- 1Department of Physical Medicine and Rehabilitation, Harvard Medical School, Boston, MA, United States
- 2Spaulding Rehabilitation Hospital, Charlestown, MA, United States
- 3Spaulding Research Institute, Charlestown, MA, United States
- 4MassGeneral Hospital for Children Sports Concussion Program, Boston, MA, United States
- 5Home Base, A Red Sox Foundation and Massachusetts General Hospital Program, Charlestown, MA, United States
- 6Department of Psychology, University of Kentucky, Lexington, KY, United States
Importance: Prior research has shown a statistically significant association between sustaining a concussion and suicidality in adolescents, but this prior research controlled for relatively few variables predictive of suicidality.
Objective: To examine whether sustaining a concussion remained a significant predictor of suicidality after controlling for relevant covariates (e.g., sexual abuse/assault, bullying, substance use, depression), hypothesizing that the relationship between concussion and suicidality would become non-significant after controlling for these variables.
Design: This study involved secondary data analysis of the 2019 Youth Risk Behavior Surveillance (YRBS) System, a national cross-sectional study of adolescents. Analyses were stratified by gender.
Setting: A national sampling of U.S. high school students.
Participants: Eleven thousand two hundred sixty-two students in the YRBS database, including 5,483 boys and 5,779 girls.
Exposure(s): Participants included in the analyses reported whether, in the last year, they experienced a concussion and/or suicidality.
Main Outcomes and Measures: The main outcome was suicidality (i.e., ideation, planning, attempt), which was predicted by concussion in an unadjusted analysis and by concussion along with other risk factors in a multivariable analysis.
Results: The final sample included 11,262 participants with available data on concussion and suicidality in the last year (14–18 years-old; 51.3% girls; 49.0% White). Per unadjusted odds ratios with 95% confidence intervals, there was a relationship between concussion and suicidal ideation [girls: OR = 1.46 (1.24, 1.73); boys: OR = 1.69 (1.41, 2.03)], planning (girls: OR = 1.39 [1.16, 1.66]; boys: OR = 1.76 [1.44, 2.14]), and attempt [girls: OR = 1.70 (1.32, 2.19); boys: OR = 3.13, (2.37, 4.15)]. These relationships became mostly non-significant after controlling for relevant risk factors for suicidality. The adjusted odds ratios showed no relationship between concussion and suicidal ideation [girls: OR = 1.11 (0.86, 1.44); boys: OR = 1.24 (0.92, 1.69)] or planning (girls: OR = 1.07 [0.82, 1.40]; boys: OR = 1.12 [0.82, 1.55]); but a significant relationship with suicide attempts in boys [OR = 1.98 (1.28, 3.04)], but not girls [OR = 1.05 (0.74, 1.49)].
Conclusions and Relevance: There was an association between concussion and suicidality in U.S. high school students; however, after controlling for other variables (e.g., depression, sexual abuse/assault, illicit drug use), there was no association between concussion and suicidality aside from a significant relationship between concussion and attempts in boys.
Introduction
Suicidal thoughts and behaviors during adolescence are considered to be a public health problem, and many factors are known to be associated with increased risk for suicidality including genetics (1); female sex (2–4); mental disorders (5), such as depression (5, 6) and anxiety (6); impulsivity (7); attention-deficit hyperactivity disorder (8, 9); chronic illness (10); and sleep problems (11, 12). Substance use is associated with suicidality in adolescents (10), including illicit drugs (13, 14), marijuana (14, 15), alcohol (13, 15), and tobacco (13, 15). Psychosocial stressors and adverse childhood experiences also are associated with suicidality, including cyberbullying (16–18); not feeling safe at school (19); and sexual abuse, physical abuse, emotional abuse, and neglect (20–23).
Parental psychological distress (24), marital problems (25, 26), academic problems (27), and being bullied (27, 28) at school are risk factors for mental health difficulties in youth. In contrast, a high level of physical activity, and participation in team sports, are associated with higher self-esteem and life satisfaction, and lower risk for psychological distress (29–32). Adolescents who are physically active have a lower risk for experiencing a mood disorder (33) and suicidality (34). Adolescents who participate in sports are less likely to report depression (35) or suicidal ideation (35–37). Involvement in school sports during adolescence is associated with better mental health in young adulthood (38), and adolescents who are physically active in general, and maintain that behavior into early adulthood, experience better mental health (39). Factors that are associated with lower risk for suicidality in youth include regular exercise (40) and if they perceive that their parents understand their problems, monitor their academic and leisure time activities, and respect their privacy (3).
In recent years, epidemiological survey studies have found an association between sustaining a concussion, mostly during sports or recreational activities, and suicidality in high school students (41–43)—even after controlling for some factors known to be associated with suicidality, such as sex (2, 42, 43), depression (41), and bullying (42). However, none of these studies controlled for sexual abuse or assault, and none of the studies statistically modeled a more comprehensive set of factors known to be associated with suicidality in youth. Examining these associations is complex because some associations are small, and depression can be both a direct risk factor (i.e., a determinant) and a mediating variable (e.g., bullying leads to depression and suicidality). This gap in the literature was addressed, in the present study, by examining data from the 2019 “Youth Risk Behavior Survey” (YRBS) (44). Every 2 years, the Center for Disease Control and Prevention in the United States conducts a national survey of high school students (i.e., the YRBS). The purpose of this study is to examine the association between concussion and suicidality in high school students in the United States. It was hypothesized that in univariate analyses concussion would be associated with suicidality, similar to prior studies, but when controlling for other variables the association would be greatly attenuated or become non-significant.
Materials and Methods
Survey Methodology
The national survey is conducted every 2 years, during odd-numbered years, among students in grades 9–12 who attend a public and private schools in the United States. The Institutional Review Board of the CDC approved the protocol for the survey. The survey procedures were designed to allow for voluntary and anonymous participation. The students completed the survey in school during a single class period (~45 min).
The total national sample included 13,872 students from 136 schools (44). The response rate for the schools was 75.1%, the response rate for the students was 80.3%, yielding an overall response rate of 60.3% [i.e., (student response rate) × (school response rate)]. A questionnaire failed quality control if fewer than 20 responses remained after editing or if the student marked the same answer for 15 or more consecutive questions—yielding 195 questionnaires that failed quality control. The survey data from 1991 through 2019 are publicly available (https://www.cdc.gov/healthyyouth/data/yrbs/).
Survey Questions and Combined Variables
There were 99 questions, 89 of which were included in the standard questionnaire and 10 additional questions were added to address areas of interest for CDC and other stakeholders. The survey questions, recall periods, response options, and definitions of each variable are provided in the 2019 YRBS questionnaire and data user's guide available on the website (https://www.cdc.gov/healthyyouth/data/yrbs/). The survey questions used in this study are reprinted in Table 1. In addition, variables were combined based on two or more survey questions, and those variables are also presented in Table 1.
Statistical Analyses
The frequency of suicidal ideation, making a suicide plan, and making a suicide attempt was compared between boys and girls using χ2 tests, with p < 0.05 indicating a significant difference in frequency on these variables between gender groups. Three sets of binary logistic regressions were conducted separately in boys and girls, with (1) suicidal ideation, (2) making a suicide plan, and (3) making a suicide attempt serving as dichotomous dependent variables. Each suicide variable was predicted by each of the following variables in bivariate models, with the unadjusted odds ratio (OR) reported for each analysis: (1) being physically active for 5 or more days, (2) history of sexual abuse or assault, (3) feeling unsafe at school, (4) being threatened at school, (5) being bullied electronically or at school, (6) having on average D or F grades, (7) having insufficient sleep (i.e., 5 or fewer h on school nights), (8) current binge drinking, (9) current cigarette use, (10) lifetime use of 3 or more illicit drugs, (11) depression (i.e., feeling sad or hopeless), and (12) having a concussion from playing a sport or physical activity. Table 1 provides the specific question text of each of these variables. An OR above 1.00 with a 95% confidence interval (CI) not including 1.00 indicated the predictor was associated with greater odds of endorsing the dependent variable, whereas an OR below 1.00 with a 95% CI not including 1.00 indicated the predictor was associated with reduced odds of endorsing the dependent variable. A multivariable logistic regression was conducted including all predictors in the same model to examine the association between concussion and the suicide-related variables controlling for other variables protective against or increasing risk for suicide. The ORs can be interpreted in the same manner, but they reflect the increase or decrease in odds of suicidal ideation, suicide planning, and suicide attempt among adolescents with a concussion in the prior year, controlling for all other variables in the model.
Results
There are 13,677 students in the database, of whom 151 had missing data on their sex and 72 had missing data on their age. Of those 13,442 students between the ages of 14 and 18, 13,243 (98.5%) answered the question about suicidal ideation, and of those there were 11,262 who answered the question about concussion as well. For the final sample of 11,262, there were 5,779 girls (51.3%) and 5,483 boys (48.7%). In regard to self-identified race and ethnicity, the sample had the following composition: 49.0% White, 15.8% Multiracial and Hispanic/Latinx, 13.6% Black/African American, 8.3% Hispanic/Latinx, 5.0% Asian, 4.8% Multiracial and non-Hispanic/Latinx, 0.8% American Indian or Alaskan Native, 0.4% Native Hawaiian or Pacific Islander, and 2.2% with no reported race/ethnicity.
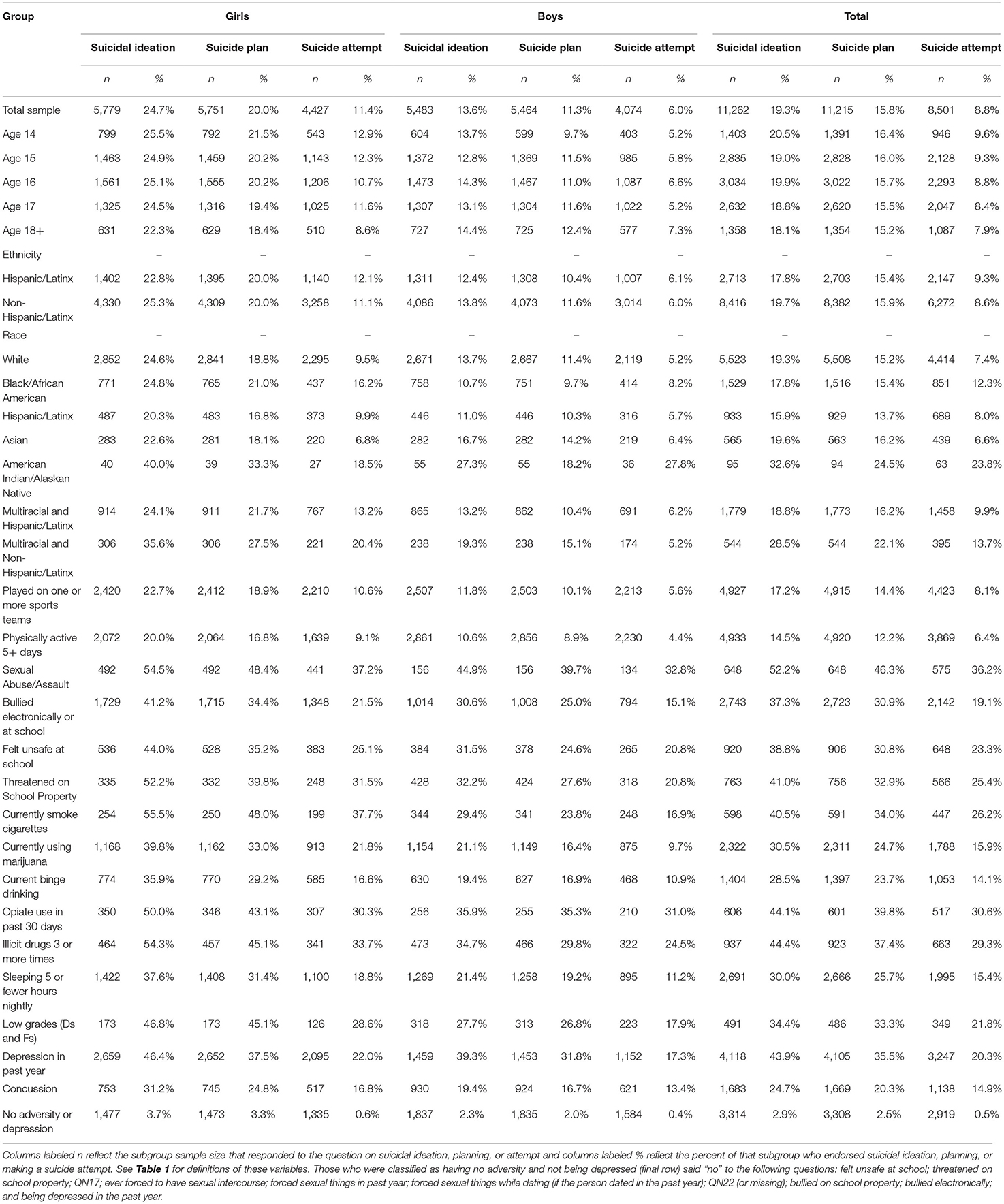
In the total sample, 19.3% endorsed having suicidal ideation in the past year, 15.7% endorsed having a plan for suicide, and 6.6% endorsed having attempted suicide. Girls endorsed suicidal ideation (24.7%) more frequently than boys [13.6%; χ2(1) = 221.49, p < 0.001; OR = 2.08 (95% CI: 1.89, 2.29)]; girls reported making a suicide plan (20.0%) more frequently than boys [11.3%; χ2(1) = 158.63, p < 0.001; OR = 1.96 (1.76, 2.18)]; and girls reported attempting suicide (11.4%) more frequently than boys [6.0%; χ2(1) = 75.63, p < 0.001; OR = 2.00 (95% CI: 1.71, 2.35)]. The percentages of youth endorsing suicidal ideation, plans, and attempts, stratified by sex and subgroups, are presented in Table 2. See Figure 1 for the percentages of youth, in specific subgroups, who endorsed suicidal ideation in the past year.
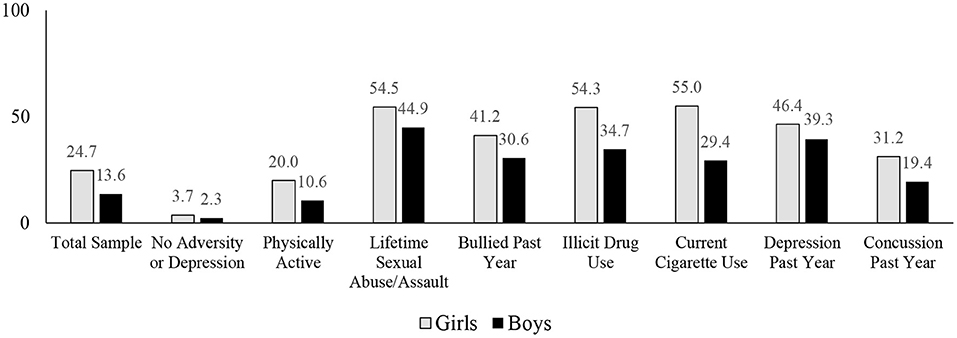
Figure 1. Percentages of high school students endorsing suicidal ideation over the past year. See Table 1 for the definitions of the variables. See Table 2 for the sample sizes. The no adversity or depression group responded “no” to all of the questions relating to sexual abuse or assault, feeling unsafe at school, being bullied, and being depressed in the past year. The physically active group reported being active for 60 min or more for at least 5 of the past 7 days. The illicit drug use groups reported a lifetime history of using drugs 3 or more times.
In the total sample, 12.8% reported sustaining a concussion in the past year (11.2% of girls and 14.4% of boys). Students who reported sustaining a concussion in the past year endorsed suicidal ideation more frequently (24.7%) than students who did not sustain a concussion in the past year [18.3%; χ2(1) = 36.69, p < 0.001; OR = 1.46 (1.29, 1.65)]. Students who reported sustaining a concussion endorsed a plan for suicide more frequently (20.3%) than students who did not sustain a concussion in the past year [15.0%; χ2(1) = 30.66, p < 0.001; OR = 1.45 (1.27, 1.65)]. Students who reported sustaining a concussion endorsed a suicide attempt more frequently (14.9%) than students who did not sustain a concussion in the past year [7.9%; χ2(1) = 61.72, p < 0.001; OR = 2.06 (1.72, 2.48)].
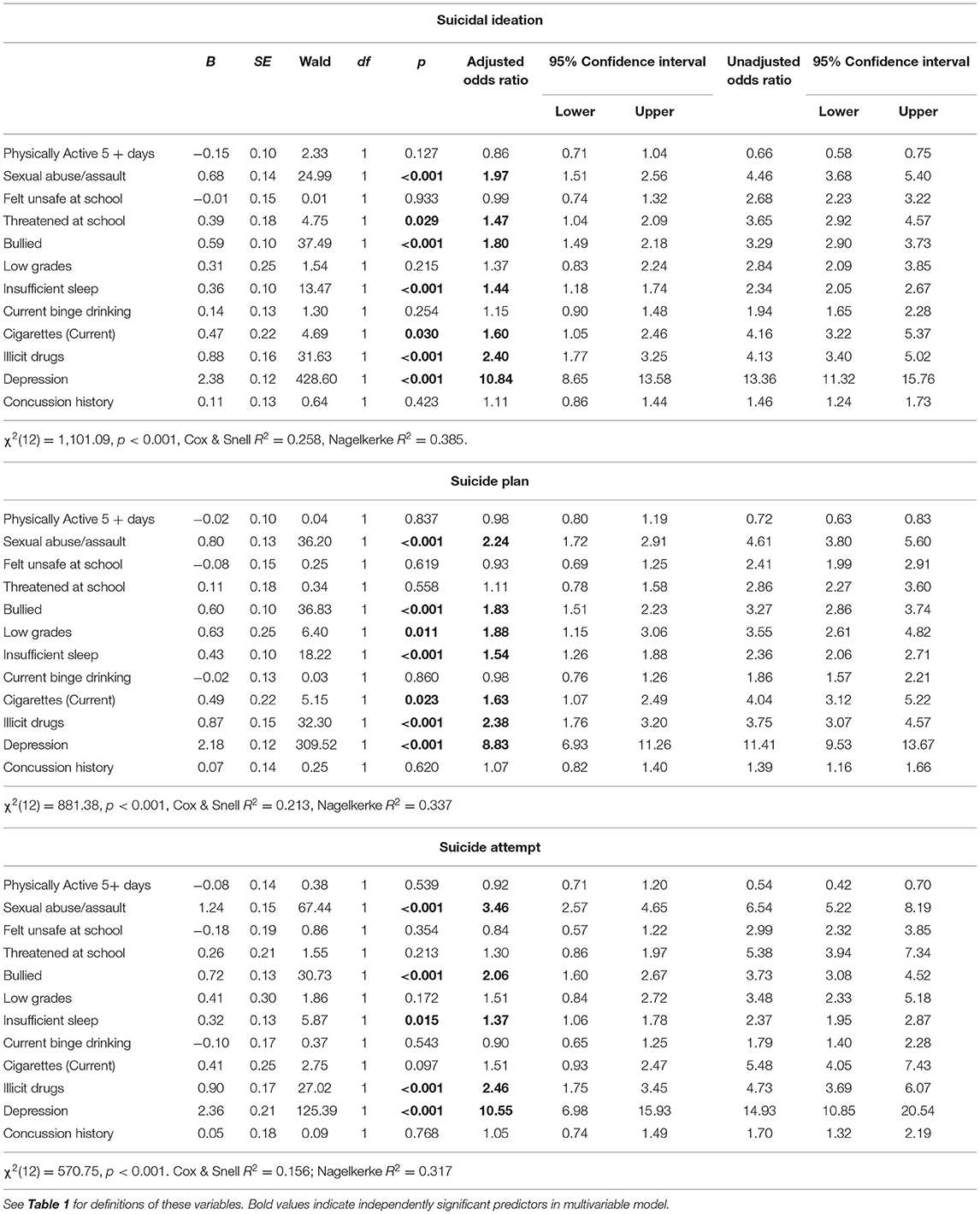
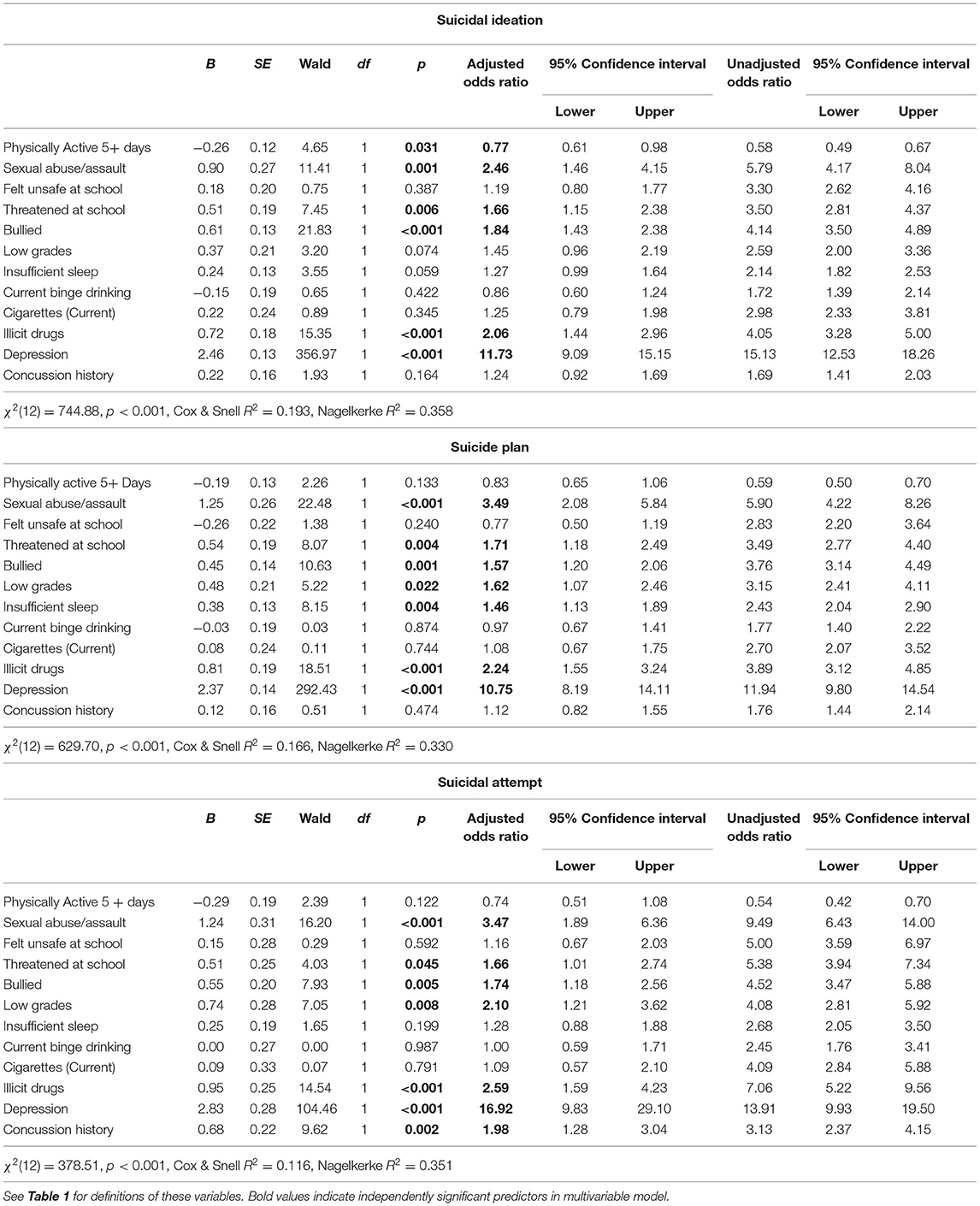
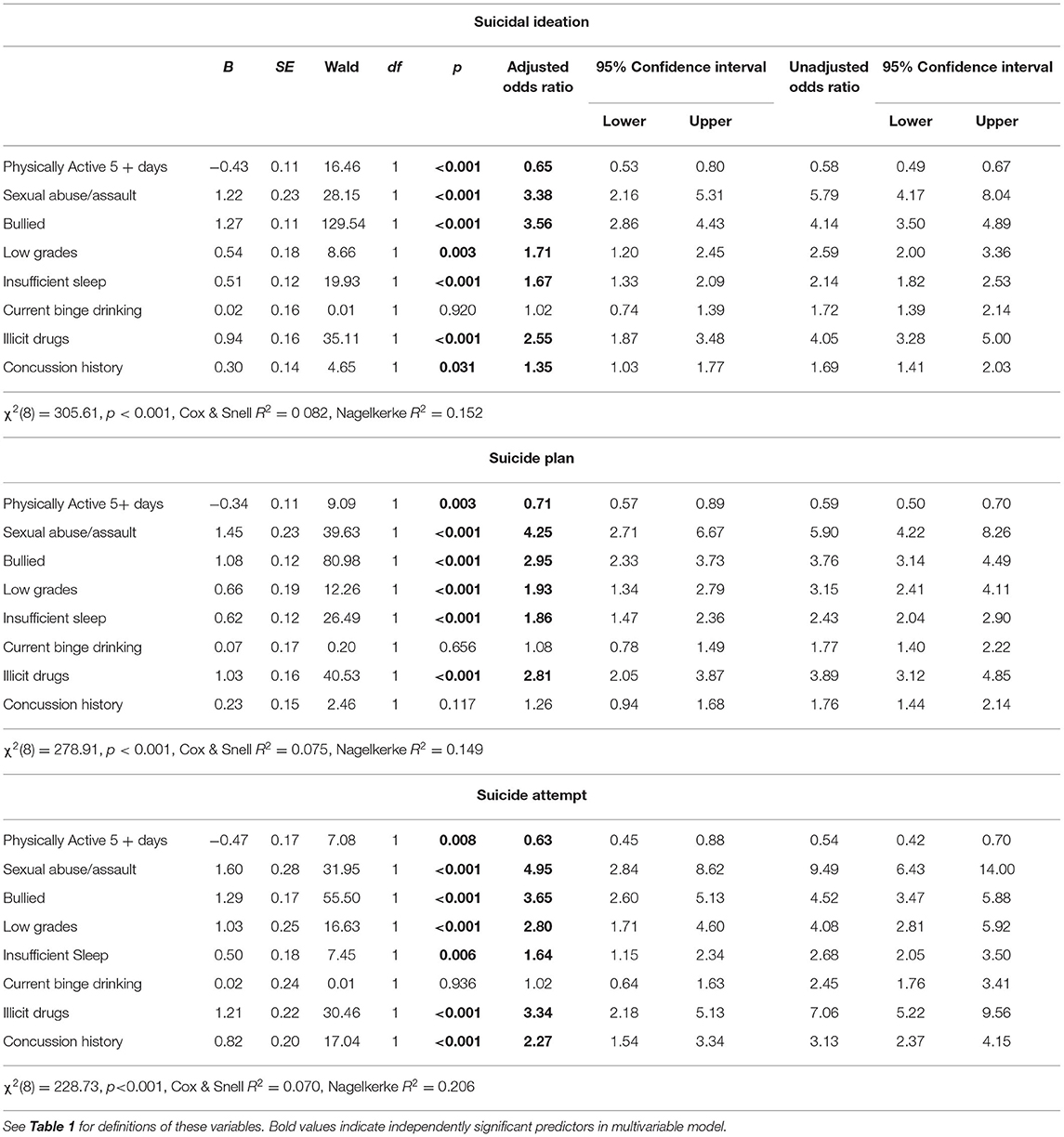
Multivariable binary logistic regression was used to examine the association between sustaining a concussion and suicidality after controlling for other known risk factors and correlates of suicidality. The results of the unadjusted and multivariable adjusted analyses for the girls are presented in Table 3 and for boys in Table 4. For girls, there was no significant association between sustaining a concussion and suicidal ideation, plans, or attempts after controlling for other risk factors. For boys, there was no significant association between sustaining a concussion and suicidal ideation or plans after controlling for other risk factors. However, there was a significant independent association between sustaining a concussion and suicide attempts.
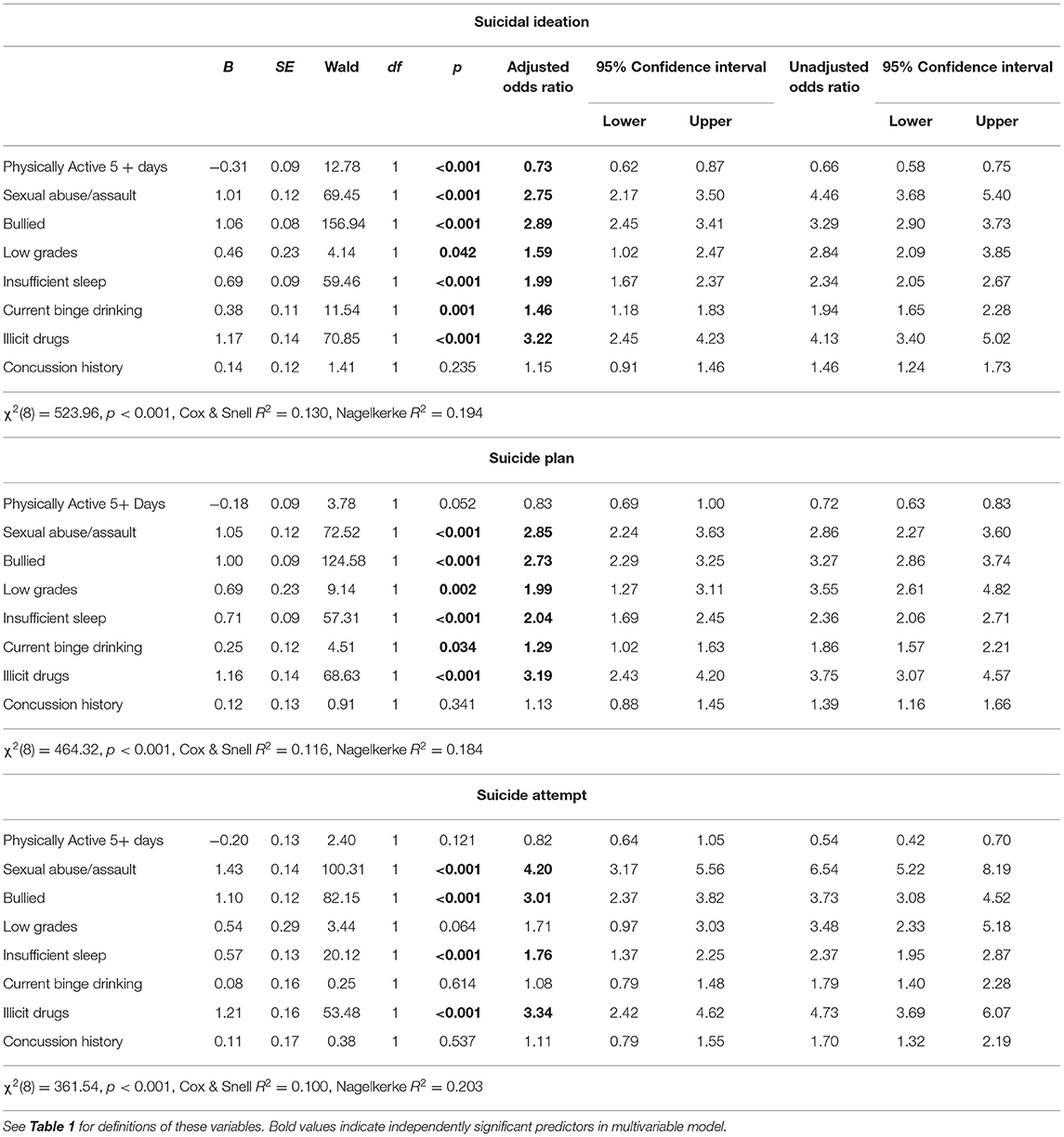
Exploratory logistic regressions were conducted without including depression as a variable, given its strong association with suicidality, as both a direct determinant and a mediator variable between the other covariates, and also how it might arise as a consequence of concussion. In addition, other variables were removed to examine whether concussion was associated with suicidality after removing additional variance associated with those variables, and to reduce the large number of predictors from 12 to 8 (i.e., Tables 5, 6). Feeling unsafe at school was removed because it was not a significant predictor in the larger model and due to some conceptual redundancy (shared variance) with bullying. Being threatened at school was also removed due to some potential redundancy with bullying. Current cigarette use was removed because it was a low frequency behavior relating to substance use (Table 2), and we wanted to keep higher frequency substance use behaviors such as binge drinking and illicit substance use in the model.
Again, for girls, there was no significant association between sustaining a concussion and suicidal ideation, plans, or attempts after controlling for other risk factors. For boys, there was a modest association between sustaining a concussion and suicidal ideation with the reduced set of predictors that was not observed when including the larger set of predictors in the model [p = 0.031, OR = 1.35 (95% CI: 1.03, 1.77)], meaning variance in suicidal ideation was explained by the removed predictors (e.g., current cigarette use and feeling unsafe or being threatened at school). The significant independent association between sustaining a concussion and suicide attempts [p < 0.001, OR = 2.27 (1.54, 3.34)] was observed in the reduced model, as was observed in the model with the full set of predictors. There was no significant association between sustaining a concussion and suicide planning after controlling for other risk factors.
Discussion
There was an association between sustaining a concussion in sports or recreational activity and suicidality in high school students surveyed in the United States in 2019. This is consistent with prior research using epidemiological survey data collected during 2013 (45) and 2017 (41–43, 46). After controlling for other variables, however, the associations between concussion and suicidality were greatly attenuated or became non-significant. For high school girls, there were no statistically significant associations in the adjusted analysis between concussion and suicidal thoughts, plans, or attempts. For girls, significant predictors of suicidal thoughts, in decreasing order of magnitude, were depression, sexual abuse/assault, current cigarette use, lifetime illicit drug use, being threatened at school, being bullied at school or electronically, low grades, feeling unsafe at school, insufficient sleep, and current binge drinking. For high school boys, there were no statistically significant associations in the adjusted analysis between concussion and suicidal thoughts or plans, but there was an association between concussion and suicide attempts. For boys, significant predictors of suicidal thoughts, in decreasing order of magnitude, were depression, sexual abuse/assault, being bullied at school or electronically, lifetime illicit drug use, being threatened at school, feeling unsafe at school, current cigarette use, low grades, insufficient sleep, and current binge drinking. Being physically active in the last 5 days was protective against suicidal ideation in both boys and girls, reducing the odds of suicidal thoughts by about half.
Past researchers using data from the YRBS have reported that suicidality in high school students is associated with female sex (2, 4), sexual minority status (47–49), adverse childhood experiences (50, 51), physical teen dating violence (52), forced sexual intercourse (18, 53), body weight perceptions [both overweight (54, 55) and underweight (55)], illicit drug use (13, 18), prescription opioid misuse (56–58) [especially in girls (59)], alcohol use (15, 18, 60, 61), marijuana use (13, 15, 62), bullying (18, 55, 63, 64) and cyberbullying (18, 55, 63–65), frequent physical fighting (66), excessive television/video game/internet use (67, 68), insufficient sleep (69), and even soft drink consumption (70). With so many variables being associated with suicidality in youth—especially given the very large national sample allowing the identification of statistically significant findings with small effect sizes—it is not particularly surprising that concussion was also associated in the present study, in univariate analyses, and in prior studies using the 2013 (45) and 2017 YRBS (41–43, 46). These studies found associations between concussion and suicidal ideation (41, 42, 45), planning (41, 45), and attempts (41–43, 45) through unadjusted analyses and multivariable analyses adjusting for some relevant variables. These prior studies controlled for demographic variables (e.g., age, gender, race/ethnicity, sexual orientation) and some other variables associated with mental health problems, such as alcohol use (45); bullying (42, 46); grades (41, 43); and physical activity, grades, sports participation, poor sleep, alcohol use, marijuana use, and depression (41). In general, the previous studies controlled for a relatively small number of variables, however, and none controlled for a history of sexual abuse or assault. The current study included all of these variables and more in a single multivariable logistic regression model, observing only an increased risk of suicide attempt in boys associated with concussion. When including multiple variables in the model, most predictors have a large reduction in effect size because the predictors are interrelated (i.e., they share variance), and the predictors with the smallest univariate odd ratios (including concussion) become non-significant (see Tables 3, 4).
As prior authors using YRBS data have noted, we cannot infer a causal association between concussion and suicidality given this is a cross-sectional survey study (41–43, 45, 46). That said, the association may be due, at least in part, to concussion being a major life stressor in boys, especially those with high athletic identity in their sport. Sustaining an injury in sports can be a major life stressor, and it can trigger or unmask difficulties with depression and suicidality (71). Concussions can remove athletes from their peer group and regular physical exercise, disrupt their academic performances, and lead to uncertainty about their futures. Such a disruption may have substantial psychological consequences for some adolescent boys. Among samples of predominantly male athletes, greater athletic identity has been associated with greater symptoms of depression following sport-related injuries (72), which may explain, in part, the current finding.
The array of vulnerability and risk factors for suicidality likely co-occur as precipitants to, and/or consequences of, psychological distress. Adolescents who engage in substance use may do so to cope with underlying emotional problems, or they may do so as recreation with their peers, with increased or riskier use leading to psychological distress. Adolescents who have experienced sexual violence may reside in environments with greater risk for being bullied, threatened, or further victimized, contributing to mental health problems and increasing risk for suicidality. A student-athlete who experiences a concussion may be removed from the social support of a team setting and may exercise less frequently when removed from practice or play. Considering the relationship between physical activity, mental health, and cognitive functioning (73), student-athletes removed from sport may have worse mental health, struggle more in school, and engage in high-risk activities to cope with their distress (e.g., substance use), which may contribute to greater distress.
Limitations
This study has several important limitations. The methodology, of course, was a survey—and this cross-sectional survey study does not allow us to draw causal inferences. The survey was administered during a single class period and the students were surrounded by their peers. The CDC implemented a system check that attempted to identify surveys that reflected mischievous responding by excluding those who responded the same way 15 or more times in a row. There are other possible response biases and styles that could have been operative among some students, such as social desirability, under or over-reporting, extreme response styles, acquiescence response styles, or yea-saying and nay-saying. Attempting to study different types of response styles and response biases is beyond the scope of this study; it is possible that some students' survey responses were influenced by certain bias, styles, or mischievous responding. The students were not asked any details about their concussions, such as the severity of their symptoms, the extent to which they received treatment or rehabilitation, or their recovery time—and there is no way to determine, from this cross-sectional survey, how many students developed depression and/or suicidality after sustaining a concussion, or whether depression or suicidality appeared to be causally related to sustaining a concussion.
There are also important statistical considerations. It is important to appreciate that we did not attempt to Model suicidality in youth, per se, but rather we aimed to examine the association of concussion with suicidality while considering multiple other variables of interest. There would be, as expected, some modest overfitting of the statistical model given the large number of variables included, although this overfitting is mitigated by the very large sample size. However, the most notable statistical issue relates to confounding and mediation. Depression is by far the strongest correlate with suicidality (i.e., greatest effect size). However, several of the other variables, for example sexual abuse/assault, illicit drug use, and bullying, are determinants of, or presumably causally linked to, depression. Thus, depression is a likely mediator between the predictors and suicidality. By including depression in the statistical model there is an introduction of bias due to either confounding (i.e., bidirectional relationship between depression and covariates) or mediation (i.e., a directional relationship). Therefore, the models are also presented without including depression (Tables 5, 6). It is also important to appreciate that other variables might contribute to confounding, mediation, or both. For example, bullying might also be linked to substance use. These interrelationships contribute to the large reductions in effect sizes, in the analyses, between the unadjusted (single variables) and adjusted (multiple variables) effect sizes.
Conclusions
Suicidality in high school students is a public health problem. There are many known predictors and correlates of suicidality in youth, with depression having, by far, the strongest association with suicidality in the present study. Other significant predictors, in both boys and girls, included a history of sexual abuse or assault and the use of illicit drugs. Concussion was not a significant predictor of ideation, plans, or attempts in girls after controlling for other variables, and it was not a significant predictor of ideation or plans in boys in multivariable analyses. Concussion remained a significant predictor in boys for suicide attempts after controlling for other variables. That said, children and adolescents presenting to specialty clinics for treatment and rehabilitation following concussion often experience emotional health difficulties, such as anxiety and depression (74, 75). Having pre-injury mental health problems is a risk factor for experiencing post-injury anxiety and depression (74, 76, 77)—and these are risk factors for suicidality. Because concussion can disrupt a young person's lifestyle in fairly dramatic ways, there are multiple potential reasons why some students who sustain concussions might evolve into experiencing depression and suicidality, and health care providers are encouraged to be mindful of this possibility and to provide swift, evidence-informed mental health care for youth who are suffering.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: Centers for Disease Control and Prevention (CDC) Youth Risk Behavior Surveillance System (YRBSS), https://www.cdc.gov/healthyyouth/data/yrbs/data.htm.
Ethics Statement
The Institutional Review Board of the CDC approved the protocol for the YRBS. Survey procedures were designed to protect students' privacy by allowing for anonymous and voluntary participation. Before survey administration, local parental permission procedures were followed.
Author Contributions
GI: conceptualized the study, conducted the literature review, conceptualized the statistical analyses, conducted the analyses, and drafted portions of the manuscript. JK: assisted with the literature review, conducted the analyses, drafted portions of the manuscript, and reviewed and approved the final manuscript. All authors contributed to the article and approved the submitted version.
Funding
GI has received unrestricted philanthropic support from ImPACT Applications, Inc., the Mooney-Reed Charitable Foundation, the National Rugby League, the Boston Bolts, and the Spaulding Research Institute. None of the above entities were involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Conflict of Interest
GI serves as a scientific advisor for NanoDx® Inc., Sway Operations, LLC, and Highmark, Inc. He has a clinical and consulting practice in forensic neuropsychology, including expert testimony, involving individuals who have sustained mild TBIs (including athletes). He has received research funding from several test publishing companies, including ImPACT Applications, Inc., CNS Vital Signs, and Psychological Assessment Resources (PAR, Inc.). He has received research funding as a principal investigator from the National Football League, and salary support as a collaborator from the Harvard Integrated Program to Protect and Improve the Health of National Football League Players Association Members.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zalsman G. Genetics of suicidal behavior in children and adolescents. In: Dwivedi Y, editor. The Neurobiological Basis of Suicide Frontiers in Neuroscience. Boca Raton (FL): CRC Press/Taylor & Francis (2012).
2. Pontes NMH, Ayres CG, Pontes MCF. Trends in depressive symptoms and suicidality: youth risk behavior survey 2009–2017. Nurs Res. (2020) 69:176–85. doi: 10.1097/NNR.0000000000000424
3. Kushal SA, Amin YM, Reza S, Shawon MSR. Parent-adolescent relationships and their associations with adolescent suicidal behaviours: secondary analysis of data from 52 countries using the global school-based health survey. EClinicalMedicine. (2021) 31:100691. doi: 10.1016/j.eclinm.2020.100691
4. West BA, Swahn MH, McCarty F. Children at risk for suicide attempt and attempt-related injuries: findings from the 2007 youth risk behavior survey. West J Emerg Med. (2010) 11:257–63.
5. Gili M, Castellvi P, Vives M., de la Torre-Luque A, Almenara J, Blasco MJ, et al. Mental disorders as risk factors for suicidal behavior in young people: A meta-analysis and systematic review of longitudinal studies. J Affect Disord. (2019) 245:152–62. doi: 10.1016/j.jad.2018.10.115
6. Soto-Sanz V, Castellvi P, Piqueras JA, Rodriguez-Marin J, Rodriguez-Jimenez T, Miranda-Mendizabal A, et al. Internalizing and externalizing symptoms and suicidal behaviour in young people: a systematic review and meta-analysis of longitudinal studies. Acta Psychiatr Scand. (2019) 140:5–19. doi: 10.1111/acps.13036
7. McHugh CM, Chun Lee RS, Hermens DF, Corderoy A, Large M, Hickie IB. Impulsivity in the self-harm and suicidal behavior of young people: a systematic review and meta-analysis. J Psychiatr Res. (2019) 116:51–60. doi: 10.1016/j.jpsychires.2019.05.012
8. Balazs J, Kereszteny A. Attention-deficit/hyperactivity disorder and suicide: A systematic review. World J Psychiatry. (2017) 7:44–59. doi: 10.5498/wjp.v7.i1.44
9. Septier M, Stordeur C, Zhang J, Delorme R, Cortese S. Association between suicidal spectrum behaviors and attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Neurosci Biobehav Rev. (2019) 103:109–18. doi: 10.1016/j.neubiorev.2019.05.022
10. Weeks M, Colman I. Predictors of suicidal behaviors in canadian adolescents with no recent history of depression. Arch Suicide Res. (2017) 21:354–64. doi: 10.1080/13811118.2016.1193076
11. Kearns JC, Coppersmith DDL, Santee AC, Insel C, Pigeon WR, Glenn CR. Sleep problems and suicide risk in youth: a systematic review, developmental framework, and implications for hospital treatment. Gen Hosp Psychiatry. (2020) 63:141–51. doi: 10.1016/j.genhosppsych.2018.09.011
12. Verkooijen S, de Vos N, Bakker-Camu BJW, Branje SJT, Kahn RS, Ophoff RA, et al. Sleep disturbances, psychosocial difficulties, and health risk behavior in 16,781 dutch adolescents. Acad Pediatr. (2018) 18:655–61. doi: 10.1016/j.acap.2018.03.003
13. Wong SS, Zhou B, Goebert D, Hishinuma ES. The risk of adolescent suicide across patterns of drug use: a nationally representative study of high school students in the United States from 1999 to 2009. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:1611–20. doi: 10.1007/s00127-013-0721-z
14. Mars B, Heron J, Klonsky ED, Moran P, O'Connor RC, Tilling K, et al. Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: a population-based birth cohort study. Lancet Psychait. (2019) 6:327–37. doi: 10.1016/S2215-0366(19)30030-6
15. Kahn GD, Wilcox HC. Marijuana use is associated with suicidal ideation and behavior among US adolescents at rates similar to tobacco and alcohol. Arch Suicide Res. (2020):1–14. doi: 10.1080/13811118.2020.1804025
16. John A, Glendenning AC, Marchant A, Montgomery P, Stewart A, Wood S, et al. Self-Harm, suicidal behaviours, and cyberbullying in children and young people: systematic review. J Med Internet Res. (2018) 20:e129. doi: 10.2196/jmir.9044
17. Moore SE, Norman RE, Suetani S, Thomas HJ, Sly PD, Scott JG. Consequences of bullying victimization in childhood and adolescence: a systematic review and meta-analysis. World J Psychiatry. (2017) 7:60–76. doi: 10.5498/wjp.v7.i1.60
18. Baiden P, Tadeo SK. Investigating the association between bullying victimization and suicidal ideation among adolescents: evidence from the 2017 youth risk behavior survey. Child Abuse Negl. (2020) 102:104417. doi: 10.1016/j.chiabu.2020.104417
19. Mori Y, Tiiri E, Khanal P, Khakurel J, Mishina K, Sourander A. Feeling unsafe at school and associated mental health difficulties among children and adolescents: a systematic review. Children (Basel). (2021) 8:232. doi: 10.3390/children8030232
20. Miller AB, Esposito-Smythers C, Weismoore JT, Renshaw KD. The relation between child maltreatment and adolescent suicidal behavior: a systematic review and critical examination of the literature. Clin Child Fam Psychol Rev. (2013) 16:146–72. doi: 10.1007/s10567-013-0131-5
21. Serafini G, Muzio C, Piccinini G, Flouri E, Ferrigno G, Pompili M, et al. Life adversities and suicidal behavior in young individuals: a systematic review. Eur Child Adolesc Psychiatry. (2015) 24:1423–46. doi: 10.1007/s00787-015-0760-y
22. Perez-Gonzalez A, Pereda N. Systematic review of the prevalence of suicidal ideation and behavior in minors who have been sexually abused. Actas Esp Psiquiatr. (2015) 43:149–58.
23. Evans E, Hawton K, Rodham K. Suicidal phenomena and abuse in adolescents: a review of epidemiological studies. Child Abuse Negl. (2005) 29:45–58. doi: 10.1016/j.chiabu.2004.06.014
24. Roustit C, Campoy E, Chaix B, Chauvin P. Exploring mediating factors in the association between parental psychological distress and psychosocial maladjustment in adolescence. Eur Child Adolesc Psychiatry. (2010) 19:597–604. doi: 10.1007/s00787-010-0094-8
25. Lamela D, Figueiredo B. Coparenting after marital dissolution and children's mental health: a systematic review. J Pediatr (Rio J). (2016) 92:331–42. doi: 10.1016/j.jped.2015.09.011
26. Harold GT, Sellers R. Annual research review: interparental conflict and youth psychopathology: an evidence review and practice focused update. J Child Psychol Psychiatry. (2018) 59:374–402. doi: 10.1111/jcpp.12893
27. Myklestad I, Roysamb E, Tambs K. Risk and protective factors for psychological distress among adolescents: a family study in the nord-trondelag health study. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:771–82. doi: 10.1007/s00127-011-0380-x
28. Sampasa-Kanyinga H, Lalande K, Colman I. Cyberbullying victimisation and internalising and externalising problems among adolescents: the moderating role of parent-child relationship and child's sex. Epidemiol Psychiatr Sci. (2018) 29:e8. doi: 10.1017/S2045796018000653
29. Guddal MH, Stensland SO, Smastuen MC, Johnsen MB, Zwart JA, Storheim K. Physical activity and sport participation among adolescents: associations with mental health in different age groups. results from the Young-HUNT study: a cross-sectional survey. BMJ Open. (2019) 9:e028555. doi: 10.1136/bmjopen-2018-028555
30. Steptoe A, Butler N. Sports participation and emotional wellbeing in adolescents. Lancet. (1996) 347:1789–92. doi: 10.1016/S0140-6736(96)91616-5
31. McMahon EM, Corcoran P, O'Regan G, Keeley H, Cannon M, Carli V, et al. Physical activity in European adolescents and associations with anxiety, depression and well-being. Eur Child Adolesc Psychiatry. (2017) 26:111–22. doi: 10.1007/s00787-016-0875-9
32. Eime RM, Young JA, Harvey JT, Charity MJ, Payne WR. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: informing development of a conceptual model of health through sport. Int J Behav Nutr Phys Act. (2013) 10:98. doi: 10.1186/1479-5868-10-98
33. He JP, Paksarian D, Merikangas KR. Physical activity and mental disorder among adolescents in the United States. J Adolesc Health. (2018) 63:628–35. doi: 10.1016/j.jadohealth.2018.05.030
34. Brown DR, Galuska DA, Zhang J, Eaton DK, Fulton JE, Lowry R, et al. Psychobiology and behavioral strategies. physical activity, sport participation, and suicidal behavior: US high school students. Med Sci Sports Exerc. (2007) 39:2248–57. doi: 10.1249/mss.0b013e31815793a3
35. Babiss LA, Gangwisch JE. Sports participation as a protective factor against depression and suicidal ideation in adolescents as mediated by self-esteem and social support. J Dev Behav Pediatr. (2009) 30:376–84. doi: 10.1097/DBP.0b013e3181b33659
36. Sabo D, Miller KE, Melnick MJ, Farrell MP, Barnes GM. High school athletic participation and adolescent suicide: a Nationwide US study. Int Rev Sociol Sport. (2005) 40:5–23. doi: 10.1177/1012690205052160
37. Taliaferro LA, Rienzo BA, Miller MD, Pigg RM. Jr., Dodd VJ High school youth and suicide risk: exploring protection afforded through physical activity and sport participation. J Sch Health. (2008) 78:545–53. doi: 10.1111/j.1746-1561.2008.00342.x
38. Jewett R, Sabiston CM, Brunet J, O'Loughlin EK, Scarapicchia T, O'Loughlin J. School sport participation during adolescence and mental health in early adulthood. J Adolesc Health. (2014) 55:640–4. doi: 10.1016/j.jadohealth.2014.04.018
39. Rangul V, Bauman A, Holmen TL, Midthjell K. Is physical activity maintenance from adolescence to young adulthood associated with reduced CVD risk factors, improved mental health and satisfaction with life: the HUNT study, Norway. Int J Behav Nutr Phys Act. (2012) 9:144. doi: 10.1186/1479-5868-9-144
40. Sibold J, Edwards E, Murray-Close D, Hudziak JJ. Physical activity, sadness, and suicidality in bullied US adolescents. J Am Acad Child Adolesc Psychiatry. (2015) 54:808–15. doi: 10.1016/j.jaac.2015.06.019
41. Miller GF, DePadilla L, Jones SE, Bartholow BN, Sarmiento K, Breiding MJ. The association between sports- or physical activity-related concussions and suicidality among US high school students, 2017. Sports Health. (2021) 13:187–97. doi: 10.1177/1941738120939913
42. Mantey DS, Omega-Njemnobi O, Barroso CS, Kelder SH. Self-reported history of concussions is associated with risk factors for suicide completion among high school students. J Affect Disord. (2020) 263:684–91. doi: 10.1016/j.jad.2019.11.047
43. Yang MN, Clements-Nolle K, Parrish B, Yang W. Adolescent concussion and mental health outcomes: a population-based study. Am J Health Behav. (2019) 43:258–65. doi: 10.5993/AJHB.43.2.3
44. Underwood JM, Brener N, Thornton J, Harris WA, Bryan LN, Shanklin SL, et al. Overview and methods for the youth risk behavior surveillance system - United States, 2019. MMWR Suppl. (2020) 69:1–10. doi: 10.15585/mmwr.su6901a1
45. Wangnoo T, Zavorsky GS, Owen-Smith A. Association between concussions and suicidal behaviors in adolescents. J Neurotrauma. (2020) 37:1401–7. doi: 10.1089/neu.2018.5721
46. Mantey DS, Omega-Njemnobi O, Kelder SH. Self-reported history of concussions is associated with risk factors for suicide completion among middle school students: a cross-sectional study. J Psychiatr Res. (2021) 132:191–4. doi: 10.1016/j.jpsychires.2020.10.022
47. Pollitt AM, Mallory AB. Mental and sexual health disparities among bisexual and unsure latino/a and black sexual minority youth. LGBT Health. (2021) 8:254–62. doi: 10.1089/lgbt.2020.0374
48. Johns MM, Lowry R, Haderxhanaj LT, Rasberry CN, Robin L, Scales L, et al. Trends in violence victimization and suicide risk by sexual identity among high school students - youth risk behavior survey, United States, 2015–2019. MMWR Suppl. (2020) 69:19–27. doi: 10.15585/mmwr.su6901a3
49. Liu RT, Walsh RFL, Sheehan AE, Cheek SM, Carter SM. Suicidal ideation and behavior among sexual minority and heterosexual youth: 1995–2017. Pediatrics. (2020) 145: e20192221. doi: 10.1542/peds.2019-2221
50. Aytur SA, Carlino S, Bernard F, West K, Dobrzycki V, Malik R. Social-ecological theory, substance misuse, adverse childhood experiences, and adolescent suicidal ideation: Applications for community-academic partnerships. J Community Psychol. (2021). doi: 10.1002/jcop.22560
51. Johnson RM, Hill AV, Jones VC, Powell TW, Dean LT, Gilreath TD. Racial/Ethnic inequities in adverse childhood experiences and selected health-related behaviors and problems among maryland adolescents. Health Promot Pract. (2021). doi: 10.1177/15248399211008238
52. Baiden P, Mengo C, Small E. History of physical teen dating violence and its association with suicidal behaviors among adolescent high school students: results from the. youth risk behavior survey. J Interpers Violence. (2015) 2019:886260519860087. doi: 10.1177/0886260519860087
53. Basile KC, Clayton HB, Rostad WL, Leemis RW. Sexual violence victimization of youth and health risk behaviors. Am J Prev Med. (2020) 58:570–9. doi: 10.1016/j.amepre.2019.11.020
54. Daly M, Robinson E, Sutin AR. Perceived overweight and suicidality among US adolescents from 1999 to 2017. Int J Obes (Lond). (2020) 44:2075–9. doi: 10.1038/s41366-020-0620-9
55. Singh S, Thompson CJ, Kak R, Smith LN, Quainoo N. Impact of body weight perceptions and electronic bullying on suicide-related risk behaviors among youth: results from youth risk behavior surveillance system, 2015. J Sch Health. (2021) 91:29–36. doi: 10.1111/josh.12974
56. Wilkins NJ, Clayton H, Jones CM, Brown M. Current prescription opioid misuse and suicide risk behaviors among high school students. Pediatrics. (2021) 147. doi: 10.1542/peds.2020-030601
57. Clayton HB, Bohm MK, Lowry R, Ashley C, Ethier KA. Prescription opioid misuse associated with risk behaviors among adolescents. Am J Prev Med. (2019) 57:533–9. doi: 10.1016/j.amepre.2019.05.017
58. Divin AL, Zullig KJ. The Association between non-medical prescription drug use and suicidal behavior among United States adolescents. AIMS Public Health. (2014) 1:226–40. doi: 10.3934/Publichealth.2014.4.226
59. Pontes NMH, Ayres C, Wunnenberg M, Pontes MCF. Gender differences in the relationship between prescription opioid misuse and depressive symptoms and suicidality among US high school students. Nurs Outlook. (2021) 69:641–51. doi: 10.1016/j.outlook.2021.01.006
60. Phillips GL 2nd, Turner BC, Felt D, Marro RL, Wang X, Ruprecht MM, et al. Alcohol use and suicidality by sexual orientation among U.S. youth, 2009–2017. Am J Prev Med. (2020)59:394–403. doi: 10.1016/j.amepre.2020.03.024
61. Hingson RW, Zha W. Binge drinking above and below twice the adolescent thresholds and health-risk behaviors. Alcohol Clin Exp Res. (2018) 42:904–13. doi: 10.1111/acer.13627
62. Chadi N, Li G, Cerda N, Weitzman ER. Depressive symptoms and suicidality in adolescents using e-cigarettes and marijuana: a secondary data analysis from the youth risk behavior survey. J Addict Med. (2019) 13:362–5. doi: 10.1097/ADM.0000000000000506
63. Humphries KD Li L, Smith GA, Bridge JA, Zhu M. Suicide attempts in association with traditional and electronic bullying among heterosexual and sexual minority U. S high school students. J Adolesc Health. (2021) 68:1211–4. doi: 10.1016/j.jadohealth.2020.12.133
64. Messias E, Kindrick K, Castro J. School bullying, cyberbullying, or both: correlates of teen suicidality in the 2011 CDC youth risk behavior survey. Compr Psychiatry. (2014) 55:1063–8. doi: 10.1016/j.comppsych.2014.02.005
65. Sibold J, Edwards EM, O'Neil L, Murray-Close D, Hudziak JJ. Bullying environment moderates the relationship between exercise and mental health in bullied US Children. J Sch Health. (2020) 90:194–9. doi: 10.1111/josh.12864
66. Swahn MH, Bossarte RM, Palmier JB, Yao H, Van Dulmen MH. Psychosocial characteristics associated with frequent physical fighting: findings from the 2009 national youth risk behavior survey. Inj Prev. (2013) 19:143–6. doi: 10.1136/injuryprev-2012-040381
67. Rostad WL, Basile KC, Clayton HB. Association among television and computer/video game use, victimization, and suicide risk among U. S high school students J Interpers Violence. (2021) 36:2282–305. doi: 10.1177/0886260518760020
68. Messias E, Castro J, Saini A, Usman M, Peeples D. Sadness, suicide, and their association with video game and internet overuse among teens: results from the youth risk behavior survey 2007 and 2009. Suicide Life Threat Behav. (2011) 41:307–15. doi: 10.1111/j.1943-278X.2011.00030.x
69. McKnight-Eily LR, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, Perry GS. Relationships between hours of sleep and health-risk behaviors in US adolescent students. Prev Med. (2011) 53:271–3. doi: 10.1016/j.ypmed.2011.06.020
70. Solnick SJ, Hemenway D. Soft drinks, aggression and suicidal behaviour in US high school students. Int J Inj Contr Saf Promot. (2014) 21:266–73. doi: 10.1080/17457300.2013.815631
71. Putukian M. The psychological response to injury in student athletes: a narrative review with a focus on mental health. Br J Sports Med. (2016) 50:145–8. doi: 10.1136/bjsports-2015-095586
72. Renton T, Petersen B, Kennedy S. Investigating correlates of athletic identity and sport-related injury outcomes: a scoping review. BMJ Open. (2021) 11:e044199. doi: 10.1136/bmjopen-2020-044199
73. Biddle SJ, Ciaccioni S, Thomas G, Vergeer I. Physical activity and mental health in children and adolescents: an updated review of reviews and an analysis of causality. Psychol Sport Exerc. (2019) 42:146–55. doi: 10.1016/j.psychsport.2018.08.011
74. Ellis MJ, Ritchie LJ, Koltek M, Hosain S, Cordingley D, Chu S, et al. Psychiatric outcomes after pediatric sports-related concussion. J Neurosurg Pediatr. (2015) 16:709–18. doi: 10.3171/2015.5.PEDS15220
75. Gornall A, Takagi M, Morawakage T, Liu X, Anderson V. Mental health after paediatric concussion: a systematic review and meta-analysis. Br J Sports Med. (2021) 55:1048–58. doi: 10.1136/bjsports-2020-103548
76. Vargas G, Rabinowitz A, Meyer J, Arnett PA. Predictors and prevalence of postconcussion depression symptoms in collegiate athletes. J Athl Train. (2015) 50:250–5. doi: 10.4085/1062-6050-50.3.02
Keywords: suicide, concussion, head injury, traumatic brain injury, sports
Citation: Iverson GL and Karr JE (2022) Association Between Concussions and Suicidality in High School Students in the United States. Front. Neurol. 13:810361. doi: 10.3389/fneur.2022.810361
Received: 06 November 2021; Accepted: 09 March 2022;
Published: 12 April 2022.
Edited by:
Cameron Bass, Duke University, United StatesReviewed by:
Jason Luck, Duke University, United StatesHal S. Wortzel, Veterans Health Administration (VHA), United States
Copyright © 2022 Iverson and Karr. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Grant L. Iverson, Z2l2ZXJzb25AbWdoLmhhcnZhcmQuZWR1
 Grant L. Iverson
Grant L. Iverson Justin E. Karr
Justin E. Karr