
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 29 July 2022
Sec. Neurological Biomarkers
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.877143
Introduction/Objectives: In addition to cognitive decline, one of the most important problems for caregivers of patients with Alzheimer's is neuropsychiatric symptoms (NPS). This study aimed to evaluate the NPS in patients with Alzheimer's disease (AD) and investigate its relationship with caregiver burden (CB).
Methods: In a cross-sectional study of 85 patients with AD referred to Shafa Hospital in Rasht and their caregivers in 2020, information was collected using a demographic questionnaire, Neuropsychiatric Inventory Questionnaire (NPI-Q), and the Caregiver Burden Inventory (CBI). Data were analyzed by Spearman correlation, t-test, and linear regression, with SPSS version 22.
Results: The mean age of the patients and their caregivers were 74.95 ± 8.87 years and 43.98 ± 11.38 years, respectively. The mean total score of NPS in patients with AD was 44.25 (0–144) and the mean CB score was 36.27 (0–96), which was a moderate level. According to the results, 91% of patients had apathy, while happiness/euphoria was reported as the most uncommon symptom. In addition, there was a significant relationship between the score of NPS and CB (r = 0.542, P < 0.0001), as well as all its sub-components, time-dependence burden with more correlation (r = 0.509, P < 0.0001), and social burden with less correlation (r = 0.352, P < 0.001). NPS, hallucination, aberrant motor behavior (AMB), delusion, and depression were most correlated with CB. Also, the mean score of CB was significantly higher in women than in men (P = 0.045). Living in a rural area had a significant relationship with NPS score (P = 0.026). Also, linear regression showed that with increasing 1 year of patients' age, the mean score of patient's NPS decreased by 0.374 (P = 0.048).
Conclusion: Neuropsychiatric symptoms, especially hallucination, aberrant motor behavior (AMB), delusion, and depression were associated with caregiver burden. Apathy was the most common symptom in patients with AD.
Increasing the number of older people is one of the important issues in the twenty-first century (1). An increase in the rate of aging is inevitable, and of course, Alzheimer's disease (AD) is the most common cause of dementia in older adults (2). Around the world, over 50 million people are currently living with AD-related dementia, and this number could also rise to 152 million by 2050 (World Alzheimer's Report 2019) (3). AD is a progressive and irreversible brain disorder (4) that affects ~300–450 thousand Iranians (5). In a recent study in 2019, the prevalence of AD in Iran was estimated at 2.3% (6). Iran is one of the leading and increasing aging populations in the world. As a global health problem, concerns raises about the pace of future economic growth, performance and financial integrity of health care systems, and pensions and the health and wellbeing of the elderly (7).
In the vast majority (>80%) of the patient with AD, in addition to cognitive decline, the onset of functional and behavioral deficits, which are known as neuropsychiatric symptoms (NPS) (8), can increase the caregiver burden (CB) (9). The coincidence of NPS and mild cognitive impairment (MCI) are associated with an increased risk of dementia (10). As a result, subtle NPS is one of the first preclinical signs of AD (8, 11, 12). So, detection and treatment of NPS, especially apathy, in early dementia can delay the progression of the disease (13).
NPS is often overlooked, especially when the patient has a cognitive impairment in dementia (14, 15), and is the major contributor to CB (16). They exacerbate functional deficits and disabilities in social skills, accelerate cognitive decline in patients (12), increase CB, distress, and adverse outcomes, such as depression and reduced quality of life. Also, they can cause further neuropathological symptoms (17, 18).
The study by Mavounza et al. (19) found that the frequency/severity of NPS in patients and the emotional distress of caregivers had a positive association. In a review study about CB and NPS presence in patients, results showed that caregivers of patients with AD experience more stress than caregivers of older adults in lack NPS. Moreover, the presence of NPS in patients was related to more CB (16). Yu et al. (20) found that more severe AD and more caregiving time were associated with more CB.
In a study in Iran, the level of CB in most caregivers was moderate to severe. The high level of CB was significantly associated with gender, patient education, and patient's level of dependence on daily activities (21). In another study in 2010, the level of general mental health problems was moderate to severe in about 75% of female caregivers of patients with AD (22).
Inadequate knowledge about Alzheimer's disease and poor premorbid relationships with patients can predict CB (16). These characteristics are the only face of the Rubik's Cube. Many others that can be predictors or protective factors of this burden should be evaluated to solve this puzzle.
Patients' characteristics, such as AD's severity, MCI, the decline in or loss of functional activities of daily living, and demographic features (23, 24) and caregivers' characteristics (25) have been investigated as a predictor of NPS in many studies.
Caring for a person with Alzheimer's is more stressful than other chronic disorders (26). Sleep in Alzheimer's caregivers has always been of low quality and quantity. Caregivers are often woken up overnight by their patients, and as a result, they find that they will have a better sleep when they rest from caring for a person with Alzheimer's (27). Most caregivers are family, friends, or neighbors. This means that caregivers may be older than patients and not physically and mentally healthy. Although young caregivers especially children of patients have many responsibilities in middle age and in addition to their relationship with the patients, they lose their free time and have problems in their jobs, and experience anxiety and depression. Therefore, dealing with AD, in general, can harm the physical, psychological, emotional health, and social and economic life of caregivers (28), young and old alike.
Due to the high prevalence of Alzheimer's disease as the most common cause of dementia in the world and the large number of people involved in the care of these people and limited studies in this field in our country, this study aimed to evaluate neuropsychiatric symptoms in patients with AD and its relationship with CB.
In this cross-sectional study, patients with AD who had been referred to Shafa Hospital of Rasht in 2020 and their caregivers were included in the study after obtaining informed consent and ensuring that the inclusion criteria were met.
Inclusion criteria for patients were confirming the AD diagnosis by one of the hospital psychiatrists. Caregivers should not have a history of cognitive impairment, traumatic brain injury, or neurological disorders and take care of patients for at least 1 night a week for 1 month.
To reduce the coronavirus disease 2019 (COVID-19) spread, the sample information was collected through their files in the hospital. Most of the questionnaires were filled out via telephone or email. Some of them were done in a private area at the center with full compliance with the health protocols. The questionnaires were given to 89 caregivers (58 people virtually and 21 physically). Four out of all participants were excluded from the study due to incomplete questionnaires, so 85 individuals were included.
Demographic questionnaire, Neuropsychiatric Inventory (NPI) (29), and Caregiver Burden Inventory (CBI) (30) were used for the measure of the study.
This scale is a caregiver-based questionnaire, in which the carer indicates the presence or absence of neuropsychiatric symptoms in the patient during the last few weeks, including 12 neuropsychiatric symptoms: delusions, hallucinations, agitation/aggression, dysphoria/depression, anxiety, euphoria/elation, apathy/indifference, disinhibition, irritability/lability, aberrant motor behaviors (AMB), night-time behavioral disturbances, and appetite/eating disturbances. After answering the screening question by the caregivers, they answer the sub-questions related to each behavior, and then, indicate the frequency (1 rarely, less than once per week to 4 very often, once, or more per day) and severity (1 mild to 3 severe) of it. To assess the caregiver's distress score, after determining the severity and frequency of the symptom, we ask the caregiver: “How much do these symptoms cause you discomfort?” Caregiver stress is scored between 0 (no distress) and 5 (extreme distress). For each symptom, the total score is calculated by the equation frequency × severity. The total NPI scores are within 0–144. The original instrument had good validity and reliability (29). The internal consistency by Cronbach's α was 0.9 and concurrent validity was obtained between 0.3 and 0.9 (P < 0.05) in the Persian version of this scale (31).
This scale consists of 24 open-ended and fixed choice questions. The instrument assesses the CB (4 nearly always to 0 never), with each of the following 5 dimensions of CB: time-dependence, developmental, physical, social, and emotional dimensions. Total scores can range from 0 to 96, and higher scores indicate greater CB. The total CBI score between 0–15 is considered to be mild, 16–47 moderate, and 48–96 severe. Cronbach's alpha for the scale was 0.9, and the test and retest scores were 0.8 (32).
Interviewees also answered a series of demographic questions. The interview took approximately 1 h.
No animals were used in this study. This study was conducted based on the ethical principles for medical research involving human subjects by the World Medical Association Declaration of Helsinki. It was approved by the Ethical Committee of Guilan University of Medical Sciences (IR.GUMS.REC.1399.177).
The demographic feature, prevalence, and incidence of NPI and CBI scores were assessed in patients and caregivers using t-test, analysis of variance (ANOVA) test, and correlation test (Bivariate analysis with SPSS version 22). Multiple regression analysis and simple correlation analyses were used to demonstrate the factors affecting the CB, according to the presumptions of parametric tests in the present study. To investigate the relationship between two continuous variables, the score of NPS and CB, due to the lack their normality, they were measured by Shapiro-Wilkes's test (P < 0.0001). The Spearman correlation coefficient has been used to determine the relationship between the score of NPS and CB.
A total of 85 patients with AD and their caregivers participated in the study. The mean age of patients and caregivers was 74.95 ± 8.87 and 43.98 ± 11.38 years, respectively, and the mean time of AD in patients participating in this study was 5.09 ± 3.26 years. The median number of caregivers was 3 (2–4), and the mean duration of caring by caregivers was 40.26 ± 34.22 months. Among the drugs used by the patients, most of them were acetylcholinesterase inhibitors (AchEs) (82.4%), Benzodiazepines (72.9%), and selective serotonin reuptake inhibitors (SSRIs) (49.4%) respectively. Demographic and clinical characteristics of patients and caregivers are displayed in Table 1.
The mean total score of NPS in patients with AD participating in this study was 44.25 based on 12 symptoms.
Table 2 shows the prevalence, frequency, and severity of NPS in the total sample. Almost all patients in this study had apathy. Symptoms of depression, anxiety, change in appetite, and irritation/aggression have been observed to be high. The sign of happiness/euphoria has been observed with the lowest frequency.
According to the results, there was a statistically significant relationship between the score of NPS and CB as well as all its sub-components, by the Spearman correlation coefficient (Table 3).
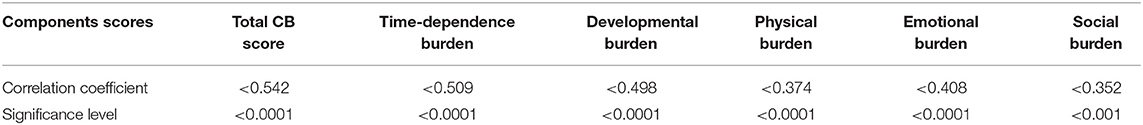
Table 3. The relationship between the mean score of neuropsychoatric symptoms (NPS), total caregiver burden (CB) score, and sub-components of CB.
The relationships between each NPS with CB are presented in Table 4. According to the findings, hallucinations, AMB, delusion, and depression had the most correlation with CB, respectively. The least correlation belonged to apathy.
The mean CB score in caregivers was 36.27 ± 18.21, which was the moderate level. Of the five dimensions of CB, only the time-dependence burden with a mean of 11.93 ± 5.78 was higher than the mean score (scoring between 0 and 20).
In addition, among the demographic variables, the place of residence had a statistically significant relationship with the score of NPS (P = 0.026). The score of NPS in patients living in rural areas with a mean ± standard deviation (SD) of 42.48 ± 18.36 was significantly higher than the score of these symptoms in urban residents with an average of 33.03 ± 16.51.
Table 5 shows that apart from the caregiver age, other demographic variables of caregivers have a significant effect on CB.
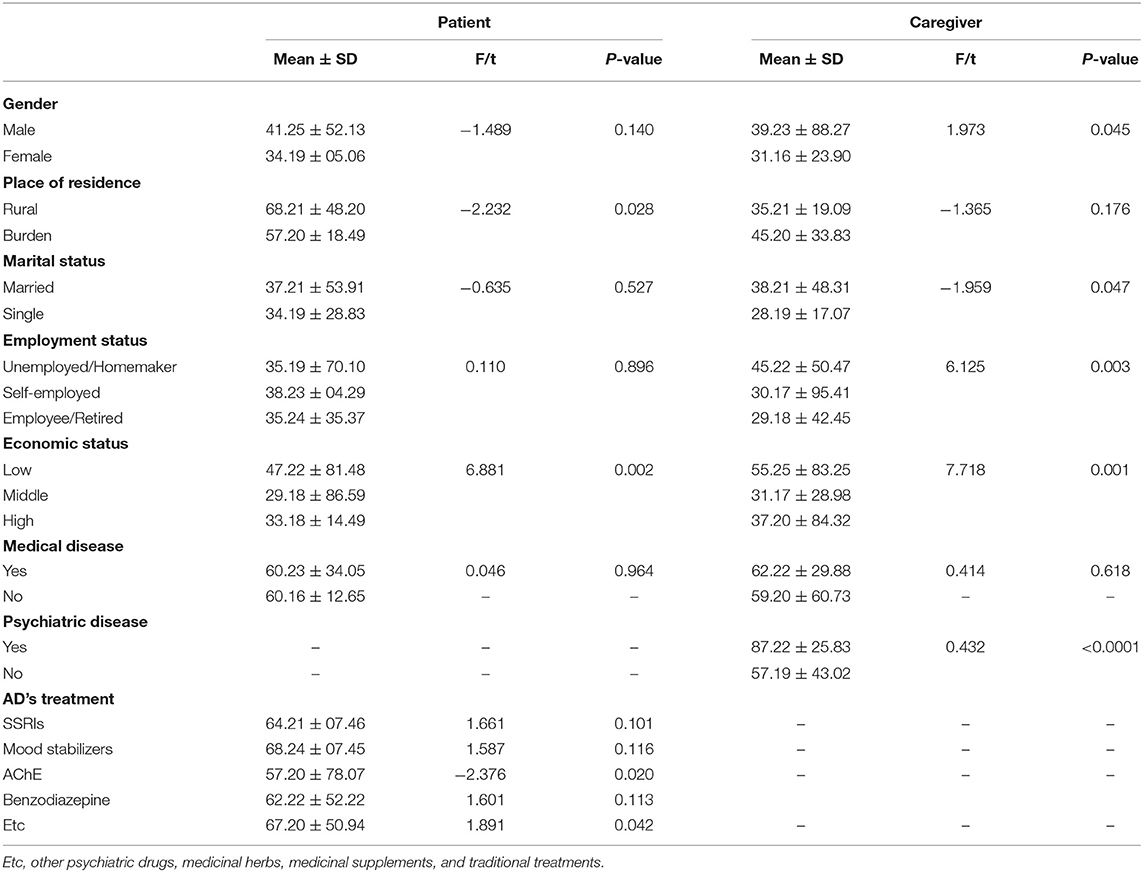
Table 5. Descriptive and inferential results of the relationship between demographic variables and CB of caregivers of patients with Alzheimer's disease (AD).
A linear regression model was used to investigate the relationship between the continuous variables of age, education, and duration of disease with the score of neuropsychiatric symptoms. A significance level of age variable with the value of 0.048 showed that with increasing 1 year of patients' age, the average score of the patient's neuropsychiatric symptoms has decreased by 0.374 units. A significance level of the fitted regression model for the education variable (P = 0.639) and duration of illness (P = 0.380) indicated that there is no significant relationship between these two factors and the score of neuropsychiatric symptoms. The distribution diagram and the fitted regression line are shown in Figure 1.
This study aimed to measure the NPS, as a core feature of AD and assess the CB in the caregivers. This study showed that apathy, depression, aggression, and anxiety are the most common NPSs in patients with AD. According to a systematic review and meta-analysis of the 48 original types of research in America, Europe, and Asia, the most frequent NPS was apathy and similar to our study the least common was euphoria (33). Also, in the study by Lanctôt et al. (34), Delfino et al. (35), and Chen et al. (36), apathy was increasingly recognized as an important NPS in AD.
We found that NPS was associated with CB and there was a statistically significant relationship between all sub-components of CB and NPS. The results of this study are in line with previous findings showing that the presence of NPS in people with AD is associated with both increased burden and lower quality of life in caregivers (37). Also, in the study by Chen et al., the results showed that NPI score was independently associated with mean NPI-burden score (38). Pinyopornpanish et al. (39) study in 2021 also showed that the higher the NPS score, the higher the care pressure. In addition, among neuropsychiatric symptoms, hallucination (P = 0.010), AMD (P = 0.011), delusion (P = 0.003), depression (P = 0.001), and changes in appetite/eating (P = 0.013) had significant association with CB. Previous studies showed different findings. In a recent study on female patients with AD, specific NPS including crying spells, anger, and aggression were associated with higher level of CB (40). In another study by Chen et al. among NPS, apathy, irritability, sleep disturbance, anxiety, and delusions were related with caregiver burden (36). According to a systematic review in 2012, it was reported that CB was negatively associated with depression, aggression, and sleep disturbances (41). In another systematic review study in 2017, irritability, agitation, sleep disturbances, anxiety, apathy, and delusion had the most relationship with CB (42). In our study apathy had the least correlation with CB. It seems that apathy with lack of motivation, emotion and poor physical activity is less annoying for caregivers than other symptoms.
Our study showed that with increasing one year of patients' age, the mean score of the NPS decreased by 0.374 score, but in the study by Okura et al. (43), the older the patient, who had more severe cognitive impairment, the greater the NPS.
We found that patients living in rural areas had higher NPS. It seems that low level of education and awareness in rural patients and caregivers might affect dealing with the disease. On the other hand, treatment may be delayed or interrupted due to difficult access to the therapist or financial problems. So, it might lead to higher NPS and CB.
The results of our study showed no significant correlation between caregiver age and CB. Some studies reported that younger caregivers had greater burden (44, 45). On the contrary, Tsai et al. (46) reported that older caregivers have much more CB; while in Pattanayak study, older caregivers perceived more spouse related burden (47). Given these contradictory results, it is not possible to make a definitive statement about the relationship between the age of the caregiver and the CB, and it seems that several other factors also play a role in this issue.
In our study, it was demonstrated that CB in females is significantly higher, especially in housewife ones. This result was in agreement with the findings of many other studies (9, 48–50). The majority of the caregivers in our sample were the children of the patients and most of them were housewives. Females have multiple roles and responsibilities in a traditionally oriented household. In addition to playing the role of mother to their children, they must take care of their older generation and live with their spouse. This condition requires a flexible personality and is normally stressful and may lead to anxiety and depression. So, female caregivers face the risk to perceive an especially higher burden. Contrary to our results, the Pinyopornpanish et al. (39) study showed that no sociodemographic variables were significantly related to CB and NPI.
The results of this study, like the study by García-Alberca (9), have shown that the duration of caregiving has a positive association with level of CB. Also, we found that by increasing caregiver education, the level of CB decreased. This result is in line with more previous studies (9, 38, 51). It seems that people with higher education have more knowledge and awareness, which can help them adapt to difficult situations.
About 9.4% of caregivers had psychiatric illness and as expected, CB was significantly higher in them. In the study by Hosseiny et al. (52), caregivers believed that caring for the elderly reduced their health and led to mental fatigue, burden of care, mental disorders, and so on. They considered caring for the elderly as a stressful experience and often found themselves unsuccessful in dealing with stress. In contrast, in a study in Spain, the majority of caregivers, who lived with the patient, had excellent mental and physical health (9). In many developed countries, there is a wide range of social support for patients with AD and their caregivers, and support groups provide a wide range of services to these individuals, thus, reducing their caregiver burden.
Our sampling was done from a hospital treatment center. Therefore, it is likely that our patients have more severe symptoms and more cognitive decline than patients in the community.
Neuropsychiatric symptoms were associated with caregiver burden. Apathy was the most and happiness/euphoria was the least symptoms in patients with AD. The symptoms of hallucination, aberrant motor behavior (AMB), delusion, and depression had the most correlation with CB, respectively. People in rural areas had more NPS and NPS decreased with increasing the age of patients. CB in female, married, unemployed/ homemaker, and low economic status caregivers was significantly higher. The level of CB decreased with increasing level of education, the number of caregivers, and declining duration of care.
It is recommended that future studies investigate the role of supportive and psychosocial interventions on CB and patients' NPS. Also, more extensive studies on patients with mild symptoms in the community are recommended.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
This study was approved by Ethical Committee of Guilan University of Medical Sciences. The patients/participants provided their written informed consent to participate in this study.
Study design and drafting manuscript: BI, EA, FE-S, and RS. Gathering data: EA. Data analysis: BI and EA. All authors contributed to the article and approved the submitted version.
This study was the result of a MD (medical doctor) thesis approved by Guilan University of Medical Sciences.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
NPS, Neuropsychiatric symptoms; CB, Caregiver burden; AD, Alzheimer's disease; NPI-Q, Neuropsychiatric Inventory Questionnaire; CBI, Caregiver Burden Inventory; AMB, Aberrant motor behavior; MCI, Mild cognitive impairment; ANOVA, Analysis of variance; AchEs, Acetylcholinesterase inhibitors; SSRIs, Selective serotonin reuptake inhibitors.
1. Stucki G, Bickenbach J, Gutenbrunner C, Melvin J. Rehabilitation: the health strategy of the 21st century. J Rehabil Med. (2018) 50:309–16. doi: 10.2340/16501977-2200
2. Weller J, Budson A. Current understanding of Alzheimer's disease diagnosis and treatment. F1000Res. (2018) 7:F1000. doi: 10.12688/f1000research.14506.1
3. Kumar S, Reddy PH. Elevated levels of MicroRNA-455-3p in the cerebrospinal fluid of Alzheimer's patients: a potential biomarker for Alzheimer's disease. Biochim Biophys Acta Mol Basis Dis. (2021) 1867:166052. doi: 10.1016/j.bbadis.2020.166052
4. James TA, James D, Larkey LK. Heart-focused breathing and perceptions of burden in Alzheimer's caregivers: an online randomized controlled pilot study. Geriatr Nurs. (2021) 42:397–404. doi: 10.1016/j.gerinurse.2021.02.006
5. Pourmollamirza A, Sharifi F, Etesam F, Navab E. Abuse of people with Alzheimer's disease by family caregivers: a review. Iran J Nurs Res. (2020) 15:96–108. Available online at: http://ijnr.ir/article-1-2335-en.html
6. Navipour E, Neamatshahi M, Barabadi Z, Neamatshahi M, Keykhosravi A. Epidemiology and risk factors of Alzheimer's Disease in Iran: a systematic review. Iran J Public Health. (2019) 48:2133–9. doi: 10.18502/ijph.v48i12.3544
7. Noroozian M. The elderly population in iran: an ever growing concern in the health system. Iran J Psychiatry Behav Sci. (2012) 6:1–6.
8. Papma JM, Franzen S, van Swieten JC, Ossenkoppele R, Coesmans M, van den Berg E. [P1–311]: the role of neuropsychiatric symptoms in ad differential diagnosis. AD. (2017) 13:P372–3. doi: 10.1016/j.jalz.2017.06.327
9. García-Alberca JM, Lara JP, Garrido V, Gris E, González-Herero V, Lara A. Neuropsychiatric symptoms in patients with Alzheimer's disease: the role of caregiver burden and coping strategies. Am J Alzheimers Dis Other Demen. (2014) 29:354–61. doi: 10.1177/1533317513518649
10. Rosenberg PB, Mielke MM, Appleby BS, Oh ES, Geda YE, Lyketsos CG. The association of neuropsychiatric symptoms in MCI with incident dementia and Alzheimer disease. Am J Geriatr Psychiatry. (2013) 21:685–95. doi: 10.1016/j.jagp.2013.01.006
11. Eikelboom WS, van den Berg E, Coesmans M, Singleton EH, van Swieten JC, Pijnenburg YA, et al. O2-11-02: neuropsychiatric and cognitive symptoms in Alzheimer's Disease: a study in AD biomarker confirmed patients across the clinical spectrum. AD. (2019) 15:P567–8. doi: 10.1016/j.jalz.2019.06.4512
12. Sannemann L, Schild AK, Altenstein S, Bartels C, Brosseron F, Buerger K, et al. Neuropsychiatric symptoms in at-risk groups for AD dementia and their association with worry and AD biomarkers-results from the DELCODE study. Alzheimers Res Ther. (2020) 12:131. doi: 10.1186/s13195-020-00701-7
13. Low K, Ali N, Chan M, Tay L, Lim WS, Chew J. P3-307: Neuropsychiatric symptoms as predictors of progression in mild cognitive impairment (MCI) and mild Alzheimer's disease (AD): the role of apathy. AD. (2019) 15:P1055–P. doi: 10.1016/j.jalz.2019.06.3339
14. Woolley JD, Khan BK, Murthy NK, Miller BL, Rankin KP. The diagnostic challenge of psychiatric symptoms in neurodegenerative disease: rates of and risk factors for prior psychiatric diagnosis in patients with early neurodegenerative disease. J Clin Psychiatry. (2011) 72:126–33. doi: 10.4088/JCP.10m06382oli
15. Cieslak A, Smith EE, Lysack J, Ismail Z. Case series of mild behavioral impairment: toward an understanding of the early stages of neurodegenerative diseases affecting behavior and cognition. Int Psychogeriatr. (2018) 30:273–80. doi: 10.1017/S1041610217001855
16. Isik AT, Soysal P, Solmi M, Veronese N. Bidirectional relationship between caregiver burden and neuropsychiatric symptoms in patients with Alzheimer's disease: a narrative review. Int J Geriatr Psychiatry. (2019) 34:1326–34. doi: 10.1002/gps.4965
17. Parrotta I, De Mauleon A, Abdeljalil AB, De Souto Barreto P, Lethin C, Veerbek H, et al. Depression in people with Dementia and Caregiver outcomes: results from the European right time place care study. J Am Med Dir Assoc. (2020) 21:872–8.e1. doi: 10.1016/j.jamda.2020.02.023
18. Ismail Z, Goodarzi Z. Neuropsychiatric aspects of Alzheimer's disease. Pract Neurol. (2019) 78–83. Available online at: https://practicalneurology.com/articles/2019-june/neuropsychiatric-aspects-of-alzheimers-disease
19. Mavounza C, Ouellet MC, Hudon C. Caregivers' emotional distress due to neuropsychiatric symptoms of persons with amnestic mild cognitive impairment or Alzheimer's disease. Aging Ment Health. (2020) 24:423–30. doi: 10.1080/13607863.2018.1544208
20. Yu H, Wang X, He R, Liang R, Zhou L. Measuring the caregiver burden of caring for community-residing people with Alzheimer's disease. PLoS ONE. (2015) 10:e0132168. doi: 10.1371/journal.pone.0132168
21. Abdollahpour I, Noroozian M, Nedjat S, Majdzadeh R. Caregiver burden and its determinants among the family members of patients with dementia in Iran. Int J Prev Med. (2012) 3:544–51.
22. Bastani F, Hosseiny RS, Baniasad M, Haghni H. Investigation of general health in female care givers of elderly people with Alzheimer. Iran J Ageing. (2010) 5:43–51. Available online at: https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=275232
23. García-Alberca JM, Lara JP, Berthier ML, Cruz B, Barbancho M, Green C, et al. Can impairment in memory, language and executive functions predict neuropsychiatric symptoms in Alzheimer's disease (AD)? Findings from a cross-sectional study. Arch Gerontol Geriatr. (2011) 52:264–9. doi: 10.1016/j.archger.2010.05.004
24. Karttunen K, Karppi P, Hiltunen A, Vanhanen M, Välimäki T, Martikainen J, et al. Neuropsychiatric symptoms and quality of life in patients with very mild and mild Alzheimer's disease. Int J Geriatr Psychiatry. (2011) 26:473–82. doi: 10.1002/gps.2550
25. Lin PC, Lin HT, Yang YH, Yang YH. The effects of caregiver characteristics on behavioral and psychological symptoms of dementia of patients with dementia. Aging Ment Health. (2022) 26:263–9. doi: 10.1080/13607863.2020.1857693
26. Anand KS, Dhikav V, Sachdeva A, Mishra P. Perceived caregiver stress in Alzheimer's disease and mild cognitive impairment: a case control study. Ann Indian Acad Neurol. (2016) 19:58–62. doi: 10.4103/0972-2327.167695
27. Varela G, Varona L, Anderson K, Sansoni J. Alzheimer's care at home: a focus on caregivers strain. Prof Inferm. (2011) 64:113–7.
28. Sansoni J, Anderson KH, Varona LM, Varela G. Caregivers of Alzheimer's patients and factors influencing institutionalization of loved ones: some considerations on existing literature. Ann Ig. (2013) 25:235–46. doi: 10.7416/ai.2013.1926
29. Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. (1994) 44:2308–14. doi: 10.1212/WNL.44.12.2308
30. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. (1980) 20:649–55. doi: 10.1093/geront/20.6.649
31. Malakouti SK, Panaghi L, Foroughan M, Salehi M, Zandi T. Farsi version of the Neuropsychiatric Inventory: validity and reliability study among Iranian elderly with dementia. Int Psychogeriatr. (2012) 4:223–30. doi: 10.1017/S1041610211001797
32. Valer DB, Aires M, Fengler FL, Paskulin LM. Adaptation and validation of the Caregiver Burden Inventory for use with caregivers of elderly individuals. Rev Lat Am Enfermagem. (2015) 23:130–8. doi: 10.1590/0104-1169.3357.2534
33. Zhao QF, Tan L, Wang HF, Jiang T, Tan MS, Tan L, et al. The prevalence of neuropsychiatric symptoms in Alzheimer's disease: systematic review and meta-analysis. J Affect Disord. (2016) 190:264–71. doi: 10.1016/j.jad.2015.09.069
34. Lanctôt KL, Scherer RW Li A, Vieira D, Coulibaly H, Rosenberg PB, et al. Measuring apathy in Alzheimer's Disease in the apathy in dementia methylphenidate trial 2 (ADMET 2): a comparison of instruments. Am J Geriatr Psychiatry. (2021) 29:81–9. doi: 10.1016/j.jagp.2020.05.020
35. Delfino LL, Komatsu RS, Komatsu C, Neri AL, Cachioni M. Neuropsychiatric symptoms associated with family caregiver burden and depression. Dement Neuropsychol. (2021) 15:128–35. doi: 10.1590/1980-57642021dn15-010014
36. Chen P, Guarino PD, Dysken MW, Pallaki M, Asthana S, Llorente MD, et al. Neuropsychiatric symptoms and caregiver burden in individuals with Alzheimer's disease: the TEAM-AD VA cooperative study. J Geriatr Psychiatry Neurol. (2018) 31:177–85. doi: 10.1177/0891988718783897
37. Majer R, Adeyi O, Bagoly Z, Simon V, Csiba L, Kardos L, et al. Neuropsychiatric symptoms, quality of life and caregivers' burden in dementia. Open Med (Wars). (2020) 15:905–14. doi: 10.1515/med-2020-0124
38. Chen CT, Chang CC, Chang WN, Tsai NW, Huang CC, Chang YT, et al. Neuropsychiatric symptoms in Alzheimer's disease: associations with caregiver burden and treatment outcomes. QJM. (2017) 110:565–70. doi: 10.1093/qjmed/hcx077
39. Pinyopornpanish M, Pinyopornpanish K, Soontornpun A, Tanprawate S, Nadsasarn A, Wongpakaran N, et al. Perceived stress and depressive symptoms not neuropsychiatric symptoms predict caregiver burden in Alzheimer's disease: a cross-sectional study. BMC Geriatr. (2021) 21:180. doi: 10.1186/s12877-021-02136-7
40. Chen YA, Chang CC, Wang WF, Lin YS, Jhang KM, Lo TY, et al. Association between caregivers' burden and neuropsychiatric symptoms in female patients with Alzheimer's disease with varying dementia severity. J Multidiscip Healthc. (2021) 14:929–40. doi: 10.2147/JMDH.S298196
41. Ornstein K, Gaugler JE. The problem with “problem behaviors”: a systematic review of the association between individual patient behavioral and psychological symptoms and caregiver depression and burden within the dementia patient-caregiver dyad. Int Psychogeriatr. (2012) 24:1536–52. doi: 10.1017/S1041610212000737
42. Terum TM, Andersen JR, Rongve A, Aarsland D, Svendsboe EJ, Testad I. The relationship of specific items on the Neuropsychiatric Inventory to caregiver burden in dementia: a systematic review. Int J Geriatr Psychiatry. (2017) 32:703–17. doi: 10.1002/gps.4704
43. Okura T, Langa KM. Caregiver burden and neuropsychiatric symptoms in older adults with cognitive impairment: the aging, demographics, and memory study (ADAMS). Alzheimer Dis Assoc Disord. (2011) 25:116–21. doi: 10.1097/WAD.0b013e318203f208
44. Fu W, Li J, Fang F, Zhao D, Hao W, Li S. Subjective burdens among informal caregivers of critically ill patients: a cross-sectional study in rural Shandong, China. BMC Palliat Care. (2021) 20:167. doi: 10.1186/s12904-021-00858-4
45. Kang HS, Myung W, Na DL, Kim SY, Lee JH, Han SH, et al. Factors associated with caregiver burden in patients with Alzheimer's disease. Psychiatry Investig. (2014) 11:152–9. doi: 10.4306/pi.2014.11.2.152
46. Tsai CF, Hwang WS, Lee JJ, Wang WF, Huang LC, Huang LK, et al. Predictors of caregiver burden in aged caregivers of demented older patients. BMC Geriatr. (2021) 21:59. doi: 10.1186/s12877-021-02007-1
47. Pattanayak RD, Jena R, Tripathi M, Khandelwal SK. Assessment of burden in caregivers of Alzheimer's disease from India. Asian J Psychiatr. (2010) 3:112–6. doi: 10.1016/j.ajp.2010.06.002
48. Akpinar B, Küçükgüçlü O, Yener G. Effects of gender on burden among caregivers of Alzheimer's patients. J Nurs Scholarsh. (2011) 43:248–54. doi: 10.1111/j.1547-5069.2011.01402.x
49. Sousa MF, Santos RL, Turró-Garriga O, Dias R, Dourado MC, Conde-Sala JL. Factors associated with caregiver burden: comparative study between Brazilian and Spanish caregivers of patients with Alzheimer's disease (AD). Int Psychogeriatr. (2016) 28:1363–74. doi: 10.1017/S1041610216000508
50. Kahn PV, Wishart HA, Randolph JS, Santulli RB. Caregiver stigma and burden in memory disorders: an evaluation of the effects of caregiver type and gender. Curr Gerontol Geriatr Res. (2016) 2016:8316045. doi: 10.1155/2016/8316045
51. Adib-Hajbaghery M, Ahmadi B. Caregiver burden and its associated factors in caregivers of children and adolescents with chronic conditions. Int J Commun Based Nurs Midwifery. (2019) 7:258–69. doi: 10.30476/IJCBNM.2019.73893.0
52. Hosseiny R, Bastani F, Sayahi S, Momen-Abadi H, Alijanpoor-Aghamaleki M. The effect of educational-counseling program on general health of women as caregivers of patient, with Alzheimer disease. J Shahrekord Univ Med Sci. (2011) 13:83–92. Available online at: http://journal.skums.ac.ir/browse.php?a_id=921&sid=1&slc_lang=en
Keywords: neuropsychiatric symptoms, Alzheimer's disease, caregiver burden, Alzheimer's, caregiver
Citation: Iravani B, Abdollahi E, Eslamdoust-Siahestalkhi F and Soleimani R (2022) Neuropsychiatric Symptoms of Alzheimer's Disease and Caregiver Burden. Front. Neurol. 13:877143. doi: 10.3389/fneur.2022.877143
Received: 16 February 2022; Accepted: 12 May 2022;
Published: 29 July 2022.
Edited by:
Wesam Kooti, Kurdistan University of Medical Sciences, IranReviewed by:
Maedeh Sharghi, Azad Shoushtar University, IranCopyright © 2022 Iravani, Abdollahi, Eslamdoust-Siahestalkhi and Soleimani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elaheh Abdollahi, ZWxhaGVoYWJkb2xsYWhpMjVAZ21haWwuY29t; ZWFiZG9sbGFoaUByb2NrZXRtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.