- 1Department of Rehabilitation Medicine, Tianjin Medical University General Hospital, Tianjin, China
- 2Department of Neurology, Tianjin Medical University General Hospital, Tianjin, China
- 3Laboratory of Epidemiology, Tianjin Neurological Institute, Tianjin, China
- 4Key Laboratory of Post-Neuroinjury Neuro-Repair and Regeneration in Central Nervous System, Tianjin Neurological Institute, Ministry of Education and Tianjin City, Tianjin, China
- 5Center of Clinical Epidemiology and Evidence-Based Medicine, Tianjin Jizhou People's Hospital, Tianjin, China
- 6Department of Acupuncture, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine & National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion, Tianjin, China
- 7Department of Cardiology, Tianjin Medical University General Hospital, Tianjin, China
- 8Department of Neurosurgery, Tianjin Jizhou People's Hospital, Tianjin, China
- 9Department of General Medicine, Tianjin Medical University General Hospital, Tianjin, China
The burden of cognitive impairment and dementia is particularly severe in low- and middle-income countries. Although hypertension is an important risk factor for cognitive impairment, the influence of different hypertension classification on cognitive impairment remains controversial. To explore the impact of hypertension and hypertension classification on cognitive function, this study was based on a low-income population aged over 60 years in northern China. This population-based, cross-sectional study was conducted from April 2014 to January 2015 in rural areas of Tianjin, China. A total of 1,171 participants aged ≥ 60 years were included. Participants were interviewed by professional researchers face-to-face, using the pre-designed questionnaire. Cognitive function was assessed using the Mini-mental State Examination (MMSE). Multivariate regression analysis was used to calculate the odds ratio (OR) value. There was a significant association between hypertension and cognitive impairment (OR, 1.415; 95% CI: 1.005–1.992; P = 0.047) and a significant positive association between stage 3 hypertension (OR, 1.734; 95% CI: 1.131–2.656; P = 0.012) and the prevalence of cognitive impairment. To prevent dementia, clinicians should consider the cognitive function and blood pressure control of low-income individuals aged over 60 years with hypertension in northern China, especially those with stage 3 hypertension. In addition, the inconsistent effects of blood pressure on different cognitive functions should also be considered; special attention should be paid to orientation and concentration.
Introduction
Hypertension is a major risk factor for cognitive decline and dementia (1). However, the claim that lowering blood pressure reduces the risk of cognitive impairment remains controversial. Some studies report that controlling blood pressure can effectively reduce the risk of cognitive decline (1, 2). Regardless, using a systolic blood pressure target of <120 mmHg in patients with hypertension does not significantly reduce the risk of dementia compared to that of 140 mmHg (3). Similarly, the Secondary Prevention of Small Subcortical Strokes Trial (SPS3 trial) indicated that short-term blood pressure-lowering treatment does not improve the cognitive function of patients with lacunar stroke aged over 60 years (4). Previous studies have also shown a U-shaped relationship between blood pressure and cognition, with either high or low blood pressure adversely affecting cognition (5, 6). Accordingly, the relationship between blood pressure and brain health is complex. The age of hypertension onset and the use of antihypertensive drugs can both affect the impact of blood pressure on cognition (2, 7, 8). The above studies suggest the need for further research regarding the impact of blood pressure classification on cognition.
Moreover, more than 50 million people worldwide suffer from dementia, and the number of patients is expected to triple by 2050 (9). Notably, about two-thirds of individuals with dementia live in low- and middle-income countries, which exerts a heavy medical burden for these countries (10). Furthermore, the prevalence of hypertension is higher in low- and middle-income countries (1), whereas the awareness rate and control rate of hypertension is low (11, 12).
Thus, this study focused on a low-income population in China to study the impact of hypertension classification on cognitive function. These findings will provide some theoretical basis regarding the control of hypertension for the prevention of dementia in low- and middle-income countries.
Materials and Methods
Patient Selection
This was a population-based, cross-sectional study conducted from April 2014 to January 2015 in rural areas of Tianjin, China. The participants were from a sub-cohort of the Tianjin Brain Study (13, 14), which has been described previously. Briefly, approximately 95% of the individuals in this study reported a 2014 disposable income per capita of <1,600 USD (15). All residents aged 60 years and older without vision or auditory dysfunction were recruited. Individuals with history of myocardial infarction, stroke, congenital hypophrenia, traumatic brain injury, and mental illness were excluded.
The study was approved by the Ethics Committee at Tianjin Medical University General Hospital to conform to the Declaration of Helsinki regarding use of human subjects (IRB2018-100-01), and written informed consent was obtained from each patient during recruitment.
Risk Factors and Physical Examinations
The specific information collected and the associated processes have been described in detail (14). Using pre-designed questionnaires, uniformly trained investigators collect participants' information through face-to-face interviews. Demographic information included name, sex, date of birth, and education level; personal history included the presence of hypertension and diabetes and lifestyle factors (including smoking and drinking). Physical examination included height, weight, waist circumference, hip circumference, blood pressure, and heart rate.
Fasting blood glucose, total cholesterol, triglyceride, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol were measured at the Central Laboratory of Tianjin Jizhou People's Hospital.
Definitions
Hypertension was defined as a history of hypertension self-reported by the subject and in the medical records of the health center, or the mean systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥ 90 mmHg of two measurements of blood pressure at rest; or the patient was taking antihypertensive drugs (16). Stage of hypertension was defined according to the 2018 Chinese hypertension guideline (17): stage 1, systolic blood pressure 140–159 mmHg or diastolic blood pressure 90–99 mmHg; stage 2, systolic blood pressure 160–179 mmHg or diastolic blood pressure 100–109 mmHg; stage 3, systolic blood pressure ≥180 mmHg or diastolic blood pressure ≥ 110 mmHg or the use of antihypertensive medications. Diabetes was defined as a fasting blood glucose ≥7.0 mmol/L and diagnosed by a superior hospital, taking medication for diabetes, or a self-reported history of diabetes. Smoking was defined as smoking ≥1 cigarette daily for more than 1 year. Alcohol intake was defined as drinking >50 mL of alcohol at least once per week for more than 6 months. Moreover, the participants were categorized into four age groups (60–64, 65–69, 70–74, and ≥75 years) and three educational groups according to the length of formal education [0–5 (illiterate), 6–8 (primary school), and ≥9 years (junior high school and above)].
Cognitive Function Screening
The Mini-mental State Examination (MMSE) was used to assess the cognitive function of study participants (18). Cognitive impairment was defined in association with education level: MMSE score <17 points in the illiterate group, <22 points in the primary school group, and <26 points in the junior high school and above group (19).
Statistical Analysis
Continuous variables are described as means and standard deviations. Categorical variables are presented as numbers with frequencies, and the chi-squared test was performed to compare the differences between two groups in the univariate analysis. Risk factors for cognitive dysfunction were studied using multivariate logistic regression analysis, with independent variables selected as statistically significant factors in univariate analyses. A linear regression model was used to test the correlation of multidimensional MMSE score and hypertension (yes or no)/blood pressure classification, and score of multidimensional MMSE as the dependent variable. The independent variables in the regression model were found to be statistically significant in the multivariate analysis as well as to test the correlation of cognitive score and hypertension/blood pressure grading, which was adjusted according to age, sex, education, and drinking history. All statistical analyses were performed using SPSS version 25.0 statistical software (SPSS Inc., Chicago, IL), and a two-sided P ≤ 0.05 was considered as statistically significant.
Results
During 2001-2012, total 2,442 residents aged ≥ 60 years old were qualified in this population. Of these, 839 residents with previous stroke, Audio-visual obstacles, traumatic brain injury, congenital hypophrenia, and psychosis were excluded in this study; 474 elderly who did not participant the questionnaire survey and physical examination were excluded in this study; 46 elderly refused evaluate of MMSE and 32 elderly without completed data of physical examination. Finally, 1,171 elderly were assessed in this study (Figure 1).
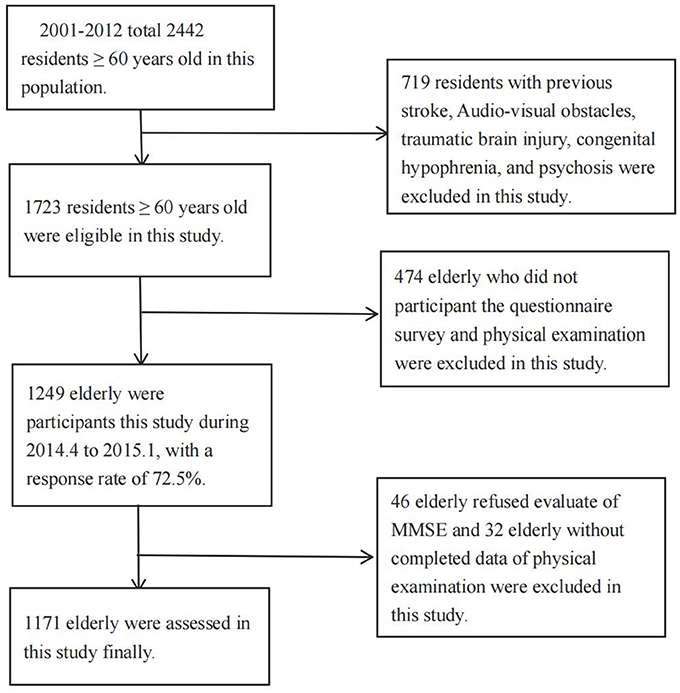
Figure 1. Flow chart of participants. 2001-2012 total 2,442 residents ≥ 60 years old in this population. Eight hundred and thirty nine residents with previous stroke, Audio-visual obstacles, traumatic brain injury, congenital hypophrenia, and psychosis were excluded in this study; 474 elderly who did not participant the questionnaire survey and physical examination were excluded in this study; 46 elderly refused evaluate of MMSE and 32 elderly without completed data of physical examination. Finally, 1,171 elderly were assessed in this study.
Baseline Characteristics
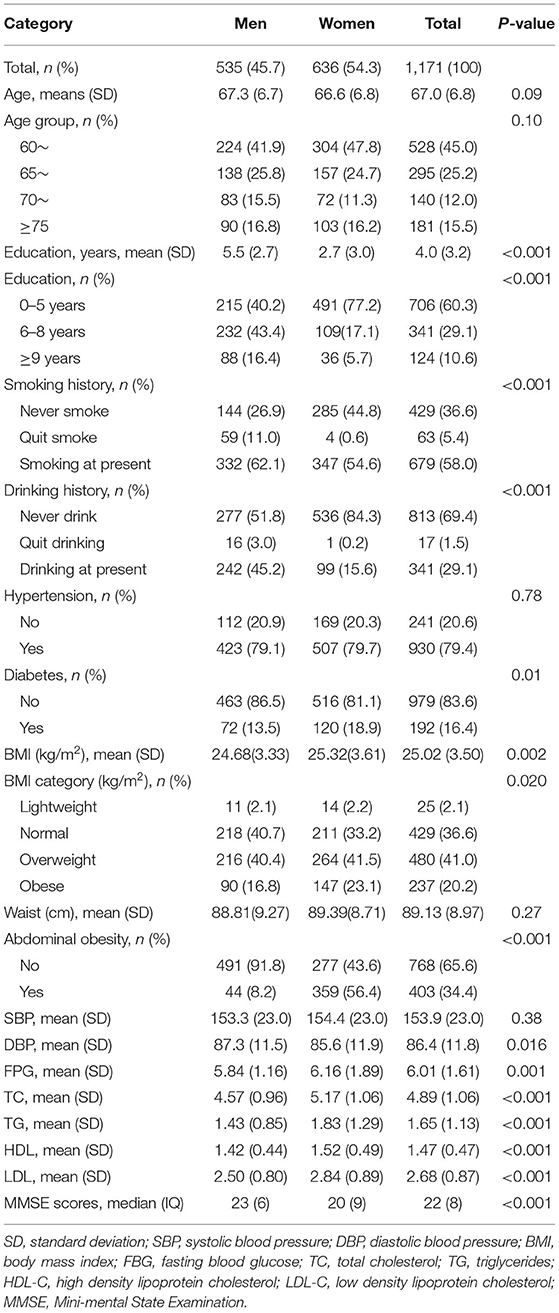
Among 1,171 participants, 45.7% were male, and 54.3% were female. The mean age (standard deviation) was 66.84 years overall, 67.31 years for male participants, and 66.64 years for female participants (P > 0.05). The average educational level was 3.95 years overall, 5.45 years for male participants, and 2.69 years for female participants (P < 0.05). In addition, 60.5% had 0–5 years of education, 29.6% had 6–8 years, and 9.9% had ≥ 9 years; The proportion of residents with no education was 27.8%. The prevalence of cognitive impairment was 32.4% overall, 25.6% for male participants, and 38.1% for female participants. The prevalence of hypertension was 79.4%, diabetes 16.4%, obesity 20.2%, abdominal obesity 34.4%, smoking 58.0%, drinking 29.1%, respectively (Table 1).
Influence of Hypertension on Cognitive Impairment in Multivariate Analysis
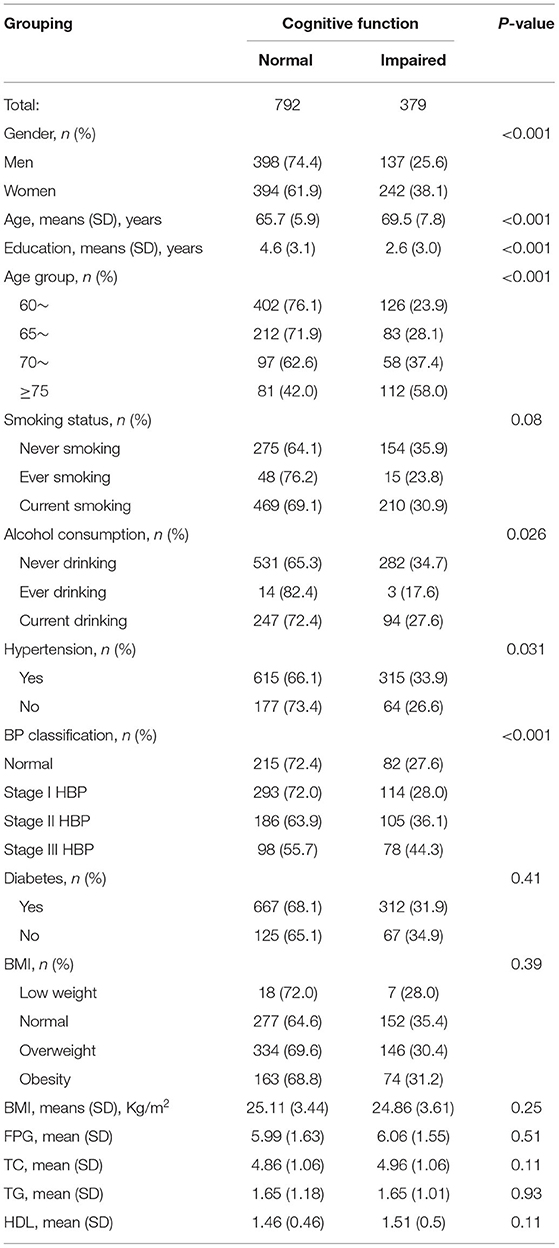
The multivariate analysis was adjusted for age group, sex, drinking history, and education level, which were associated factors of cognitive impairment in the univariate analysis (Table 2).
Figure 2 shows a significant difference between hypertension and cognitive impairment (odds ratio, 1.42; 95% confidence interval: 1.01–1.99; P = 0.047). Compared with normal blood pressure, there were no significant differences between stage 1 hypertension (P = 0.84) and stage 2 hypertension (P = 0.05) and the prevalence of cognitive impairment; in contrast, there was a significant positive correlation between stage 3 hypertension (odds ratio, 1.73; 95% confidence interval: 1.13–2.66; P = 0.012) and the prevalence of cognitive impairment.
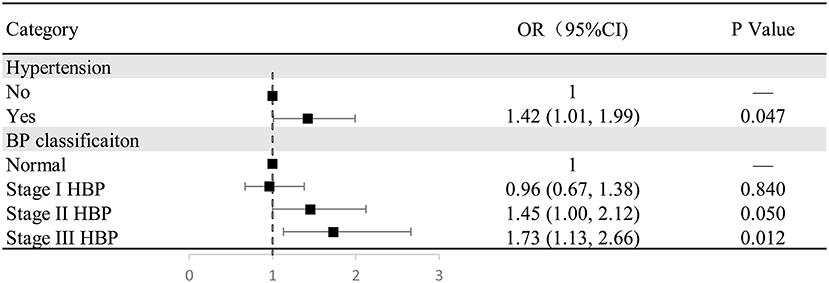
Figure 2. The relationship between hypertension/hypertension classification and cognitive impairment in the multivariate analysis. Figure shows a significant difference between hypertension and cognitive impairment (odds ratio, 1.42; 95% confidence interval: 1.01–1.99; P = 0.047). Compared with normal blood pressure, there were no significant differences between stage 1 hypertension (P = 0.84) and stage 2 hypertension (P = 0.05) and the prevalence of cognitive impairment; in contrast, there was a significant positive correlation between stage 3 hypertension (odds ratio, 1.73; 95% confidence interval: 1.13–2.66; P = 0.012) and the prevalence of cognitive impairment.
Influence of Hypertension on Cognitive Score in Multivariate Analysis
The hypertension and blood pressure classification were both included in one model, which is mainly adjusted for age group, sex, drinking history, and education. There was a significant association of both hypertension and blood pressure classification with MMSE score (P < 0.05). In addition, scores for orientation, attention and calculation, and language significantly decreased by 0.24, 0.23, and 0.27 points, respectively, in the hypertension group compared with the non-hypertension group (all P < 0.05). Similarly, compared with the normal blood pressure classification, with each increase in the blood pressure classification, scores for orientation, attention and calculation, and language significantly decreased by 0.13, 0.18, and 0.18 points, respectively, (all P < 0.05). However, registration and recall scores were not associated with hypertension and blood pressure classification (Figure 3).
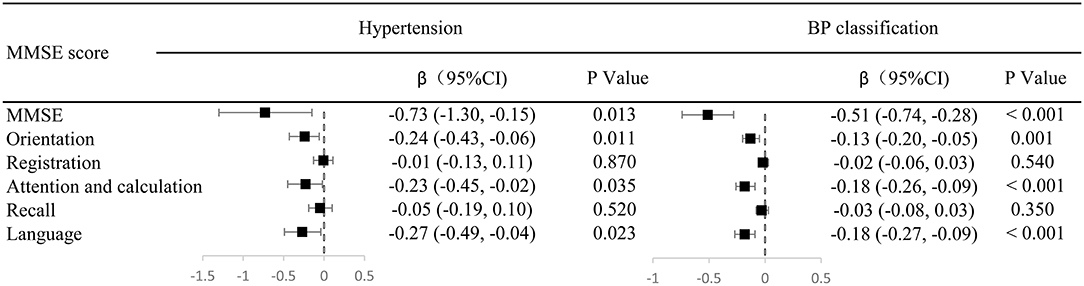
Figure 3. Odd ratios of cognitive function in hypertension and blood pressure grading in multivariate analysis. The hypertension and blood pressure classification were both included in one model, which is mainly adjusted for age group, sex, drinking history, and education. There was a significant association of both hypertension and blood pressure classification with MMSE score (P < 0.05). In addition, scores for orientation, attention and calculation, and language significantly decreased by 0.24, 0.23, and 0.27 points, respectively, in the hypertension group compared with the non-hypertension group (all P < 0.05). Similarly, compared with the normal blood pressure classification, with each increase in the grade of hypertension, scores for orientation, attention and calculation, and language significantly decreased by 0.13, 0.18, and 0.18 points, respectively, (all P < 0.05). However, registration and recall scores were not associated with hypertension and blood pressure classification.
Discussion
This study focused on the relationship of hypertension and blood pressure classification with cognitive function among a low-income elderly population in rural areas of northern China. In this study, the prevalence of cognitive impairment in the hypertension group and the stage 3 hypertension group increased 41.5 and 73.4%, respectively, compared to that in the non-hypertension group. Further analysis showed that compared with the normal blood pressure group, the orientation, attention and calculation, and language scores of the hypertension group decreased by more than 0.2 points. With each increase in hypertension stage, scores for MMSE decreased by more than 0.5 points. The uniqueness of this work is that it is based on a low-income population in northern China and that blood pressure classification were used to further understand the relationship between blood pressure and different cognitive functions.
Relationship Between Hypertension and Cognitive Impairment
As early as the 1950's and 1960's, some scholars began to systematically study the impact of hypertension on cognitive function (20, 21). Previous studies showed that hypertension can cause a decline in cognitive function, and hypertension with onset in middle ages has the strongest impact on the cognition in elderly individuals (22–25). Consistent with the results of previous studies, compared with individuals with normal blood pressure, the prevalence of cognitive impairment in individuals with hypertension is significantly higher by 41%. The contribution of the present study to the literature is that analyzing by blood pressure classification shows that only stage 3 hypertension is associated with increased prevalence of cognitive impairment. However, the relationship between blood pressure and cognition cannot be generalized, and there may be a non-linear dose-response relationship (26). Another study indicated that among ambulatory adults with hypertension, controlling the target systolic blood pressure below 120 mmHg will not significantly reduce the risk of dementia compared with 140 mmHg (27). In adults with hypertension, decreased renal function as measured by the estimated glomerular filtration rate is associated with increased risk of dementia; nevertheless, intensive hypertension treatment did not reduce the risk (28). This may be related to the relationship between blood pressure and cerebral perfusion, wherein after intensive blood pressure reduction, hypotension and cerebral hypoperfusion may negatively impact the brain cognitive function (29, 30). Therefore, physicians should targeted intervention blood pressure levels in patients with grade 3 hypertension to reduce the negative effects of blood pressure on cognition in an elderly population.
Hypertension and Different Cognitive Functions
Hypertension is related to almost all areas of cognitive function (31). However, blood pressure affects white matter volume in frontal lobes higher than in occipital, parietal, and temporal lobes (32, 33). Recent studies have shown a larger volume of deep forehead white matter hyperintensities among hypertensive patients (34), which are related to worse scores on cognitive tests of memory (pairs matching), executive function (tower rearranging), and reasoning (matrix pattern) (35). In the current study, the orientation, attention and calculation, and language scores of hypertensive patients were significantly reduced. This may be because different brain tissues have different sensitivity to blood pressure (36), and more in-depth research on the effect of blood pressure grading on brain tissue is necessary.
Hypertension is a major risk factor for vascular dementia (37, 38). Previous studies have shown that changes in blood pressure are associated with changes in cerebral perfusion and metabolism (5, 39, 40). Neurovascular units within the vascular region and the entire brain can respond to changes in blood pressure and increased metabolic demands. But endothelial dysfunction associated with hypertensive patients underlies altered neurovascular coupling and a local decrease in vasomotor reserve (39). Furthermore, increased vascular endothelial oxidative stress and inflammation caused by hypertension lowers the intrinsic threshold for cell survival (39). Therefore, the effect of blood pressure on cognition may be accomplished through multiple pathways.
There are some limitations in this study. Firstly, this study was a single-center cross-sectional study with limited population representation, and the relationship between hypertension and cognition is only a correlation, not a causal relationship. Secondly, this study did not evaluate the effect of hypertension medication on cognitive function, but the rates of awareness of hypertension and of hypertension medications in the study population was low (41), thus the effect of antihypertensive drugs on cognition may be small in this study. Third, in this study, the MMSE score was used to assess the cognitive function of the participants. Although the MMSE did not reveal impaired cognitive function of patients with higher education (42), the study population was low-income and low-educated, with an average education level of just 3.95 years; thus, the screening for cognitive impairment was accurate. Fourth, the effect of hypertension and blood pressure classification on the MMSE score in this study was only 0.5 points. Although there was statistical significance, the clinical significance may not be significant. In clinical work, professional clinicians are required to make judgments based on the actual situation of the patient. Finally, information of quantitative alcohol consumption was lacking of in this study, this may affect the evaluation of the impact alcohol intaking on cognitive. The further quantitative analysis was needed.
Conclusion
Among a low-income population over 60 years old in northern China, the prevalence of cognitive impairment in hypertensive patients is significantly higher, especially in those with grade 3 hypertension. In addition, in this study, hypertension mainly affects the abilities of orientation, language, and attention and calculation; this may provide some theoretical basis for the prevention of dementia in low- and middle-income countries.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee at Tianjin Medical University General Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
XN, YS, and JLi were involved in conception and design, data interpretation for this article, and involved critical review in for this article. JB, JLiu, ZL, ZZ, XS, JS, and JT were involved in data collection, case diagnosis, and confirmation for this article. JB, JLiu, and ZL were involved in manuscript drafting. JW was involved in data analysis for this article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank all participants of the Tianjin Brain Study, and local medical care professionals for their valuable contributions.
References
1. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. (2016) 134:441–50. doi: 10.1161/CIRCULATIONAHA.115.018912
2. Walker KA, Power MC, Gottesman RF. Defining the relationship between hypertension, cognitive decline, and dementia: a review. Curr Hypertens Rep. (2017) 19:24. doi: 10.1007/s11906-017-0724-3
3. Rajan KB, Weuve J, Barnes LL, Wilson RS, Evans DA. Prevalence and incidence of clinically diagnosed Alzheimer's disease dementia from 1994 to 2012 in a population study. Alzheimers Dement. (2019) 15:1–7. doi: 10.1016/j.jalz.2018.07.216
4. Pearce LA, McClure LA, Anderson DC, Jacova C, Sharma M, Hart RG, et al. Effects of long-term blood pressure lowering and dual antiplatelet treatment on cognitive function in patients with recent lacunar stroke: a secondary analysis from the SPS3 randomised trial. Lancet Neurol. (2014) 13:1177–85. doi: 10.1016/S1474-4422(14)70224-8
5. Novak V, Hajjar I. The relationship between blood pressure and cognitive function. Nat Rev Cardiol. (2010) 7:686–98. doi: 10.1038/nrcardio.2010.161
6. Razay G, Williams J, King E, Smith AD, Wilcock G. Blood pressure, dementia and Alzheimer's disease: the OPTIMA longitudinal study. Dement GeriatrCognDisord. (2009) 28:70–4. doi: 10.1159/000230877
7. Shang X, Hill E, Zhu Z, Liu J, Ge BZ, Wang W, et al. The association of age at diagnosis of hypertension with brain structure and incident dementia in the UK biobank. Hypertension. (2021) 78:1463–74. doi: 10.1161/HYPERTENSIONAHA.121.17608
8. Noriega de la Colina A, Badji A, Robitaille-Grou MC, Gagnon C, Boshkovski T, Lamarre-Cliche M, et al. Associations between relative morning blood pressure, cerebral blood flow, and memory in older adults treated and controlled for hypertension. Hypertension. (2021) 77:1703–13. doi: 10.1161/HYPERTENSIONAHA.120.16124
9. Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet. (2020) 396:413–46. doi: 10.1016/S0140-6736(20)30367-6
10. Lane CA, Barnes J, Nicholas JM, Sudre CH, Cash DM, Parker TD, et al. Associations between blood pressure across adulthood and late-life brain structure and pathology in the neuroscience substudy of the 1946 British birth cohort (Insight 46): an epidemiological study. Lancet Neurol. (2019) 18:942–52. doi: 10.1016/S1474-4422(19)30228-5
11. Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. (2011) 378:1231–43. doi: 10.1016/S0140-6736(11)61215-4
12. Avezum A, Oliveira G, Lanas F, Lopez-Jaramillo P, Diaz R, Miranda JJ, et al. Secondary CV prevention in South America in a community setting: the PURE study. Glob Heart. (2017) 12:305–13. doi: 10.1016/j.gheart.2016.06.001
13. Liu J, Lin Q, Guo D, Yang Y, Zhang X, Tu J, et al. Association between pulse pressure and carotid intima-media thickness among low-income adults aged 45 years and older: a population-based cross-sectional study in rural China. Front Cardiovasc Med. (2020) 7:547365. doi: 10.3389/fcvm.2020.547365
14. Zhan C, Wang Q, Liu J, Wang L, Chen Z, Pang H, et al. Relationship between metabolic syndrome and cognitive function: a population-based study of middle-aged and elderly adults in rural China. Diabetes Metab Syndr Obes. (2021) 14:1927–35. doi: 10.2147/DMSO.S308250
15. Administration NHS,. Statistical Bulletin on Healthcare Security. (2014). Available online at: http://www.nhsa.gov.cn/art/2019/
16. Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. The task force for the management of arterial hypertension of the European society of cardiology (ESC) and the European society of hypertension (ESH). G Ital Cardiol. (2018) 19:3S–73. doi: 10.1097/HJH.0000000000001940
17. Joint Committee for Guideline Revision. Chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of Chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. (2019) 16:182–241. doi: 10.11909/j.issn.1671-5411.2019.03.014
18. Pottie K, Rahal R, Jaramillo A, Birtwhistle R, Thombs BD, Singh H, et al. Recommendations on screening for cognitive impairment in older adults. CMAJ. (2016) 188:37–46. doi: 10.1503/cmaj.141165
19. Ren L, Bai L, Wu Y, Ni J, Shi M, Lu H, et al. Prevalence of and risk factors for cognitive impairment among elderly without cardio- and cerebrovascular diseases: a population-based study in rural China. Front Aging Neurosci. (2018) 10:62. doi: 10.3389/fnagi.2018.00062
20. Kety SS, Hafkenschiel JH, Jeffers WA, Leopold IH, Shenkin HA. The blood flow, vascular resistance, and oxygen consumption of the brain in essential hypertension J Clin Invest. (1948) 27:511–4. doi: 10.1172/JCI101998
21. Wilkie F, Eisdorfer C. Intelligence and blood pressure in the aged. Science. (1971) 172:959–62. doi: 10.1126/science.172.3986.959
22. Debette S, Seshadri S, Beiser A, Au R, Himali JJ, Palumbo C, et al. Midlife vascular risk factor exposure accelerates structural brain aging and cognitive decline. Neurology. (2011) 77:461–8. doi: 10.1212/WNL.0b013e318227b227
23. Knopman DS, Gottesman RF, Sharrett AR, Tapia AL, DavisThomas S, Windham BG, et al. Midlife vascular risk factors and midlife cognitive status in relation to prevalence of mild cognitive impairment and dementia in later life: the atherosclerosis risk in communities study. Alzheimers Dement. (2018) 14:1406–15. doi: 10.1016/j.jalz.2018.03.011
24. Scheltens P, De Strooper B, Kivipelto M, Holstege H, Chételat G, Teunissen CE, et al. Alzheimer's disease. Lancet. (2021) 397:1577–90. doi: 10.1016/S0140-6736(20)32205-4
25. Gottesman RF, Schneider AL, Albert M, Alonso A, Bandeen-Roche K, Coker L, et al. Midlife hypertension and 20-year cognitive change: the atherosclerosis risk in communities neurocognitive study. JAMA Neurol. (2014) 71:1218–27. doi: 10.1001/jamaneurol.2014.1646
26. Li C, Ma Y, Hua R, Yang Z, Zhong B, Wang H, et al. Dose-response relationship between long-term blood pressure variability and cognitive decline. Stroke. (2021) 52:3249–57. doi: 10.1161/STROKEAHA.120.033697
27. SPRINT MIND Investigators for the SPRINT Research Group Williamson JD Pajewski NM Auchus AP Bryan RN Chelune G . Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA. (2019) 321:553–61. doi: 10.1001/jama.2018.21442
28. Kurella Tamura M, Gaussoin SA, Pajewski NM, Chelune GJ, Freedman BI, Gure TR, et al. Kidney disease, intensive hypertension treatment, and risk for dementia and mild cognitive impairment: the systolic blood pressure intervention trial. J Am Soc Nephrol. (2020) 31:2122–32. doi: 10.1681/ASN.2020010038
29. Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. (2008) 358:1887–98. doi: 10.1056/NEJMoa0801369
30. Kilbourne S, Krupnick AS. How low can you go. J Thorac Cardiovasc Surg. (2018) 156:892–3. doi: 10.1016/j.jtcvs.2018.04.023
31. Waldstein SR, Manuck SB, Ryan CM, Muldoon MF. Neuropsychological correlates of hypertension: review and methodologic considerations. Psychol Bull. (1991) 110:451–68. doi: 10.1037/0033-2909.110.3.451
32. Lyall DM, Celis-Morales CA, Anderson J, Gill JM, Mackay DF, McIntosh AM, et al. Associations between single and multiple cardiometabolic diseases and cognitive abilities in 474 129 UK biobank participants. Eur Heart J. (2017) 38:577–83. doi: 10.1093/eurheartj/ehw528
33. Veldsman M, Tai XY, Nichols T, Smith S, Peixoto J, Manohar S, et al. Cerebrovascular risk factors impact frontoparietal network integrity and executive function in healthy ageing. Nat Commun. (2020) 11:4340. doi: 10.1038/s41467-020-18201-5
34. Raz N, Yang YQ, Rodrigue KM, Kennedy KM, Lindenberger U, Ghisletta P. White matter deterioration in 15 months: latent growth curve models in healthy adults. Neurobiol Aging. (2012) 33:429. doi: 10.1016/j.neurobiolaging.2010.11.018
35. Kuller LH, Margolis KL, Gaussoin SA, Bryan NR, Kerwin D, Limacher M, et al. Relationship of hypertension, blood pressure, and blood pressure control with white matter abnormalities in the women's health initiative memory study (WHIMS)-MRI trial. J Clin Hypertens. (2010) 12:203–12. doi: 10.1111/j.1751-7176.2009.00234.x
36. Triantafyllou A, Ferreira JP, Kobayashi M, Micard E, Xie Y, Kearney-Schwartz A, et al. Longer duration of hypertension and mri microvascular brain alterations are associated with lower hippocampal volumes in older individuals with hypertension. J Alzheimers Dis. (2020) 74:227–35. doi: 10.3233/JAD-190842
37. Rundek T, Tolea M, Ariko T, Fagerli EA, Camargo CJ. Vascular cognitive impairment (VCI). Neurotherapeutics. (2021). doi: 10.1007/s13311-021-01170-y
38. Emdin CA, Rothwell PM, Salimi-Khorshidi G, Kiran A, Conrad N, Callender T, et al. Blood pressure and risk of vascular dementia: evidence from a primary care registry and a cohort study of transient ischemic attack and stroke. Stroke. (2016) 47:1429–35. doi: 10.1161/STROKEAHA.116.012658
39. Girouard H, Iadecola C. Neurovascular coupling in the normal brain and in hypertension, stroke, and Alzheimer disease. J Appl Physiol (1985). (2006) 100:328–35. doi: 10.1152/japplphysiol.00966.2005
40. Qiu C, Winblad B, Fratiglioni L. The age-dependent relation of blood pressure to cognitive function and dementia. Lancet Neurol. (2005) 4:487–99. doi: 10.1016/S1474-4422(05)70141-1
41. Wang J, Ning X, Yang L, Lu H, Tu J, Jin W, et al. Trends of hypertension prevalence, awareness, treatment and control in rural areas of northern China during 1991-2011. J Hum Hypertens. (2014) 28:25–31. doi: 10.1038/jhh.2013.44
42. Pendlebury ST, Mariz J, Bull L, Mehta Z, Rothwell PM. MoCA, ACE-R, and MMSE versus the national institute of neurological disorders and stroke-Canadian stroke network vascular cognitive impairment harmonization standards neuropsychological Battery after TIA and stroke. Stroke. (2012) 43:464–9. doi: 10.1161/STROKEAHA.111.633586
Keywords: hypertension and cognitive function in elderly population hypertension, cognitive function, elderly, epidemiology, risk factors
Citation: Bao J, Liu J, Li Z, Zhang Z, Su X, Sun J, Tu J, Wang J, Li J, Song Y and Ning X (2022) Relationship Between Hypertension and Cognitive Function in an Elderly Population: A Population-Based Study in Rural Northern China. Front. Neurol. 13:885598. doi: 10.3389/fneur.2022.885598
Received: 28 February 2022; Accepted: 21 April 2022;
Published: 16 May 2022.
Edited by:
Elizabeta Blagoja Mukaetova-Ladinska, University of Leicester, United KingdomReviewed by:
Lucy Beishon, University of Leicester, United KingdomLi-Nien Chien, Taipei Medical University, Taiwan
Xian-Le Bu, Third Military Medical University, China
Copyright © 2022 Bao, Liu, Li, Zhang, Su, Sun, Tu, Wang, Li, Song and Ning. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xianjia Ning, eG5pbmdAdG11LmVkdS5jbg==; Yijun Song, c29uZ3lqQHRtdS5lZHUuY24=; Jidong Li, amRfbGlfZG9jdG9yQDE2My5jb20=
†These authors have contributed equally to this work
 Jie Bao1†
Jie Bao1† Jie Liu
Jie Liu Zhiying Li
Zhiying Li Jinghua Wang
Jinghua Wang Yijun Song
Yijun Song Xianjia Ning
Xianjia Ning