
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 15 June 2022
Sec. Endovascular and Interventional Neurology
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.856022
Objective: To investigate the surgical outcomes of single-position oblique lateral interbody fusion (OLIF) combined with percutaneous pedicle screw fixation (PPSF) in treating degenerative lumbar spondylolisthesis (DLS).
Methods: We retrospectively analyzed 85 patients with DLS who met the inclusion criteria from April 2018 to December 2020. According to the need to change their position during the operation, the patients were divided into a single-position OLIF group (27 patients) and a conventional OLIF group (58 patients). The operation time, intraoperative blood loss, hospitalization days, instrumentation accuracy and complication rates were compared between the two groups. The visual analog scale (VAS) and Oswestry Disability Index (ODI) were used to evaluate the clinical efficacy. The surgical segment's intervertebral space height (IDH) and lumbar lordosis (LL) angle were used to evaluate the imaging effect.
Results: The hospital stay, pedicle screws placement accuracy, and complication incidence were similar between the two groups (P > 0.05). The operation time and intraoperative blood loss in the single-position OLIF group were less than those in the conventional OLIF group (P < 0.05). The postoperative VAS, ODI, IDH and LL values were significantly improved (P < 0.05), but there was no significant difference between the two groups (P > 0.05).
Conclusions: Compared with conventional OLIF, single-position OLIF combined with PPSF is also safe and effective, and it has the advantages of a shorter operation time and less intraoperative blood loss.
Degenerative lumbar spondylolysis (DLS) refers to the displacement of the lumbar vertebral body relative to the lower vertebral body due to lumbar degenerative changes. The prevalence rate is approximately 4.1 ~ 11.1% (1). When severe neurological deficits occur or medical treatment is unsuccessful, surgery can be proposed. Traditional surgical methods include anterior lumbar interbody fusion (ALIF), lateral lumbar interbody fusion (LLIF), posterior lumbar interbody fusion (PLIF), translaminar lumbar interbody fusion (TLIF), etc. However, the fixed fusion segment is long and the trauma is large. It is necessary to strip the paraspinal muscles and remove the lamina or articular process, which can lead to many postoperative complications such as ischemic contracture of the paraspinal muscles, denervation, nerve damage, and large blood vessel damage.
Therefore, orthopedic surgeons need new surgical techniques to treat DLS, such as extreme lateral lumbar interbody fusion (XLIF) and oblique lumbar interbody fusion (OLIF), which avoid the need for paraspinal muscles, articular processes, spinal canal, dural sac, etc. The destruction of the structure has the advantages of less trauma and high fusion rate. XLIF is a retroperitoneal intermuscular muscle fiber of the psoas muscle. The deficiency of XLIF is mainly reflected in the lumbar plexus branches running in the psoas muscle, especially the L4/5 segment. Thigh pain, numbness, and weakness may occur after surgery. Since there are blood vessels in the psoas major muscle vertically distributed on the lateral side of the intervertebral disc, the puncture and expansion process may damage the blood vessels, resulting in hemorrhage and hematoma. The OLIF surgical technique, which has emerged in recent years, uses an approach that targets the region between the abdominal aorta and the psoas major in the retroperitoneal space, reducing the risk of damage to the psoas major and vascular nerves without the need for neuromonitoring during surgery. OLIF has the advantages of reduced trauma, better biomechanical stability and faster functional recovery, and it is gradually being used in clinical practice (2, 3).
Percutaneous pedicle screw fixation (PPSF) is a technique of inserting pedicle screws under X-ray and is a minimally invasive treatment technique. PPSF does not require a traditional large posterior incision, extensive dissection and traction on the paraspinal muscles, which can significantly reduce postoperative pain and recovery time (4). In recent years, PPSF has been widely used in clinical surgery with satisfactory results in the treatment of spinal degenerative diseases and fractures (5, 6).
However, conventional OLIF requires intervertebral fusion cage placement in the lateral position and pedicle screw placement in the prone position, which significantly increases the operative duration and risks of life-threatening complications, such as tracheal intubation falling off during anesthesia (7). Therefore, single-position OLIF combined with PPSF may be an effective and improved treatment for DLS. This study evaluated and analyzed the clinical, surgical and radiographic outcomes of single-position OLIF combined with PPSF in treating DLS.
This study was approved by the ethics committee of the Lanzhou University Second Hospital, and this study has been reported in line with the Strengthening the Reporting of Cohort Studies in Surgery (STROCSS) criteria (8). The inclusion criteria were as follows: persistent low back pain and lower extremity pain that was unresponsive to conservative treatment; determination of the affected level by computed tomography (CT) and magnetic resonance imaging (MRI); Meyerding classification of first- or second-degree DLS (Figure 1); complete clinical and imaging data; and follow-up of more than 12 months. The exclusion criteria were as follows: history of lumbar spine surgery; patients with lumbar trauma, infection, tumor or basic disease who could nottolerate surgery; coagulation dysfunction; inability to self-evaluate due to mental illness; and missing follow-up data. There were 27 patients in the single-position OLIF group, 10 males and 17 females, with an average age of 57.70 ± 7.20 years (range 46–74), and this group included 6 cases in L3/4 segments and 21 cases in L4/5 segments. The follow-up time was 25.15 ± 4.78 (range 16–33) months. There were 58 patients in the conventional OLIF group, 24 males and 34 females, with an average age of 60.88 ± 9.51 years (range 26–75), and this group included two cases in L2/3 segments, 10 cases in L3/4 segments and 46 cases in L4/5 segments. The follow-up time was 25.91 ± 5.26 (range 14–33) months.
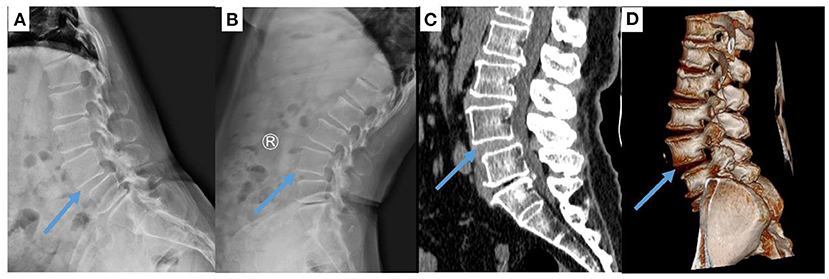
Figure 1. Image of L4/5 spondylolisthesis in a 65-year-old woman. (A,B) X-ray and (C,D) CT images show that the L4/5 vertebral body has slipped forward.
All the surgical procedures were performed by one orthopedic surgeon with extensive experience in spinal surgery in the Lanzhou University Second Hospital. The patient's sex and age, nail accuracy, operative duration, blood loss, hospitalization duration, complication incidence and other general data were collected and recorded. All patients were placed PPSF with “freehand,” since the OLIF procedure is already a standard procedure, not repeated in this paper (9) (Figure 2). The difference between the established and performed procedures was that we placed the cage and pedicle screws when the patient was in the right decubitus position. Since there was no difference in postoperative X-ray examination between the two groups, we reported only one case of DLS treated with OLIF (Figure 3).
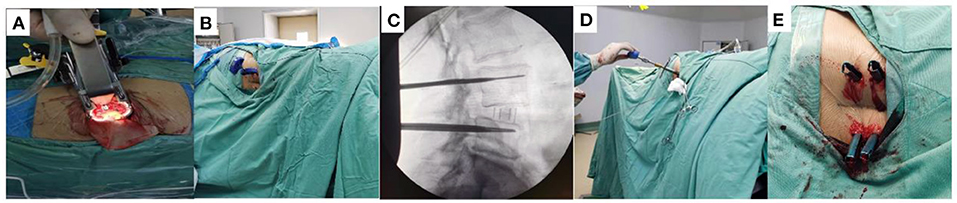
Figure 2. Surgical procedure for single-position OLIF. (A) Establish OLIF channel and place cage. (B) Place puncture needle in the lateral position by “freehand”. (C) Verification of whether the guidewire positioning is satisfactory by fluoroscopy. (D) Pedicle screw placement. (E) Installation of the pedicle screw system.
Data were collected from all patients before the operation, 1-week after the operation and at the last follow-up (> 12 months). The VAS score (10) and ODI (11) were used to evaluate pain and spinal function improvements. According to Lee et al. (12), the screw placement's accuracy was assessed as follows: level 0, the screw was located entirely in the pedicle; level I, <25% of the screw diameter broke through the pedicle; level, 25–50% of the screw broke through the pedicle; and level III, more than 50% of the screw diameter broke through the pedicle. The number of screws with a placement level of 0 was recorded. The lumbar lordosis (LL) angle and intervertebral disc height (IDH) were measured by lateral X-ray. The IDH was the distance from the highest portion of the lower endplate of the cephalad vertebra to the closest portion of the upper endplate of the caudal vertebra (13).
The data were analyzed using SPSS (version 26.0). The results are expressed as the mean ± standard deviation. The parametric data were tested by t-test, and the nonparametric data were tested by chi-square test. P < 0.05 was considered to indicate a significant difference.
All 85 patients completed the operation. The average operative durations of the single-position OLIF group and the conventional OLIF group were 118.56 ± 15.74 min and 133.19 ± 24.94 min, respectively, and the intraoperative blood loss was 66.96 ± 14.77 ml and 88.10 ± 16.25 ml, respectively; these values of the single-position OLIF group were significantly lower than those of the conventional OLIF group (p < 0.05). The patients' ages in the single-position OLIF group and the conventional OLIF group were 57.70 ± 7.20 and 60.88 ± 9.51, respectively, and the hospitalization days were 7.44 ± 2.01 days and 7.34 ± 1.48 days, respectively, and the values were not significantly different (Table 1).
In the single-position OLIF group, the postoperative lumbar VAS score decreased from 6.89 ± 1.21 points to 2.85 ± 0.99 points and was 1.67 ± 0.92 points at the last follow-up. The postoperative lower extremity VAS score decreased significantly from 6.61 ± 0.98 points to 2.81 ± 0.79 points and was 1.56 ± 0.75 points at the last follow-up. The postoperative ODI decreased from 56.15 ± 8.99 to 24.30 ± 7.03 and was 16.74 ± 5.65 at the last follow-up. Similarly, in the conventional OLIF group, the postoperative VAS score significantly decreased from 7.01 ± 1.18 to 2.93 ± 1.09 and was 1.55 ± 0.78 points at the last follow-up. The postoperative lower extremity VAS score also significantly decreased from 6.57 ± 1.01 to 2.88 ± 0.94 and was 1.71 ± 0.75 at the last follow-up. The postoperative ODI decreased from 55.26 ± 7.55 to 25.72 ± 8.42 and was 16.66 ± 5.06 at the last follow-up. Compared with the preoperative VAS and ODI scores, the postoperative VAS and ODI scores in both groups were significantly improved (P < 0.05). There was no significant difference in VAS or ODI between the two groups preoperatively, postoperatively or at the last follow-up (P > 0.05) (Table 2).

Table 2. Comparison of the lumbar VAS score and lower limb VAS score between the two groups preoperatively, postoperatively and at the last follow-up.
In the single-position OLIF group, the IDH was 8.30 ± 1.00 mm preoperatively, 13.58 ± 1.47 at 1 week postoperatively, and 13.31 ± 1.57 mm at the last follow-up. The LL angle was 35.31 ± 8.24 preoperatively, 47.37 ± 10.07 at 1 week postoperatively, and 46.76 ± 10.13 at the last follow-up. Similarly, in the conventional OLIF group, the IDH was 8.43 ± 1.44 mm preoperatively, 13.15 ± 1.50 mm at 1 week postoperatively, and 12.78 ± 1.64 mm at the last follow-up. The LL was 36.63 ± 8.73 preoperatively, 48.12 ± 10.39 at 1 week postoperatively, and 47.07 ± 10.09 at the last follow-up. The postoperative LL and IDH of the two groups were significantly improved compared with the preoperative LL and IDH of the two groups (P < 0.05), but there was no significant difference between the two groups (P > 0.05) (Table 3).
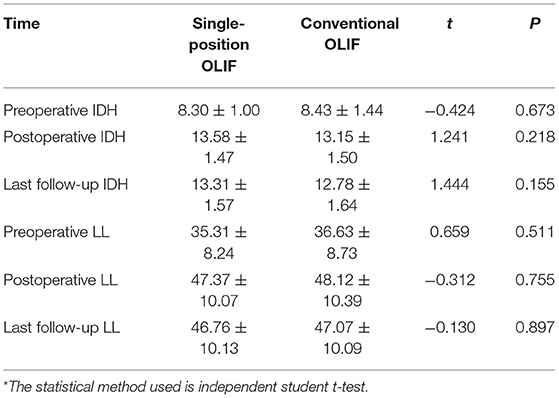
Table 3. Comparison of the ODI and IDH between the two groups preoperatively, postoperatively and at the last follow-up.
In the single-position OLIF group, the incidence of complications was 21.43% (6/27); three patients had transient high pain or numbness, and the symptoms disappeared naturally within half a year. One patient had segmental vascular injury. One patient had pain in the operation area of the iliac bone. One patient had cerebrospinal fluid leakage. After lying on his back and rehydration for 3 days, the symptoms of dizziness gradually relieved. One patient developed an abdominal bulge at the wound site. In the conservative OLIF group, the incidence of complications was 27.59% (16/58). During the operation, there were two cases of peritoneal injury and two cases of endplate injury. Five patients had transient thigh pain or numbness, one patient had low back pain, and two patients had lumbar myasthenia, and the symptoms gradually disappeared within half a year without treatment; two patients had transient hip flexion weakness, and the symptoms disappeared after nerve detumescence treatment; two patients had cerebrospinal fluid leakage, and the symptoms of dizziness gradually decreased after lying down and rehydration for seven days. There was no significant difference in the incidence of complications between the two groups (χ2 = 0.276, P = 0.599). In the single-position OLIF group, the pedicle screws placement accuracy was 96.30% (104/108), and that in the conventional OLIF group was 94.83% (220/232). There was no significant difference between the two groups (χ2 = 0.254, P = 0.614).
Over time, doctors have increasingly favored minimally invasive surgery. While ensuring clinical results, minimally invasive procedures minimize surgical trauma and ease patient suffering. Various minimally invasive techniques have been applied in the clinic and have benefitted many patients (14, 15). In recent years, the clinic has widely used minimally invasive oblique lateral spinal fusion surgery via OLIF. This procedure uses extraperitoneal blood vessels and the psoas muscle space for entry, allows the implantation of a larger fusion cage, increases the bone contact surface, and thus increases the fusion rate. This approach also allows complete opening of the intervertebral space, expansion of the intervertebral foramen area, and restoration of the spinal canal volume to achieve indirect decompression (2, 16). OLIF is widely used because of its ability to provide indirect decompression and its minimal invasiveness; it also helps restore the sagittal curve and coronal balance. It can be applied to treat various lumbar degenerative diseases, especially lumbar spondylolisthesis (17). Because of the lack of an ideal effect and the insufficient rotational stability achieved with a fusion cage alone, bilateral pedicle screw fixation is still the gold standard (18).
However, in conventional OLIF, the patient usually needs to be in the lateral position for cage placement and then transitioned to the prone position for pedicle screw placement. In this study, single-position OLIF significantly reduced the intraoperative blood loss and shortened the operation time compared with conventional OLIF. Single-position OLIF does not require repositioning, which helps save operative time. Additionally, because the operation time is reduced, the intraoperative blood loss and anesthesia time are reduced, which helps decrease the risk of infection and anesthesia decannulation. Although no patients with anesthesia decannulation and infection were observed in this study, patients may benefit from the close attention of anesthesiologists and strict compliance with routine aseptic procedures.
Similar to previous reports, the advantages of single-position OLIF and single-position LLIF over dual-position appear to be consistent and reduce the occupancy time of the operating room and workforce requirements (19, 20). The LLIF approach is an excellent choice for sagittal and coronal deformity correction, especially for lumbar degenerative scoliosis with lateral slippage (21). However, the LLIF approach may not be suitable for severe central canal stenosis, bony lateral recess stenosis, and high-grade slippage (22). Additionally, it is not suitable for patients with a history of retroperitoneal surgery or a retroperitoneal abscess, as well as patients with abnormal vascular anatomy. Potential risks of this technique include lumbar plexus, psoas, and bowel injury, especially at the L4/5 level (23). Vascular injury can be difficult to control once it occurs and represents another risk of the lateral transpsoas approach (21, 24). The shortcomings of OLIF are mainly reflected in the limitation of the approach and the limitation of the operative segment (only used for L2-5), the limitation of indirect decompression, and it cannot directly remove the prominent disc. In conclusion, single position technology may be an effective improvement measure.
In addition, the VAS score and ODI in this study were significantly lower after the operation than before the operation. The lumbar and lower limb symptoms were significantly improved. Similarly, IDH and LL on imaging were considerably enhanced compared with those before operation. Loss of the LL angle and changes in the IDH are closely related to the development of DLS. Therefore, it has important clinical significance to study the changes in the LL and IDH in DLS patients. The loss of LL is a key cause of low back pain in patients (25), and the restoration of the IDH at the affected segment improves the compression of the nerve root at the corresponding segment. In this study, single-position and conventional OLIF can significantly restore lumbar lordosis and intervertebral space height. There was no significant difference in the VAS, ODI, IDH, and LL between the two groups at the last follow-up. In short, single-position OLIF has clinical efficacy, high safety, and feasibility that are similar to those of conventional OLIF. Similar results have been obtained in other studies (9, 26).
The two groups of patients inevitably had different degrees of complications. Vascular injury, which is mainly the injury of vertebral segmental vessels and iliac vessels, is a common complication of OLIF (27). The risk of vascular injury by the OLIF technique is mainly related to the process of incision exposure, separation of psoas muscle and vascular sheath, and deep clearance of intervertebral space (28). Endplate injury mostly occurs in patients with osteoporosis (2). Improper operations during surgery, such as directly using a sharp reamer to remove the nucleus pulposus or following the wrong direction during intervertebral disc cleaning, can cause endplate damage. For patients with intraoperative endplate injury, screw fixation is necessary (29). Among our patients who underwent single-position OLIF, three patients (11.11%) had transient leg weakness during follow-up, and four patients (8.62%) in the conventional OLIF group had transient leg weakness during follow-up. The numbers were within the normal range (6.1–60.3%) (16, 30, 31). It can be seen that there is no significant difference between single-position OLIF and traditional OLIF in the incidence of postoperative complications, which is related to the OLIF procedure (32). Postoperative thigh numbness and hip flexion weakness may be caused by retraction of the psoas muscle and associated sensory nerves (33). These symptoms are mostly transient, and postoperative rehabilitation exercises can facilitate recovery in a short period. Hiyama et al. (34) reported that to prevent postoperative motor weakness regardless of the operation time, surgeons should be aware of the potential for surgical invasive of the psoas muscle during LLIF in older people ADDIN EN.CITE (34).
Pedicle screw misplacement is a common complication in spinal surgery. This study used “freehand” screw placement. “Freehand” is the manual placement of PPSF without using a robot, but still requires C-arm perspective assistance. According to reports, the displacement rate of “freehand” pedicle screw placement is 1.5–14.3% (35–37). Although the development of robotic technology (computer navigation technology) has helped to improve accuracy (38, 39), sometimes hospitals do not have computer technology navigation technology and often still perform “freehand” operations.
The single-position OLIF may be a new technology worthy of recommendation. Recently, Kotani et al. (40) found that single-position OLIF can provide a comparable fusion rate, segmental radiologic alignment, and symptomatic adjacent segment degeneration to MIS-TLIF surgery. Pham et al. (41) presented a novel technical report on the recommended workflow of simultaneous robotic single-position OLIF and demonstrated the'feasibility of placement of sacroiliac fixation in the lateral decubitus position. In addition, Diaz-Aguila et al. (26) found that robot-assisted OLIF can reduce the operative time while ensuring accurate and timely screen placement with minimal complications. As medical technology continues to develop, minimally invasive, robot-assisted surgical treatment will be increasingly used. We expect to see more reports on robot-assisted treatments for lumbar degenerative disease. In short, single-position OLIF serves as a safe, minimally invasive and effective surgical modality that saves valuable operating room time and is worth popularizing.
Although OLIF has advantages over conventional surgery in terms of the operative duration. However, we believe that surgeons should pay attention to the following factors. First, surgeons must have sufficient experience with OLIF combined with “freehand” placement of PPSF. Second, the patient's position is significant. There is a learning curve required for the surgeon to insert the percutaneous pedicle screw on the patient's right side (37, 42). On the one hand, being too close to the bed will affect the fluoroscopy. On the other hand, being too far away from the bed will limit the puncture angle of PPSF. ADDIN EN.CITE (42). According to our experience, the average time required to insert each percutaneous pedicle screw on the patient's right side was significantly longer than that required to insert each screw on the left side. This difference may occur because it is easier to apply force while inserting the percutaneous pedicle screw from the left side. It will limits the surgeon's ability to place the hand low enough to medialize the pedicle screw on the underside (42). Therefore, the patient's position should be as close as possible to the side of the operating bed so as not to block the operating bed when the nail is placed on the right side. In our opinion, the ideal position is from the edge of the bed to a quarter of the width of the bed.
There are some limitations to our study. First, because the single-position OLIF method has not yet been popularized, the sample size of our study is small and the follow-up time is short, and larger sample size and longer follow-up time are needed to confirm its safety and efficacy. Second, the survey subjects were limited to LDS patients treated at Lanzhou University Second Hospital. There may be differences among medical institutions due to differences in medical equipment. Third, surgeons may have varying experiences with OLIF techniques.
Single-position OLIF combined with PPSF significantly shortens the operation time, reduces the amount of intraoperative blood loss, is clinically effective, substantially improves the operation efficiency, and has good feasibility and safety. Thus, the treatment of DLS with single-position OLIF may be worth promoting.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Lanzhou University Second Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
PC and X-bZ conceived the study design and drafted the manuscript. Q-mZ supervised the data collection. H-hZ contributed to the revision. All authors contributed to the article and approved the submitted version.
This work was supported by the Natural Science Foundation of China (no. 31960175), the Natural Science Foundation of Gansu Province (no. 21JR1RA127), and the Natural Science Foundation of Gansu Province (no. 17JR5RA235).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
OLIF, Oblique lateral interbody fusion; PPSF, Percutaneous pedicle screw fixation; DLS, Degenerative lumbar spondylolisthesis; VAS, Visual Analog Scale; ODI, Oswestry Disability Index; IDH, Intervertebral disc height; LL, Lumbar lordosis; ALIF, Axial lumbar interbody fusion; LLIF, Lateral lumbar interbody fusion; PLIF, Posterior lumbar interbody fusion; TLIF, Translaminar lumbar interbody fusion; XLIF, Lateral lumbar interbody fusion; STROCSS, Strengthening the Reporting of Cohort Studies in Surgery; CT, Computed tomography; MRI, Magnetic resonance imaging; MIS-TLIF, Minimally invasive transforaminal interbody fusion.
1. Yi P, Tang X, Yang F. and Tan M. A retrospective controlled study protocol of transforaminal lumbar interbody fusion compared with posterior lumbar interbody fusion for spondylolisthesis. Medicine. (2020) 99:e22878. doi: 10.1097/MD.0000000000022878
2. Sato J, Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. and Takahashi K. Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J. (2017) 26:671–8. doi: 10.1007/s00586-015-4170-0
3. Li HM, Zhang RJ. and Shen CL. Radiographic and clinical outcomes of oblique lateral interbody fusion vs. minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar disease. World Neurosurg. (2019) 122:e627–38. doi: 10.1016/j.wneu.2018.10.115
4. Alander DH. and Cui S. Percutaneous pedicle screw stabilization: surgical technique, fracture reduction, and review of current spine trauma applications J Am Acad Orthop Surg. (2018) 26:231–40. doi: 10.5435/JAAOS-D-15-00638
5. Tian F, Tu LY, Gu WF, Zhang EF, Wang ZB, Chu G, et al. and Zhao J. Percutaneous vs. open pedicle screw instrumentation in treatment of thoracic and lumbar spine fractures: A systematic review and meta-analysis. Medicine. (2018) 97:e12535. doi: 10.1097/MD.0000000000012535
6. Jin M, Zhang J, Shao H, Liu J. and Huang Y. Percutaneous transforaminal endoscopic lumbar interbody fusion for degenerative lumbar diseases: a consecutive case series with mean 2-year follow-up. Pain Physician. (2020) 23:165–74. doi: 10.36076/ppj.2020/23/165
7. Cappuccino A, Cornwall GB, Turner AW, Fogel GR, Duong HT, Kim KD. and Brodke DS. Biomechanical analysis and review of lateral lumbar fusion constructs. Spine. (2010) 35:S361–367. doi: 10.1097/BRS.0b013e318202308b
8. Agha R, Abdall-Razak A, Crossley E, Dowlut N, Iosifidis C and Mathew G. STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int J Surg. (2019) 72:156–65. doi: 10.1016/j.ijsu.2019.11.002
9. Tan Y, Tanaka M, Sonawane S, Uotani K, Oda Y, Fujiwara Y, et al. and Ito Y. Comparison of simultaneous single-position oblique lumbar interbody fusion and percutaneous pedicle screw fixation with posterior lumbar interbody fusion using o-arm navigated technique for lumbar degenerative diseases. J Clin Med. (2021) 10:4938. doi: 10.3390/jcm10214938
11. Fairbank JC, Couper J, Davies JB. and O'brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. (1980) 66:271–3. doi: 10.1037/t04205-000
12. Lee SH, Kim KT, Suk KS, Lee JH, Son ES, Kwack YH. and Oh HS. Assessment of pedicle perforation by the cervical pedicle screw placement using plain radiographs: a comparison with computed tomography. Spine. (2012) 37:280–5. doi: 10.1097/BRS.0b013e31822338ad
13. Li Z, Yu S, Zhao Y, Hou S, Fu Q, Li F, et al. and Zhong H. Clinical and radiologic comparison of dynamic cervical implant arthroplasty versus anterior cervical discectomy and fusion for the treatment of cervical degenerative disc disease. J Clin Neurosci. (2014) 21:942–8. doi: 10.1016/j.jocn.2013.09.007
14. Momin AA. and Steinmetz MP. Evolution of minimally invasive lumbar spine surgery. World Neurosurg. (2020) 140:622–6. doi: 10.1016/j.wneu.2020.05.071
15. Smith ZA. and Fessler RG. Paradigm changes in spine surgery: evolution of minimally invasive techniques. Nat Rev Neurol. (2012) 8:443–50. doi: 10.1038/nrneurol.2012.110
16. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M. and Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine. (2015) 40:E175–182. doi: 10.1097/BRS.0000000000000703
17. Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, et al. and Takahashi K. Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J. (2015) 56:1051–9. doi: 10.3349/ymj.2015.56.4.1051
18. Reis MT, Reyes PM. Bse, Altun I, Newcomb AG, Singh V, Chang SW, Kelly BP and Crawford NR. Biomechanical evaluation of lateral lumbar interbody fusion with secondary augmentation. J Neurosurg Spine. (2016) 25:720–6. doi: 10.3171/2016.4.SPINE151386
19. Guiroy A, Carazzo C, Camino-Willhuber G, Gagliardi M, Fernandes-Joaquim A, Cabrera JP, et al. and Asghar J. Single-position surgery vs. lateral-then-prone-position circumferential lumbar interbody fusion: a systematic literature review. World Neurosurg. (2021) 151:e379–86. doi: 10.1016/j.wneu.2021.04.039
20. Ouchida J, Kanemura T, Satake K, Nakashima H, Ishikawa Y. and Imagama S. Simultaneous single-position lateral interbody fusion and percutaneous pedicle screw fixation using O-arm-based navigation reduces the occupancy time of the operating room. Eur Spine J. (2020) 29:1277–86. doi: 10.1007/s00586-020-06388-6
21. Arnold PM, Anderson KK. and Mcguire RA Jr. The lateral transpsoas approach to the lumbar and thoracic spine: A review. Surg Neurol Int. (2012) 3:S198–215. doi: 10.4103/2152-7806.98583
22. Malham GM, Parker RM, Goss B. and Blecher CM. Clinical results and limitations of indirect decompression in spinal stenosis with laterally implanted interbody cages: results from a prospective cohort study. Eur Spine J. (2015) 24 Suppl 3:339–45. doi: 10.1007/s00586-015-3807-3
23. Malham GM, Ellis NJ, Parker RM. and Seex KA. Clinical outcome and fusion rates after the first 30 extreme lateral interbody fusions. Sci World J. (2012) 2012:246989. doi: 10.1100/2012/246989
24. Lee YS, Park SW. and Kim YB. Direct lateral lumbar interbody fusion: clinical and radiological outcomes. J Neurosurg Spine. (2014) 55:248–54. doi: 10.3340/jkns.2014.55.5.248
25. Labelle H, Mac-Thiong JM. and Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J. (2011) 20 Suppl 5:641–6. doi: 10.1007/s00586-011-1932-1
26. Diaz-Aguilar LD, Shah V, Himstead A, Brown NJ, Abraham ME. and Pham MH. Simultaneous Robotic Single-Position Surgery (SR-SPS) with oblique lumbar interbody fusion: a case series. World Neurosurg. (2021) 151:e1036–43. doi: 10.1016/j.wneu.2021.05.043
27. Woods KR, Billys JB. and Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. (2017) 17:545–53. doi: 10.1016/j.spinee.2016.10.026
28. Zeng ZY, Xu ZW, He DW, Zhao X, Ma WH Ni WF, Song YX, et al. and Sui DX. Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop Surg. (2018) 10:98–106. doi: 10.1111/os.12380
29. He W, He D, Sun Y, Xing Y, Wen J, Wang W, et al. and Ye X. Standalone oblique lateral interbody fusion vs combined with percutaneous pedicle screw in spondylolisthesis. BMC Musculoskelet Disord. (2020) 21:184. doi: 10.1186/s12891-020-03192-7
30. Gammal ID, Spivak JM. and Bendo JA. Systematic review of thigh symptoms after lateral transpsoas interbody fusion for adult patients with degenerative lumbar spine disease. Int J Spine Surg. (2015) 9:62. doi: 10.14444/2062
31. Digiorgio AM, Edwards CS, Virk MS, Mummaneni PV. and Chou D. Stereotactic navigation for the prepsoas oblique lateral lumbar interbody fusion: technical note and case series. Neurosurg Focus. (2017) 43:E14. doi: 10.3171/2017.5.FOCUS17168
32. Hiyama A, Katoh H, Sakai D, Sato M, Tanaka M. and Watanabe M. Comparison of radiological changes after single- position versus dual- position for lateral interbody fusion and pedicle screw fixation. BMC Musculoskelet Disord. (2019) 20:601. doi: 10.1186/s12891-019-2992-3
33. Xu DS, Walker CT, Godzik J, Turner JD, Smith W. and Uribe JS. Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: a literature review. Ann Transl Med. (2018) 6:104. doi: 10.21037/atm.2018.03.24
34. Hiyama A, Katoh H, Nomura S, Sakai D, Sato M. and Watanabe M. Radiographs assessment of changes in the psoas muscle at L4-L5 level after single-level lateral lumbar interbody fusion in patients with postoperative motor weakness. J Clin Neurosci. (2021) 90:165–70. doi: 10.1016/j.jocn.2021.05.057
35. Smith ZA, Sugimoto K, Lawton CD. and Fessler RG. Incidence of lumbar spine pedicle breach after percutaneous screw fixation: a radiographic evaluation of 601 screws in 151 patients. J Spinal Disord Tech. (2014) 27:358–63. doi: 10.1097/BSD.0b013e31826226cb
36. Raley DA. and Mobbs RJ. Retrospective computed tomography scan analysis of percutaneously inserted pedicle screws for posterior transpedicular stabilization of the thoracic and lumbar spine: accuracy and complication rates. Spine. (2012) 37:1092–100. doi: 10.1097/BRS.0b013e31823c80d8
37. Blizzard DJ. and Thomas JA. MIS Single-position Lateral and Oblique Lateral Lumbar Interbody Fusion and Bilateral Pedicle Screw Fixation: feasibility and perioperative results. Spine. (2018) 43:440–6. doi: 10.1097/BRS.0000000000002330
38. Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC, et al. and Xenakis TA. Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. (2012) 21:247–55. doi: 10.1007/s00586-011-2011-3
39. Helm PA, Teichman R, Hartmann SL. and Simon D. Spinal Navigation and imaging: history, trends, and future. IEEE Trans Med Imaging. (2015) 34:1738–46. doi: 10.1109/TMI.2015.2391200
40. Kotani Y, Koike Y, Ikeura A, Tokunaga H. and Saito T. Clinical and radiologic comparison of anterior-posterior single-position lateral surgery versus MIS-TLIF for degenerative lumbar spondylolisthesis. J Orthop Sci. (2021) 26:992–8. doi: 10.1016/j.jos.2020.10.013
41. Pham MH, Diaz-Aguilar LD, Shah V, Brandel M, Loya J. and Lehman RA. Simultaneous robotic single position oblique lumbar interbody fusion with bilateral sacropelvic fixation in lateral decubitus. Neurospine. (2021) 18:406–12. doi: 10.14245/ns.2040774.387
Keywords: degenerative lumbar spondylolisthesis, oblique lumbar interbody fusion, single-position, minimally invasive spinal fusion, surgical technique
Citation: Cheng P, Zhang X-b, Zhao Q-m and Zhang H-h (2022) Efficacy of Single-Position Oblique Lateral Interbody Fusion Combined With Percutaneous Pedicle Screw Fixation in Treating Degenerative Lumbar Spondylolisthesis: A Cohort Study. Front. Neurol. 13:856022. doi: 10.3389/fneur.2022.856022
Received: 15 March 2022; Accepted: 16 May 2022;
Published: 15 June 2022.
Edited by:
Olivier De Witte, Université libre de Bruxelles, BelgiumReviewed by:
Panagiotis Korovessis, Olympion Medical Center, GreeceCopyright © 2022 Cheng, Zhang, Zhao and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hai-hong Zhang, aGFpaG9uZ3poYW5nMTk2OEAxNjMuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.