- 1Department of Biomedical Science, College of Health Science, Debre Tabor University, Debre Tabor, Ethiopia
- 2Department of Pediatrics and Child Health, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 3Department of Psychiatry, Dr. Amebachew Memorial Hospital, Tach Gaynt, Ethiopia
- 4Pharmacology and Toxicology Unit, Department of Pharmacy, College of Health Science, Debre Tabor University, Debre Tabor, Ethiopia
- 5Addis Zemen Hospital, Addis Zemen, Ethiopia
Introduction: The occurrence of three or more of the following signs and symptoms, such as headache, dizziness, exhaustion, irritability, sleeplessness, difficulties in concentrating, or memory problems, following a head injury is referred to as post-concussion syndrome (PCS). Even though post-concussion syndrome has not been studied in Ethiopia, the productive age group is frequently affected by health issues related to head trauma, which either directly or indirectly affect the growth of the nation.
Objective: To assess the prevalence and associated factors of post-concussion syndrome among patients with traumatic brain injury at Debre Tabor Comprehensive Hospital, Debre Tabor, North Central Ethiopia.
Methods: A successive sampling technique was used to conduct a hospital-based cross-sectional study on 405 traumatic brain injury patients at Debre Tabor Comprehensive Hospital from January 1, 2022, to May 30, 2022. SPSS version 25 was used to analyze the data. The factors connected to post-concussion syndrome were found using bivariate and multivariable logistic regression analysis. Statistical significance was determined by a P-value of ≤ 0.05.
Results: During the data collection period, 405 cases in total were interviewed, with a 98% response rate. More than half (60.7%) of patients were married, with the majority of patients (39.8%) falling between the ages of 18 and 29. At least three post-concussion syndrome symptoms were present in 42.8% of subjects. A history of comorbidities, GCS levels of 8 or below, 9 to 12 at the time of presentation, brain neuroimaging findings, and having fair or poor social support were found to be substantially linked with PCS in multivariate logistic regression.
Conclusion: About 41.5% of study participants had at least three symptoms of PCS. The Glasgow coma scale level at the time of presentation, the reason for the injury, social support, and the site of the injury were all significantly associated with the occurrence of PCS.
Introduction
The World Health Organization (WHO) defines post-concussion syndrome (PCS) as the occurrence of three or more of the signs and symptoms listed below following a head injury such as headache, dizziness, exhaustion, irritability, sleeplessness, difficulties concentrating, or memory problems (1). The symptoms of post-concussion syndrome (PCS) may persist for weeks, months, or even a year or more following a concussion (2, 3). Approximately 34–35% of concussion victims have ongoing or long-standing symptoms 3–6 months after the incident (4). Having concussion symptoms for more than four weeks after the initial injury in children, and for weeks or months in adults is referred to as a prolonged concussion (5).
A conclusive test does not exist for post-concussion syndrome. The primary factors in the diagnosis include a history of head trauma and reported symptoms. To assess symptoms, a physical examination and potentially a head CT or MRI scan may be performed. To rule out further causes of symptoms, such as infection, bleeding into the brain, or poisoning, additional tests may be performed (6–8). Despite the lack of a specific treatment for PCS, medications, physical, and behavioral therapy can help resolve symptoms. It is crucial to provide information regarding symptoms and recovery expectations (9).
According to estimates, 40–80% of the 2 million Americans who experience a minor head injury (MHI) each year go on to develop post-concussive syndrome (PCS), which can cause them to miss work or school and impair their social behavior (10).
One of the most frequent consequences of TBI is post-concussion syndrome (PCS), which consists of somatic, cognitive, and emotional symptoms (6). Studies on PCS have revealed significant variations in the syndrome's prevalence, ranging from <5% (11) to 58% (12), while 10–15% of concussions are most frequently observed. The disagreement over the definition of PCS is a key factor in this wide range. However, there is a significant chance that PCS will be misdiagnosed because the majority of its symptoms are either common or could be made worse by other illnesses. For instance, headaches following a concussion could resemble migraines or tension headaches (13).
Age, gender, expectations of disability, and somatic illnesses or mental illnesses are a few risk factors that have been linked to PCS. The development of PCS is thought to be influenced by physiological and psychological occurrences before, during, and after the injury. A long-running controversy surrounds PCS's cause, which is still being discussed today. Some experts claim that post-concussion symptoms are brought on by structural damage to the brain or disruption of neurotransmitter systems. However, radiological evidence of brain damage was absent in 38% of people who experienced concussion-like symptoms following a head injury (14, 15).
The prevalence of a group of physical, mental, emotional, and behavioral symptoms that can be identified in victims of traumatic brain injury ranges from 11 to 64% (16). It is not known how common persistent symptoms are after a year, although it is assumed to be 5%. Although PCS is prevalent, there are issues regarding its accuracy since children typically exhibit behavioral abnormalities after any accident and because circumstances that existed prior to the damage, as well as medical and legal concerns after the injury, may have an impact on recovery (17). Up to 60% of individuals with mild traumatic brain injury (MTBI) may experience the post-concussion syndrome (PCS), which is characterized by the persistence of symptoms such as headaches, fatigue, memory loss, and emotional instability (18).
Numerous international studies have shown that brain injuries are a common health problem that mostly affects the world's productive age groups and greatly increases medical costs. Most commonly impacting the population's productive age group and contributing significantly to morbidity and death in Africa, head injuries have negative economic effects on both individuals and the continent's community (19).
Although the limited study on post-concussion syndrome in Ethiopia, it is a common health problem that affects the productive age group and either directly or indirectly affects the development of the country (15). Because the issue affects the country's most productive age group, it is crucial to focus on doing this study on the prevalence and associated factors of post-concussion syndrome.
Methods
Study design, study area and study period
A hospital-based based cross-sectional study was conducted in Emergency department of Debre Tabor Comprehensive (DTCH), from January 1, 2022 to May 30, 2022, which is found in Debre Tabor city and found 665 km from Addis Ababa (the capital city of Ethiopia). The hospital is the largest in the South Gondar zone, which was established in 1953 and serves more than 2.5 million population in its catchment area. With 160 inpatient beds across five major departments, the hospital has more than 40 specialists in a variety of medical specialties along with 250 additional health workers.
Source and study population
The source population consisted of all patients who presented to the adult emergency department of DTCH with head injury and the study population was made up of all patients who had traumatic brain injuries and had visited the adult emergency department of DTCH throughout the study period.
Inclusion and exclusion criteria
Patients who were seriously ill or unconscious during the data collection period were excluded from the study, while patients with traumatic brain injuries who were 18 years of age or older were all included.
Sample size determination and sampling techniques
The required sample size was determined using the single population proportion formula by taking the prevalence of PCS (41.5%) among head injury patients from a study done at the emergency department of Hawassa University Comprehensive and Specialized Hospital (15), with a 95% level of confidence and 5% margin of error.
Adding a 10% non-response rate. The final sample size was 405. A consecutive sampling technique was used to select the respondents for their participation.
Data collection tool and procedures
Data on the prevalence of PCS were gathered using a standard questionnaire. The most widely used tool is the Rivermead Post-Concussion Symptoms Questionnaire (RPQ), which has been shown to have validity and reliability (20, 21). With consideration for the high baseline incidence of symptoms, this questionnaire asks patients to rank the severity of each of 16 symptoms in comparison to before the mild traumatic brain injury (MTBI). Face-to-face interviews at appointed follow-ups during the first 12 months after injury were undertaken. The interview covered details on sociodemographic factors, clinical traits, and behavioral facets. Two medical intern students who were working in the emergency room were participated in collected the data. For ensuring the validity of the data, the interviewees were questioned in Amharic, their native tongue.
Data quality control measures
Trained medical interns gathered the data. The questionnaire was pre-tested on 5% of the study participants before the actual data-collecting period to make sure it was clear, comprehensible, and complete. The results of the final analysis did not include the pre-test data.
Data processing and analysis
Before being subjected to SPSS version 25 analysis, the data was double-checked for accuracy, coded, and entered into Epi-info version 7.2. Using descriptive statistical analysis, the estimated frequencies and percentages of the variables were computed. To investigate the link between the outcome and the explanatory variables, analyses of multivariate and bivariate logistic regression were performed. A P-value of 0.05 or less was regarded as statistically significant, and an odds ratio with a 95% confidence interval was used to assess the strength of associations.
Results
Socio-demographic characteristics
Out of 405 selected traumatic brain injury patients, 397 patients have participated in this study with a response rate of 98%. Two hundred eighty-three (71.3%) were male patients. The patients' mean (standard deviation) age was 34.4 (16.7) years. About 241 (60.7%) of the patients were married, and only 47 (11.8%) were unable to read and write. Most of the patients (318, 80.1%) were orthodox religious followers, and more than two-thirds (298, 75.1%) were from rural residences (Table 1).
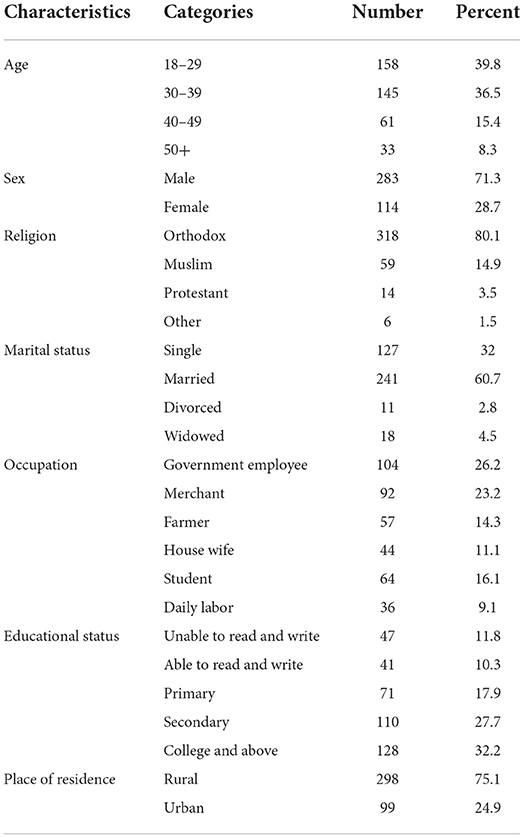
Table 1. Socio-demographic characteristics of study participants attending emergency outpatient department of DTCH, Debre Tabor, Ethiopia (n = 405).
Clinical characteristics
Concerning the duration of illness, 67.5% of study participants were sick for 1 week, and 31.0% were injured in the right lateral part of their brain. Regarding social support, 28.0% of respondents have very good social support. In terms of injury causes, 39.3% of study participants were injured in a car accident (Table 2).
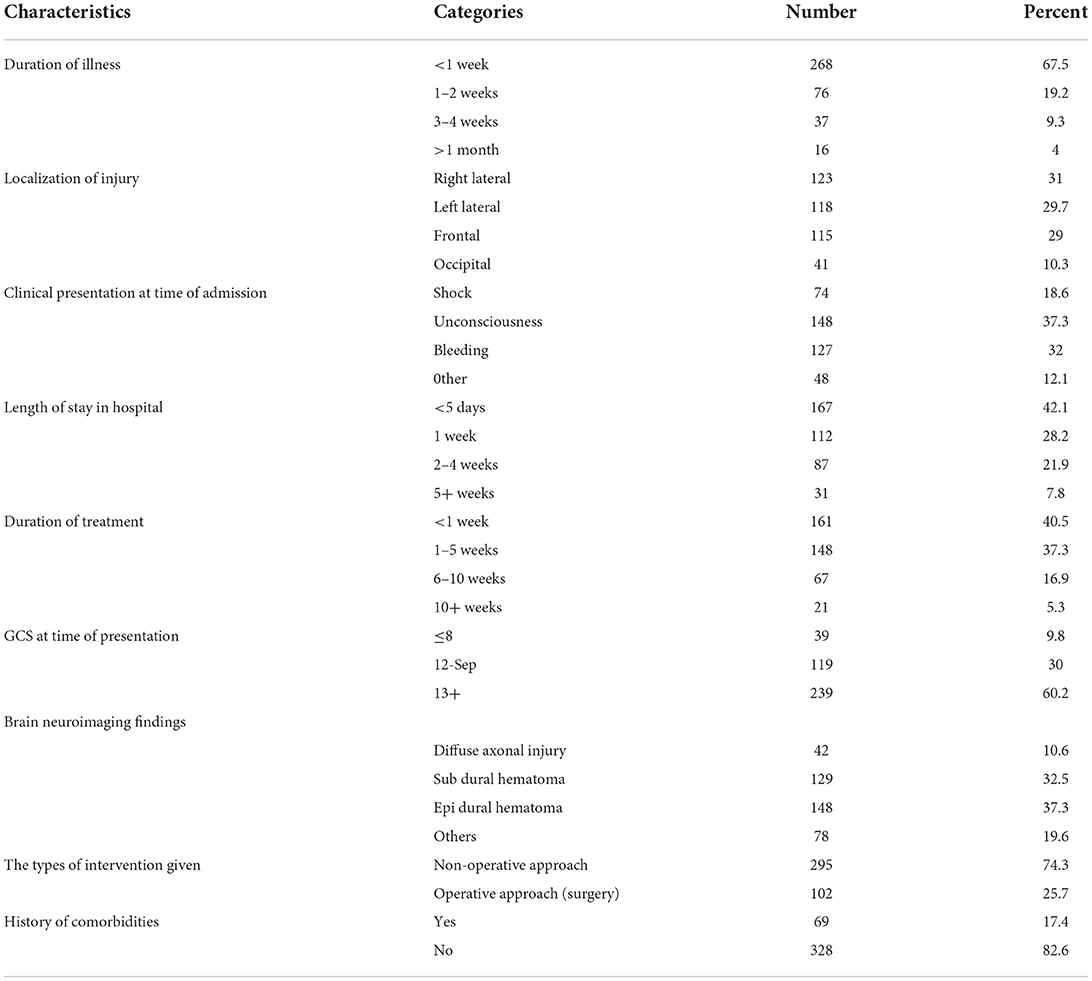
Table 2. Characteristics of injures of study participants attending emergency outpatient department of DTCH, Debre Tabor, Ethiopia (n = 405).
Prevalence and factors associated with PCS
In this study, the overall prevalence of post-concussion syndrome was 42.8%. Moderate traumatic brain injury accounts 47.6% of post-concussion syndrome (Figure 1). In the bivariate analysis, having a history of comorbidities, GCS values of eight or less, 9–12 at time of presentation, trauma features and having fair and poor social support were identified to be significantly associated with PCS. Likewise, during multivariate logistic regression, the above variables are significantly associated with PCS. Head injury patients with fair or poor [AOR = 2.51; 95% CI (1.37–3.83)] social support were 2.5 times more likely to have PCS than those with strong social support. Head injury patients who have a history of comorbidities [AOR = 1.79; 95% CI (1.04–2.76)] were 1.8 times more likely to have PCS than those who do not. At the time of presentation, patients with a GCS of 8 or less (AOR = 3.75; 95% CI (2.09–8.41) or 9-12 (AOR = 3.42; 95% CI (2.24–5.77) were 3.75 and 3.42 times more likely to develop PCS than patients with a GCS of 13+. Traumatic brain injury patients who had brain neuroimaging findings of Diffuse axonal injury, subdural hematoma and epidural hematoma [AOR = 15.34; 95% CI (5.76–39.73)], [AOR = 5.25; 95% CI (2.16–10.64)], [AOR = 8.53; 95% CI (3.92–21.32)] were 15.34, 5.25 and 8.53 times more likely to have PCS than those who have other findings, respectively (Table 3).
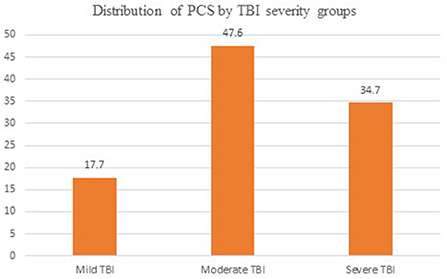
Figure 1. Distributions of PCS by TBI severity groups by percentage. PCS, post-concussion syndrome; TBI, traumatic brain injury.
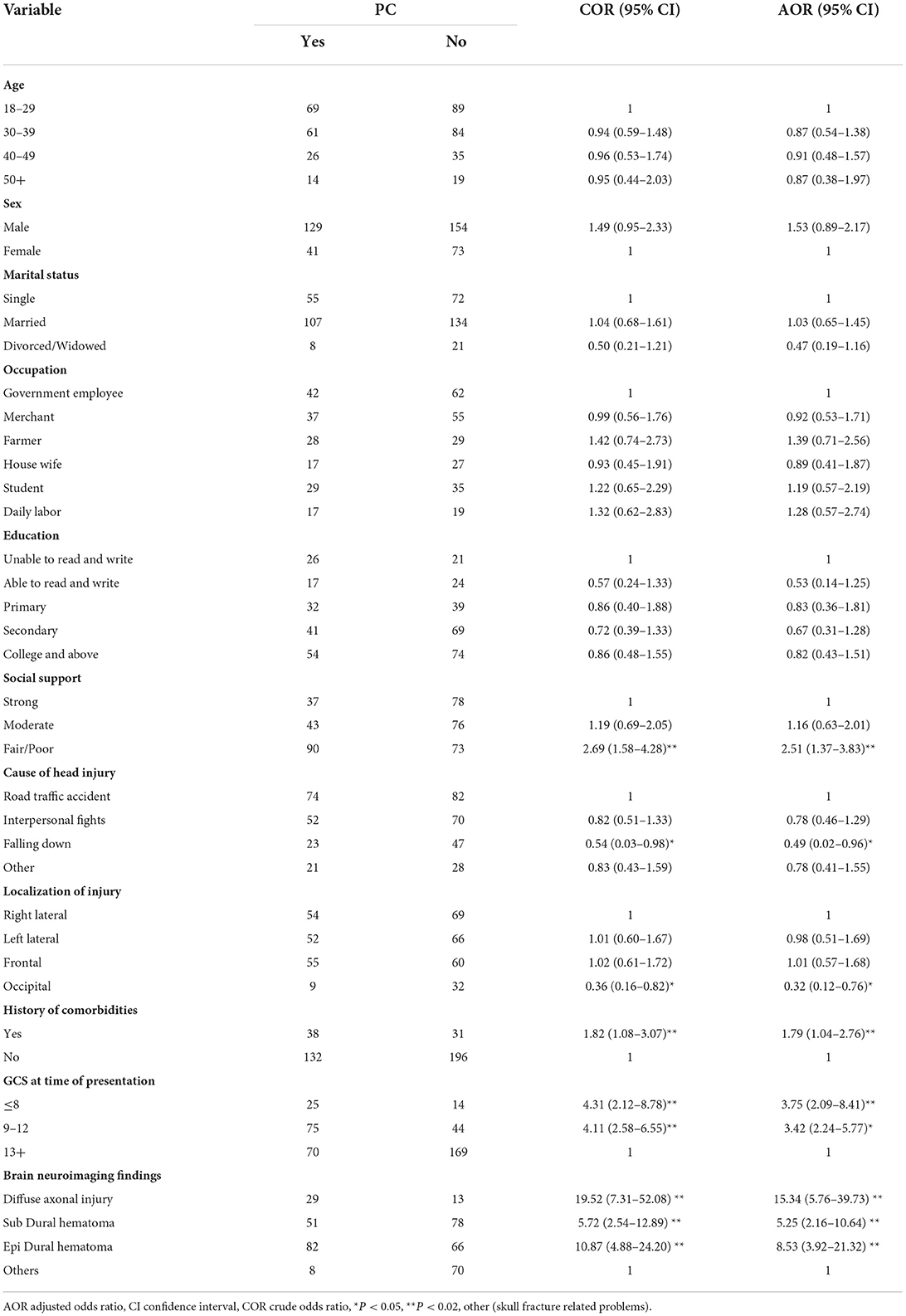
Table 3. Factors associated PCS (bivariate and multivariate logistic regression) of study participants attending emergency outpatient department of Debre Tabor Compressive Hospital, Debre Tabor, Ethiopia (n = 397).
Discussion
The dorsal raphe nucleus is one of the crucial circuitry systems in the brain that is probably harmed by concussion. Within the brainstem, the serotenergic fiber tracts are under the direction of the dorsal raphe nucleus. Due to their far-reaching projections, the fiber tracts are vulnerable to damage and shearing during the impact of a concussion (22, 23).
In this study, post-concussion syndrome was prevalent in 42.8, or 95% CI (36.7–45.4%) among head injury patients who visited the DTCH emergency room. While the results of this study were more significant, a study conducted a CENTER-TBI (the Collaborative European Neurotrauma Effectiveness Research) found that PCS symptoms were present in 58% of the subjects (24). Additionally, it was much greater than studies done in Malaysia, which discovered 34% of patients who survived mild TBI acquired PCS (25). The fact that the present study's study location, sample size, and socioeconomic makeup differ from the one previously stated could be the cause of the discrepancy. On the other hand, this outcome was equivalent to the 41.5% (15) at the comprehensive specialized hospital of Hawassa University in Ethiopia.
According to this study, the majority of injuries were caused by interpersonal conflicts (122, 30.7%) and road traffic accidents (156, 39.3%). Interpersonal conflicts accounted for 38.5% of head injury cases at Jimma University Hospital in Southwest Ethiopia, while road traffic accidents accounted for 36.5% of those cases (26) and a study from Gondar University Referral Hospital in Northwest Ethiopia also revealed findings that were similar to these (27). Contradicting this report, a study conducted in Australia found that the majority of injuries resulted from sporting and recreational activities (28). This variation may be due to the difference in socio-cultural and behavioral characteristics of the study participants.
In comparison to patients who sustained right lateral injuries, those with occipital brain injuries had a 32% decreased likelihood of developing PCS. A study conducted at the Hawassa University Comprehensive Specialized Hospital in southern Ethiopia also lends credence to this result (15). additionally, a follow-up study conducted in the United States discovered that participants with frontotemporal and parietal head injuries had more severe effects and atrophied more rapidly than those with lesions to other regions of the brain (29).
The current study found that social support was a significant factor in the development of post-concussion syndrome, which is consistent with the scientific justification of the neuropsychiatrist's theory that patients with fair or poor social support were more likely to develop PCS than patients with strong social support. Those with fair or poor social support had 2.47 and 2.62 times the likelihood of developing PCS compared to patients with excellent social support after a head injury. Other research carried out at the Hawassa University Comprehensive Specialized Hospital in southern Ethiopia does not agree with this report. As was shown, 41.1% (15) of study participants who experienced PCS had just fair to poor social support.
Patients with head injuries and GCS values of eight or less and 9–12 at the time of presentation were 3.75 (AOR = 3.75, 95% CI, 2.09–8.41) and 3.42 (AOR = 3.42, 2.24–5.77) times more likely to develop PCS, respectively, than patients with head injuries and GCS values of 13 or higher. This conclusion is reinforced by the fact that the GCS is still an important tool for neurological evaluation following a head injury and that, in the majority of studies, the classification of the trauma's severity is still dependent on the admission GCS (15, 30). A score of eight or less is required to distinguish between a serious head injury and a moderate to mild head injury; in this study, the development of PCS increases with the severity of the head injury, in line with findings in a one-year prospective study done from April 21, 2006-April 20, 2007 in Nigeria's new neurosurgical centers (31).
Conclusion
About 42.8% of those who took part in the study showed at least three PCS symptoms. The Glasgow coma scale level at the time of presentation, the reason for the injury, social support, and the site of the injury were all significantly associated with the occurrence of PCS.
Recommendation
Future research ought to take into account the imaging findings of people who have suffered head injuries as supporting evidence in addition to evaluating the symptoms listed in the PCS tool.
Limitation
The cross-sectional nature of the study precludes the inference of causality.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Review Committee of the College of Health Science at Debre Tabor University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
MM, MS, AA, TA, and EA participated in the conception, design of the study, reviewing the proposal, data analysis, and report writing. NB, GA, YM, GY, TY, and KS were participated in data analysis and report writing. AT performed data analysis and prepared the manuscript for publication. All authors read and approved the final manuscript.
Acknowledgments
We are grateful to extend our gratitude to study participants and staff from Debre Tabor Comprehensive Hospital for devoting their time to contributing their ideas during data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, Adjusted odds ratio; CI, Confidence Interval; DTCH, Debre Tabor Comprehensive Hospital; GCS, Glasgow Coma Scale; MTBI, minor traumatic brain injury; MHI, minor head injury; PCS, Post -concussion syndrome; RPQ, Rivermead Post-Concussion Symptoms Questionnaire; SD, Standard deviation; SPSS, Stastical Package for Social Science; WHO, World Health Organization.
References
1. Santé O, World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization (1992).
2. Rao V, Lyketsos C. Neuropsychiatric sequelae of traumatic brain injury. Psychosomatics. (2000) 41:95–103. doi: 10.1176/appi.psy.41.2.95
3. Mittenberg W, Strauman S. Diagnosis of mild head injury and the post-concussion syndrome. J Head Trauma Rehabil. (2000) 15:783–91. doi: 10.1097/00001199-200004000-00003
4. Voormolen DC, Haagsma JA, Polinder S, Maas AI, Steyerberg EW, Vuleković P, et al. Post-concussion symptoms in complicated vs. uncomplicated mild traumatic brain injury patients at three and six months post-injury: results from the CENTER-TBI study. J Clin Med. (2019) 8:1921. doi: 10.3390/jcm8111921
5. Margulies S. The post-concussion syndrome after mild head trauma: is brain damage overdiagnosed? Part 1 J Clin Neurosci. (2000) 7:400–8. doi: 10.1054/jocn.1999.0681
6. Sigurdardottir S, Andelic N, Roe C, Jerstad T, Schanke A-K. Post-concussion symptoms after traumatic brain injury at 3 and 12 months post-injury: a prospective study. Brain Injury. (2009) 23:489–97. doi: 10.1080/02699050902926309
7. Babcock L, Byczkowski T, Wade SL, Ho M, Mookerjee S, Bazarian JJ. Predicting post-concussion syndrome after mild traumatic brain injury in children and adolescents who present to the emergency department. JAMA Pediatr. (2013) 167:156–61. doi: 10.1001/jamapediatrics.2013.434
8. Broshek DK, De Marco AP, Freeman JR. A review of post-concussion syndrome and psychological factors associated with concussion. Brain Injury. (2015) 29:228–37. doi: 10.3109/02699052.2014.974674
9. Leddy JJ, Sandhu H, Sodhi V, Baker JG, Willer B. Rehabilitation of concussion and post-concussion syndrome. Sports Health. (2012) 4:147–54. doi: 10.1177/1941738111433673
10. King NS, Kirwilliam S. Permanent post-concussion symptoms after mild head injury. Brain Injury. (2011) 25:462–70. doi: 10.3109/02699052.2011.558042
11. Iverson GL. Outcome from mild traumatic brain injury. Curr Opin Psychiatry. (2005) 18:301–17. doi: 10.1097/01.yco.0000165601.29047.ae
12. Bazarian JJ, Wong T, Harris M, Leahey N, Mookerjee S, Dombovy M. Epidemiology and predictors of post-concussive syndrome after minor head injury in an emergency population. Brain Injury. (1999) 13:173–89. doi: 10.1080/026990599121692
13. Bigler ED. Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. J Int Neuropsychol Soc. (2008) 14:1–22. doi: 10.1017/S135561770808017X
14. Machamer J, Temkin N, Dikmen S, Nelson LD, Barber J, Hwang P, et al. Symptom frequency and persistence in the first year after traumatic brain injury: a TRACK-TBI study. J Neurotrauma. (2022) 39:358–70. doi: 10.1089/neu.2021.0348
15. Bedaso A, Geja E, Ayalew M, Oltaye Z, Duko B. Post-concussion syndrome among patients experiencing head injury attending emergency department of Hawassa University Comprehensive specialized hospital, Hawassa, southern Ethiopia. J Headache Pain. (2018) 19:1–6. doi: 10.1186/s10194-018-0945-0
16. Bryant RA. Disentangling mild traumatic brain injury and stress reactions. New England J Med. (2008) 358:525. doi: 10.1056/NEJMe078235
17. Lee LK. Controversies in the sequelae of pediatric mild traumatic brain injury. Pediatr Emerg Care. (2007) 23:580–3. doi: 10.1097/PEC.0b013e31813444ea
18. Jasper U, Opara M, Pyiki E, Akinrolie O. The epidemiology of hospital-referred head injury in Northern Nigeria. J Sci Res Rep. (2014) 3:2055–64. doi: 10.9734/JSRR/2014/9645
19. Bergersen K, Halvorsen JØ, Tryti EA, Taylor SI, Olsen A, A. systematic literature review of psychotherapeutic treatment of prolonged symptoms after mild traumatic brain injury. Brain Injury. (2017) 31:279–89. doi: 10.1080/02699052.2016.1255779
20. Crawford S, Wenden F, Wade D. The Rivermead head injury follow up questionnaire: a study of a new rating scale and other measures to evaluate outcome after head injury. J Neurol Neurosurg Psychiatry. (1996) 60:510–4. doi: 10.1136/jnnp.60.5.510
21. King N, Crawford S, Wenden F, Moss N, Wade D. The Rivermead post-concussion symptoms questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. J Neurol. (1995) 242:587–92. doi: 10.1007/BF00868811
22. Dioso E, Cerillo J, Azab M, Foster D, Smith I, Leary O, et al. Subconcussion, concussion, and cognitive decline: the impact of sports related collisions. J Med Res Surgery. (2022) 3:54. doi: 10.52916/jmrs224081
23. Byrd M, Dixon C, Lucke-Wold B. Examining the correlation between acute behavioral manifestations of concussion and the underlying pathophysiology of chronic traumatic encephalopathy: a pilot study. J Neurol Psychol. (2018) 6:1–4. doi: 10.13188/2332-3469.1000037
24. Zeldovich M, Wu Y-J, Gorbunova A, Mikolic A, Polinder S, Plass AM, et al. Influence of sociodemographic, premorbid, and injury-related factors on post-concussion symptoms after traumatic brain injury. J Clin Med. (2020) 9:1931. doi: 10.3390/jcm9061931
25. Lannsjö M., Geijerstam J-La, Johansson U, Bring J, Borg J. Prevalence and structure of symptoms at 3 months after mild traumatic brain injury in a national cohort. Brain Injury. (2009) 23:213–9. doi: 10.1080/02699050902748356
26. Aenderl I, Gashaw T, Siebeck M, Mutschler W. Head injury-a neglected public health problem: a four-month prospective study at Jimma University specialized hospital, Ethiopia. Ethiop J Health Sci. (2014) 24:27–34. doi: 10.4314/ejhs.v24i1.4
27. Ayele TA, Zeleke BM, Tessema GA, Melak MF. Magnitude and patterns of injuries among patients in Gondar University Hospital, northwest Ethiopia: an institutional-based study. Open Access Surgery. (2017) 10:25–31. doi: 10.2147/OAS.S126043
28. Amaranath JE, Ramanan M, Reagh J, Saekang E, Prasad N, Chaseling R, et al. Epidemiology of traumatic head injury from a major paediatric trauma centre in New South Wales, Australia. ANZ J Surg. (2014) 84:424–8. doi: 10.1111/ans.12445
29. Saulle M, Greenwald BD. Chronic traumatic encephalopathy: a review. Rehabilitat Res Practice. (2012) 2022:1–9. doi: 10.1155/2012/816069
30. Forbes AE, Schutzer-Weissmann J, Menassa DA, Wilson MH. Head injury patterns in helmeted and non-helmeted cyclists admitted to a London Major Trauma Centre with serious head injury. PLoS ONE. (2017) 12:e0185367. doi: 10.1371/journal.pone.0185367
Keywords: post-concussion syndrome, head injury, associated factors, Debre Tabor, traumatic brain injury
Citation: Teshome AA, Ayehu GW, Yitbark GY, Abebe EC, Mengstie MA, Seid MA, Molla YM, Baye ND, Amare TJ, Abate AW, Yazie TS and Setargew KH (2022) Prevalence of post-concussion syndrome and associated factors among patients with traumatic brain injury at Debre Tabor Comprehensive Hospital, North Central Ethiopia. Front. Neurol. 13:1056298. doi: 10.3389/fneur.2022.1056298
Received: 30 September 2022; Accepted: 07 November 2022;
Published: 21 November 2022.
Edited by:
David M. Niddam, National Yang Ming Chiao Tung Unviersity, TaiwanReviewed by:
Nada Andelic, University of Oslo, NorwayBrandon Peter Lucke-Wold, University of Florida, United States
Copyright © 2022 Teshome, Ayehu, Yitbark, Abebe, Mengstie, Seid, Molla, Baye, Amare, Abate, Yazie and Setargew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Assefa Agegnehu Teshome, YXNzZWZhYWdlZ25laHU3QGdtYWlsLmNvbQ==
 Assefa Agegnehu Teshome
Assefa Agegnehu Teshome Gashaw Walle Ayehu
Gashaw Walle Ayehu Getachew Yideg Yitbark
Getachew Yideg Yitbark Endeshaw Chekol Abebe
Endeshaw Chekol Abebe Misganaw Asmamaw Mengstie
Misganaw Asmamaw Mengstie Mohammed Abdu Seid
Mohammed Abdu Seid Yalew Melkamu Molla2
Yalew Melkamu Molla2 Nega Dagnaw Baye
Nega Dagnaw Baye Agmas Wassie Abate
Agmas Wassie Abate Taklo Semineh Yazie
Taklo Semineh Yazie