
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 14 July 2022
Sec. Neuro-Otology
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.934627
This article is part of the Research Topic Challenges and Current Research Status of Vertigo/Vestibular Diseases View all 39 articles
Background: Dizziness is a common complaint in older adults. To know which factors are instrumental in enabling patients with chronic dizziness to tolerate their symptoms to a certain degree in everyday life can help to develop tailored therapies.
Methods: Data from 358 patients with chronic dizziness and vertigo who had attended a multimodal daycare treatment program were recorded. Data included sociodemographic parameters, dizziness-related characteristics, the Vertigo Symptom Scale (VSS), and the Hospital Anxiety and Depression Scale (HADS). Descriptive statistics, elastic net regression, and mediation analysis were used.
Results: A higher tolerance of dizziness was associated with higher age, higher intensity of dizziness, lower burden of dizziness, higher HADS depression, structural reason for dizziness (type), permanent dizziness, absence of attacks, and longer disease duration. In contrast, younger persons with attack-like dizziness reported to tolerate less dizziness. Age had a significant direct effect on tolerance (72% of the total effect) and a significant indirect effect via intensity on tolerance (28% of the total effect) in the mediation analysis.
Conclusion: It can only be speculated that negative stereotypes about age-related complaints may play a role in this. Why older people tolerate more dizziness and to what extent this may contribute to lower healthcare utilization need to be investigated in further studies.
Vertigo and dizziness have a high lifetime prevalence and affect about 15% to over 20% of adults yearly in large population-based studies (1). They are caused by a variety of conditions and strongly influence activities of daily living and quality of life. Chronic or permanent dizziness often requires a multidisciplinary approach in specialized centers (2, 3) and goes along with high personal and healthcare burden (4). Especially, for chronic dizziness, it is essential that patients cope with the dizziness symptoms in daily living. In many chronic forms of dizziness, this means that patients have to tolerate dizziness to various degrees. The subjective perception of chronic dizziness is influenced by personality traits, psychosocial factors (e.g., anxiety with regard to unforeseeable recurrence), associated symptoms, and the course of disease (unpredictable attacks or permanent problems) (5). With regard to therapeutic approaches, it is crucial to know what factors influence the patient's ability to deal with chronic dizziness.
Every person has different desires and expectations that are usually different from their current state of living. In the context of quality of life, this difference or gap between the hopes/expectations and actual experiences of an individual is called the Calman gap (6). This gap mainly influences the quality of life and individual satisfaction. If the individual's current condition worsens in the context of a disease (e.g., chronic vertigo), then the gap between the current and desired state may increase, thereby lowering the satisfaction of the individual. On the other hand, individuals can adapt their expectations and desires (e.g., tolerate dizziness under some circumstances). Patients can have different understandings of their illness and other reference points, which can change over time or with regard to treatment options. In the case of chronic diseases, patients do not necessarily expect the complaints/symptoms to disappear completely as a result of treatment (6). Rather, patients are willing to tolerate some of the discomfort. In the context of this study, we were interested in understanding which factors are instrumental in enabling patients with chronic dizziness to tolerate their symptoms to a certain degree in everyday life. This should serve as the basis for future studies that aim to adapt therapy programs more individually (e.g., focus on personal resources and resilience). Therefore, our question was how much dizziness intensity can be tolerated by affected persons and what factors modulate this tolerance to dizziness?
Based on theoretical considerations and the existing literature, we considered the following parameters as relevant for our research question. First, we considered the individual intensity of dizziness and the burden due to dizziness as relevant cofactors. These are linked to the type of dizziness (attack vs. permanent) and the dizziness-associated handicap (7–9). Two patient-reported scales have been widely used to evaluate dizziness-associated handicap and severity in patients with vertigo: the Dizziness Handicap Inventory (DHI) and the Vertigo Symptom Scale (VSS) (10, 11). In contrast to the DHI, the VSS assesses the frequency of vestibular-balance symptoms and the severity of autonomic-anxiety symptoms, which have a great impact on quality of life. We therefore used the VSS to comprehensively describe dizziness. We also assumed that the vertigo diagnosis plays a role, in particular, with regard to the distinction between somatic vs. psychic reasons for chronic dizziness (7, 9). Dizziness symptoms are often accompanied and interact with psycho-physiological symptoms, especially depression and anxiety (11–14). Besides anxiety and depression, autonomic symptoms are also known to affect dizziness handicap (15). In addition, age and gender might influence how much dizziness a person is willing to tolerate. It is known from other studies that coping with distinct or multiple diseases is influenced by age and sex (16).
To answer our research question, we analyzed data from patients with chronic dizziness attending our multimodal treatment program in the Center for Vertigo and Dizziness, Jena, Germany (3).
This was a subgroup analysis of a larger longitudinal observational study in people with chronic dizziness attending a specialized vertigo center (17). The study was approved by the local ethics committee (Ethics Committee of the Friedrich-Schiller-University Jena, Number 5426-02/18), and written informed consent for study participation was obtained from all patients. The Center for Vertigo and Dizziness is a tertiary care outpatient project consisting of neurology, ear, nose, and throat and physiotherapy departments. The center provides interdisciplinary diagnoses of patients with chronic vertigo and dizziness and a day care multimodal therapy (2). Requirements for participation in this outpatient treatment program were chronic dizziness and vertigo (i.e., symptoms have persisted for at least 3 months or attacks have recurred at least 5 days per month), physical independence (i.e., walking independently), and no cognitive limitations that may affect the activities of daily living (3). During the study period (June 2013 to September 2017), 754 patients were treated in this therapy program. Six months after attendance of the therapy week, the patients were contacted via mail and asked to fill out questionnaires for follow-up assessment. Here, 444 (58.9%) of the patients completed the questionnaire and sent it back. Comparison between people with and without follow-up is given in Supplement Table S1. From these 444 datasets, 358 provided information about the dependent variable.
The item “Now indicate what intensity of dizziness would be tolerable for you with successful treatment?” (German “Geben Sie jetzt an, welche Schwindelintensität für Sie bei erfolgreicher Behandlung erträglich wäre.”) was rated on a visual analog scale from 0 (no dizziness tolerable) to 10 (the strongest dizziness). This variable is termed “tolerance” (metric).
We assessed the following sociodemographic and vertigo- and dizziness-related data:
• Age (metric; years), gender (binominal; male/female).
• Vertigo diagnosis as defined at our center; advanced neurologists and vertigo specialists medically diagnosed and psychologically evaluated every patient. Diagnoses are generally based on the International Classification of Vestibular Disorders (ICVD) of the Bárány Society.
• Description of symptoms (binominal; the presence or absence of attacks, permanent dizziness/vertigo).
• Duration of symptoms (binominal, 3–6 months, >6 months).
• The intensity of vertigo/dizziness in the last 6 months was quantified using a visual analog scale from 0 (no intensity) to 10 (maximal intensity).
• Burden due to vertigo/dizziness in the last 6 months was quantified using a visual analog scale from 0 (no burden) to 10 (maximal burden; German: “Wie belastet waren Sie durch den Schwindel durchschnittlich in den letzten 6 Monaten?”).
• Hospital Anxiety and Depression Scale (HADS) to estimate depression (18).
• Vertigo Symptom Scale to quantify the symptoms of vertigo and dizziness (19) by vertigo-balance (VSS-V) and autonomic-anxiety (VSS-A) subscale.
All analyses were conducted using IBM SPSS Statistics (version 25), R (version 4.1.1), and Jamovi (Version 1.8.2). Values are the mean and standard deviation (SD) or numbers and percentages. Normal distribution was determined using the Shapiro–Wilk test. Missing data were treated according to the pairwise deletion process. Spearman correlations were used for correlation analyses between different variables. Correlation between subgroups was compared using Fisher's z (20). Elastic net regularization was performed to determine the predictors of the dependent variable (tolerance). Elastic net regularization leads to parsimonious models, which are easier to interpret. Variable selection is performed by shrinking the parameters toward zero and attenuating overfitting, a well-known problem when applying regression models with a large number of predictors. A 10-fold cross-validation was performed to choose the best model with the lowest mean cross-validated error. Within the elastic net algorithm, variables remain in the model if the prediction error averaged over the 10-fold cross-validation samples is reduced. Regression coefficients of the model with confidence intervals (CIs) were reported. Elastic net regularization was performed using the package glmnet in R (version 3.6.2). Finally, a simple mediation model as implemented in Jamovi was used to study the mediating effect of age on tolerance via intensity by using a 1.000 bootstrapping procedure. All statistical tests were applied two-sided at a significance level of 0.05.
Sociodemographic parameters, diagnoses, and vertigo characteristics of the entire cohort are given in Table 1. The distributions of intensity, burden, and tolerance are displayed in Figure 1. The mean difference between the actual intensity of dizziness and the hypothetically tolerated dizziness (tolerance) was 2.0 (SD = 1.93) points on the visual analog scale. This means that patients wished that dizziness is reduced by ~20%.
Spearman correlation between tolerance and independent variables is displayed in Figure 2. Here, tolerance correlated with age, the intensity of dizziness, the burden of dizziness, and HADS depression. In the non-parametric tests, significant group differences for tolerance were found in dizziness type (higher tolerance for organic reasons in comparison to psychic or unspecific vertigo), the permanence of vertigo (higher tolerance in permanent dizziness), attack-like dizziness (lower tolerance for attacks), and duration of dizziness (higher tolerance for longer disease duration), but not for sex (p = 0.63; Figure 3).
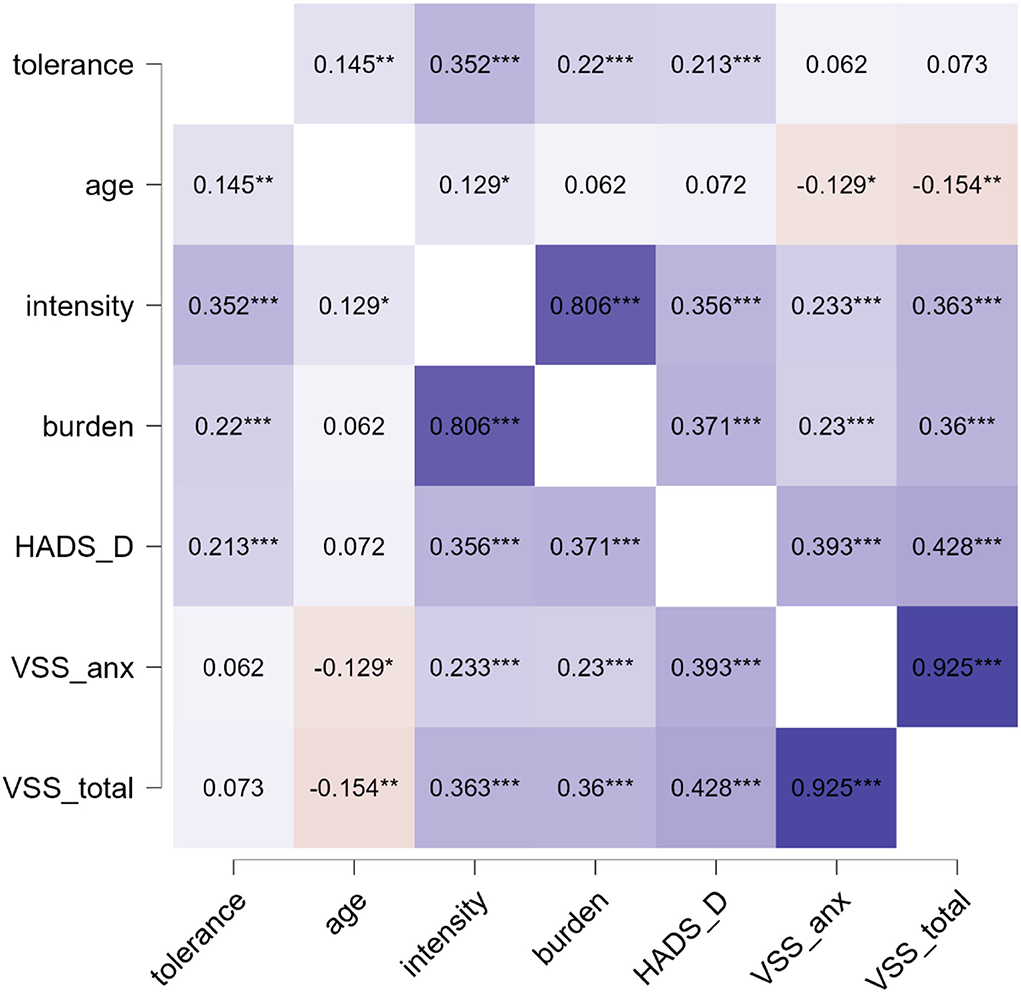
Figure 2. Spearman's rho heatmap. *p < 0.05, **p < 0.01, ***p < 0.001. Blue indicates positive and red indicated negative correlation. HADS, hospital anxiety and depression scale; VSS_anx, vertigo severity scale autonomic-anxiety; VSS_total, total vertigo severity scale.
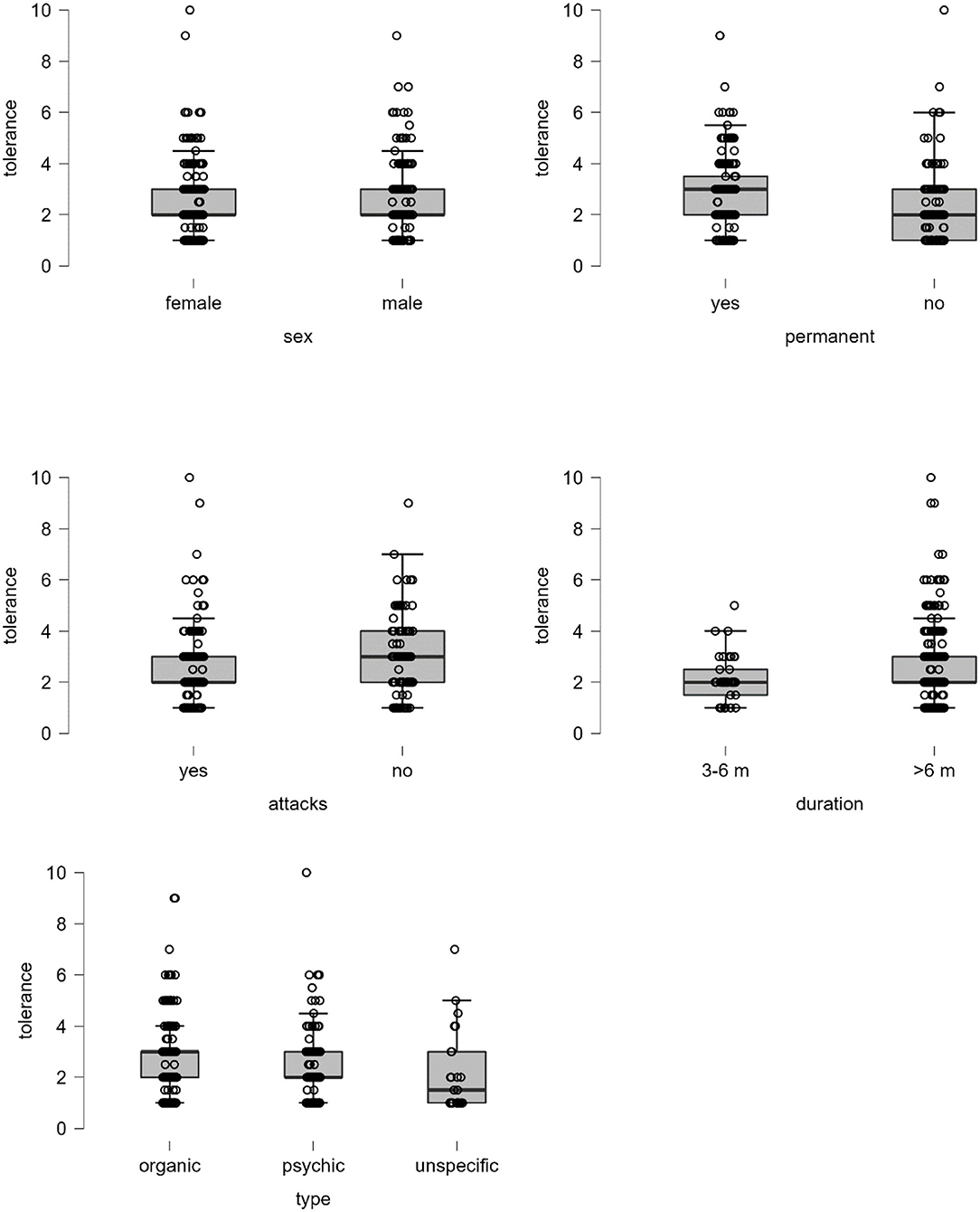
Figure 3. Boxplots for tolerance. Test statistics for Mann–Whitney U-test: sex p = 0.632, permanent p < 0.001, attack p < 0.001, and duration p = 0.026. Test statistic for Kruskal–Wallis test: type p = 0.001, unspecific – psychic p = 0.075, unspecific – organic p = 0.002, psychic – organic p = 0.016.
The significant parameters from univariate analyses were then entered into an elastic-net model. A higher tolerance of dizziness was associated with higher age, higher intensity of dizziness, lower burden of dizziness, higher HADS depression, organic reason for dizziness (type), permanent dizziness, absence of attacks, and longer disease duration (Table 2).
The flexplot in Figure 4 shows that the correlation between tolerance and intensity differed between younger (r = 0.28, p = 0.003), middle-aged (r = 0.226, p = 0.012), and older persons (r = 0.50, p < 0.001). This means that higher intensity of dizziness is related to higher tolerance and this relationship is strongest in older adults (Fisher's z = −1.9780, p = 0.048 for young vs. older; Fisher's z = −2.3824, p = 0.017 for middle-aged vs. older). Given that age is also weakly correlated with intensity (Figure 2), we finally tested if the effect of age on tolerance could be mediated by intensity. Mediation analysis with 1.000 bootstrapping revealed that age had a significant direct effect on tolerance (72% of the total effect) and a significant indirect effect via intensity on tolerance (28% of the total effect; Table 3). Therefore, the effect of age on tolerance occurs mainly independent of the perceived influence.
Dizziness and vertigo are common complaints associated with a substantial individual burden (4, 21–23). It is important to understand the impact of dizziness on individual wellbeing (24). In this study, we investigated which factors influence the ability of patients with chronic dizziness to tolerate their dizziness symptoms in everyday life. Our independent variables included age, sex, common dizziness-related measures, and psychological parameters. In terms of dizziness-related measures, we found that dizziness can be better tolerated when a higher baseline intensity of dizziness is present, when the burden is low, when there is a structural reason for dizziness (type), and when the disease duration is longer. In addition, permanent dizziness is better tolerated than attack-like dizziness. Moreover, we found that dizziness is better tolerated in higher age and people with depressive symptoms. The strongest influence on tolerance has the intensity and burden of dizziness.
When patients were asked how much dizziness was tolerable for them, they indicated on average that 20% less dizziness would be desirable. Only a small proportion stated that dizziness was not tolerable at all (i.e., rated 0 on the visual analog scale). This difference is comparable to the Calman gap, i.e., the difference between the current quality of life and desired quality of life in people with chronic diseases (6). We acknowledge that there are different methods (e.g., Pictorial Representation of Illness and Self Measure) to measure the burden of dizziness (24). However, here we used simple visual analog scales to measure intensity, burden, and tolerance to dizziness in order to get comparable outcome parameters.
The intensity of dizziness/vertigo, age, depression, type of vertigo (somatic vs. non-somatic), and persistence of symptoms (permanent or attack-like) play a role in how much dizziness/vertigo is tolerable. Patients tolerate more dizziness/vertigo with increasing age. This could be demonstrated in the elastic net model after correction for cofactors and in the flexplot (Figure 4). This effect occurred independent from the intensity of dizziness/vertigo, although it is known that dizziness-associated handicap increases with age (25) and older patients with dizziness have less anxiety than younger patients (26).
In an earlier study, we found that younger people were more frequently hospitalized due to dizziness than older adults, and the number of consultations of healthcare providers was considerably higher in younger patients (26). Now, we can hypothesize that a higher tolerance of dizziness increases the threshold to initiate specialized vertigo therapy and could partly explain lower healthcare utilization in older patients. However, why older people tolerate more dizziness and to what extent this may contribute to lower healthcare utilization need to be investigated in further studies. At this point, it can only be speculated that also negative stereotypes about age-related complaints may play a role in this. Many studies provided evidence that ageism affects health outcomes (27–29). For example, when older adults are randomly assigned to a negative-age-stereotype condition, it impairs performance in cognitive tasks (30, 31). However, also age stereotypes that are directed at oneself in old age (self-perceptions of aging) affect functional health (29, 32, 33). Moreover, age stereotypes tend to be resistant to even extremely stressful events (34).
Another influencing factor for higher tolerance may be the finding that anxiety (measured with the VSS) does not play such a prominent role in the older patients with dizziness than in younger patients (3). Instead, we found that depressive symptoms (higher HADS-D) correlate with tolerance. To understand this finding, one has to keep in mind that depressive symptoms also correlate with the current intensity of dizziness. This means that people with depressive symptoms in general rate their current and tolerable dizziness higher in comparison to people with a lower HADS-D (while the gap between both remains stable). Given that older people with chronic dizziness report lower levels of depression and anxiety (26), we assume that the higher tolerance with increasing age occurs independently of these psychological cofactors. Our findings are in line with earlier studies, showing that depression is frequent and clinically relevant in people with dizziness and that depression influences the severity and outcome of dizziness (12, 35–37).
Our study has several limitations. Patients in our sample attended a highly specialized treatment program for chronic dizziness. Thus, there is a selection bias regarding their underlying diagnoses and the findings should be generalized with caution. For example, only a few people had benign paroxysmal positional vertigo (BPPV) in our cohort, a common cause of dizziness among older adults (38). This is because many patients with BPPV were already treated by their general physicians, which makes an appointment in our center not necessary. Patients are referred to our tertiary care center only if symptoms become chronic. Although the response rate to our survey was relatively good for a postal/mail survey, this also limits the generalizability of the results. Our dependent variable was so far not validated. Nevertheless, we assume that a visual analog scale is suitable to track differences in the individual perceptions of illness. It is worth to note that other methods also exist to determine the burden of dizziness (i.e., Pictorial Representation of Illness and Self-Measure) (24) and that the kind of assessment may influence the results. Finally, our analysis is driven by a theoretical selection of independent variables. Further studies are therefore needed to gain a deeper understanding of the relationship between, for example, age and tolerance of dizziness.
The ability to cope and tolerate dizziness depends on the type and presentation of vertigo, age, and psychological comorbidities. Looking at how much dizziness patients can tolerate in order to cope with everyday life could be an interesting approach to develop new therapies. At least this view enriches the mere consideration of the handicap caused by the dizziness. In further studies, our approach could be used to focus more on the resources and resilience of patients in order to strengthen them and thus to cope better with dizziness in everyday life.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics Committee of the Friedrich-Schiller-University Jena, Number 5426-02/18. The patients/participants provided their written informed consent to participate in this study.
TP: design of the study and writing of the paper and analysis. HA: collection of data. HA and SM: revision of the paper. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.934627/full#supplementary-material
1. Neuhauser HK. The epidemiology of dizziness and vertigo. Handb Clin Neurol. (2016) 137:67–82. doi: 10.1016/B978-0-444-63437-5.00005-4
2. Axer H, Finn S, Wassermann A, Guntinas-Lichius O, Klingner CM, Witte OW, et al. Multimodal treatment of persistent postural-perceptual dizziness. Brain Behav. (2020) 10:e01864. doi: 10.1002/brb3.1864
3. Dietzek M, Finn S, Karvouniari P, Zeller MA, Klingner CM, Guntinas-Lichius O, et al. In older patients treated for dizziness and vertigo in multimodal rehabilitation somatic deficits prevail while anxiety plays a minor role compared to young and middle aged patients. Front Aging Neurosci. (2018) 10:345. doi: 10.3389/fnagi.2018.00345
4. Neuhauser HK, Radtke A, von Brevern M, Lezius F, Feldmann M, Lempert T, et al. Burden of dizziness and vertigo in the community. Arch Intern Med. (2008) 168:2118–24. doi: 10.1001/archinte.168.19.2118
5. Duracinsky M, Mosnier I, Bouccara D, Sterkers O, Chassany O, Working Working Group of the Société Française d'Oto-Rhino-Laryngologie (ORL). Literature review of questionnaires assessing vertigo and dizziness, and their impact on patients' quality of life. Value Health. (2007) 10:273–84. doi: 10.1111/j.1524-4733.2007.00182.x
6. Prell T, Teschner U, Witte OW, Kunze A. Current and desired quality of life in people with Parkinson's disease: the calman gap increases with depression. J Clin Med. (2020) 9:E1496. doi: 10.3390/jcm9051496
7. Best C, Tschan R, Eckhardt-Henn A, Dieterich M. Who is at risk for ongoing dizziness and psychological strain after a vestibular disorder? Neuroscience. (2009) 164:1579–87. doi: 10.1016/j.neuroscience.2009.09.034
8. Porter M, Boothroyd RA. Symptom severity, social supports, coping styles, and quality of life among individuals' diagnosed with Ménierè's disease. Chronic Illn. (2015) 11:256–66. doi: 10.1177/1742395314567926
9. Tschan R, Best C, Beutel ME, Knebel A, Wiltink J, Dieterich M, et al. Patients' psychological well-being and resilient coping protect from secondary somatoform vertigo and dizziness (SVD) 1 year after vestibular disease. J Neurol. (2011) 258:104–12. doi: 10.1007/s00415-010-5697-y
10. Jacobson GP, Newman CW. The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg. (1990) 116:424–7. doi: 10.1001/archotol.1990.01870040046011
11. Yardley L, Masson E, Verschuur C, Haacke N, Luxon L. Symptoms, anxiety and handicap in dizzy patients: development of the vertigo symptom scale. J Psychosom Res. (1992) 36:731–41. doi: 10.1016/0022-3999(92)90131-K
12. Best C, Eckhardt-Henn A, Tschan R, Dieterich M. Psychiatric morbidity and comorbidity in different vestibular vertigo syndromes. Results of a prospective longitudinal study over one year. J Neurol. (2009) 256:58–65. doi: 10.1007/s00415-009-0038-8
13. Godemann F, Schabowska A, Naetebusch B, Heinz A, Ströhle A. The impact of cognitions on the development of panic and somatoform disorders: a prospective study in patients with vestibular neuritis. Psychol Med. (2006) 36:99–108. doi: 10.1017/S0033291705005921
14. Godemann F, Siefert K, Hantschke-Brüggemann M, Neu P, Seidl R, Ströhle A, et al. What accounts for vertigo one year after neuritis vestibularis - anxiety or a dysfunctional vestibular organ? J Psychiatr Res. (2005) 39:529–34. doi: 10.1016/j.jpsychires.2004.12.006
15. Piker EG, Jacobson GP, McCaslin DL, Grantham SL. Psychological comorbidities and their relationship to self-reported handicap in samples of dizzy patients. J Am Acad Audiol. (2008) 19:337–47. doi: 10.3766/jaaa.19.4.6
16. Cheng C, Inder K, Chan SW-C. Coping with multiple chronic conditions: an integrative review. Nurs Health Sci. (2020) 22:486–497. doi: 10.1111/nhs.12695
17. Prell T, Finn S, Zipprich HM, Axer H. What predicts improvement of dizziness after multimodal and interdisciplinary day care treatment? J Clin Med. (2022) 11:2005. doi: 10.3390/jcm11072005
18. Andersson E. The Hospital Anxiety and Depression Scale: homogeneity of the subscales. Soc Behav Pers. (1993) 21:197–204. doi: 10.2224/sbp.1993.21.3.197
19. Tschan R, Wiltink J, Best C, Bense S, Dieterich M, Beutel ME, et al. Validation of the German version of the Vertigo Symptom Scale (VSS) in patients with organic or somatoform dizziness and healthy controls. J Neurol. (2008) 255:1168–75. doi: 10.1007/s00415-008-0863-1
21. Neuhauser HK. [Epidemiology of dizziness and vertigo]. Nervenarzt. (2009) 80:887–94. doi: 10.1007/s00115-009-2738-9
22. Ruthberg JS, Rasendran C, Kocharyan A, Mowry SE, Otteson TD. The economic burden of vertigo and dizziness in the United States. J Vestib Res. (2021) 31:81–90. doi: 10.3233/VES-201531
23. Wang X, Strobl R, Holle R, Seidl H, Peters A, Grill E, et al. Vertigo and dizziness cause considerable more health care resource use and costs: results from the KORA FF4 study. J Neurol. (2019) 266:2120–8. doi: 10.1007/s00415-019-09386-x
24. Weidt S, Bruehl AB, Moergeli H, Straumann D, Hegemann S, Büchi S, et al. Graphic representation of the burden of suffering in dizziness patients. Health Qual Life Outcomes. (2014) 12:184. doi: 10.1186/s12955-014-0184-2
25. Wassermann A, Finn S, Axer H. Age-associated characteristics of patients with chronic dizziness and vertigo. J Geriatr Psychiatry Neurol. (2021) 35:580–5. doi: 10.1177/08919887211036185
26. Prell T, Finn S, Axer H. How healthcare utilization due to dizziness and vertigo differs between older and younger adults. Front Med. (2022) 9:852187. doi: 10.3389/fmed.2022.852187
27. Lamont RA, Swift HJ, Abrams D. A review and meta-analysis of age-based stereotype threat: negative stereotypes, not facts, do the damage. Psychol Aging. (2015) 30:180–93. doi: 10.1037/a0038586
28. Meisner BA. A meta-analysis of positive and negative age stereotype priming effects on behavior among older adults. J Gerontol B Psychol Sci Soc Sci. (2012) 67:13–7. doi: 10.1093/geronb/gbr062
29. Westerhof GJ, Miche M, Brothers AF, Barrett AE, Diehl M, Montepare JM, et al. The influence of subjective aging on health and longevity: a meta-analysis of longitudinal data. Psychol Aging. (2014) 29:793–802. doi: 10.1037/a0038016
30. Hehman JA, Bugental DB. Responses to patronizing communication and factors that attenuate those responses. Psychol Aging. (2015) 30:552–60. doi: 10.1037/pag0000041
31. Levy BR, Leifheit-Limson E. The stereotype-matching effect: greater influence on functioning when age stereotypes correspond to outcomes. Psychol Aging. (2009) 24:230–3. doi: 10.1037/a0014563
32. Levy BR, Slade MD, Kasl SV. Longitudinal benefit of positive self-perceptions of aging on functional health. J Gerontol B Psychol Sci Soc Sci. (2002) 57:409–17. doi: 10.1093/geronb/57.5.P409
33. Wurm S, Tesch-Römer C, Tomasik MJ. Longitudinal findings on aging-related cognitions, control beliefs, and health in later life. J Gerontol B Psychol Sci Soc Sci. (2007) 62:156–64. doi: 10.1093/geronb/62.3.P156
34. Levy BR, Slade MD, Chung PH, Gill TM. Resiliency over time of elders' age stereotypes after encountering stressful events. J Gerontol B Psychol Sci Soc Sci. (2015) 70:886–90. doi: 10.1093/geronb/gbu082
35. Eckhardt-Henn A, Best C, Bense S, Breuer P, Diener G, Tschan R, et al. Psychiatric comorbidity in different organic vertigo syndromes. J Neurol. (2008) 255:420–8. doi: 10.1007/s00415-008-0697-x
36. Eckhardt-Henn A, Dieterich M. Psychiatric disorders in otoneurology patients. Neurol Clin. (2005) 23:731–49. doi: 10.1016/j.ncl.2005.01.008
37. Nagarkar AN, Gupta AK, Mann SB. Psychological findings in benign paroxysmal positional vertigo and psychogenic vertigo. J Otolaryngol. (2000) 29:154–8.
Keywords: dizziness, vertigo, older age, depression, mediation
Citation: Prell T, Mendorf S and Axer H (2022) Tolerance to Dizziness Intensity Increases With Age in People With Chronic Dizziness. Front. Neurol. 13:934627. doi: 10.3389/fneur.2022.934627
Received: 02 May 2022; Accepted: 21 June 2022;
Published: 14 July 2022.
Edited by:
Leonardo Manzari, MSA ENT Academy Center, ItalyReviewed by:
Erin Gillikin Piker, James Madison University, United StatesCopyright © 2022 Prell, Mendorf and Axer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tino Prell, dGluby5wcmVsbEB1ay1oYWxsZS5kZQ==; orcid.org/0000-0002-6423-3108
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.