
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 22 December 2022
Sec. Neurological Biomarkers
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.1036433
This article is part of the Research Topic Potential Biomarkers in Neurovascular Disorders, volume II View all 19 articles
 Long Zhao1,2,3†
Long Zhao1,2,3† Yi Zhang2†
Yi Zhang2† Ping Lin2
Ping Lin2 Weida Li2
Weida Li2 Xingyuan Huang4
Xingyuan Huang4 Hangyang Li2
Hangyang Li2 Mingkai Xia5
Mingkai Xia5 Xinlong Chen2
Xinlong Chen2 Xi Zhu6*
Xi Zhu6* Xiaoping Tang1,3*
Xiaoping Tang1,3*Objective: Red blood cell (RBC) parameters are associated with outcomes following aneurysmal subarachnoid hemorrhage (aSAH), but their predictive value remains uncertain. This study aimed to detect the association between RBC parameters and functional outcome in aSAH patients undergoing surgical clipping.
Methods: This retrospective observational study included aSAH patients who underwent surgical clipping at Affiliated Hospital of North Sichuan Medical College between August 2016 and September 2019. The functional outcome following aSAH was assessed by modified Rankin Scale (mRS), and mRS 3–6 was defined as poor functional outcome.
Results: Out of 187 aSAH patients included (62% female, 51–66 years old), 73 patients had poor functional outcome. Multivariate logistic regression of admission parameters showed that World Federation of Neurosurgical Societies (WFNS) grade (odds ratio [95% CI]: 1.322 [1.023–1.707], p = 0.033) and white blood cell (WBC) (odds ratio [95% CI]: 1.136 [1.044–1.236], p = 0.003) were independently associated with poor functional outcome. In postoperative parameters, RBC distribution width (RDW) (odds ratio [95% CI]: 1.411 [1.095–1.818], p = 0.008), mean platelet volume (MPV, odds ratio [95% CI]: 1.253 [1.012–1.552], p = 0.039) and admission WFNS grade (odds ratio [95% CI]: 1.439 [1.119–1.850], p = 0.005) were independently associated with poor functional outcome. The predictive model including WFNS grade, admission WBC, and postoperative RDW and MPV had significantly higher predictive power compared to WFNS grade alone (0.787 [0.722–0.852] vs. 0.707 [0.630–0.784], p = 0.024). The combination of WFNS grade and WBC on admission showed the highest positive predictive value (75.5%) and postoperative RDW and MPV combined with admission WFNS grade and WBC showed the highest negative predictive value (83.7%).
Conclusion: Postoperative RDW is independently associated with poor functional outcome in aSAH patients undergoing surgical clipping. A combined model containing postoperative RDW may help predict good outcome in patients with aSAH after timely aneurysm clipping.
Aneurysmal subarachnoid hemorrhage (aSAH), a severe type of hemorrhagic stroke, results from the rupture of intracranial aneurysms (1). With significant morbidity and mortality, such disease continues to be a clinical emergency despite advances in strategies of diagnosis, treatment, and neurocritical care (2). When a rupture occurs, guidelines recommend the repair be conducted as soon as possible (3, 4). Though endovascular coiling is widely performed, some forms of aSAH are suitable for surgical clipping. This requires complicated perioperative management and leads to clinical problems, such as the relationship between anemia, intraoperative blood loss and outcomes, which are still under investigation. Therefore, biomarkers predicting outcomes after surgical clipping are needed for advanced clinical care.
Red blood cell (RBC) parameters have been reported to predict poor outcomes after an aSAH event. Postoperative hemoglobin, an anemia biomarker, is observed to be an independent risk factor of poor neurological outcomes (5). Gong et al. found that mean corpuscular volume (MCV) and mean corpuscular hemoglobin (MCH) are predictors of cognitive impairment (6). Recent studies also have shown that RBC distribution width (RDW) is associated with outcome indicators such as functional outcome, mortality, delayed cerebral ischemia (DCI) and cerebral infarction following aSAH (7–9). Since the role of blood transfusion in the management of aSAH is still controversial and there is a lack of practical indicators for reference in the management of blood volume clinically, it is of great significance to continue evaluating the role of RBC parameters in aSAH.
Although several studies discussed the predictive value of RBC parameters, few considered the craniotomy performed in relation to the analysis, which may affect RBC parameters and outcome. Moreover, these studies have not been externally validated. It is unclear whether these results are broadly applicable and whether postoperative RBC parameters are associated with outcomes of aSAH patients after clipping. Therefore, this retrospective case-control study was conducted to comprehensively analyze the relationship between RBC parameters on admission and after surgical clipping and functional outcome of aSAH patients, and to screen parameters with independent predictive value.
This retrospective observational study included consecutive patients with aSAH admitted to Affiliated Hospital of North Sichuan Medical College between August 2016 and September 2019. The inclusion criteria were: (1) age >18 years; (2) patients with aSAH confirmed by computed tomographic angiography or digital subtraction angiography; (3) admitted within 24 h of initial symptom onset; (4) undergoing surgical clipping within 72 h of the onset; (5) complete blood count (CBC) test was completed within 24 h after admission and within 6 h after surgery. The exclusion criteria were: (1) patients with a history of primary or secondary central nervous system diseases, acute or chronic infections, or systemic diseases; (2) patients with trauma, surgery, bleeding events or blood donation within 3 months; (3) patients with incomplete information. This study was performed according to the TRIPOD statement (10), followed the revised Declaration of Helsinki and was approved by the ethics committee of Affiliated Hospital of North Sichuan Medical College. Patients' consent was waived due to the retrospective nature of this study.
Data were collected from the electronic medical records, including demographics (age, gender), addictions (smoking and alcohol consumption), medical history (hypertension, diabetes mellitus), admission clinical grades, aneurysm characteristics, and admission and postoperative CBC parameters. Clinical grades included the World Federation of Neurosurgical Society (WFNS) grade and modified Fisher (mFisher) grade. Aneurysm characteristics included location and number. Location was divided into “anterior” and “posterior” circulation, and number was divided into “single” and “multiple”. RBC parameters including hemoglobin, RBC, hematocrit, MCV, MCH, mean corpuscular hemoglobin concentration (MCHC), and RDW were collected on admission and postoperatively. Other CBC parameters reported as outcome predictors were also collected, including white blood cell (WBC), neutrophil, lymphocyte, monocyte, platelet and mean platelet volume (MPV) (11–13). Differences between admission and postoperative RBC parameters were calculated by subtracting the admission values from the postoperative values. For data accuracy and comparability, only the first CBC results after admission and surgery were collected separately.
Functional outcome was assessed through telephone interview or outpatient visit at 3 months by fixed staff who was blind to laboratory data of patients, following the modified Rankin scale (mRS) (14). The mRS is scored 0–6: 0 (no symptoms), 1 or 2 (functional independence), 3 (moderate handicap), 4 or 5 (moderate to severe handicap) and 6 (death). We defined good functional outcome as 3-month mRS between 0 and 2 and poor outcome as mRS between 3 and 6 (15). Patients were dichotomized into two groups (mRS 0–2 vs. mRS 3–6).
Statistical analysis was performed with SPSS Statistics 26 (IBM, Armonk, NY, USA), and p < 0.05 was considered significant. Categorical variables were presented as number (percentage) and compared by Chi-square or Fisher's exact test. Continuous variables that conformed to normal distribution were expressed as mean ± standard deviation and compared by Student's t-test. Continuous variables that conformed to skewed distribution were expressed as median with interquartile range (25th−75th percentile) and compared by the Mann-Whitney U test, which was also applied to rank variables. Multivariate logistic regression was performed to identify the independent predictors of poor functional outcome. Variables considered clinically relevant or with p < 0.05 in univariate analyses were incorporated into multivariate logistic regression models. Receiver operating characteristic (ROC) analysis was conducted to evaluate the predictive value and to determine the cutoff value by calculating Youden's index. Delong's test compared areas under ROC curves (AUCs).
A total of 187 patients were included in this study, of which 114 (61.0%) had good functional outcome while 73 (39.0%) had poor functional outcome, including 15 patients (8.0%) who died within 3 months of the onset (Figure 1). Of the included cases, 122 were included in a published article to establish an early predictive nomogram for DCI after aSAH (13). Parameters of demographics, addictions, medical history and aneurysm characteristics showed no significant differences between two groups. In contrast, parameters of admission clinical grades differed significantly between two groups (WFNS grade, p < 0.001; mFisher grade, p = 0.011; Table 1).
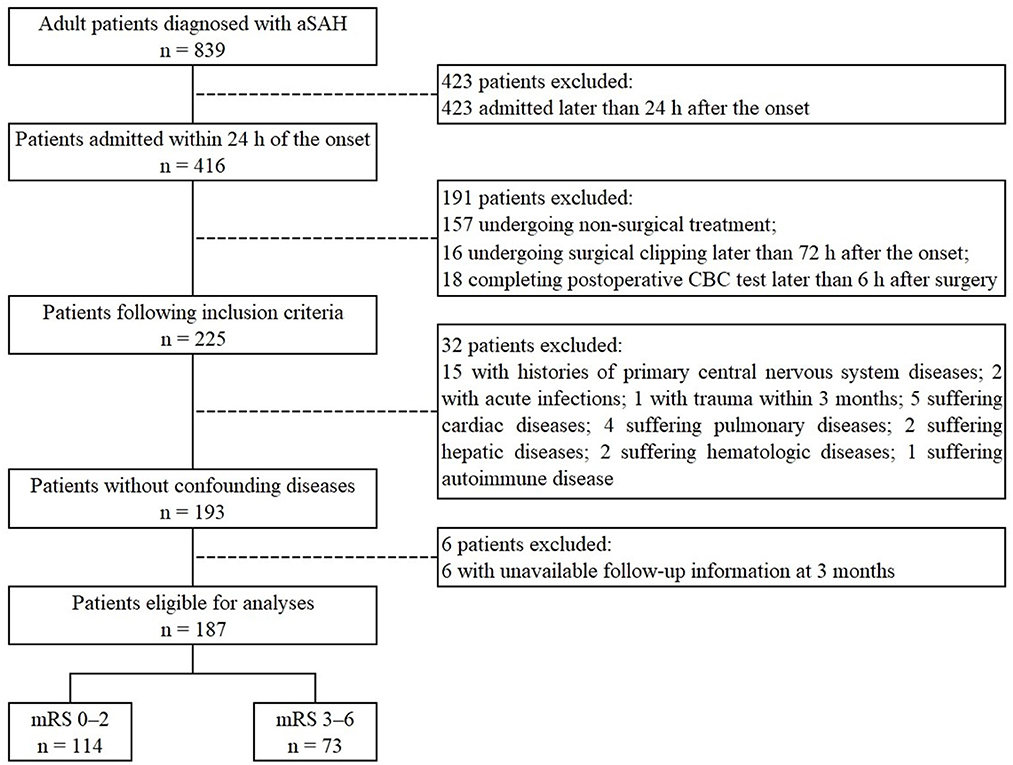
Figure 1. Flowchart of patients included in the study. aSAH, aneurysmal subarachnoid hemorrhage; CBC, complete blood count; mRS, modified Rankin Scale.
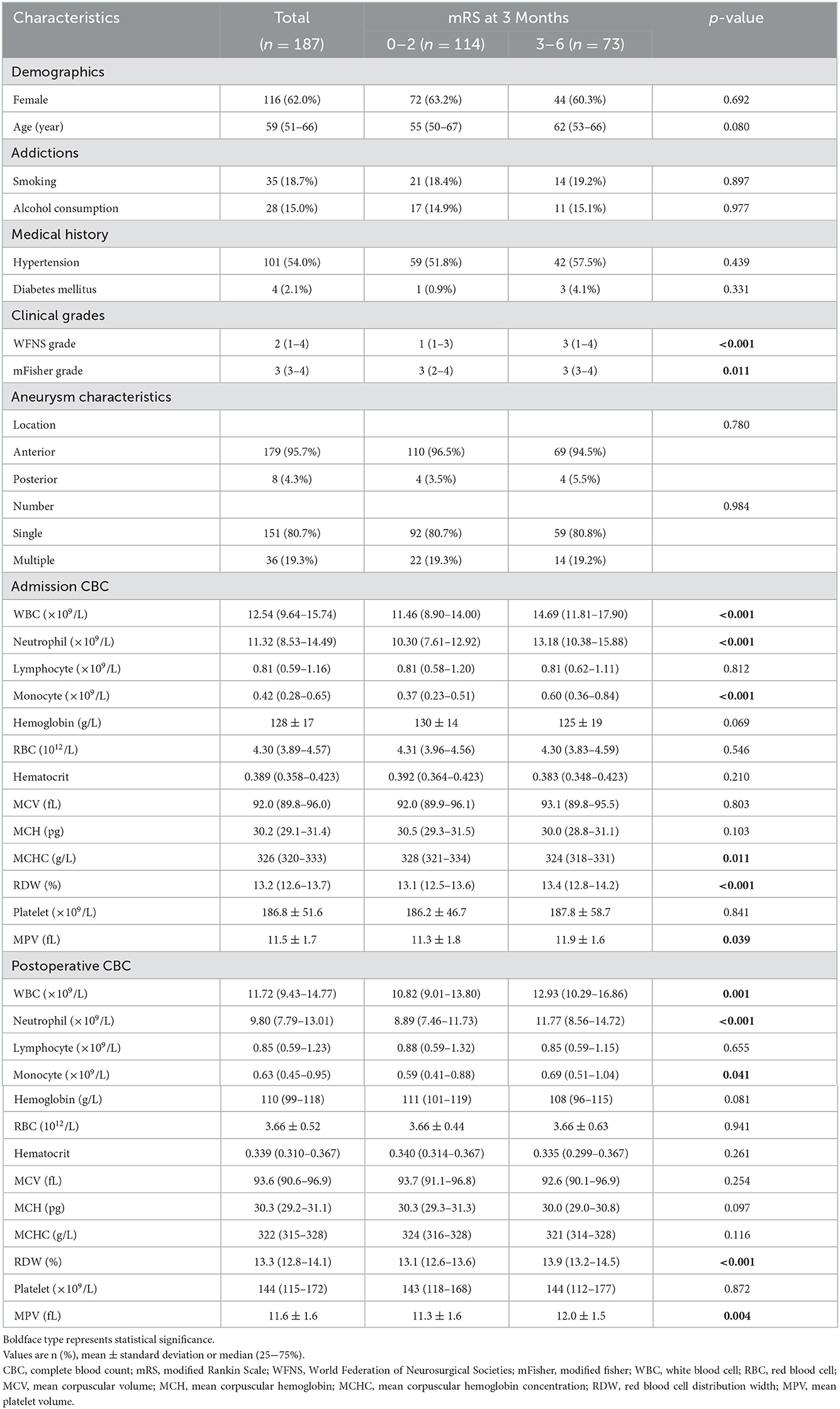
Table 1. Univariate analysis of baseline characteristics and CBC parameters associated with poor functional outcome at 3 months.
Admission CBC parameters showed that WBC (11.46 [8.90–14.00] vs. 14.69 [11.81–17.90], p < 0.001), neutrophil (10.30 [7.61–12.92] vs. 13.18 [10.38–15.88], p < 0.001), monocyte (0.37 [0.23–0.51] vs. 0.60 [0.36–0.84], p < 0.001) and RDW (13.1 [12.5–13.6] vs. 13.4 [12.8–14.2], p < 0.001) in patients with poor functional outcome were significantly higher than those in patients with good functional outcome (Table 1). Patients with poor functional outcome also had significantly lower MCHC (328 [321–334] vs. 324 [318–331], p = 0.011; Table 1). Multivariate logistic regression showed that WFNS grade (odds ratio [95% CI]: 1.322 [1.023–1.707], p = 0.033) and WBC (odds ratio [95% CI]: 1.136 [1.044–1.236], p = 0.003) predicted poor functional outcome independently (Table 2).
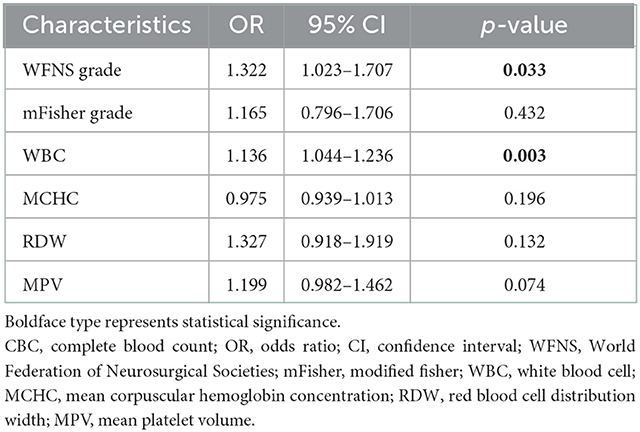
Table 2. Multivariate logistic regression of baseline characteristics and admission CBC parameters associated with poor functional outcome at 3 months.
In postoperative CBC parameters, WBC (10.82 [9.01–13.80] vs. 12.93 [10.29–16.86], p = 0.001), neutrophil (8.89 [7.46–11.73] vs. 11.77 [8.56–14.72], p < 0.001), monocyte (0.59 [0.41–0.88] vs. 0.69 [0.51–1.04], p = 0.041), RDW (13.1 [12.6–13.6] vs. 13.9 [13.1–14.5], p < 0.001) and MPV (11.3 ± 1.6 vs. 12.0 ± 1.5, p = 0.004) in patients with poor functional outcome were significantly higher than those with good functional outcome (Table 1). Results of multivariate logistic regression revealed that WFNS grade (odds ratio [95% CI]: 1.439 [1.119–1.850], p = 0.005), MPV (odds ratio [95% CI]: 1.253 [1.012–1.552], p = 0.039) and RDW (odds ratio [95% CI]: 1.411 [1.095–1.818], p = 0.008) independently predicted poor functional outcome (Table 3).
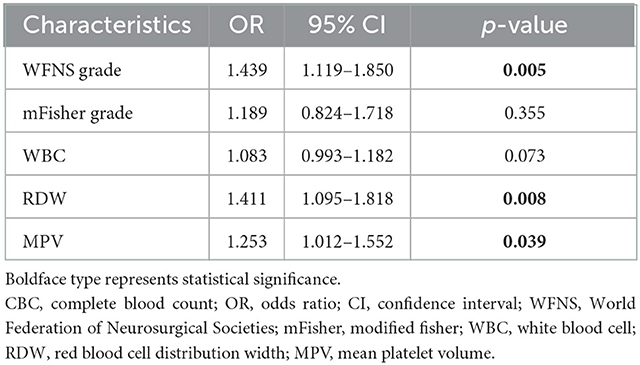
Table 3. Multivariate logistic regression of baseline characteristics and postoperative CBC parameters associated with poor functional outcome at 3 months.
The variation of RBC parameters was analyzed and only RDW showed significant difference. The difference of RDW in patients with poor functional outcome was higher than those with good functional outcome (0.2 [−0.2 to 1.0] vs. 0.0 [−0.3 to 0.4], p = 0.010).
The AUCs of WFNS grade, admission WBC and postoperative RDW and MPV were 0.670 (0.589–0.750), 0.704 (0.626–0.781), 0.707 (0.630–0.784) and 0.623 (0.542–0.704), respectively (Figure 2). The best cutoff point of WFNS grade predicting poor functional outcome (Youden's index = 0.286) was 2.5, where the sensitivity was 57.5% and the specificity was 71.1%. The positive predictive value (PPV) was 56.0% and the negative predictive value (NPV) was 72.3%. The best cutoff point of admission WBC predicting poor functional outcome (Youden's index = 0.383) was 12.875×109/L, where the sensitivity was 69.9% and the specificity was 68.4%. The PPV was 58.6% and the NPV was 78.0%. The best cutoff point of postoperative RDW predicting poor functional outcome (Youden's index = 0.383) was 13.65%, where the sensitivity was 60.3% and the specificity was 78.1%. The PPV was 63.8% and the NPV was 75.4%. The best cutoff point of postoperative MPV predicting poor functional outcome (Youden's index = 0.247) was 11.25 fL, where the sensitivity was 71.2% and the specificity was 53.5%. The PPV was 49.5% and the NPV was 74.4%. There was no significant difference between the AUCs of the four ROC curves (WFNS grade vs. admission WBC, p = 0.462; WFNS grade vs. postoperative RDW, p = 0.477; WFNS grade vs. postoperative MPV, p = 0.419; admission WBC vs. postoperative RDW, p = 0.949; admission WBC vs. postoperative MPV, p = 0.182; postoperative RDW vs. postoperative MPV, p = 0.112). The AUC of postoperative RDW was significantly larger than the difference of RDW (p = 0.020).
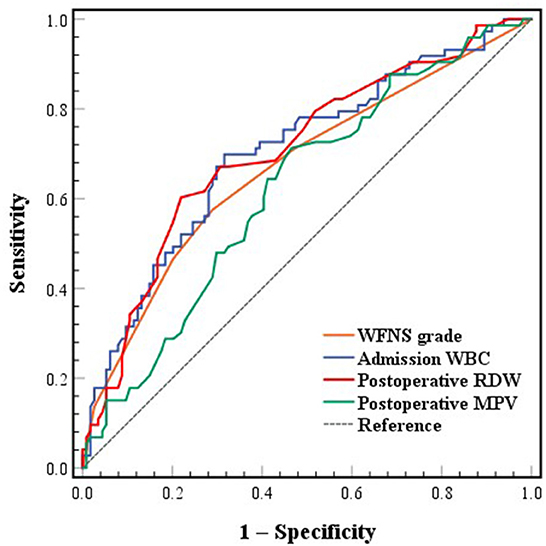
Figure 2. ROC curves of WFNS grade, admission WBC, postoperative RDW and MPV associated with poor functional outcome at 3 months. ROC, receiver operating characteristic; WFNS, World Federation of Neurosurgical Societies; WBC, white blood cell; RDW, red blood cell distribution width; MPV, mean platelet volume.
Three combined diagnostic models based on WFNS grade, admission WBC and postoperative RDW and MPV were established and evaluated to achieve better predictive value. The AUC of parameter combination A (WFNS grade and admission WBC) and B (WFNS grade and postoperative RDW and MPV) was 0.734 (0.657–0.811) and 0.753 (0.685–0.822), respectively (Figure 3). The sensitivity was 54.8% and the specificity was 88.6% at the best cutoff point of parameter combination A (Youden's index = 0.434). The PPV was 75.5% and the NPV was 75.4%. The sensitivity was 50.7% and the specificity was 86.8% at the best cutoff point of parameter combination B (Youden's index = 0.375). The PPV was 71.2% and the NPV was 73.3%. The AUC of parameter combination C (all four parameters) was 0.787 (0.722–0.852) (Figure 3). The sensitivity was 80.8% and the specificity was 63.2% at the best cutoff point of parameter combination C (Youden's index = 0.440). The PPV was 58.4% and the NPV was 83.7%. The AUC of parameter combination C was higher than parameter combination A and B with statistical significance (parameter combination A vs. parameter combination C, p = 0.029; parameter combination B vs. parameter combination C, p = 0.048). The AUC of parameter combination A was significantly higher than WFNS grade (p = 0.018). The AUC of parameter combination B was significantly higher than WFNS grade and postoperative MPV (parameter combination B vs. WFNS grade, p = 0.005; parameter combination B vs. postoperative MPV, p = 0.001). The AUC of parameter combination C was higher than all four parameters alone (parameter combination C vs. WFNS grade, p < 0.001; parameter combination C vs. admission WBC, p = 0.009; parameter combination C vs. postoperative RDW, p = 0.024; parameter combination C vs. postoperative MPV, p < 0.001).
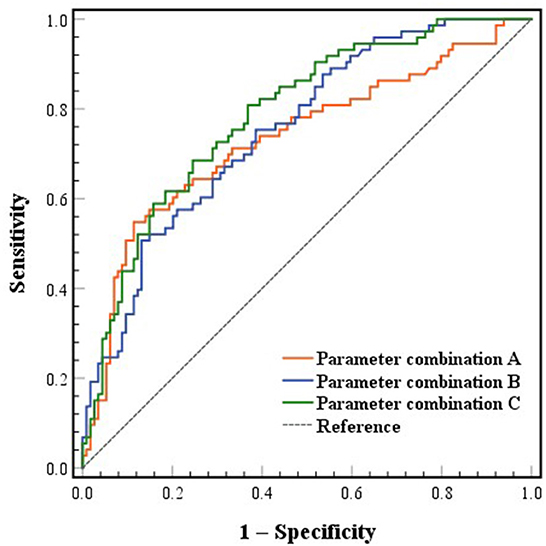
Figure 3. ROC curves of combined parameters predicting poor functional outcome at 3 months. ROC, receiver operating characteristic. Parameter combination A included World Federation of Neurosurgical Societies (WFNS) grade and admission white blood cell (WBC). Parameter combination B included WFNS grade and postoperative red blood cell distribution width (RDW) and mean platelet volume (MPV). Parameter combination C included WFNS grade, admission WBC and postoperative RDW and MPV.
This study showed that admission WBC and postoperative RDW and MPV were associated with poor functional outcome in aSAH patients undergoing surgical clipping, and combining them with WFNS grade could improve the predictive value. It also revealed that combining RBC parameters could substantially increase the clinical prediction of functional outcome.
RDW changes dynamically with the development of aSAH. When an aSAH happens, body damage is inevitable. Clinicians and scientists have been investigated pathophysiological mechanisms following aSAH for decades. Several studies have found that the rupture of an aneurysm leads to a series of mechanisms such as cerebral edema, inflammation, oxidative stress and microthrombosis (16–18). A recent study has shown that the toll-like receptor (TLR) 4/myeloid differentiation primary response protein (MyD) 88/nuclear factor (NF)-κB pathway plays an essential role in the neuroinflammation following aSAH (19). After the activation of TLR4 by endogenous ligands with damage-associated molecular patterns produced after aSAH, the MyD88-dependent pathway activates the transcription factor NF-κB. It also produces pro-inflammatory cytokines such as tumor necrosis factor (TNF)-α, interleukins, intercellular adhesion molecule-1 (19), etc. According to the research by Wang et al. (20), RDW predicts significant inflammation in patients with autoimmune hepatitis. RDW is also associated with serum TLR4 and TNF-α (21, 22), both belonging to the TLR4/MyD88/NF-κB pathway. Therefore, it could be inferred that RDW is a biomarker of inflammation following aSAH. In an animal experiment by Zhao et al. (21), RDW is associated with serum superoxide dismutase and malondialdehyde, representing oxidative stress. Oxidative stress reduces the survival rate of RBCs, causing immature RBCs to increase in circulation, contributing to an increase in RDW. Furthermore, RDW is associated with stroke, cerebral infarction and cerebral vein thrombosis (23, 24). The release of internal organelles and the externalization of vesicular contents in the maturation process of the immature RBCs may lead to the activation of the coagulation system and thrombosis (25). Studies mentioned above suggest that inflammatory response, oxidative stress and microthrombosis are all related to RDW changes after aSAH. Although the admission RDW in the group of poor outcome was found to be significantly higher than the group of good outcome, admission RDW did not predict functional outcome independently in this study. In contrast, WFNS grade and admission WBC, which were deemed to be confounders, showed statistical significance in multivariate logistic regression. Additionally, RDW may not change in such a short amount of time, and factors like nutritional status can also affect the level of RDW, which could explain the results of multivariate logistic regression.
In this study, postoperative RDW was found to independently predict poor functional outcome at 3 months after surgical clipping in patients with aSAH, whereas admission RDW was not a predictor. The elevation of RDW on admission may reflect pathophysiological damage mediated by bleeding, as it is generally known that RDW increases with blood loss. Since blood loss and occasional RBC transfusions are inevitable in craniotomy, an increase in RDW is likely to occur (26). Besides, inflammation, oxidative stress and a hypercoagulable state of blood are everyday events after craniotomy, all probably elevating the RDW level. Since these mechanisms also occur at the initial stage of aSAH, we infer that the disadvantages of surgical clipping may magnify the pathophysiological changes present on admission.
RDW has been widely used for the differential diagnosis of anemia over the past few decades (27, 28). Recent studies have shown that the function of RDW is mainly applied in cardiovascular and cerebrovascular diseases (29). In diagnosing acute myocardial infarction (AMI) among patients with chest pain and the discrimination of stroke subtypes in young patients, RDW demonstrates excellent diagnostic accuracy (30, 31). Other studies have suggested that RDW could also be a risk and outcome predictor. In patients with coronary artery diseases, RDW is associated with myocardial scar burden, impaired left ventricular function and postoperative cognitive dysfunction (32, 33). In patients suffering from atrial fibrillation, RDW enhances the risk of major adverse cardiovascular events, thromboembolic events and all-cause mortality (34–36). In patients undergoing ischemic stroke, RDW predicts worse neurological improvement and mortality (37, 38). RDW also shows predictive performance in hemorrhagic cerebrovascular diseases like spontaneous intracerebral hemorrhage (39) and aSAH (7–9), the latter of which our study focused on.
This study presents the first published analysis investigating the relationship between postoperative RDW and functional outcome in aSAH patients undergoing surgical clipping. Three previous studies performed dynamic monitoring of RDW. Fontana et al. monitored RDW daily from the day of admission for a maximum of 7 days during the intensive unit stay (7), and Siegler et al. (9) and Chugh et al. (15) collected RDW data continuously for up to 10 days or longer after aSAH onset. However, these studies did not mention whether patients received surgical treatment and when the surgical treatment was performed. As we explained above, admission and postoperative RDW are different, so evaluating RDW levels by calculating the maximum or mean throughout the aSAH course is likely to cause bias. In addition, high RDW levels at different periods will correspond to different strategies of clinical management. Hence, the separate assessment of admission and postoperative RDW may provide more practical guidance for the perioperative management of aSAH. Therefore, we selected patients who only underwent surgical clipping to reduce the confounding bias.
In addition to screening for independent predictors of poor functional outcome, we evaluated the differentiation and predictive potential of each predictor individually and in combination for functional outcome by comparing AUCs and calculating PPVs and NPVs. The result of AUC comparison showed that combined models had a higher degree of differentiation than single predictors and the combined model of all four predictors was the highest. The PPVs indicated that the combination of WFNS grade and admission WBC appeared to provide the best predictive power of poor outcome. However, the combination of all parameters had the highest NPV, 83.7%, which could be used to predict good outcome. These results suggest that adding RDW to the predictive model improves the predictive power and has greater potential for predicting good outcome.
The RDW test is an excellent strategy of biomarker detection because it is easy to implement, inexpensive, and noninvasive. Since RDW is independently associated with functional outcome, it could guide clinical decisions in the perioperative management of aSAH, especially in the postoperative management. If the application of RDW is combined with demographics, medical history, clinical grades, radiological data and other laboratory data, it may contribute to better assessment, improve functional outcome and bring great benefit to patients. For example, RBC transfusion is usually given at the discretion of treating physicians when patients suffer blood loss in craniotomy or (and) anemia caused by other factors (40). However, the effect of RBC transfusion in aSAH can be detrimental. Several studies have shown that RBC transfusion is associated with unfavorable functional outcome indicators, such as poor functional outcome, mortality, acute lung injury, acute respiratory distress syndrome and thrombotic events (41–43). RDW is elevated during the regeneration of RBCs after blood loss and help diagnose some types of anemia. However, there is no specific guideline for RBC transfusion in aSAH. Thus, we hypothesize that combining hemoglobin and RDW to adjust transfusion practice may contribute to better functional outcome.
This study has several limitations. First, it is a retrospective study performed at a single center with a small sample size, which is less persuasive than a large prospective study. Second, although baseline information regarding demographics, addictions, medical history, admission clinical grades and aneurysm characteristics was collected, some data like nutritional status, reticulocyte count and RBC transfusion records were not obtained. Third, other outcome indicators such as mortality, cerebral infarction, cognitive impairment, etc., were not collected. Finally, dynamic monitoring of RDW wasn't performed, which could provide more in-depth analysis.
Postoperative RDW is independently associated with poor functional outcome in aSAH patients undergoing surgical clipping. Combing postoperative RDW and MPV with WFNS grade and WBC on admission may help predict good outcome more accurately. Further research is demanded to determine the clinical value and relevant mechanisms.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Medical Ethics Committee of Affiliated Hospital of North Sichuan Medical College. The Ethics Committee waived the requirement of written informed consent for participation.
This study was conceptualized and designed by LZ, YZ, XZ, and XT. Data collection and analysis were performed by LZ, YZ, PL, WL, XH, HL, MX, and XC. The original manuscript was written by LZ and YZ. Review and revision of the manuscript were performed by XZ and XT. All authors read and approved the final manuscript. All authors commented on previous versions of the manuscript.
This study was supported by the Funds for Cooperation Project of Nanchong City and North Sichuan Medical College, Grant No. 20SXQT0317 (to LZ), Research and Development Project of Affiliated Hospital of North Sichuan Medical College, Grant No. 2022SK021 (to XZ), and Innovation and Entrepreneurship Training Program for College Students in Sichuan Province, Grant No. S202210634098 (to YZ).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Tawk RG, Hasan TF, D'Souza CE, Peel JB, Freeman WD. Diagnosis and Treatment of Unruptured Intracranial Aneurysms and Aneurysmal Subarachnoid Hemorrhage. Mayo Clin Proc. (2021) 96:1970–2000. doi: 10.1016/j.mayocp.2021.01.005
2. Daou BJ, Koduri S, Thompson BG, Chaudhary N, Pandey AS. Clinical and experimental aspects of aneurysmal subarachnoid hemorrhage. CNS Neurosci Ther. (2019) 25:1096–112. doi: 10.1111/cns.13222
3. Diringer MN, Bleck TP, Claude Hemphill J. 3rd, Menon D, Shutter L, Vespa P, et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the neurocritical care society's multidisciplinary. Consen Conferen Neurocrit Care. (2011) 15:211–40. doi: 10.1007/s12028-011-9605-9
4. Connolly ES. Jr., Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke. Assoc Stroke. (2012) 43:1711–37. doi: 10.1161/STR.0b013e3182587839
5. Ayling OGS, Ibrahim GM, Alotaibi NM, Gooderham PA, Macdonald RL. Anemia after aneurysmal subarachnoid hemorrhage is associated with poor outcome and death. Stroke. (2018) 49:1859–65. doi: 10.1161/strokeaha.117.020260
6. Gong L, Gu Y, Dong Q, Zhang X, Wang H, Zhao Y, et al. A direct correlation between red blood cell indices and cognitive impairment after aneurysmal subarachnoid hemorrhage (Asah). Curr Neurovasc Res. (2019) 16:142–7. doi: 10.2174/1567202616666190412142718
7. Fontana V, Bond O, Spadaro S, Annoni F, Nobile L, Badenes R, et al. Red cell distribution width after subarachnoid hemorrhage. J Neurosurg Anesthesiol. (2018) 30:319–27. doi: 10.1097/ana.0000000000000459
8. Hong DY, Kim SY, Kim JY, Kim JW. Red blood cell distribution width is an independent predictor of mortality in patients with aneurysmal subarachnoid hemorrhage. Clin Neurol Neurosurg. (2018) 172:82–6. doi: 10.1016/j.clineuro.2018.06.044
9. Siegler JE, Marcaccio C, Nawalinski K, Quattrone F, Sandsmark DK, Maloney-Wilensky E, et al. Elevated red cell distribution width is associated with cerebral infarction in aneurysmal subarachnoid hemorrhage. Neurocrit Care. (2017) 26:26–33. doi: 10.1007/s12028-016-0306-2
10. Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (tripod): the tripod statement. BMJ. (2015) 350:g7594. doi: 10.1136/bmj.g7594
11. Tao C, Wang J, Hu X, Ma J, Li H, You C. Clinical value of neutrophil to lymphocyte and platelet to lymphocyte ratio after aneurysmal subarachnoid hemorrhage. Neurocrit Care. (2017) 26:393–401. doi: 10.1007/s12028-016-0332-0
12. Feghali J, Kim J, Gami A, Rapaport S, Caplan JM, McDougall CG, et al. Monocyte-based inflammatory indices predict outcomes following aneurysmal subarachnoid hemorrhage. Neurosurg Rev. (2021) 44:3499–507. doi: 10.1007/s10143-021-01525-1
13. Zhao L, Chen T, Yan HJ, Liu C, Cao Y, Zhang Y, et al. Development and validation of an early predictive nomogram for delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Ann Transl Med. (2021) 9:1664. doi: 10.21037/atm-21-5200
14. Wolfe CD, Taub NA, Woodrow EJ, Burney PG. Assessment of scales of disability and handicap for stroke patients. Stroke. (1991) 22:1242–4. doi: 10.1161/01.str.22.10.1242
15. Chugh C, Nyirjesy SC, Nawalinski KP, Sandsmark DK, Frangos S, Maloney-Wilensky E, et al. Red blood cell distribution width is associated with poor clinical outcome after subarachnoid hemorrhage: a pilot study. Neurocrit Care. (2015) 23:217–24. doi: 10.1007/s12028-015-0117-x
16. van Lieshout JH, Dibué-Adjei M, Cornelius JF, Slotty PJ, Schneider T, Restin T, et al. An introduction to the pathophysiology of aneurysmal subarachnoid hemorrhage. Neurosurg Rev. (2018) 41:917–30. doi: 10.1007/s10143-017-0827-y
17. Hayman EG, Wessell A, Gerzanich V, Sheth KN, Simard JM. Mechanisms of global cerebral edema formation in aneurysmal subarachnoid hemorrhage. Neurocrit Care. (2017) 26:301–10. doi: 10.1007/s12028-016-0354-7
18. Wu F, Liu Z, Li G, Zhou L, Huang K, Wu Z, et al. Inflammation and oxidative stress: potential targets for improving prognosis after subarachnoid hemorrhage. Front Cell Neurosci. (2021) 15:739506. doi: 10.3389/fncel.2021.739506
19. Okada T, Suzuki H. Toll-like receptor 4 as a possible therapeutic target for delayed brain injuries after aneurysmal subarachnoid hemorrhage. Neural Regen Res. (2017) 12:193–6. doi: 10.4103/1673-5374.200795
20. Wang H, Wang J, Huang R, Xia J, Zuo L, Yan X, et al. Red blood cell distribution width for predicting significant liver inflammation in patients with autoimmune hepatitis. Eur J Gastroenterol Hepatol. (2019) 31:1527–32. doi: 10.1097/meg.0000000000001447
21. Zhao Z, Liu T, Li J, Yang W, Liu E, Li G. Elevated red cell distribution width level is associated with oxidative stress and inflammation in a canine model of rapid atrial pacing. Int J Cardiol. (2014) 174:174–6. doi: 10.1016/j.ijcard.2014.03.189
22. Lorente L, Martín MM, Abreu-González P, Solé-Violán J, Ferreres J, Labarta L, et al. Red blood cell distribution width during the first week is associated with severity and mortality in septic patients. PLoS ONE. (2014) 9:e105436. doi: 10.1371/journal.pone.0105436
23. Söderholm M, Borné Y, Hedblad B, Persson M, Engström G. Red cell distribution width in relation to incidence of stroke and carotid atherosclerosis: a population-based cohort study. PLoS ONE. (2015) 10:e0124957. doi: 10.1371/journal.pone.0124957
24. Maino A, Abbattista M, Bucciarelli P, Artoni A, Passamonti SM, Lanfranconi S, et al. Red cell distribution width and the risk of cerebral vein thrombosis: a case-control study. Eur J Intern Med. (2017) 38:46–51. doi: 10.1016/j.ejim.2016.10.017
25. Thachil J. Immature reticulocytes and its relevance to thrombosis. Ann Hematol. (2008) 87:1025–6. doi: 10.1007/s00277-008-0524-6
26. Spadaro S, Taccone FS, Fogagnolo A, Franchi F, Scolletta S, Ragazzi R, et al. The effects of blood transfusion on red blood cell distribution width in critically ill patients: a pilot study. Transfusion. (2018) 58:1863–9. doi: 10.1111/trf.14759
27. Salvagno GL, Sanchis-Gomar F, Picanza A, Lippi G. Red blood cell distribution width: a simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci. (2015) 52:86–105. doi: 10.3109/10408363.2014.992064
28. Said AS, Spinella PC, Hartman ME, Steffen KM, Jackups R, Holubkov R, et al. RBC distribution width: biomarker for red cell dysfunction and critical illness outcome? Pediatr Crit Care Med. (2017) 18:134–42. doi: 10.1097/pcc.0000000000001017
29. Li N, Zhou H, Tang Q. Red blood cell distribution width: a novel predictive indicator for cardiovascular and cerebrovascular diseases. Dis Markers. (2017) 2017:7089493. doi: 10.1155/2017/7089493
30. Lippi G, Filippozzi L, Montagnana M, Salvagno GL, Franchini M, Guidi GC, et al. Clinical usefulness of measuring red blood cell distribution width on admission in patients with acute coronary syndromes. Clin Chem Lab Med. (2009) 47:353–7. doi: 10.1515/cclm.2009.066
31. Demir R, Saritemur M, Atis O, Ozel L, Kocaturk I, Emet M, et al. Can we distinguish stroke and stroke mimics via red cell distribution width in young patients? Arch Med Sci. (2015) 11:958–63. doi: 10.5114/aoms.2014.40995
32. Magri CJ, Tian TX, Camilleri L, Xuereb R, Galea J, Fava S. Red Blood cell distribution width and myocardial scar burden in coronary artery disease. Postgrad Med J. (2017) 93:607–12. doi: 10.1136/postgradmedj-2016-134781
33. Wan J, Luo P, Du X, Yan H. Preoperative red cell distribution width predicts postoperative cognitive dysfunction after coronary artery bypass grafting. Biosci Rep. (2020) 40:4. doi: 10.1042/bsr20194448
34. Wan H, Yang Y, Zhu J, Huang B, Wang J, Wu S, et al. The relationship between elevated red cell distribution width and long-term outcomes among patients with atrial fibrillation. Clin Biochem. (2015) 48:762–7. doi: 10.1016/j.clinbiochem.2015.06.001
35. Cha MJ, Lee HS, Kim HM, Jung JH, Choi EK, Oh S. Association between red cell distribution width and thromboembolic events in patients with atrial fibrillation. Eur J Intern Med. (2017) 46:41–6. doi: 10.1016/j.ejim.2017.07.028
36. Saliba W, Barnett-Griness O, Rennert G. Red cell distribution width and all-cause mortality in patients with atrial fibrillation: a cohort study. J Arrhythm. (2017) 33:56–62. doi: 10.1016/j.joa.2016.06.001
37. Turcato G, Cappellari M, Follador L, Dilda A, Bonora A, Zannoni M, et al. Red blood cell distribution width is an independent predictor of outcome in patients undergoing thrombolysis for ischemic stroke. Semin Thromb Hemost. (2017) 43:30–5. doi: 10.1055/s-0036-1592165
38. Wang L, Wang C, Wu S, Li Y, Guo W, Liu M. Red blood cell distribution width is associated with mortality after acute ischemic stroke: a cohort study and systematic review. Ann Transl Med. (2020) 8:81. doi: 10.21037/atm.2019.12.142
39. Pinho J, Silva L, Quintas-Neves M, Marques L, Amorim JM, Reich A, et al. Red cell distribution width is associated with 30-day mortality in patients with spontaneous intracerebral hemorrhage. Neurocrit Care. (2021) 34:825–32. doi: 10.1007/s12028-020-01103-1
40. Sampson TR, Dhar R, Diringer MN. Factors associated with the development of anemia after subarachnoid hemorrhage. Neurocrit Care. (2010) 12:4–9. doi: 10.1007/s12028-009-9273-1
41. Kumar MA, Levine J, Faerber J, Elliott JP, Winn HR, Doerfler S, et al. The effects of red blood cell transfusion on functional outcome after aneurysmal subarachnoid hemorrhage. World Neurosurg. (2017) 108:807–16. doi: 10.1016/j.wneu.2017.09.038
42. Festic E, Rabinstein AA, Freeman WD, Mauricio EA, Robinson MT, Mandrekar J, et al. Blood transfusion is an important predictor of hospital mortality among patients with aneurysmal subarachnoid hemorrhage. Neurocrit Care. (2013) 18:209–15. doi: 10.1007/s12028-012-9777-y
Keywords: aneurysmal subarachnoid hemorrhage, red blood cell distribution width, surgical clipping, functional outcome, predictor
Citation: Zhao L, Zhang Y, Lin P, Li W, Huang X, Li H, Xia M, Chen X, Zhu X and Tang X (2022) Postoperative red blood cell distribution width predicts functional outcome in aneurysmal subarachnoid hemorrhage after surgical clipping: A single-center retrospective study. Front. Neurol. 13:1036433. doi: 10.3389/fneur.2022.1036433
Received: 04 September 2022; Accepted: 30 November 2022;
Published: 22 December 2022.
Edited by:
Jun Xu, Beijing Tiantan Hospital, Capital Medical University, ChinaReviewed by:
Sebastian Major, Charité Universitätsmedizin Berlin, GermanyCopyright © 2022 Zhao, Zhang, Lin, Li, Huang, Li, Xia, Chen, Zhu and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xi Zhu,  bnNtY196aHVxaWFuQDE2My5jb20=; Xiaoping Tang,
bnNtY196aHVxaWFuQDE2My5jb20=; Xiaoping Tang,  bnNtY190eHBpbmcxOTcxQDE2My5jb20=
bnNtY190eHBpbmcxOTcxQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.