
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 15 September 2022
Sec. Neurological Biomarkers
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.875134
This article is part of the Research TopicPotential Biomarkers in Neurovascular DisordersView all 50 articles
 Anran Wang1
Anran Wang1 Yapeng Li1
Yapeng Li1 Lue Zhou1
Lue Zhou1 Kai Liu1
Kai Liu1 Shaohua Li1
Shaohua Li1 Ce Zong1
Ce Zong1 Bo Song1
Bo Song1 Yuan Gao1
Yuan Gao1 Yusheng Li1
Yusheng Li1 Chuansheng Tian2
Chuansheng Tian2 Yurong Xing3
Yurong Xing3 Yuming Xu1*
Yuming Xu1* Longde Wang1,4*
Longde Wang1,4*Background: Carotid atherosclerosis, especially the rupture of unstable plaques, plays an important role in the development of stroke. A novel lipid ratio, the non-high-density lipoprotein cholesterol (non-HDL-C)/high-density lipoprotein cholesterol (HDL-C) ratio, contains both atherogenic and anti-atherogenic particle information, and has been shown to be associated with carotid atherosclerosis. However, there is no data on evaluating the association between non-HDL-C/HDL-C ratio and carotid plaque stability.
Methods: This study was carried out on 27,436 urban workers aged 20 years or older who participated in a comprehensive health screening between January 2016 and December 2017. Carotid plaque stability was assessed using ultrasonography. Multinomial logistic regression models were used to explore the relationship between the non-HDL-C/HDL-C ratio and carotid plaque stability by odds ratios (ORs) and 95% confidence intervals (CIs). Subgroup and sensitivity analyses were performed to verify the robustness of the results.
Results: Carotid plaque was detected in 7,161 (26.1%) participants, with stable and unstable plaque accounting for 3,277 (11.9%) and 3,884 (14.2%), respectively. The prevalence of stable carotid plaque substantially increased with increasing non-HDL-C/HDL-C ratio quartile levels (p for trend < 0.001) and with a similar association for unstable carotid plaque (p for trend < 0.001). The mean non-HDL-C/HDL-C ratios (mean ± SD) of non-carotid plaque (2.9 ± 1.1), stable carotid plaque (3.2 ± 1.2), and unstable carotid plaque (3.4 ± 1.4) gradually increased (p < 0.001). In multinomial logistic regression, ORs (95% CIs) for the highest vs. lowest quartile of the non-HDL-C/HDL-C ratio were 1.70 (1.48–1.95) between stable carotid plaques and no carotid plaque, 2.34 (2.06–2.67) between unstable carotid plaques and no carotid plaque, and 1.38 (1.18–1.61) between unstable carotid plaques and stable carotid plaque, after adjusting for common cardiovascular risk factors. The results of subgroup analysis and sensitivity analysis were similar.
Conclusion: Our findings suggested that the non-HDL-C/HDL-C ratio was significantly associated with carotid plaque stability and might be a useful indicator for the early identification of high-risk carotid plaque.
Stroke is a leading cause of death and disability worldwide (1). Carotid plaque stability plays a fundamental role in the development of ischemic stroke (2, 3). Rupture of unstable carotid plaque can lead to thrombosis, resulting in cerebrovascular occlusion and infarction. Approximately, 18–25% of ischemic stroke thromboembolisms originate from ruptured carotid plaques (4), and carotid plaque is also an important cause of cryptogenic stroke (5). However, carotid ultrasound screening in the general population is not recommended in the current guideline (6). Therefore, early identification of carotid plaque stability could help discover people at high risk of stroke, who might benefit from early pharmacological or surgical intervention.
It is well-known that high-density lipoprotein cholesterol (HDL-C) and non-HDL cholesterol (non-HDL-C) are associated with atherosclerosis (7–9). Non-HDL-C is considered to be a key factor underlying the process contributing to cardiovascular disease and atherosclerosis (10). The National Lipid Association has identified non-HDL-C as a primary therapeutic target (11), HDL-C, which is composed of the smallest and densest lipoprotein particles, inhibits atherosclerosis (12). HDL-C is negatively associated with cardiovascular (CV) events with each 1 mg/dl increase reducing CV events by 2–3% (7, 13, 14), and it exerts cardiovascular protective effects mainly through reverse cholesterol transfer, anti-inflammatory, antioxidant, anti-apoptotic, and vasodilatory effects (14). A novel lipid ratio, the non-HDL-C/HDL-C ratio, contains both atherogenic and anti-atherogenic particles information, and has been shown to be associated with a variety of dyslipidemia-related diseases such as diabetes mellitus (15–17), liver disease (18, 19), metabolic syndrome (20), and previous studies also demonstrated that the non-HDL-C/HDL-C ratio was associated with carotid atherosclerosis (21–23). In addition, the Atherosclerosis Risk in Communities (ARIC) study even found an independent association between non-HDL-C/HDL-C ratio and carotid plaque lipid core (24). The thicker the lipid core, the more likely it is to cause expansion of the necrotic core of the plaque, resulting in plaque rupture (25). Moreover, recently studies showed that the non-HDL-C/HDL-C ratio might be a better predictor of cardiovascular events than traditional lipid indices (26, 27). However, to date, there is no data on evaluating the association between non-HDL-C/HDL-C ratio and carotid plaque stability.
Therefore, we performed this study to clarify whether non-HDL-C/HDL-C ratio is significantly associated with carotid plaque stability.
The study population consisted of 28,537 Chinese adults who participated in a health examination in stroke screening sites of the First Affiliated Hospital of Zhengzhou University from January 2016 to December 2017. The exclusion criteria of this study were: subjects with any history of malignancy, infectious diseases, acute inflammation, liver disease, or renal disease. We also excluded subjects with missing data on TC or fasting blood glucose (FBG). After applying our exclusion criteria, a total of 27,436 participants were enrolled in this study.
We collected individual sociodemographic information (e.g., sex, age, and education), history of chronic diseases (e.g., diabetes, dyslipidemia, hypertension, coronary heart disease, and stroke), and lifestyle factors (e.g., smoking, drinking, vegetable and fruit consumption, physical activity, etc.) via a standard questionnaire by trained interviewers. Definition of history of stroke and coronary artery disease: previously diagnosed by a medical specialist or provided imaging data to support the diagnosis. Smoking, defined as smoking 1 cigarette per day for more than 1 year. Drinking, defined as alcoholic drink of at least ≥45 g each time per day during the last year. Vegetable consumption and Fruit consumption were divided into two groups (≥5 days/week and <5 days/week) using a standard consumption of 200 g per day. Physical activity, defined as regular exercise for at least 30 min per time in no less than 3 times per week. We measured weight, height, and resting blood pressure such as systolic blood pressure (SBP) and diastolic blood pressure (DBP). Obesity was defined as BMI ≥ 28 kg/m2.
In addition, overnight fasting blood samples were obtained from all subjects. Fasting blood glucose was measured using the glucose oxidase method. Lipid levels including total cholesterol (TC), triglyceride (TG), HDL-C, and low-density lipoprotein cholesterol (LDL-C) were measured using Olympus Au5400 automated biochemistry analyzer (First Chemical Co, Ltd, Japan). Hypertension was defined as SBP and/or DBP ≥ 140/90 mmHg, or the usage of antihypertensive medications. Dyslipidemia was defined as TG ≥ 2.26 mmol/L, TC ≥ 6.22 mmol/L, HDL-C < 1.04 mmol/L, LDL-C ≥ 4.14 mmol/L, self-reported history, or taking lipid-lowering drugs. Diabetes mellitus (DM) was defined as self-reported history, FPG ≥ 7.0 mmol/L, or taking antidiabetic agents.
Ultrasound technologists evaluated carotid plaques by qualified sonographers using the iU22 (Philips Healthcare), HA500 (Hitachi Healthcare), and DC-8 (Mindray), ultrasound system with 5–10 MHz transmission frequency. Two qualified sonographers measured each participant separately; discrepancies in measurement data were resolved by consensus. We examined plaques of bilateral common carotid artery, internal carotid artery, external carotid artery, and bulb. Carotid plaque was defined as a focal structure encroaching into the arterial lumen by at least 0.5 mm or 50% of the surrounding CIMT value, or CIMT > 1.5 mm (28, 29). Stable carotid plaques had a high level of homogeneous echogenicity and homogeneous texture with a regular smooth morphology. Unstable carotid plaques had an incomplete fibrous cap or ulceration with low level or heterogeneous echogenicity (30).
The population was divided into four groups based on the quartiles of the non-HDL-C/HDL-C ratio. Categorical variables were presented as frequency (%), which was compared using chi-square analysis. Continuous variables were described as the median with an interquartile range owing to the skewed distribution, which were compared by variance (ANOVA) or Mann–Whitney U-tests for continuous variables.
When participants were divided into 3 groups according to carotid plaque stability (non-carotid plaque, stable carotid plaque, and unstable carotid plaque), multinomial logistic regression models were used to explore the relationship between the non-HDL-C/HDL-C ratio and carotid plaque stability. To adjust for potential confounders, two models were developed: Model 1, adjusted for age, sex, education, smoking status, drinking status, vegetable consumption, fruit consumption, physical activity, BMI ≥ 28 kg/m2 (yes or no), stroke, coronary heart disease, hypertension, antihypertensive agents, diabetes mellitus, antidiabetic agents, lipid-lowering agents; Model 2, further adjusted for TG and FBG. The results were presented as odds ratios (ORs) and 95% confidence intervals (CIs). To verify the robustness of the relationship between non-HDL-C/HDL-C ratio and carotid plaque stability, analyses were carried out for different subgroups. In view of the effect of lipid-lowering agents on non-HDL-C/HDL-C ratio and carotid plaque stability, sensitivity analysis was performed after excluding people taking lipid-lowering agents.
All analyses above were conducted using R software (version 3.6.3). A two-sided p < 0.05 was considered statistically significant.
A total of 27,436 participants were recruited, 12,866 (46.9%) of them were male. The median (IQR) age of overall participants was 48 (41–55) years, and the median non-HDL-C/HDL-C ratio was 2.82 (IQR: 2.16–3.60). Compared with participants in the lowest quartile of non-HDL-C/HDL-C ratio, those with higher non-HDL-C/HDL-C ratio were more likely to be older and male; to be smoking, drinking, vegetable, and fruit consumption, active physical activity, obesity; to have a higher prevalence of hypertension, diabetes, and dyslipidemia; to have higher use of antidiabetic, antihypertensive, and lipid-lowering agents use, to have a higher level of SBP, DBP, FBG, TC, TG, LDL-C, and non-HDL level, while more likely to have a lower level of HDL-C. The characteristics of participants according to quartiles of the non-HDL-C/HDL-C ratio are presented in Table 1.
Carotid plaque was detected in 7,161 (26.1%) respondents, with stable and unstable plaque accounting for 3,277 (11.9%) and 3,884 (14.2%), respectively. As non-HDL-C/HDL-C ratio levels increased from the lowest quartile to the highest quartile, the prevalence was increased from 8.2 to 16% for stable carotid plaque (p for trend < 0.001) and from 7.7 to 20.8% for unstable carotid plaque (p for trend < 0.001). The mean non-HDL-C/HDL-C ratios of non-carotid plaque (mean ± SD, 2.9 ± 1.1), stable carotid plaque (mean ± SD, 3.2 ± 1.2), and unstable carotid plaque (mean ± SD, 3.4 ± 1.4) increased gradually and this trend was statistically significant (p < 0.001; Figure 1).
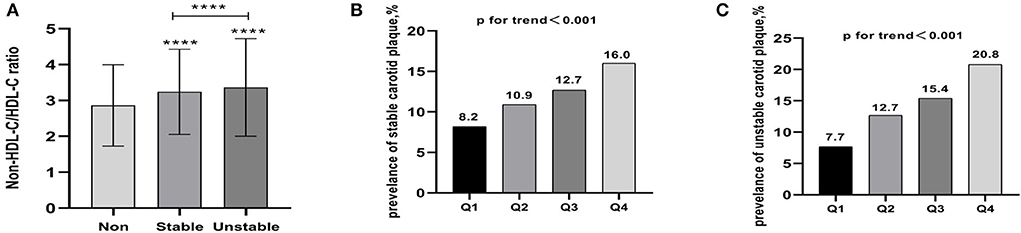
Figure 1. (A) The mean non-HDL-C /HDL-C ratios of non-carotid plaque, stable carotid plaque, and unstable carotid plaque (mean ± SD) increased gradually and this trend was statistically significant. (B) Prevalence of stable carotid plaque stratified by quartile the non-HDL-C/HDL-C ratio. (C) Prevalence of unstable carotid plaque stratified by quartile the non-HDL-C/HDL-C ratio. **** p < 0.001.
In multinomial logistic regression model 1 compared stable carotid plaques with no carotid plaque, the ORs (95% CIs) for the highest quartile of the non-HDL-C/HDL-C ratios were 1.71 (1.51–1.94). For every 1 unit increase in the non-HDL-C/HDL-C ratio, the prevalence of stable carotid plaque increased by 1.17 times. Compared unstable carotid plaques with no carotid plaque, the ORs (95% CIs) for the highest quartile of the non-HDL-C/HDL-C ratios were 2.21 (1.96–2.49). Moreover, for every 1 unit increase in the non-HDL-C/HDL-C ratio, the prevalence of unstable carotid plaque increased by 1.21 times. Compared to unstable carotid plaques with stable carotid plaque, the ORs (95% CIs) for the highest quartile of the non-HDL-C/HDL-C ratios were 1.29 (1.12–1.50). Moreover, for every 1 unit increase in the non-HDL-C/HDL-C ratio, the prevalence of unstable carotid plaque increased by 1.04 times.
Further adjustment for TG and FBG in model 2 did not change the association between the non-HDL-C/HDL-C ratio and carotid plaque stability. The corresponding ORs (95% CIs) for the highest vs. lowest quartile of the non-HDL-C/HDL-C ratio were 1.70 (1.48–1.95) between stable carotid plaques and no carotid plaque, 2.34 (2.06–2.67) between unstable carotid plaques and no carotid plaque, and 1.38 (1.18–1.61) between unstable carotid plaques and stable carotid plaque (Table 2).
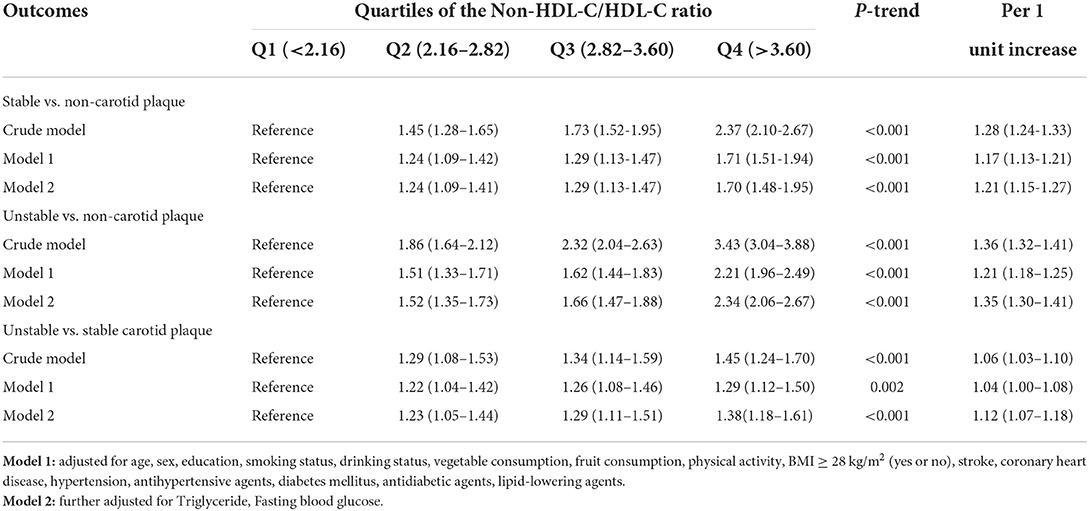
Table 2. Multinomial logistic odds ratios (ORs) (95% CI) of the association of the non-HDL-C/HDL-C ratio with carotid stability.
When the non-HDL-C/HDL-C ratio was considered as a continuous variable, subgroup analysis was conducted by stratification according to sex, age, BMI, hypertension, and diabetes. After the full adjustment variables, the association between non-HDL-C/HDL-C ratio and carotid plaque stability remained significant in gender, age, hypertension, and diabetes subgroups. While in a subgroup analysis of BMI ≥ 28 (kg/m2), there was no statistical significance between unstable carotid plaques and no carotid plaque (OR 1.06, 95% CI 0.95–1.17; Figure 2).
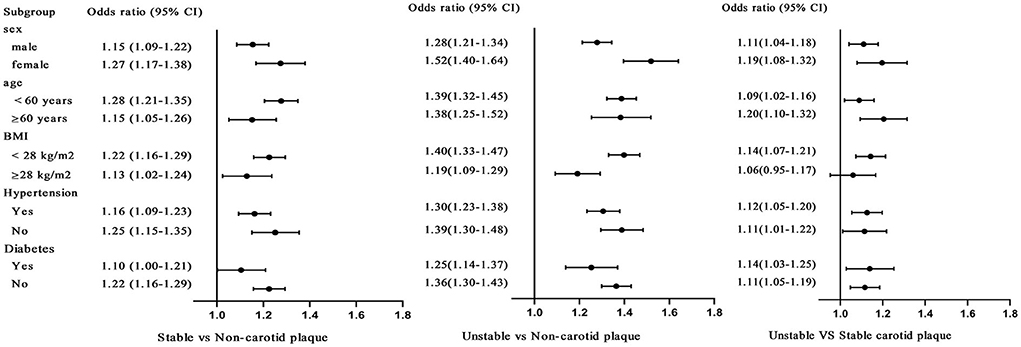
Figure 2. Subgroup analysis was conducted by stratification according to sex, age, BMI, hypertension, and diabetes, when the non-HDL-C/HDL-C ratio was considered as a continuous variable. After the fully adjustment, the same variables as Model 3 in Table 2, the odds ratios (ORs; 95% CIs) of the non-HDL-C/HDL-C ratio and carotid stability.
This sensitivity analysis was performed to assess the relationship between non-HDL-C/HDL-C ratio and carotid plaque stability in the subsample without taking lipid-lowering agents. After multivariable adjustment for the risk factors, sensitivity analyses showed similar results (Table 3).
This is the first population-based study to explore the relationship between non-HDL-C/HDL-C ratio and carotid plaque stability. We found that the prevalence of both stable and unstable carotid plaque increased significantly with increasing non-HDL-C/HDL-C ratios, independent of other relevant factors. Meanwhile, the mean non-HDL-C /HDL-C ratio gradually increased for non-carotid plaques, stable carotid plaques, and unstable carotid plaques; and this trend was statistically significant. Our findings, for the first time, demonstrated that non-HDL-C /HDL-C ratio was associated with carotid plaque stability in the general population.
Early atherosclerosis occurs mainly in the peripheral vasculature, such as the femoral and carotid arteries (31). The burden of carotid atherosclerosis has been increasing. A systematic review revealed the global burden of carotid atherosclerotic disease, with 21.1% of people aged 30–79 years suffering from carotid plaque in 2020, equivalent to 815.76 million people (32), and it was known that unstable plaque was an important factor in the development of cardiovascular disease (33). Moreover, many studies had shown that early preventive treatment and risk factor intervention were beneficial (34–36). However, carotid ultrasound screening in the general population is not recommended in the current guideline (6). Therefore, simple and accessible biomarkers for early determination of carotid plaque stability can help improve the understanding of the pathophysiology of cardiovascular disease and identify high-risk patients who may benefit from early intervention.
Our study found a gradual increase in the prevalence of carotid plaque as the non-HDL-C/HDL-C ratio gradually increased. As with our findings, the previous studies had shown that the non-HDL-C/HDL-C ratio was associated with carotid atherosclerosis (21–23). Qin et al. (21) found that carotid intima-media thickness gradually increased in the quartile of non-HDL-CHDL-C ratio in Chinese individuals of metabolic syndrome (p trend < 0.05). A multicenter study (22) found that postmenopausal women with higher non-HDL-C/HDL-C ratios had a greater chance of developing carotid atherosclerotic plaque (OR: 1.30, 95% CI: 1.07–1.58, p = 0.009) when adjusted for other cardiovascular risk factors. Recently, studies found that the non-HDL-C/HDL-C ratio might be a more accurate predictor of cardiovascular disease (26, 27). In addition, an asymptomatic polyvascular abnormalities in Community study (37) found that the odds of unstable carotid plaques at non-HDL-C levels in the middle and highest trilaterals were 1.02 (95% CI, 0.84–1.23) and 1.50 (95% CI, 1.23–1.82), respectively, after adjusting for confounders. Moreover, ARIC (24) study even found an independent association between non-HDL-C/HDL-C ratio and carotid plaque lipid core. It is well-known that plaque rich in lipid core is unstable and easy to rupture (25). All the above studies indirectly supported our findings that the non-HDL-C/HDL-C ratio might be associated with carotid plaque stability.
As a clinically easily accessible biomarker, the non-HDL-C/HDL-C ratio collects information on all atherogenic and antiatherogenic lipid particles. Non-high-density lipoprotein cholesterol (non-HDL-C) level is calculated by subtracting high-density lipoprotein cholesterol (HDL-C) from TC. Non-HDL-C consists of LDL-C, very low-density lipoprotein (VLDL-C), intermediate-density lipoprotein (IDL-C), chylomicrons, and their TG-rich lipoprotein remnants, and the protein mainly contains apolipoprotein B, which is a strong indicator of atherogenicity (13, 38). Non-HDL-C is considered to be a key factor underlying the process contributing to most cardiovascular diseases (10). The National Lipid Association has identified non-HDL-C as a primary therapeutic target (11), and the ESC/EAS guidelines for the management of dyslipidemia also recommended the inclusion of non-HDL in the assessment of cardiovascular disease risk (39). HDL-C is composed of the smallest and densest lipoprotein particles and mainly contains apolipoprotein A-I (APOA-I), which inhibits the production and mobilization of inflammatory cells and promotes the reversal of cholesterol transport (RCT) to inhibit atherosclerosis (12). HDL-C is thought to be negatively associated with cardiovascular disease events (7). The non-HDL-C/HDL-C ratio can reflect the balance between atherogenic and anti-atherogenic lipid particles, which may be the underlying mechanism for its relationship with plaque stability.
There are several limitations in our study. First, this is a cross-sectional study and no conclusions can be drawn on the causal relationship between non-HDL-C/HDL-C ratio and carotid plaque stability. Second, carotid plaque stability is assessed using ultrasound, which is not as accurate as MRI or angiography and cannot be verified with pathological specimens. However, we corrected for bias with a two-person blinded assessment. Third, our study did not collect information on HDL functionality, which is a better predictor of CV risk than HDL-C levels (40, 41), and it may be useful for high-risk carotid plaque identification. Finally, we did not collect follow-up information, which limited our ability to prospectively study, the impact of baseline non-HDL-C/HDL-C ratio on the evolution of plaque stability and cardiovascular events. Therefore, future prospective cohort studies are clearly needed.
In conclusion, this study found that the non-HDL-C/HDL-C ratio was associated with carotid plaque stability in the general population. The non-HDL-C/HDL-C ratio was highest in those with unstable carotid plaque, followed by those with stable carotid plaque and lowest in those with no carotid plaque. Our findings suggest that an elevated non-HDL-C/HDL-C ratio is independently associated with carotid plaque and its stability.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University. Written informed consent to participate in this study was provided by the patient/participants legal guardian/next of kin.
YMX and LW designed the research. YPL, LZ, YG, KL, SL, CZ, and YRX helped with the acquisition and analysis of the data. AW wrote the article. BS, YG, CT, and YSL contributed to the critical revision of the manuscript. All authors read and approved the final manuscript.
This work was supported by grant from the Ministry of Science and Technology of the People's Republic of China (2018YFC1311303), the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2020-PT310-01), the 2021 Youth Talent Promotion Project in Henan Province to KL (Grant No. 2021HYTP054), and 2021 Joint Construction Project of Henan Medical Science and Technology Breakthrough Plan to KL (Grant No. LHGJ20210336).
We thank the study participants and the clinical staff for their support and contribution to this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
2. Baber U, Mehran R, Sartori S, Schoos MM, Sillesen H, Muntendam P, et al. Prevalence, impact, and predictive value of detecting subclinical coronary and carotid atherosclerosis in asymptomatic adults: the bioimage study. J Am Coll Cardiol. (2015) 65:1065–74. doi: 10.1016/j.jacc.2015.01.017
3. Kamtchum-Tatuene J, Noubiap JJ, Wilman AH, Saqqur M, Shuaib A, Jickling GC. Prevalence of high-risk plaques and risk of stroke in patients with asymptomatic carotid stenosis: a meta-analysis. JAMA Neurol. (2020) 77:1524–35. doi: 10.1001/jamaneurol.2020.2658
4. Saba L, Saam T, Jäger HR, Yuan C, Hatsukami TS, Saloner D, et al. Imaging biomarkers of vulnerable carotid plaques for stroke risk prediction and their potential clinical implications. Lancet Neurol. (2019) 18:559–72. doi: 10.1016/S1474-4422(19)30035-3
5. Kopczak A, Schindler A, Bayer-Karpinska A, Koch ML, Sepp D, Zeller J, et al. Complicated carotid artery plaques as a cause of cryptogenic stroke. J Am Coll Cardiol. (2020) 76:2212–22. doi: 10.1016/j.jacc.2020.09.532
6. Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, Caughey AB, et al. Screening for asymptomatic carotid artery stenosis: us preventive services task force recommendation statement. JAMA. (2021) 325:476–81. doi: 10.1001/jama.2020.26988
7. Sun L, Clarke R, Bennett D, Guo Y, Walters RG, Hill M, et al. Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in chinese adults. Nat Med. (2019) 25:569–74. doi: 10.1038/s41591-019-0366-x
8. Holmes MV, Millwood IY, Kartsonaki C, Hill MR, Bennett DA, Boxall R, et al. Lipids, lipoproteins, and metabolites and risk of myocardial infarction and stroke. J Am Coll Cardiol. (2018) 71:620–32. doi: 10.1016/j.jacc.2017.12.006
9. Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, Thompson A, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. (2009) 302:1993–2000. doi: 10.1001/jama.2009.1619
10. Carr SS, Hooper AJ, Sullivan DR, Burnett JR. Non-HDL-cholesterol and apolipoprotein B compared with LDL-cholesterol in atherosclerotic cardiovascular disease risk assessment. Pathology. (2019) 51:148–54. doi: 10.1016/j.pathol.2018.11.006
11. Jacobson TA, Ito MK, Maki KC, Orringer CE, Bays HE, Jones PH, et al. National lipid association recommendations for patient-centered management of dyslipidemia: part 1–full report. J Clin Lipidol. (2015) 9:129–69. doi: 10.1016/j.jacl.2015.02.003
12. Di Bartolo BA, Cartland SP, Genner S, Manuneedhi Cholan P, Vellozzi M, Rye KA, et al. HDL improves cholesterol and glucose homeostasis and reduces atherosclerosis in diabetes-associated atherosclerosis. J Diabetes Res. (2021) 2021:6668506. doi: 10.1155/2021/6668506
13. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APHA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. (2019) 139:e1082–143. doi: 10.1161/CIR.0000000000000698
14. Badimón JJ, Santos-Gallego CG, Badimón L. [Importance of HDL cholesterol in atherothrombosis: how did we get here? Where are we going?]. Revista espanola de cardiologia. (2010) 63(Suppl 2):20–35. doi: 10.1016/S0300-8932(10)70150-0
15. Zhang N, Hu X, Zhang Q, Bai P, Cai M, Zeng TS, et al. Non-high-density lipoprotein cholesterol: high-density lipoprotein cholesterol ratio is an independent risk factor for diabetes mellitus: results from a population-based cohort study. J Diabetes. (2018) 10:708–14. doi: 10.1111/1753-0407.12650
16. Lin D, Qi Y, Huang C, Wu M, Wang C, Li F, et al. Associations of lipid parameters with insulin resistance and diabetes: a population-based study. Clin Nutr. (2018) 37:1423–9. doi: 10.1016/j.clnu.2017.06.018
17. Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X. Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol. (2014) 13:146. doi: 10.1186/s12933-014-0146-3
18. Yang S, Zhong J, Ye M, Miao L, Lu G, Xu C, et al. Association between the non-HDL-cholesterol to HDL-cholesterol ratio and non-alcoholic fatty liver disease in chinese children and adolescents: a large single-center cross-sectional study. Lipids Health Dis. (2020) 19:242. doi: 10.1186/s12944-020-01421-5
19. Wang K, Shan S, Zheng H, Zhao X, Chen C, Liu C. Non-HDL-cholesterol to HDL-cholesterol ratio is a better predictor of new-onset non-alcoholic fatty liver disease than non-HDL-cholesterol: a cohort study. Lipids Health Dis. (2018) 17:196. doi: 10.1186/s12944-018-0848-8
20. Kim SW, Jee JH, Kim HJ, Jin SM, Suh S, Bae JC, et al. Non-HDL-cholesterol/HDL-cholesterol is a better predictor of metabolic syndrome and insulin resistance than apolipoprotein B/apolipoprotein A1. Int J Cardiol. (2013) 168:2678–83. doi: 10.1016/j.ijcard.2013.03.027
21. Qin G, Tu J, Zhang C, Tang X, Luo L, Wu J, et al. The value of the apoB/apoA? ratio and the non-HDL-C/HDL-C ratio in predicting carotid atherosclerosis among chinese individuals with metabolic syndrome: a cross-sectional study. Lipids Health Dis. (2015) 14:24. doi: 10.1186/s12944-015-0023-4
22. Masson W, Epstein T, Huerín M, Lobo M, Molinero G, Siniawski D. Association between non-HDL-C/HDL-C ratio and carotid atherosclerosis in postmenopausal middle-aged women. Climacteric. (2019) 22:518–22. doi: 10.1080/13697137.2019.1631787
23. Liu Y, Zhang Z, Xia B, Wang L, Zhang H, Zhu Y, et al. Relationship between the non-HDLC-to-HDLC ratio and carotid plaques in a high stroke risk population: a cross-sectional study in China. Lipids Health Dis. (2020) 19:168. doi: 10.1186/s12944-020-01344-1
24. Virani SS, Catellier DJ, Pompeii LA, Nambi V, Hoogeveen RC, Wasserman BA, et al. Relation of cholesterol and lipoprotein parameters with carotid artery plaque characteristics: the atherosclerosis risk in communities (ARIC) carotid MRI Study. Atherosclerosis. (2011) 219:596–602. doi: 10.1016/j.atherosclerosis.2011.08.001
25. Nidorf SM, Fiolet A, Abela GS. Viewing atherosclerosis through a crystal lens: how the evolving structure of cholesterol crystals in atherosclerotic plaque alters its stability. J Clin Lipidol. (2020) 14:619–30. doi: 10.1016/j.jacl.2020.07.003
26. Zhu L, Lu Z, Zhu L, Ouyang X, Yang Y, He W, et al. Lipoprotein ratios are better than conventional lipid parameters in predicting coronary heart disease in Chinese Han people. Kardiologia Polska. (2015) 73:931–8. doi: 10.5603/KP.a2015.0086
27. Kouvari M, Panagiotakos DB, Chrysohoou C, Georgousopoulou EN, Tousoulis D, Pitsavos AC. Sex-related differences of the effect of lipoproteins and apolipoproteins on 10-year cardiovascular disease risk; insights from the Attica Study (2002-2012). Molecules. (2020) 25:1506. doi: 10.3390/molecules25071506
28. Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). In: An Update on Behalf of the Advisory Board of the 3rd, 4th and 5th Watching the Risk Symposia, at the 13th, 15th and 20th European Stroke Conferences. Mannheim; Brussels; Hamburg (2012). p. 290–6. doi: 10.1159/000343145
29. Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Desvarieux M, et al. Mannheim intima-media thickness consensus. Cerebrovasc Dis. (2004) 18:346–9. doi: 10.1159/000081812
30. Sztajzel R. Ultrasonographic assessment of the morphological characteristics of the carotid plaque. Swiss Med Weekly. (2005) 135:635–43.
31. Poredoš P, Cevc M, Blinc A. Characteristics of atherosclerosis in femoropopliteal artery and its clinical relevance. Atherosclerosis. (2021) 335:31–40. doi: 10.1016/j.atherosclerosis.2021.09.012
32. Song P, Fang Z, Wang H, Cai Y, Rahimi K, Zhu Y, et al. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: a systematic review, meta-analysis, and modelling study. Lancet Global Health. (2020) 8:e721–9. doi: 10.1016/S2214-109X(20)30117-0
33. Ooi YC, Gonzalez NR. Management of extracranial carotid artery disease. Cardiol Clin. (2015) 33:1–35. doi: 10.1016/j.ccl.2014.09.001
34. Naylor AR, Ricco JB, de Borst GJ, Debus S, de Haro J, Halliday A, et al. Editor's choice - management of atherosclerotic carotid and vertebral artery disease: 2017 Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg. (2018) 55:3–81. doi: 10.1016/j.ejvs.2017.10.014
35. Saba L, Brinjikji W, Spence JD, Wintermark M, Castillo M, Borst GJD, et al. Roadmap consensus on carotid artery plaque imaging and impact on therapy strategies and guidelines: an international, multispecialty, expert review and position statement. Am J Neuroradiol. (2021) 42:1566–75. doi: 10.3174/ajnr.A7223
36. Willeit P, Tschiderer L, Allara E, Reuber K, Seekircher L, Gao L, et al. Carotid intima-media thickness progression as surrogate marker for cardiovascular risk: meta-analysis of 119 clinical trials involving 100 667 patients. Circulation. (2020) 142:621–42. doi: 10.1161/CIRCULATIONAHA.120.046361
37. Wu J, Zhang J, Wang A, Chen S, Wu S, Zhao X. Association between non-high-density lipoprotein cholesterol levels and asymptomatic vulnerable carotid atherosclerotic plaques. Eur J Neurol. (2019) 26:1433–8. doi: 10.1111/ene.13973
38. Expert Expert Panel on Detection Evaluation and and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment Panel III). JAMA. (2001) 285:2486–97. doi: 10.1001/jama.285.19.2486
39. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Atherosclerosis. (2019) 290:140–205. doi: 10.1093/eurheartj/ehz455
40. Santos-Gallego CG, Rosenson RS. Role of HDL in those with diabetes. Curr Cardiol Rep. (2014) 16:512. doi: 10.1007/s11886-014-0512-5
Keywords: lipid ratio, non-HDL-C/HDL-C, carotid plaque, stability, cross-sectional study
Citation: Wang A, Li Y, Zhou L, Liu K, Li S, Zong C, Song B, Gao Y, Li Y, Tian C, Xing Y, Xu Y and Wang L (2022) Non-HDL-C/HDL-C ratio is associated with carotid plaque stability in general population: A cross-sectional study. Front. Neurol. 13:875134. doi: 10.3389/fneur.2022.875134
Received: 13 February 2022; Accepted: 15 August 2022;
Published: 15 September 2022.
Edited by:
John Zhang, Loma Linda University, United StatesReviewed by:
Danhong Wu, Fudan University, ChinaCopyright © 2022 Wang, Li, Zhou, Liu, Li, Zong, Song, Gao, Li, Tian, Xing, Xu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuming Xu, eHV5dW1pbmdAenp1LmVkdS5jbg==; Longde Wang, bG9uZ2VkX3dhbmdAeWVhaC5uZXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.