–67. doi: 10.1172/JCI80590
7. Zimmet P, Alberti K, Stern N, Bilu C, El-Osta A, Einat H, et al. The Circadian Syndrome: is the Metabolic Syndrome and much more! J Intern Med. (2019) 286:181–91. doi: 10.1111/joim.12924
8. Fodor DM, Marta MM, Perju-Dumbravă L. Implications of circadian rhythm in stroke occurrence: certainties and possibilities. Brain Sci. (2021) 11:865. doi: 10.3390/brainsci11070865
9. Walker WH, Walton JC, DeVries AC, Nelson RJ. Circadian rhythm disruption and mental health. Transl Psychiatry. (2020) 10:28. doi: 10.1038/s41398-020-0694-0
10. Videnovic A, Zee PC. Consequences of circadian disruption on neurologic health. Sleep Med Clin. (2015) 10:469–80. doi: 10.1016/j.jsmc.2015.08.004
11. Shi Z, Tuomilehto J, Kronfeld-Schor N, Alberti GK, Stern N, El-Osta A, et al. The circadian syndrome predicts cardiovascular disease better than metabolic syndrome in Chinese adults. J Intern Med. (2021) 289:851–60. doi: 10.1111/joim.13204
12. Tucker LA. Physical activity and telomere length in U.S. men and women: an NHANES investigation. Prev Med. (2017) 100:145–51. doi: 10.1016/j.ypmed.2017.04.027
13. Taylor MK, Mahnken JD, Sullivan DK. NHANES 2011-2014 reveals cognition of US older adults may benefit from better adaptation to the mediterranean diet. Nutrients. (2020) 12:1929. doi: 10.3390/nu12071929
14. Cai S, Fan J, Zhu L, Ye J, Rao X, Fan C, et al. Bone mineral density and osteoporosis in relation to all-cause and cause-specific mortality in NHANES: a population-based cohort study. Bone. (2020) 141:115597. doi: 10.1016/j.bone.2020.115597
15. Wu CC, Wang CK, Yang AM, Lu CS, Lin CY. Selenium status is independently related to bone mineral density, FRAX score, and bone fracture history: NHANES, 2013 to 2014. Bone. (2021) 143:115631. doi: 10.1016/j.bone.2020.115631
16. Chaudhary NS, Grandner MA, Jackson NJ, Chakravorty S. Caffeine consumption, insomnia, and sleep duration: results from a nationally representative sample. Nutrition. (2016) 32:1193–9. doi: 10.1016/j.nut.2016.04.005
17. Huyett P, Siegel N, Bhattacharyya N. Prevalence of sleep disorders and association with mortality: results from the NHANES 2009–2010. Laryngoscope. (2021) 131:686–9. doi: 10.1002/lary.28900
18. Bansil P, Kuklina EV, Merritt RK, Yoon PW. Associations between sleep disorders, sleep duration, quality of sleep, and hypertension: results from the National Health and Nutrition Examination Survey, 2005 to 2008. J Clin Hypertens (Greenwich). (2011) 13:739–43. doi: 10.1111/j.1751-7176.2011.00500.x
19. O'Shea PM, Griffin TP, Fitzgibbon M. Hypertension: The role of biochemistry in the diagnosis and management. Clin Chim Acta. (2017) 465:131–43. doi: 10.1016/j.cca.2016.12.014
20. Iranpour S, Sabour S. Inverse association between caffeine intake and depressive symptoms in US adults: data from National Health and Nutrition Examination Survey (NHANES) 2005–2006. Psychiatry Res. (2019) 271:732–9. doi: 10.1016/j.psychres.2018.11.004
21. Li W, Taskin T, Gautam P, Gamber M, Sun W. Is there an association among sleep duration, nap, and stroke? Findings from the China Health and Retirement Longitudinal Study. Sleep Breath. (2021) 25:315–23. doi: 10.1007/s11325-020-02118-w
22. Wang L, Li S, Sanika GHA, Zhao J, Zhang H, Zhao L, et al. Association between serum 25-hydroxyvitamin D level and stroke risk: an analysis based on the National Health and Nutrition Examination Survey. Behav Neurol. (2021) 2021:5457881. doi: 10.1155/2021/5457881
23. Aigner A, Grittner U, Rolfs A, Norrving B, Siegerink B, Busch MA. Contribution of established stroke risk factors to the burden of stroke in young adults. Stroke. (2017) 48:1744–51. doi: 10.1161/strokeaha.117.016599
24. Li X, Li X, Lin H, Fu X, Lin W, Li M, et al. Metabolic syndrome and stroke: a meta-analysis of prospective cohort studies. J Clin Neurosci. (2017) 40:34–8. doi: 10.1016/j.jocn.2017.01.018
25. Zhang F, Liu L, Zhang C, Ji S, Mei Z, Li T. Association of metabolic syndrome and its components with risk of stroke recurrence and mortality: a meta-analysis. Neurology. (2021) 97:e695–705. doi: 10.1212/wnl.0000000000012415
26. He Q, Sun H, Wu X, Zhang P, Dai H, Ai C, et al. Sleep duration and risk of stroke: a dose-response meta-analysis of prospective cohort studies. Sleep Med. (2017) 32:66–74. doi: 10.1016/j.sleep.2016.12.012
27. Gill D, James NE, Monori G, Lorentzen E, Fernandez-Cadenas I, Lemmens R, et al. Genetically determined risk of depression and functional outcome after ischemic stroke. Stroke. (2019) 50:2219–22. doi: 10.1161/strokeaha.119.026089
Keywords: circadian syndrome, stroke, correlation, (NHANES) database, symptom
Citation: Wang Y, Yang L, Zhang Y and Liu J (2022) Relationship between circadian syndrome and stroke: A cross-sectional study of the national health and nutrition examination survey. Front. Neurol. 13:946172. doi: 10.3389/fneur.2022.946172
Received: 17 June 2022; Accepted: 18 July 2022;
Published: 11 August 2022.
Edited by:
Mandip Singh Dhamoon, Icahn School of Medicine at Mount Sinai, United StatesReviewed by:
Lyudmila S. Korostovtseva, Almazov National Medical Research Centre, RussiaCopyright © 2022 Wang, Yang, Zhang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junyan Liu, bGp5ZGN0QG91dGxvb2suY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.