
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 10 November 2022
Sec. Movement Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.1036068
 Peter A. LeWitt1*
Peter A. LeWitt1* Fabrizio Stocchi2
Fabrizio Stocchi2 David Arkadir3
David Arkadir3 Yoseph Caraco4
Yoseph Caraco4 Liat Adar5
Liat Adar5 Itay Perlstein6
Itay Perlstein6 Ryan Case5
Ryan Case5 Nir Giladi7
Nir Giladi7Background: While treatment with levodopa remains the cornerstone of Parkinson's disease (PD) management, chronic oral therapy is often associated with the development of motor complications, that correlate to fluctuating levodopa plasma concentrations, limiting its clinical utility. Continuous infusion is considered to be the optimal delivery route for treating PD patients with motor fluctuations, but current infusion systems require invasive surgery. Subcutaneous infusion of (SC) levodopa has the potential to provide a better tolerated and more convenient route of continuous levodopa delivery. ND0612 is in development as a combination product providing continuous levodopa/carbidopa via a minimally invasive, subcutaneous delivery system for PD patients experiencing motor response fluctuations. We present pharmacokinetic results from a series of studies that analyzed plasma concentrations after SC levodopa delivery with ND0612 to inform the clinical development program.
Methods: We performed a series of six Phase I and II studies to characterize the pharmacokinetics of levodopa and carbidopa derived from ND0612 infusion with/without adjunct oral therapy of the same ingredients. These studies were conducted in healthy volunteers and in PD patients experiencing motor response fluctuations while on their current levodopa therapy regimen.
Results: Taken together, the results demonstrate dose-proportionality dependent on rate of subcutaneous levodopa infusion leading to stable and sustained plasma concentrations of levodopa. Subcutaneous infusion of ND0612 administered with oral levodopa/carbidopa maintained near-constant, therapeutic levodopa plasma concentrations, thereby avoiding the troughs in levodopa plasma concentrations that are associated with OFF time in PD. The data generated in this series of studies also confirmed that a levodopa/carbidopa dose ratio of 8:1 would be the most reasonable choice for ND0612 development.
Conclusions: This series of clinical pharmacokinetic studies have demonstrated that ND0612, administered continuously with a levodopa concentration of 60 mg/ml combined with carbidopa 7.5 mg/ml, and complemented with oral levodopa/carbidopa, is suitable for 24 h continuous administration in patients with PD. The stable plasma concentrations of levodopa achieved predict utility of ND0612 as a parenteral formulation for achieving clinically useful delivery of levodopa for PD patients.
Although more than two dozen drugs have undergone human testing as alternatives for achieving striatal dopaminergic stimulation, levodopa remains the most effective drug for controlling the motor symptoms of Parkinson's disease (PD) (1, 2). Most patients receiving levodopa chronically experience continuing benefits, although the consistency of antiparkinsonian effect from each oral dose tends to decline over time. A key driver in the search for improved therapies has been the problem of motor complications (response fluctuations and dyskinesia) that can develop with long-term levodopa use. Recent cohort studies estimate the 5-year cumulative incidence of response fluctuations and dyskinesias ranges between 29 and 54% in the overall levodopa-treated PD population (3–5), increasing to near-universal occurrence after 10 years or more of continuing levodopa use (5). These problems have significant impact on employment, independent functioning, safety, and quality of life (3, 6–10), particularly in patients with a younger age of onset (4). Response fluctuations evolve as patients experience the waning of the “long duration” response to levodopa dosing over time [the sustained motor improvement that builds up slowly and can persist for days after each dose (5)] and the “short duration” response (in which the therapeutic response closely parallels the plasma pharmacokinetics of levodopa) starts to predominate (11). The major pharmacodynamic challenge for optimizing PD therapeutics has been to reduce the variability of circulating levodopa concentrations to overcome the problems of the short duration response in order to lessen fluctuations in both motor and non-motor signs and symptoms.
Whereas, OFF states can have other causes to explain why PD patients are unresponsive to striatal dopaminergic stimulation (such as the phenomenon of gait freezing), the most common explanation for motor fluctuations is simply that of inconsistent levodopa delivery to the brain (11–13). Indeed, much of the blame for motor fluctuations falls on inconsistent gastrointestinal mechanisms leading to insufficient absorption of the drug, substantial intraindividual variability (14), and delayed onset of its antiparkinsonian effects (15, 16). Declining efficiency of the stomach to deliver oral levodopa to its sole absorption site in the proximal small intestine has been recognized as one of the consequences of chronic PD (16). Gastrointestinal dysfunction is frequent in PD, eventually affecting almost all patients during their disease course (16–18). For example, prolonged gastric emptying time can occur throughout the course of PD (18), and orally-administered levodopa can itself increase gastric acid secretion, impair gastric relaxation, and delay gastric emptying (19, 20).
Continuous levodopa delivery to the brain has not been possible to achieve with orally-dosed levodopa, even with pharmacological advances designed to achieve greater extension of levodopa release as compared to the immediate-release formulation (19). Drugs designed to block the peripheral catabolism of levodopa [catechol-O-methyltransferase (COMT) inhibitors] or retard the oxidative deamination of dopamine in the brain (monoamine oxidase-B inhibitors) achieve only a limited extension in duration of antiparkinsonian effect (21–23). When a patient has lost the long-duration response, the short plasma half-life of levodopa (~90–150 min) will require that immediate-release products be dosed repeatedly at intervals as close as 2–3 hourly intervals (22). Clinical experience shows that even these strategies, combined with MAO-B and COMT inhibitors, often fail to accomplish continuity of levodopa effect (24, 25). Thus, there has been a keen interest to improve levodopa therapeutics by optimizing its delivery to the brain by means of an alternative to its oral (and therefore gastrointestinal) delivery.
Pharmacodynamic studies exploring continuous intravenous levodopa infusion into a patient with PD first revealed the potential offered by parenteral levodopa delivery (26). Another route of administration has been developed in a marketed product for infusion of a carbidopa-levodopa suspension mixture continuously pumped into the proximal small intestine (27, 28). Partial reduction of OFF time and lessening of troublesome levodopa-induced dyskinesias has been accomplished by per-gastric intestinal infusion by the latter strategy. However, intra-intestinal delivery still delivers levodopa through the intestinal wall and has practical and tolerability issues that limit its use for the common problem of irregular dopaminergic effect (29, 30). One potential answer to the challenge of improving levodopa therapeutics is ND0612 (NeuroDerm, Rehovot, Israel), a combination product providing continuous levodopa/carbidopa via a minimally invasive, subcutaneous (SC) delivery system in development for people with PD experiencing motor fluctuations. As the first levodopa liquid formulation created for SC delivery, ND0612 has undergone a clinical development program with a series of early Phase I and II studies for characterizing and optimizing pharmacokinetics of its two key components, levodopa and carbidopa.
We present pharmacokinetic results from a series of Phase I and Phase II clinical studies that have analyzed plasma concentrations and pharmacodynamics of SC levodopa delivery. These studies informed the development of ND0612 as a PD therapy for patients with motor response fluctuations and have provided key information for its Phase III program. Clinical experience from these studies have provided insights into the pharmacokinetic behavior of levodopa and carbidopa when each are administered subcutaneously.
We performed a series of six Phase I and II studies to characterize the pharmacokinetics of levodopa and carbidopa derived from ND0612 infusion with/without adjunct oral therapy of the same active ingredients. These studies were conducted in healthy volunteers and in PD patients experiencing an established pattern of motor fluctuations while on their current regimen of levodopa and an inhibitor of aromatic L-amino acid decarboxylase, also known as dopa-decarboxylase (DDC), either carbidopa or benserazide. Table 1 provides an overview of the five study methodologies and Supplementary Table 1 provides further details per study. Each study was conducted in accordance with the Declaration of Helsinki and International Conference on Harmonization Good Clinical Practice Guidelines. All participants provided written informed consent. Institutional review boards at the participating sites approved the study protocol, consent forms, and associated amendments.
During each treatment period, standardized meals with a low content of protein were provided to minimize surges of dietary-derived amino acids, which in some circumstances may compete with levodopa uptake. Serial blood samples for pharmacokinetic analysis of levodopa, carbidopa, and the levodopa metabolite 3-O-Methyldopa (3-OMD) were collected at relevant time points. Plasma levodopa, carbidopa, and 3-OMD concentrations were analyzed using validated liquid chromatography coupled to tandem mass spectrometry (LC/MS/MS) methods.
For levodopa, the lower limit of quantitation (LLOQ) was 50 ng/ml, and the upper limit of quantitation (ULOQ) was 5,000 ng/ml. For carbidopa, the LLOQ was 10 ng/ml and the ULOQ was 1,000 ng/ml. The pharmacokinetic population for each study included all participants who had received at least one dose of ND0612 and had a minimum of 3 quantifiable post-dose plasma concentrations per analyte. Across the studies, pharmacokinetic analysis of the concentration-time data was performed using non-compartmental analysis to obtain the area under the concentration-time curve (AUC) and the maximum observed plasma concentrations (Cmax).
In addition, Study 003 evaluated the time the plasma concentration was above 1,000 ng/ml (T >1,000 ng/ml) (31) and the Fluctuation Index calculated as (Cmax–Cmin)/Caverage (32). Dose proportionality was assessed in Study 001 using a linear regression analysis of log-transformed levodopa AUC15 − 24 and in Study 005 using a power model on log-transformed AUC0 − inf, AUC0 − last, and Cmax, including terms for dose fitted as a fixed (continuous) effect and participant as a random effect.
Safety was assessed in each of the studies through the standard recording of adverse events. In addition, local skin safety was specifically assessed across the studies. Skin assessments typically included the assessment of nodules, hematomas and pain.
Levodopa concentrations generally increased with increasing infusion rates at a nearly dose proportional manner. In Study 001, conducted in healthy volunteers, stable levodopa and carbidopa concentrations were already attained by 15 h (timing of the first blood sample) of a 24-h continuous infusion period, and the study participants maintained these stable concentrations for the remainder of the 24-h infusion period. Mean levodopa AUC15 − 24 values ranged from 1,413 h•ng/ml in the 80 μL/h group to 4,199 h•ng/ml in the 240 μL/h group. Linear regression analysis of log-transformed mean AUC15 − 24 values demonstrated a slope value of 1.02 (95% CI: 0.92, 1.12) (Figure 1A). Mean AUC values of carbidopa from 15 to 24 h also increased with infusion rate. The average AUC values ranged from 849 h•ng/ml in the 80 μL/h group (Group 1) to 2,201 h•ng/ml in the 240 μL/h group (Group 6). The increase in carbidopa AUC15 − 24, as a function of infusion rate, was linear and proportional to rate of infusion demonstrating a slope of 0.92 (95% CI: 0.78, 1.06). Similar results demonstrating carbidopa dose proportionality were obtained for the maximum carbidopa concentration during the 15- to 24-h period and for the mean carbidopa concentration at both 15 and 24 h of the infusion period.
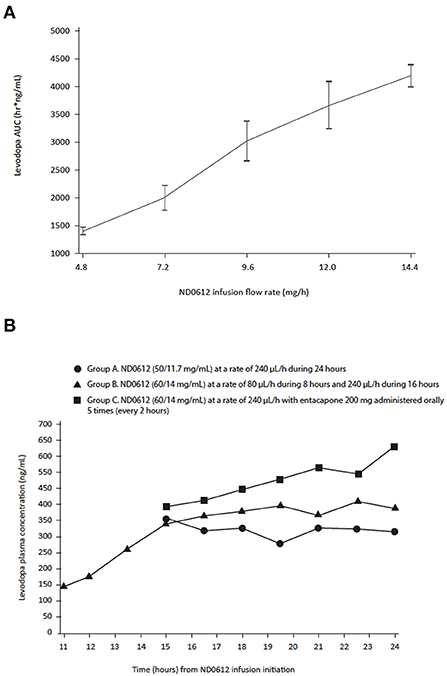
Figure 1. Levodopa (A) area under the curve (B) concentrations over time following SC infusion with ND0612 in healthy volunteers. (A) AUC comparisons between cohorts were made on the 15- to 24-h time period after the start of the infusion (B) Blood samples were collected at 11, 12, 13.5, 15 h for Group B only, and 16.5, 18, 19.5, 21, 22.5, and 24 h for all three groups.
Similar results were seen in Study 001b where, consistent with the results of the previous study, ND0612 administered SC for 24 h achieved clinically relevant plasma concentrations by at least 15 h (Figure 1B). An increase in the concentration of ND0612 (from 50/11.7 to 60/14 mg/ml levodopa/carbidopa) resulted in a corresponding increase in the mean AUC values as would be expected (from 3,070 to 3,677 h•ng/ml). When increasing the infusion rate 3-fold from 80 to 240 μL/h, mean concentrations of levodopa increased over a 4–5-h period and then stabilized. There was a further increase in levodopa concentrations with the addition of entacapone (every 2 h for the last 10 h of the 24-h infusion period) as would be expected with inhibition of COMT activity.
Stable levodopa and carbidopa concentration with ND0612 administration were also demonstrated in patients with PD. In Study 002, where SC infusion of ND0612 started in the early evening and one dose of an oral fixed combination immediate-release levodopa/carbidopa/entacapone [LD/CD/E (100/25/200)] was administered at bedtime (~3 h after the start of the infusion), stable levodopa concentrations were observed from 9 h and stable carbidopa concentrations from 7 h until the morning oral LD/CD/E dose (taken at 15 h). Increases in overall levodopa and carbidopa concentrations (i.e., levodopa and carbidopa from ND0612 + oral LD/CD/E) were observed within 1 h of the morning oral LD/CD/E dose intake with the peak levodopa concentrations occurring at 3 h post-oral LD/CD/E intake; mean levodopa plasma concentrations were sustained ≥25% higher than before administration of the oral LD/CD/E dose for the remainder of the 24-h observation period (Figure 2).
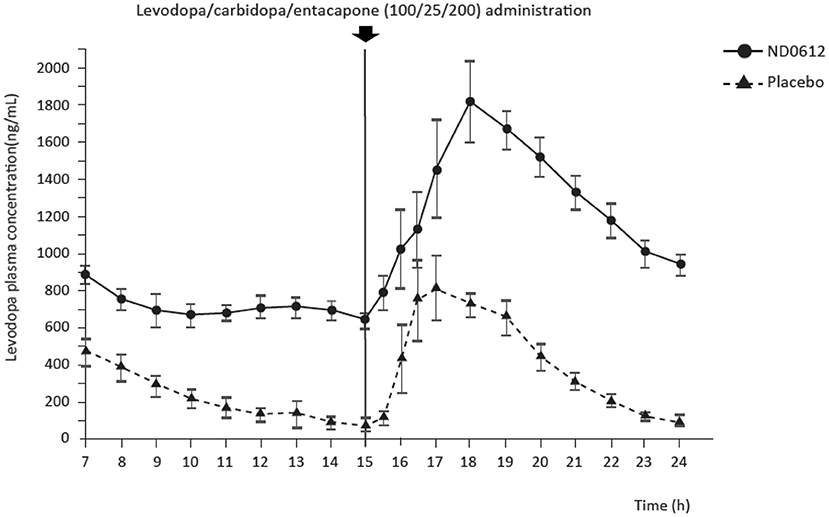
Figure 2. Mean levodopa concentrations over time in patients with Parkinson's disease. Blood sampling began at 7 h post-infusion start. Oral levodopa/carbidopa/entacapone (100/25/200) was taken at 3- and 15-h post-infusion start.
Both studies 002 and 003 used what can be considered a “low” dose of ND0612 (total daily levodopa/carbidopa dose: 270 mg/63 mg). Key pharmacokinetic parameters for levodopa and carbidopa (Cmax, AUC and fluctuation index) are summarized for studies in patients with PD in Tables 2, 3.
Despite the low dose, Study 003 showed that continuous SC administration of ND0612 + SoC oral levodopa/carbidopa ameliorated the variability in levodopa plasma concentrations as compared to placebo infusion + SoC. Patients treated with ND0612 had their plasma levodopa concentrations consistently maintained above a mean of 800 ng/ml, and completely avoided the low trough concentrations observed in the placebo group (Figure 3). There was also a significant increase in the duration that levodopa concentrations above 1,000 ng/ml (mean increase of 4.4 ± 2.2 h in a 10-h period, p < 0.0001) which was not apparent in the placebo group (mean of 4.5 h at baseline and at end of Period-1). The increase in mean levodopa exposure achieved with ND0612 + SoC was accompanied by a decreased variability in plasma levodopa concentrations, as evidenced by a decreased Fluctuation Index vs. placebo + SoC (1.6 ± 0.5 vs. 3.1 ± 1.6, respectively, at end of Period-1). The addition of entacapone to the continuous ND0612 SC infusion in Period 2 translated to an increase in mean levodopa AUC compared with monotherapy.
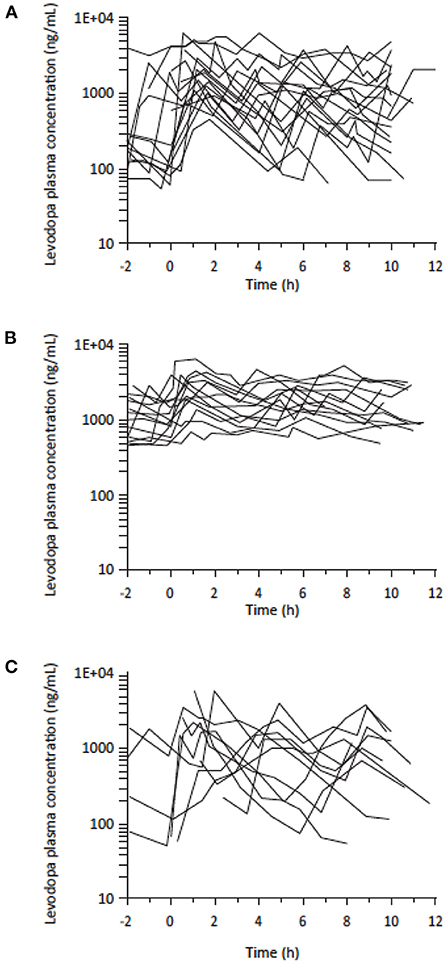
Figure 3. Levodopa plasma levels (logarithmic scale) in patients with PD experiencing motor fluctuations treated with (A) standard of care (SoC) levodopa (N = 30) (B) SoC levodopa plus ND0612 infusion (N = 19)* (C) SoC levodopa plus placebo infusion (N = 11)*. *Standard of care levodopa plus ND0612 (60/14 mg/ml) or placebo infused at a rate of 0.08 ml/h over 8 h and 0.24 ml/h over 16 h.
Study 004 explored the impact of two concentrations of carbidopa in the formulation (7.5 and 14 mg/ml, giving a LD/CD ratio of 8:1 and 4:1, respectively) on levodopa concentrations. Both the low and high ND0612 regimens maintained near-constant, therapeutic levodopa plasma concentrations. Levodopa plasma concentrations were dose proportional, with the high dose of 640 μL/h achieving around 3-fold higher plasma concentrations than the low dose 240 μL/h ND0612 regimen, which corresponds to the ~3-fold increase in daily levodopa dose infused. Figure 4 shows the mean plasma levodopa concentrations following continuous SC administration of low and high dose ND0612 with the different carbidopa concentrations in the formulation as well as adding entacapone to the high CD formulations.
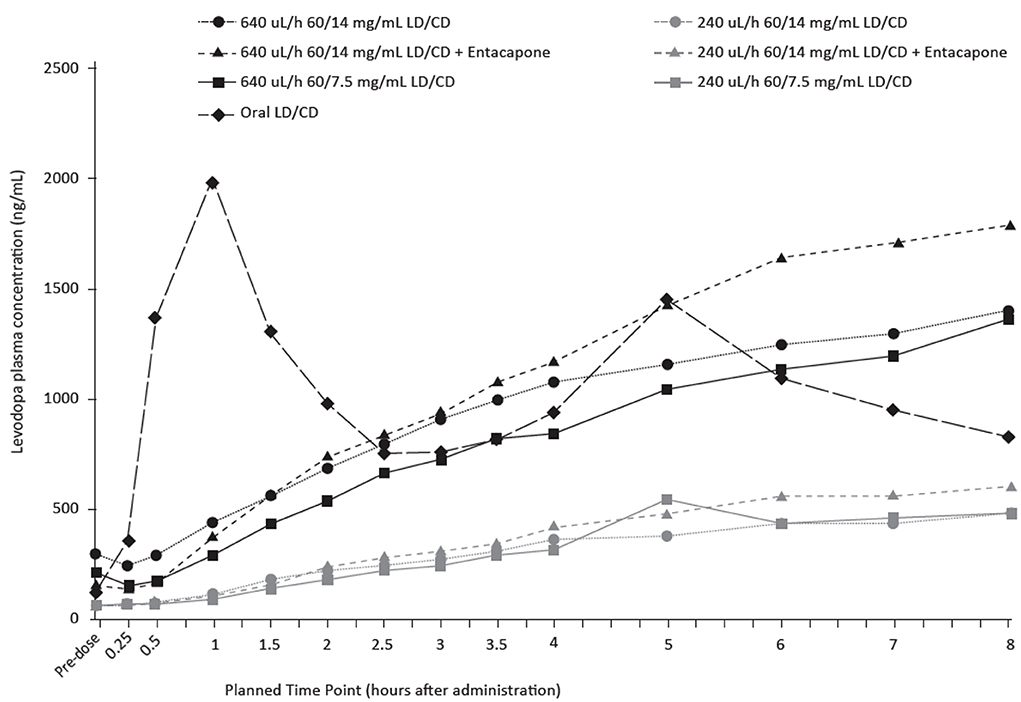
Figure 4. Mean plasma levodopa levels following continuous SC administration of ND0612 over 8 h with varying rates and carbidopa concentrations.
The magnitude of the levodopa plasma concentration differences between the two different ND0612 formulations of carbidopa concentration is likely to be not clinically relevant, with both concentrations achieving clinically relevant levodopa concentrations as compared to the oral dosing concentrations. Carbidopa exposure concentrations increased proportionally with carbidopa dose. The addition of entacapone, increased the steady state levodopa concentrations achieved with both regimens.
The effect of carbidopa concentration was further studied in the 005 study in healthy volunteers where study participants received either low or high rates (doses) of SC ND0612 infusion with three different carbidopa concentrations and ratios from levodopa (7.5 mg/ml, 4:1; 6 mg/ml, 10:1; and 4 mg/ml, 15:1). When administered at the low rate of infusion, mean [95%CI] slope estimates for levodopa exposure on the linear mixed model (log scale) were 0.004 (0.0002, 0.008) and 0.005 (0.001, 0.009) for AUC0 − last and AUC0 − 24, respectively. These slope estimates were statistically different from zero (p < 0.05), indicating that levodopa AUC rose with increasing carbidopa dose. By contrast, for the high rate of ND0612 infusion, levodopa exposure was relatively unaffected by the carbidopa dose level, with no more than a 5% difference in exposure over the dose range (Figure 5).

Figure 5. Mean plasma levodopa concentrations following continuous SC administration of ND0612 (high dose) with varying carbidopa concentrations.
For both the high and low infusion rates, carbidopa exposure increased in a dose-proportional manner with respect to increasing carbidopa dose. The 7.5 mg/ml dose of carbidopa consistently resulted in an AUC0 − inf above 2,000 ng•h/ml, which is estimated to provide maximal inhibition of DDC, while lower carbidopa concentrations could potentially compromise levodopa bioavailability (31).
Across these short-duration studies, there was no consistent pattern of an increase in frequency (number of adverse events), incidence (number of subjects with at least one adverse event), or severity of adverse events (AEs) with increasing infusion rates of ND0612. An overall summary of AEs is given in Supplementary Table 2. All AEs assessed as related to the study drug were mild or moderate in severity, and none of them led to premature treatment discontinuation. The most common AEs were infusion site reactions and/or pain at the infusion site. There were no clinically significant treatment-emergent changes in any clinical laboratory parameters, vital signs, ECG parameters, or physical examination findings.
Subcutaneous infusion of levodopa may provide a well-tolerated and convenient route of continuous levodopa delivery. However, until the development of ND0612, the poor solubility of levodopa precluded this approach. The series of studies described above formed the basis for the final formulation of ND0612 which is now in Phase III of its clinical development. Taken together, the results demonstrate that subcutaneous levodopa infusion achieves stable and sustained plasma concentrations of levodopa as well as dose-proportionality with plasma concentrations increasing with increased infusion rates. Resulting from consistent administration and bypassing the gastrointestinal tract, the stable concentrations of levodopa achieved support ND0612 as a potential parenteral formulation for achieving clinically useful delivery of levodopa for PD patients.
It is generally agreed that plasma levodopa concentration need to be maintained above a certain threshold to achieve sustained relief of PD symptoms. Several investigations have estimated this threshold concentration to be about 1,000 ng/ml (14, 33, 34). In this series of investigations, subcutaneous infusion of “high” doses of ND0612 consistently remained above this threshold and avoided the troughs below the concentrations associated with OFF episodes. Even when lower dosing regimens were trialed in Study 003, continuous SC administration of ND0612 ameliorated both the troughs in levodopa plasma concentrations and the variability in levodopa concentrations (as reflected by the Fluctuation Index vs. placebo). The Fluctuation Index is a measure of the magnitude of rise and fall of levodopa plasma concentrations relative to the average concentration; the lower the Fluctuation Index, the more likely the Cmax is blunted relative to the trough, thereby minimizing potential Cmax-related adverse effects [including peak-effect dyskinesia (33)]. From these data, it is reasonable to believe that treatment with NDO612 should also ameliorate dyskinesia (since the Cmax is lower for ND0612 vs. oral formulations). However, a limitation of current and ongoing studies is that they focus on a population of patients primarily suffering from OFF time. In Study 004, both the low and high ND0612 regimens maintained near-constant, therapeutic levodopa plasma concentrations.
Of particular note, the development plan considered that the ideal dosing of carbidopa with levodopa has never been fully established—even for oral formulations. Previous preclinical studies have shown that when carbidopa is continuously delivered subcutaneously, levodopa pharmacokinetics are improved as compared to oral carbidopa administration (35). In part, this may be because there is evidence for inconsistent uptake of oral carbidopa from the gastrointestinal tract. This inconsistency could add to the variability of oral levodopa effect (36). In Study 005 (conducted in 20 healthy volunteers), the concentration of SC infused carbidopa that achieved optimal levodopa bioavailability was found to be 7.5 mg/ml when co-administered with SC levodopa at 60 mg/ml. In other studies, higher carbidopa concentrations did not increase bioavailability of levodopa, though lower concentrations of carbidopa when administered at the “low” infusion rates were found to compromise the levodopa levels—probably due to insufficient inhibition of the DDC enzyme. Thus, taken together, the data generated in this series of investigations found that a levodopa/carbidopa dose ratio of 1:8 would be the most reasonable choice for proceeding with ND0612 in Phase III clinical trials. The choice of the solubilized constituents in ND0612 is now fixed as carbidopa 7.5 mg/ml together with levodopa 60 mg/ml.
The studies presented here also explored augmenting the SC administration of ND0612 with oral levodopa/carbidopa, administered either alone or in combination with the COMT inhibitor entacapone. The supplemental use of these oral drugs produced expected effects on plasma levodopa concentrations and suggested ways that ND0612 could be used in future clinical applications. These results indicate that oral levodopa/carbidopa (with or without a COMT inhibitor) might be a way to lessen the quantity of drug that would otherwise need to be delivered subcutaneously to achieve therapeutic concentrations of carbidopa and levodopa. This ability to predictably complement continuous SC levodopa/carbidopa infusion with oral drugs is likely to provide patients with the flexibility in dosing to optimize their pharmacotherapy (and without the need to rely on full-replacement SC levodopa/carbidopa monotherapy in order to obtain the pharmacokinetic benefits of continuous SC levodopa/carbidopa therapy). The ongoing BouNDless study (NCT04006210) starts with a “conversion period” in which each patient's ND0612 treatment is optimized with supplemental oral levodopa/carbidopa as necessary. Changes to other antiparkinsonian medications are not permitted during all periods of the study.
We have described a series of early development pharmacokinetic studies, which served as a “learning curve” for understanding the peripheral pharmacokinetics of subcutaneously delivered levodopa/carbidopa. At each stage of the program, lessons were learned that impacted subsequent planning and choice of study designs. As such, the studies share the usual early development limitations of being relatively small in size and duration. A population pharmacokinetic model, including data from these studies and additional clinical trials with pharmacokinetic data analyses, is in development. Participants in these studies were predominantly White Caucasians. A pharmacokinetic study in Japanese subjects has already been initiated. Most of the studies tested abdominal infusion placement, whereas in real-world applications, patients will require rotation of sites due to the development of transient infusion site reactions and some will use infusion sites on other areas of the body with significant SC tissue. Recent results from a study comparing the results of abdominal ND0612 infusion with sites in the lower back and thighs confirm bioequivalence from infusion at different sites (35) and peer reviewed data will be published separately. While all the studies included safety observations, the studies were too short to be of relevance and the 1-year ND0612 safety data recently reported by Poewe et al. (37) are much more informative. We note that the low dosing regimens in the very earliest clinical development studies were originally investigated to understand the feasibility of small “patch pumps” in a less severe patient population. Ultimately, it was decided to prioritize the development of the “high” dosing regimen (up to 720/90 mg/day) infused over 16 and/or 24 h because of the significant unmet needs of patients with poorly controlled motor fluctuations. Therefore, this is the chosen treatment regimen under investigation in ongoing clinical trials (37, 38). While it could be argued that a key limitation of the development program is the lack of information on the pharmacokinetics of ND0612 monotherapy in patients with PD, it is pertinent to note that ND0612 is not being developed as a “complete” dopamine replacement therapy because patients with motor fluctuations typically require relatively high levodopa doses which would be impractical to deliver as a subcutaneous infusion therapy due to skin tolerability. Rather, ND0612 is intended as the next evolution in levodopa delivery for patients with Parkinson's disease. Future studies may continue the development of lower dose ND0612 regimens for patients who require less levodopa, potentially, with small patch-pump style devices.
In summary, ND0612 is under development as a minimally invasive drug-device combination to provide continuous subcutaneous delivery of levodopa/carbidopa for patients with PD experiencing motor fluctuations. Taken together, this series of clinical pharmacokinetic investigations have demonstrated that ND0612, administered continuously with a levodopa concentration of 60 mg/ml together with carbidopa 7.5 mg/ml, and complemented with oral levodopa/carbidopa, is suitable for administration for up to 24 h in patients with PD. This formulation has been shown to be generally safe and well-tolerated in an open-label, 12-month study of over 200 patients with PD (37) and we await the results of the ongoing Phase III study which will establish whether the favorable pharmacokinetic profile of ND0612 translates into clinical efficacy.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Institutional Review Boards at the participating sites approved the study protocol, consent forms, and associated amendments. The patients/participants provided their written informed consent to participate in this study.
PL, FS, DA, YC, and NG were investigators involved in the early ND0612 clinical development program. IP provided pharmacokinetic analysis of the concentration-time data and interpretation of results. LA was involved in trial coordination and interpretation of results. PL, LA, and RC contributed to the first draft equally. All authors provided critical review of the manuscript and approved the final version of the article.
The authors thank all participants in the early clinical development program, as well as the investigators and research staff in participating institutions. We also thank Michelle Dasse, PhD for providing QC of the data and Anita Chadha-Patel, PhD, of ACP Clinical Communications Ltd. (Hertfordshire, UK) for providing medical writing support, which was funded by NeuroDerm (Rehovot, Israel) in accordance with Good Publication Practice guidelines.
Author PL reports advisory roles for Abide, Acorda Therapeutics, Adamas, Biogen, Cavion, Denali, Intec Pharma, Jazz Pharmaceuticals, Lundbeck, Neurocrine, Mitsubishi NeuroDerm Ltd., Prexton, Revance, Sage, and US WorldMeds; lecture fees from US WorldMeds, Acorda, American Academy of Neurology, and Kyowa Hakko Kirin. Research grant support from Abide, Acorda, Amneal, Lundbeck, Michael J. Fox Foundation for Parkinson's Research, Mitsubishi NeuroDerm Ltd., Parkinson Study Group; National Institute of Neurological Disorders and Stroke, Pharma 2B, Revance, Hoffmann-La Roche; Sunovion, and Sun Pharma. Author FS reports honoraria and consulting fees from Britannia Pharmaceuticals, GlaxoSmithKline, Boehringer Ingelheim, Lundbeck, Orion, NeuroDerm, Novartis, Teva, Pfizer and Zambon. Authors YC and IP report consultancy for NeuroDerm. Authors LA and RC are employed by NeuroDerm. Author NG serves as consultant to Sionara, NeuroDerm, Pharma2B, Denali, Neuron23 and Abbvie, Sanofi-Genzyme and Biogen. He receives royalties from Lysosomal Therapeutics (LTI) and payment for lectures at Abbvie, Sanofi-Genzyme and Movement Disorder Society. He received research support from the Michael J. Fox Foundation, the National Parkinson Foundation, the European Union and the Israel Science Foundation as well as from Teva NNE program, Biogen and Ionis. He receives support from the Sieratzki Family Foundation and the Aufzien Academic Center in Tel-Aviv University.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.1036068/full#supplementary-material
2. LeWitt PA. Levodopa for the treatment of Parkinson's disease. N Engl J Med. (2008) 359:2468–76. doi: 10.1056/NEJMct0800326
3. Hatano T, Kubo S-I, Shimo Y, Nishioka K, Hattori N. Unmet needs of patients with Parkinson's disease: interview survey of patients and caregivers. J Int Med Res. (2009) 37:717–26. doi: 10.1177/147323000903700315
4. García-Ruiz PJ, Del Val J, Fernández IM. Herranz A. What factors influence motor complications in Parkinson disease?: a 10-year prospective study. Clin Neuropharmacol. (2012) 35:1–5. doi: 10.1097/WNF.0b013e31823dec73
5. Anderson E, Nutt J. The long-duration response to levodopa: phenomenology, potential mechanisms and clinical implications. Parkinsonism Relat Disord. (2011) 17:587–92. doi: 10.1016/j.parkreldis.2011.03.014
6. Aquino CC, Fox SH. Clinical spectrum of levodopa-induced complications. Mov Disord. (2015) 30:80–9. doi: 10.1002/mds.26125
7. Chapuis S, Ouchchane L, Metz O, Gerbaud L, Durif F. Impact of the motor complications of Parkinson's disease on the quality of life. Mov Disord. (2005) 20:224–30. doi: 10.1002/mds.20279
8. Kuhlman GD, Flanigan JL, Sperling SA, Barrett MJ. Predictors of health-related quality of life in Parkinson's disease. Parkinsonism Relat Disord. (2019) 65:86–90. doi: 10.1016/j.parkreldis.2019.05.009
9. Hechtner MC, Vogt T, Zollner Y, Schroder S, Sauer JB, Binder H, et al. Quality of life in Parkinson's disease patients with motor fluctuations and dyskinesias in five European countries. Parkinsonism Relat Disord. (2014) 20:969–74. doi: 10.1016/j.parkreldis.2014.06.001
10. Uebelacker LA, Epstein-Lubow G, Lewis T, Broughton MK, Friedman JH. A survey of Parkinson's disease patients: most bothersome symptoms and coping preferences. J Parkinson's Dis. (2014) 4:717–23. doi: 10.3233/JPD-140446
11. Stocchi F, Jenner P, Obeso JA. When do levodopa motor fluctuations first appear in Parkinson's disease? Eur Neurol. (2010) 63:257–66. doi: 10.1159/000300647
12. Foundation MJF. Capturing Elevating the Patient Voice. (2014). Available online at: https://www.Michaeljfox.Org/Foundation/News-Detail.Php?Capturing-and-Elevating-the-Patient-Voice (accessed September 1, 2022).
13. Aradi SD, Hauser RA. Medical management and prevention of motor complications in Parkinson's disease. Neurotherapeutics. (2020) 17:1339–65. doi: 10.1007/s13311-020-00889-4
14. Stocchi F, Vacca L, Ruggieri S, Olanow CW. Intermittent Vs continuous levodopa administration in patients with advanced Parkinson disease: a clinical and pharmacokinetic study. Arch Neurol. (2005) 62:905–10. doi: 10.1001/archneur.62.6.905
15. Doi H, Sakakibara R, Sato M, Masaka T, Kishi M, Tateno A, et al. Plasma levodopa peak delay and impaired gastric emptying in Parkinson's disease. J Neurol Sci. (2012) 319:86–8. doi: 10.1016/j.jns.2012.05.010
16. Fasano A, Visanji NP, Liu LW, Lang AE, Pfeiffer RF. Gastrointestinal dysfunction in Parkinson's disease. Lancet Neurol. (2015) 14:625–39. doi: 10.1016/S1474-4422(15)00007-1
17. Woitalla D, Goetze O. Treatment approaches of gastrointestinal dysfunction in Parkinson's disease, therapeutical options and future perspectives. J Neurol Sci. (2011) 310:152–8. doi: 10.1016/j.jns.2011.06.050
18. Mukherjee A, Biswas A, Das SK. Gut dysfunction in Parkinson's disease. World J Gastroenterol. (2016) 22:5742–52. doi: 10.3748/wjg.v22.i25.5742
19. Valenzuela JE, Defilippi C, Diaz G, Navia E, Merino Y. Effect of dopamine on human gastric and pancreatic secretion. Gastroenterology. (1979) 76:323–6. doi: 10.1016/0016-5085(79)90340-8
20. Djaldetti R, Baron J, Ziv I, Melamed E. Gastric emptying in Parkinson's disease: patients with and without response fluctuations. Neurology. (1996) 46:1051–4. doi: 10.1212/WNL.46.4.1051
21. Stowe R, Ives N, Clarke CE, Handley K, Furmston A, Deane K, et al. Meta-analysis of the comparative efficacy and safety of adjuvant treatment to levodopa in later Parkinson's disease. Mov Disord. (2011) 26:587–98. doi: 10.1002/mds.23517
22. Binde CD, Tvete IF, Gasemyr J, Natvig B, Klemp M. A multiple treatment comparison meta-analysis of monoamine oxidase type B inhibitors for Parkinson's disease. Br J Clin Pharmacol. (2018) 84:1917–27. doi: 10.1111/bcp.13651
23. Talati R, Reinhart K, Baker W, White CM, Coleman CI. Pharmacologic treatment of advanced Parkinson's disease: a meta-analysis of comt inhibitors and mao-B inhibitors. Parkinsonism Relat Disord. (2009) 15:500–5. doi: 10.1016/j.parkreldis.2008.12.007
24. Larson D, Simuni T. New dopaminergic therapies for Pd motor complications. Neuropharmacology. (2022) 204:108869. doi: 10.1016/j.neuropharm.2021.108869
25. Urso D, Chaudhuri KR, Qamar MA, Jenner P. Improving the delivery of levodopa in Parkinson's disease: a review of approved and emerging therapies. CNS Drugs. (2020) 34:1149–63. doi: 10.1007/s40263-020-00769-7
26. Stocchi F, Olanow CW. Continuous dopaminergic stimulation in early and advanced Parkinson's disease. Neurology. (2004) 62(Suppl. 1):S56–63. doi: 10.1212/WNL.62.1_suppl_1.S56
27. Nyholm D, Nilsson Remahl AI, Dizdar N, Constantinescu R, Holmberg B, Jansson R, et al. Duodenal levodopa infusion monotherapy vs oral polypharmacy in advanced Parkinson disease. Neurology. (2005) 64:216–23. doi: 10.1212/01.WNL.0000149637.70961.4C
28. Olanow CW, Kieburtz K, Odin P, Espay AJ, Standaert DG, Fernandez HH, et al. Continuous intrajejunal infusion of levodopa-carbidopa intestinal gel for patients with advanced Parkinson's disease: a randomised, controlled, double-blind, double-dummy study. Lancet Neurol. (2014) 13:141–9. doi: 10.1016/S1474-4422(13)70293-X
29. Volkmann J, Albanese A, Antonini A, Chaudhuri KR, Clarke CE, de Bie RM, et al. Selecting deep brain stimulation or infusion therapies in advanced Parkinson's disease: an evidence-based review. J Neurol. (2013) 260:2701–14. doi: 10.1007/s00415-012-6798-6
30. Antonini A, Stoessl AJ, Kleinman LS, Skalicky AM, Marshall TS, Sail KR, et al. Developing consensus among movement disorder specialists on clinical indicators for identification and management of advanced Parkinson's disease: a multi-country delphi-panel approach. Curr Med Res Opin. (2018) 34:2063–73. doi: 10.1080/03007995.2018.1502165
31. LeWitt PA, Jennings D, Lyons KE, Pahwa R, Rabinowicz AL, Wang J, et al. Pharmacokinetic-pharmacodynamic crossover comparison of two levodopa extension strategies. Mov Disord. (2009) 24:1319–24. doi: 10.1002/mds.22587
32. Giladi N, Gurevich T, Djaldetti R, Adar L, Case R, Leibman-Barak S, et al. Nd0612 (Levodopa/Carbidopa for Subcutaneous Infusion) in patients with Parkinson's disease and motor response fluctuations: a randomized, placebo-controlled phase 2 study. Parkinsonism Relat Disord. (2021) 91:139–45. doi: 10.1016/j.parkreldis.2021.09.024
33. Contin M, Riva R, Martinelli P, Cortelli P, Albani F, Baruzzi A. Concentration-effect relationship of levodopa-benserazide dispersible formulation versus standard form in the treatment of complicated motor response fluctuations in Parkinson's disease. Clin Neuropharmacol. (1999) 22:351–5.
34. Contin M, Martinelli P. Pharmacokinetics of levodopa. J Neurol. (2010) 257:S253–61. doi: 10.1007/s00415-010-5728-8
35. Shaltiel-Karyo R, Caraco Y, Zawaznik E, Weinstock I, Nemas M, Oren S, et al. Subcutaneous administration of carbidopa enhances oral levodopa pharmacokinetics: a series of studies conducted in pigs, mice, and healthy volunteers. Clin Neuropharmacol. (2019) 42:111–6. doi: 10.1097/WNF.0000000000000345
36. Hauser RA, Ellenbogen A, Khanna S, Gupta S, Modi NB. Onset and duration of effect of extended-release carbidopa-levodopa in advanced Parkinson's disease. Neuropsychiatr Dis Treat. (2018) 14:839–45. doi: 10.2147/NDT.S153321
37. Poewe W, Stocchi F, Arkadir D, Ebersbach G, Ellenbogen AL, Giladi N, et al. Subcutaneous levodopa infusion for Parkinson's disease: 1-year data from the open-label beyond study. Mov Disord. (2021) 36:2687–92. doi: 10.1002/mds.28758
38. Espay A, Rascol O, Yardeni T, Adar L, Rosenfeld O, Case R, et al. The boundless study: an active-controlled, randomized, double-blind, double-dummy phase 3 study of continuous nd0612 infusion in patients with parkinson's disease experiencing motor fluctuations (4474). Neurology. (2020) 94(Supple. 15):4474. doi: 10.1016/j.parkreldis.2020.06.209
Keywords: carbidopa, clinical development, levodopa, ND0612, Parkinson's disease, pharmacokinetics
Citation: LeWitt PA, Stocchi F, Arkadir D, Caraco Y, Adar L, Perlstein I, Case R and Giladi N (2022) The pharmacokinetics of continuous subcutaneous levodopa/carbidopa infusion: Findings from the ND0612 clinical development program. Front. Neurol. 13:1036068. doi: 10.3389/fneur.2022.1036068
Received: 03 September 2022; Accepted: 24 October 2022;
Published: 10 November 2022.
Edited by:
Margherita Fabbri, INSERM CIC1436 Centre d'Investigation Clinique de Toulouse, FranceReviewed by:
Antonio Suppa, Sapienza University of Rome, ItalyCopyright © 2022 LeWitt, Stocchi, Arkadir, Caraco, Adar, Perlstein, Case and Giladi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peter A. LeWitt, YWExMTQyQHdheW5lLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.