
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Neurol., 24 June 2022
Sec. Endovascular and Interventional Neurology
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.904863
This article is part of the Research TopicEndovascular and Interventional Neurology – Case Report Collection 2022View all 23 articles
Aneurysms arising from the posterior inferior cerebellar artery (PICA) are not rare and may originate from the proximal or peripheral segment of the PICA. However, when the affected PICA is hypoplastic and plexiform, it is difficult to occlude the aneurysm without sacrificing the parent vessel, the PICA. This type of aneurysm is rare, and whether it is safe to occlude the aneurysm and the parent artery, in cases of a ruptured aneurysm of the hypoplastic and plexiform PICA, has not been adequately studied and is still open to debate. In this report, two patients with ruptured aneurysms in the hypoplastic and plexiform PICA were presented. Both patients were admitted to our hospital for subarachnoid hemorrhage. After team discussions between the neurosurgeons and neurointerventionalists, the aneurysm and parent PICA had to be occluded via endovascular treatment under general anesthesia. One of the patients developed postprocedural brainstem infarction and exhibited favorable recovery. The other patient died of pulmonary infection, although improvement in the postoperative state was observed. Although rare, aneurysms can originate from the hypoplastic and plexiform PICA. Occluding the aneurysm and hypoplastic parent PICA via endovascular treatment might be a reasonable option.
The posterior inferior cerebellar artery (PICA) is one of the three most important cerebellar arteries. Aneurysms arising from the PICA are not rare and may be located at its proximal or peripheral segment (1, 2). Generally, due to advancements in endovascular treatment (EVT), coiling the aneurysm while sparing the parent PICA is achievable because the involved PICA is often well-developed (3). However, when the affected PICA is hypoplastic and plexiform, it is difficult to occlude the aneurysm without sacrificing the parent PICA.
This type of aneurysm is rare, and whether it is safe to occlude the aneurysm and parent artery in cases of a ruptured aneurysm of the hypoplastic and plexiform PICA has not been adequately studied and is still open to debate (4, 5). In this report, we report 2 cases of ruptured aneurysms of a hypoplastic and plexiform PICA. Endovascular occlusion of the aneurysms and parent PICAs was performed, and no severe brainstem complications were encountered.
A 53-year-old male suffered a sudden severe headache and vomited 4 h before admission. He was a Chinese patient of Han nationality who was healthy and denied having a history of chronic diseases. He had no history of drug abuse or surgical treatment of craniocerebral disease. Upon admission, a physical examination was performed, and the results were unremarkable, except for nuchal rigidity. Head CT showed subarachnoid hemorrhage (SAH) concentrated at the perimesencephalic cistern with involvement of the fourth ventricle (Figure 1A). CT angiography (CTA) revealed no underlying vascular lesions (Figure 1B). Catheter angiography revealed that the left PICA was hypoplastic and plexiform. Several small arteries originated from the left vertebral artery (VA) near the origin of the PICA. A pseudoaneurysm was located in the hypoplastic and plexiform PICA (Figures 1C,D). His family had no similar diseases.
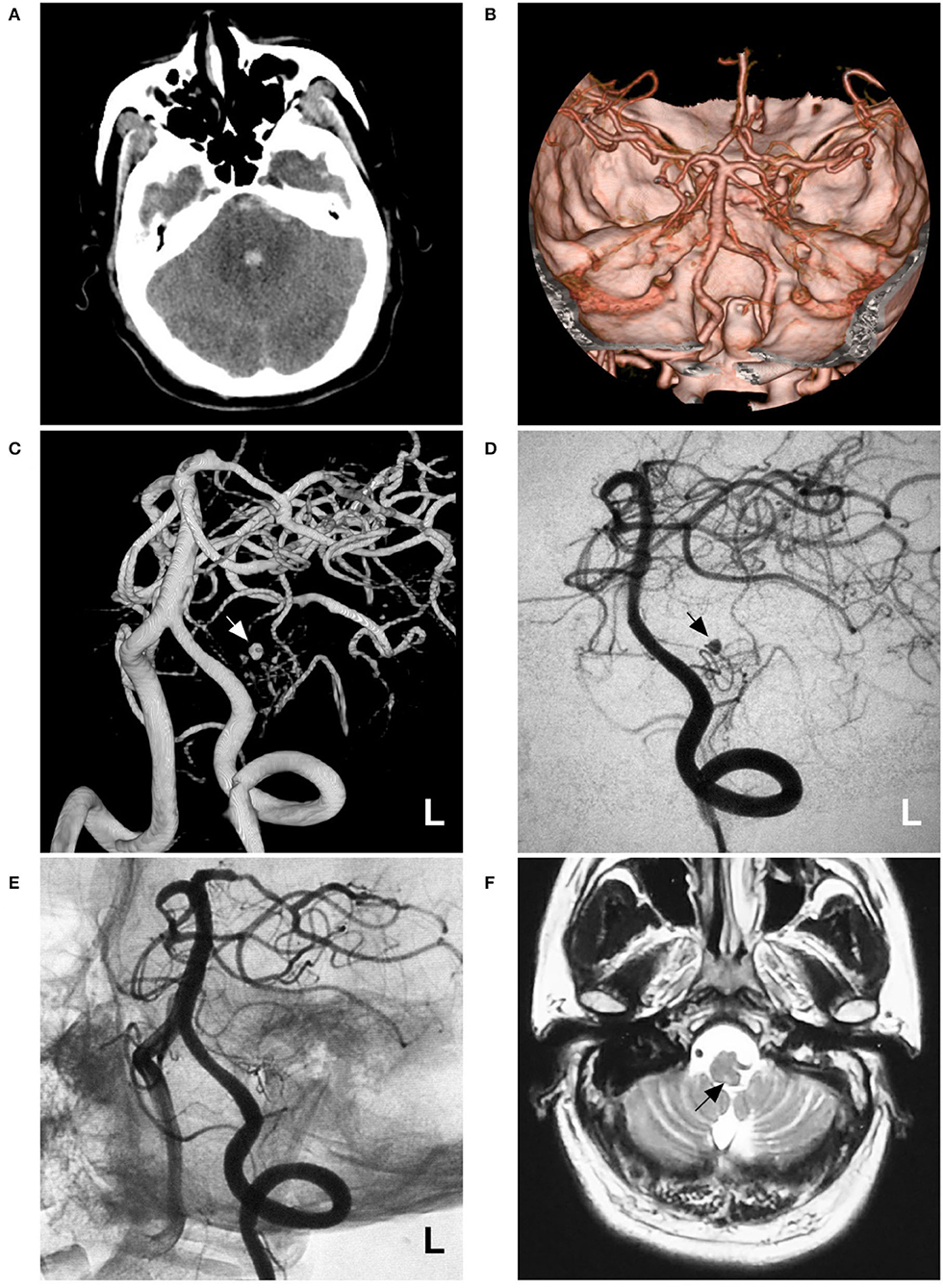
Figure 1. Imaging of case 1. (A) CT shows subarachnoid hemorrhage concentrated at the perimesencephalic cistern with involvement of the fourth ventricle. (B) CTA reveals no underlying vascular lesions. (C,D) Angiograms of the left VA show a pseudoaneurysm (arrow) located in the hypoplastic and plexiform PICA. (C) shows a three-dimensional angiogram, and (D) shows a two-dimensional angiogram. (E) Angiogram of the left VA shows that the aneurysm and parent PICA are cast with Onyx, and other branches are visualized. (F) Follow-up MRI scan shows a minor brainstem infarction (arrow). CT, computed tomography; CTA, CT angiography; L, left; MRI, magnetic resonance imaging; PICA, posterior inferior cerebellar artery; VA, vertebral artery.
Occlusion of the aneurysm and parent PICA via EVT was planned under general anesthesia. During the procedure, a Marathon microcatheter (Medtronic, Irvine, California, USA) was introduced into the PICA via the guidance of a microwire to access the aneurysm as much as possible. Then, the aneurysm and parent PICA were occluded with an Onyx liquid embolic system (Medtronic, Irvine, California, USA) (Figure 1E). Postoperatively, he showed no consciousness or movement disturbance. Mild hoarseness, dysphagia, and left central facial paralysis were noticed. The patient was discharged 1 week later. On follow-up one and a half years later, he recovered significantly, except for mild hoarseness. MRI only revealed the old brainstem infarction (Figure 1F).
A 60-year-old female suffered a sudden onset of headache and vomited 3 h before admission. She was a Chinese patient of Han nationality and had a 10-year history of diabetes, but she had no history of drug abuse or surgical treatment of craniocerebral diseases. On physical examination, she was drowsy. The strength of the four limbs was normal. Head CT showed SAH concentrated at the cisterns around the brainstem and cerebellomedullary cistern (Figure 2A). CTA revealed no vascular abnormalities that might be responsible for the SAH (Figure 2B). Catheter angiography showed that the right PICA was hypoplastic and plexiform. Multiple slim arteries originated from the right VA near the hypoplastic PICA. A pseudoaneurysm was detected in the plexiform PICA (Figures 2C,D). Her family had no similar disease.
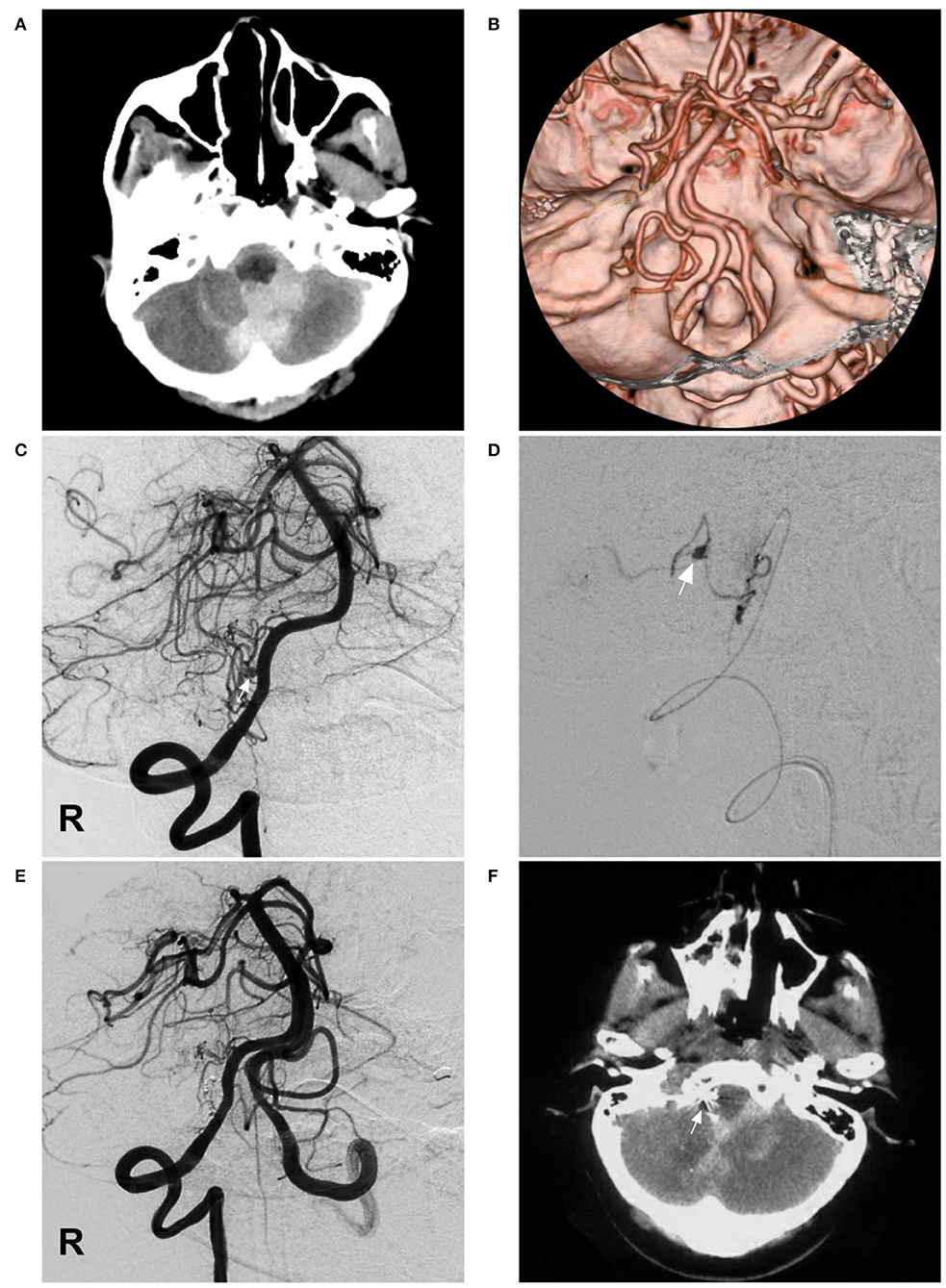
Figure 2. Imaging of case 2. (A) CT shows SAH concentrated at the cisterns around the brainstem and cerebellomedullary cistern. (B) CTA reveals no vascular abnormalities. (C) Angiogram of the right VA shows a pseudoaneurysm (arrow) located in the hypoplastic and plexiform PICA. (D) Superselective angiogram of the right PICA showing the pseudoaneurysm (arrow). (E) Angiogram of the VA shows that the aneurysm and parent PICA were cast with Onyx, and other branches are visualized. (F) Postoperative CT scan shows the location of casting Onyx (arrow) and partial resolution of the SAH. CT, computed tomography; CTA, CT angiography; PICA, posterior inferior cerebellar artery; R, right; SAH, subarachnoid hemorrhage; VA, vertebral artery.
Occlusion of the aneurysm and parent PICA via EVT was planned under general anesthesia. A Marathon microcatheter was advanced to the parent artery of the aneurysm via the guidance of a microwire to access the aneurysm. Then, the Onyx liquid embolic system was cast, successfully occluding the aneurysm and parent PICA (Figure 2E). The patient was stable postoperatively and regained consciousness 1 week later. A head CT scan performed 8 days later showed partial resolution of the SAH (Figure 2F). She was discharged to a local hospital for rehabilitation. A telephone follow-up revealed that she died of pulmonary infection 1 month later at the local hospital.
The PICA is a complex cerebellar artery (6, 7). In 80–95% of the cases, the PICA arises from the intracranial intradural VA. In 5–20% of the cases, the PICA has an extradural origin from the VA; rarely, the PICA may originate from the basilar artery (8). The PICA often begins in a single trunk, and in 2.5–6% of the cases, it begins from the VA as duplicate trunks (9). The PICA may be hypoplastic in 10–32% of the cases and absent on one side in 15–26% of the cases and on both sides in 2% of cases (10).
In hypoplastic PICA, the PICA may be plexiform and arise from the VA, consisting of multiple perforating arteries along the PICA course (8). Among these multiple perforating arteries, the strongest branch can be considered the hypoplastic PICA. These hypoplastic and plexiform PICAs mainly should perforate the brainstem rather than supply the posterior inferior facet of the cerebellum (11).
Aneurysms in hypoplastic and plexiform PICAs are rare entities. These aneurysms are dissecting aneurysms and can transform into pseudoaneurysms after rupture (1). They share the same pathophysiological mechanism with other intracranial perforator aneurysms, including the loss of internal elastic lamina induced by arteriosclerotic, hemodynamic, or inflammatory stress, such as perforating aneurysms in moyamoya disease (12, 13).
The ruptured pseudoaneurysms in hypoplastic PICA should be given aggressive treatment to avoid repeated rupture, including open surgery and EVT. The treatment with open surgery is challenging in the following two aspects: (a) it is difficult to identify the aneurysm intraoperatively, and (b) it is very hard to spare a hypoplastic PICA while occluding the aneurysm (14). Hence, EVT is a reasonable option. However, due to the narrow diameter of the PICA, it is challenging to embolize the aneurysm while sparing the parent PICA.
Therefore, occluding an aneurysm and hypoplastic parent PICA had to be performed. Although occluding an aneurysm and hypoplastic parent PICA is not technically difficult, it is unclear whether it is safe to occlude the hypoplastic PICA (1, 2).
Trivelato et al. reported that 14 patients harboring isolated dissecting aneurysms in the PICA with normal development were assigned to EVT, eight to selective coiling vs. six to parent artery occlusion (PAO). Both techniques were proven effective in preventing rebleeding; however, PAO was significantly associated with a higher risk of ischemic events (15). Based on the experience of the above study, two cases of this report can be tried to perform the occlusion of the hypoplastic and plexiform PICA.
In performing the PAO with the aneurysm in the hypoplastic and plexiform PICA, coiling was difficult to perform because the microcatheter of delivering coils was too thick and stiff, and it was difficult to go further in the hypoplastic PICA. In addition, the coil was too stiff and easily resulted in perforation of the vessel and aneurysm. Therefore, the Onyx liquid embolization system was a good choice. However, the drawback of Onyx is that it sacrifices too many normal vessels. In a previous report, for patients with basilar artery perforated aneurysms, occluding the parent vessel to the perforated aneurysm was acceptable, despite the risk of brainstem stroke in some patients (16).
However, the consequences of occluding a hypoplastic PICA have never been studied. Therefore, we tried to occlude the ruptured aneurysms in the hypoplastic and plexiform PICA because the supply region of the hypoplastic PICA might be compensated by the neighboring arteries and other cerebellar arteries. Although brainstem infarction can occur, we believe the benefits outweigh the risks. After informing the patients and families about surgical plans and risks, the occluding of ruptured aneurysms in hypoplastic and plexiform PICA was performed; fortunately, no severe complications occurred.
Aneurysms in hypoplastic and plexiform PICA were rare. Sometimes, occluding the aneurysm and the hypoplastic parent PICA via EVT had to be the last resort. Because the supply region of the hypoplastic PICA can be compensated by the neighboring arteries, occluding the ruptured aneurysms in the hypoplastic and plexiform PICA may be feasible.
This is a report of two cases, and the conclusion of this study should be cautiously interpreted. In addition, no case of surgical treatment can be provided as a comparison with EVT, which was a limitation of the study.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
JY designed the study and drafted the manuscript. KH collected the data. JY and KH confirm the authenticity of all the raw data. All authors have read and approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Hou K, Guo Y, Xu B, Xu K, Yu J. Delayed establishment of collateral circulation from posterior meningeal artery after proximal occlusion of posterior inferior cerebellar artery: case report and literature review. World Neurosurg. (2018) 115:334–7. doi: 10.1016/j.wneu.2018.04.207
2. Shi L, Xu K, Sun X, Yu J. Therapeutic progress in treating vertebral dissecting aneurysms involving the posterior inferior cerebellar artery. Int J Med Sci. (2016) 13:540–55. doi: 10.7150/ijms.15233
3. Sejkorova A, Petr O, Mulino M, Cihlar J, Hejcl A, Thome C, et al. Management of posterior inferior cerebellar artery aneurysms: what factors play the most important role in the outcome? Acta Neurochir. (2017) 159:549–58. doi: 10.1007/s00701-016-3058-z
4. Kim J, Chang C, Jung YJ. Coil Embolization results of the ruptured proximal posteriori inferior cerebellar artery aneurysm: a single-center 10 years' experience. World Neurosurg. (2018) 117:e645–52. doi: 10.1016/j.wneu.2018.06.105
5. Petr O, Sejkorova A, Bradac O, Brinjikji W, Lanzino G. Safety and efficacy of treatment strategies for posterior inferior cerebellar artery aneurysms: a systematic review and meta-analysis. Acta Neurochir. (2016) 158:2415–28. doi: 10.1007/s00701-016-2965-3
6. Tayebi Meybodi A, Lawton MT, Feng X, Benet A. Posterior inferior cerebellar artery reimplantation: buffer lengths, perforator anatomy, and technical limitations. J Neurosurg. (2016) 125:909–14. doi: 10.3171/2015.8.JNS151411
7. Hou K, Li G, Luan T, Xu K, Xu B, Yu J. Anatomical study of anterior inferior cerebellar artery and its reciprocal relationship with posterior inferior cerebellar artery based on angiographic data. World Neurosurg. (2020) 133:e459–72. doi: 10.1016/j.wneu.2019.09.047
8. Tatit RT, Pacheco C, Aguiar P, Isolan GR, Campero A, Barbo M, et al. The posterior inferior cerebellar artery (PICA): an anatomical and clinical analysis. Turk Neurosurg. (2022) 32:244–50. doi: 10.5137/1019-5149.JTN.33441-20.3
9. Fine AD, Cardoso A, Rhoton AL Jr. Microsurgical anatomy of the extracranial-extradural origin of the posterior inferior cerebellar artery. J Neurosurg. (1999) 91:645–52. doi: 10.3171/jns.1999.91.4.0645
10. Rhoton AL Jr. The cerebellar arteries. Neurosurgery. (2000) 47(3 Suppl.):S29–68. doi: 10.1097/00006123-200009001-00010
11. Lister JR, Rhoton AL Jr, Matsushima T, Peace DA. Microsurgical anatomy of the posterior inferior cerebellar artery. Neurosurgery. (1982) 10:170–99. doi: 10.1097/00006123-198202000-00004
12. Maeda K, Fujimaki T, Morimoto T, Toyoda T. Cerebral aneurysms in the perforating artery manifesting intracerebral and subarachnoid haemorrhage–report of two cases. Acta Neurochir. (2001) 143:1153–6. doi: 10.1007/s007010100006
13. Hou K, Li G, Luan T, Xu K, Yu J. The prospects and pitfalls in the endovascular treatment of moyamoya disease-associated intracranial aneurysms. Neurosurg Rev. (2021) 44:261–71. doi: 10.1007/s10143-020-01261-y
14. Djulejic V, Marinkovic S, Milic V, Georgievski B, Rasic M, Aksic M, et al. Common features of the cerebral perforating arteries and their clinical significance. Acta Neurochir. (2015) 157:743–54; discussion 54. doi: 10.1007/s00701-015-2378-8
15. Trivelato FP, Salles Rezende MT, Castro GD, Manzato LB, Santoro Araujo JF, Ulhoa AC. Endovascular treatment of isolated posterior inferior cerebellar artery dissecting aneurysms: parent artery occlusion or selective coiling? Clin Neuroradiol. (2014) 24:255–61. doi: 10.1007/s00062-013-0247-5
Keywords: posterior inferior cerebellar artery, hypoplastic, plexiform, aneurysm, endovascular treatment, subarachnoid hemorrhage
Citation: Hou K and Yu J (2022) Case Report: Can Ruptured Aneurysms in the Hypoplastic and Plexiform Posterior Inferior Cerebellar Arteries Be Safely Occluded? Front. Neurol. 13:904863. doi: 10.3389/fneur.2022.904863
Received: 28 March 2022; Accepted: 30 May 2022;
Published: 24 June 2022.
Edited by:
Osama O. Zaidat, Northeast Ohio Medical University, United StatesReviewed by:
Luis Rafael Moscote-Salazar, Latinamerican Council of Neurocritical Care (CLaNi), ColombiaCopyright © 2022 Hou and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinlu Yu, amx5dUBqbHUuZWR1LmNu; amlubHV5dUBob3RtYWlsLmNvbQ==
†ORCID: Kun Hou orcid.org/0000-0001-7112-7883
Jinlu Yu orcid.org/0000-0003-2329-7946
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.