
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 31 January 2022
Sec. Stroke
Volume 12 - 2021 | https://doi.org/10.3389/fneur.2021.822342
 Ning Chen1
Ning Chen1 Xintong Wu1
Xintong Wu1 Muke Zhou1
Muke Zhou1 Rongdong Yang2
Rongdong Yang2 Daofeng Chen3
Daofeng Chen3 Ming Liao4
Ming Liao4 Yongyi Deng5
Yongyi Deng5 Zhen Hong1
Zhen Hong1 Dong Zhou1*
Dong Zhou1* Li He1*
Li He1*Background: Intravenous thrombolysis is still underutilized in patients with acute ischemic stroke (AIS) in China. A promising strategy for addressing this issue, especially in situations, such as the global pandemic of coronavirus disease 2019 (COVID-19), is the telestroke mode, which remains to be widely implemented in China. The present study aimed to assess the effects of telemedicine for patients with stroke in Western China, as well as the impact of the pandemic on telestroke services in 1 year after the COVID-19 outbreak.
Methods: In this 2-year multicenter observational study, we retrospectively collected data from 10 hospitals within the Sichuan Telestroke and Telethrombolysis Network. Demographic and clinical characteristics of patients with IS and those relevant to thrombolysis were compared between the pre-telestroke and post-telestroke phases, and between the periods before and after declaration of the COVID-19 pandemic.
Results: A total of 11,449 admissions with a primary diagnosis of IS were recorded during the study period. Prior to telestroke implementation, 6.7% of patients (n = 367) received intravenous thrombolysis, and the proportion increased to 7.4% (n = 443; p = 0.084) in the post-telestroke phase. The thrombolysis rate was 7.4% during the COVID-19 pandemic and in the latter half of the year when the viral spread was better controlled in China. The mean door-to-needle time (DNT) was significantly shorter after implementation of the telestroke network (63.76 ± 13.50 vs. 52.66 ± 25.49 min; p < 0.001).
Conclusions: Telemedicine is effective in improving the thrombolysis administration among patients with IS in Western China. Implementation of the telestroke network should be promoted, especially when access to care is affected by public health emergencies, such as the COVID-19 pandemic.
Stroke is the third leading cause of global disease burden (1) and the leading cause of death in China (2). Ischemic stroke (IS) accounts for ~60–80% of all stroke cases (2, 3). Intravenous thrombolysis remains a standard hyperacute therapy for IS (4), but it is still underused in China. Less than 3% of patients received such treatment, a rate much lower than that in high-income countries (2). Although the patients arrived within 3.5 h after initial symptom onset, only 24.2% were treated with intravenous recombinant tissue plasminogen activator (rtPA) within 4.5 h (5). Due to the diversity of medical resources and regional economies, stroke control is still a major challenge in China (6). Arriving at rural, non-teaching hospitals without stroke centers is one of the most important factors limiting the use of acute treatments (7). Telemedicine is one way to address this issue. Indeed, telemedicine has been approved as an effective and safe for decision-making regarding thrombolysis and has been widely recommended worldwide (8).
Situations, such as the global pandemic of coronavirus disease 2019 (COVID-19), when social distancing has been implemented to contain the spread of the virus, further emphasize the benefits of telemedicine (9). However, a report from the Mayo Clinic indicated that there was a substantial decrease in telestroke activations after the WHO declared COVID-19 a pandemic. As the observation period of the study was short (30 days preceding to 30 days following the declaration), the causes of this reduction remain unclear (10).
Therefore, the present study aimed to assess the effects of telemedicine implementation for patients with stroke in Western China, and to analyze the impact of the pandemic on telestroke services in 1 year after the COVID-19 outbreak.
In this 2-year multicenter observational study, we retrospectively reviewed and collected consecutive admissions of patients with a primary diagnosis of acute ischemic stroke (AIS) between January 2019 and December 2020 treated at 10 hospitals within the Sichuan telestroke and telethrombolysis network. AIS was defined in accordance with the WHO criteria (11, 12) or the Chinese guidelines for the clinical management of ischemic cerebrovascular diseases (13). The ethics committee of West China Hospital, Sichuan University approved the study [No.2021 (1723)], and waived the need for obtaining patient informed consent, since all data were retrospectively collected and individual information were not disclosed.
The Sichuan telestroke and telethrombolysis network was established at the end of 2019, with support from the Sichuan Provincial Department of Science and Technology. This initiative aims to improve the use of intravenous thrombolysis in appropriate cases of AIS and to optimize the comprehensive stroke prevention and treatment in Sichuan province. It synergized roles of 4G/5G network, computer and smartphone applications, and the telestroke technology, based on the domestic and global evidence and experiences of telemedicine (9, 10, 14, 15). During the study period, this pilot network was composed of one academic hub center (West China Hospital of Sichuan University) and nine telemedically connected spoke hospitals located throughout the Sichuan Province in Western China (Figure 1). The mean distance between a spoke hospital and the hub is 270.6 km (range: 59–443 km). Using this network, telemedicine consultation for any candidate with possible AIS in each spoke hospital was instantly available 24 h per day and 7 days a week. Once the telestroke network was activated, the stroke experts in the hub center were able to view real-time images and data of each patient, and to supervise and guide local clinicians in spoke hospitals to do physical and neurological examinations and further assess the eligibility of patients for thrombolysis. Clinical information was recorded by each hospital and collected online. Online training sessions for the management of acute stroke were conducted regularly, to improve the professional level of local physicians in the management of stroke.
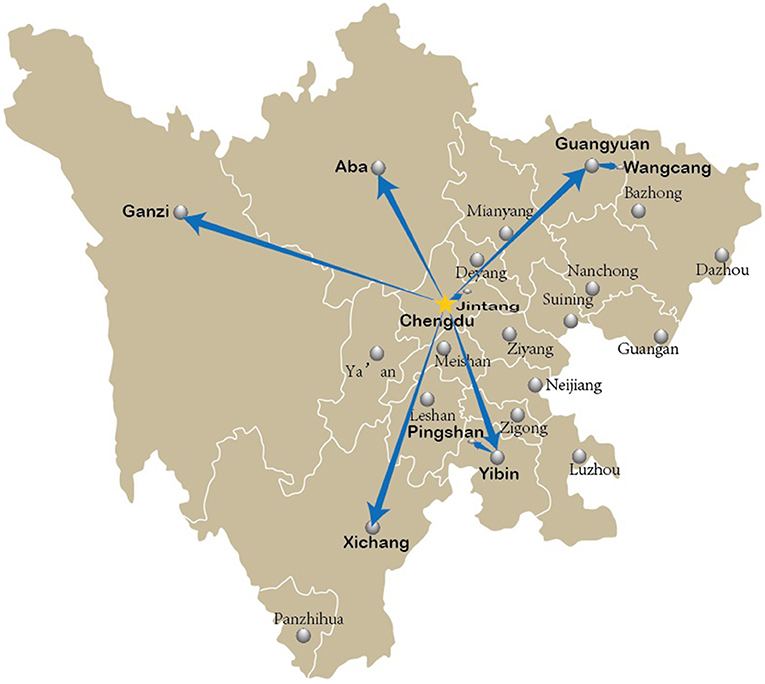
Figure 1. The pilot Telestroke and Telethrombolysis Network of Sichuan Province, China. West China Hospital of Sichuan University in Chengdu, the provincial capital, was designated as the hub center (golden star), and the network currently covers nine spoke hospitals (in boldface; two institutions in Pingshan, and one in each other region) around Sichuan.
The study period was divided into two phases: the pre-telestroke phase (January–December 2019) and the post-telestroke phase (January–December 2020). Although the COVID-19 outbreak occurred in China at the beginning of 2020, the program continued to operate since most of the work could be conducted online after the establishment of the spoke network. To explore the impact of the COVID-19 pandemic on telestroke implementation, we further divided the post-telestroke study period into two phases: the first half of the year 2020 and the latter half, during which the epidemic was well-controlled in China. Post-hoc analysis was performed between the two phases.
Statistical analysis was performed using SPSS version 25 (IBM Corp., Armonk, NY, USA). Continuous variables are presented as the mean ± SD, while categorical variables are presented as frequencies and percentages. Differences between groups were assessed using the t-test for continuous variables and the chi-square test for categorical variables. Statistical tests were two-tailed, and a p < 0.05 was considered to be statistically significant in all analyses.
During the 2-year study period, a total of 11,449 admissions with a primary diagnosis of IS were recorded from all 10 hospitals. There was a slight increase in the total number of patients with IS from 2019 to 2020 (5,466 and 5,983 cases, respectively), and there was no significant difference in the mean number of cases occurring in each month. Approximately 60.5% of the patients were men, and the mean age and sex distribution were comparable between the study phases (Table 1).
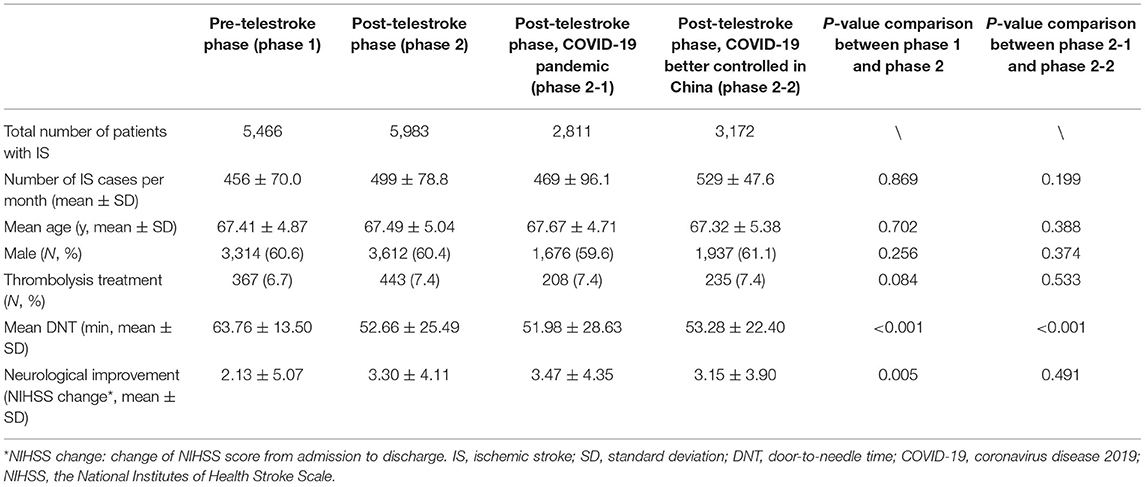
Table 1. Characteristics of patients with ischemic stroke (IS) and those receiving intravenous thrombolysis.
During the pre-telestroke phase, 6.7% of patients (n = 367) underwent intravenous thrombolysis, and the rate increased to 7.4% (n = 443) in the post-telestroke phase, although the difference between the two phases was not significant (p = 0.084). The thrombolysis rate was the same 7.4% during the COVID-19 pandemic and in the latter half of the year when the viral spread was better controlled in China. The mean door-to-needle time (DNT) was 63.76 ± 13.50 min among all patients who received thrombolytic treatment in the pre-telestroke phase. After the establishment and implementation of the telestroke network, the mean DNT was significantly decreased to 52.66 ± 25.49 min in all participating institutions (p < 0.001). The procedure seemed to be faster during the COVID-19 pandemic phase than during the better-controlled phase (51.98 ± 28.63 vs. 53.28 ± 22.40 min, p < 0.001) (Table 1). The short-term neurological improvement was evaluated by the change of National Institutes of Health Stroke Scale (NIHSS) score (16) from admission to discharge of each patient treated with intravenous rtPA. The NIHSS score decreased 2.13 ± 5.07 after treatment in the pre-telestroke phase, and a significantly better improvement was shown in the post-telestroke phase (NIHSS decreased 3.30 ± 4.11, p = 0.005) (Table 1).
We further compared thrombolysis rates between the hub center and the spoke hospitals. Figure 2 presents the comparisons and changes across the three phases. During the pre-telestroke phase, the monthly thrombolysis rate at West China Hospital was 8.0 ± 2.2%, while it was only 6.1 ± 1.5% in the other nine spoke hospitals (p = 0.174). In 2020, after the implementation of telestroke network in Sichuan, the thrombolysis rate in the spoke hospitals increased to 8.2 ± 1.8%, however, it decreased to 6.2 ± 3.3% in the hub center (p = 0.237). The proportions were similar for the two halves of 2020, and there were no significant differences between groups of hospitals (Figure 2).
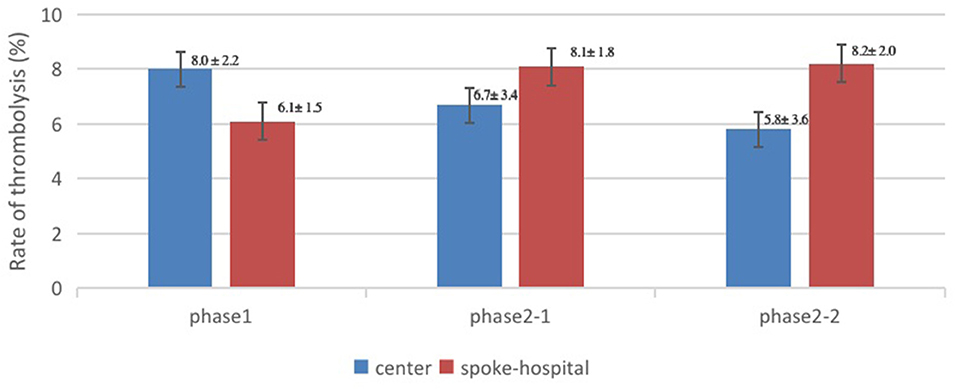
Figure 2. Comparisons of the thrombolysis rate between the hub center and spoke hospitals. Phase 1, pre-telestroke phase (January–December 2019); phase 2-1, post-telestroke phase during coronavirus disease 2019 (COVID-19) pandemic in China (January–June 2020); phase 2-2, post-telestroke phase, COVID-19 epidemic better controlled in China (July–December 2020).
In this study, we assessed the impact of telestroke implementation on the frequency and efficiency of thrombolysis treatment in patients with AIS in Sichuan Province, China. Our results indicated that the rate of intravenous thrombolysis increased after telestroke implementation, especially in the network spoke hospitals. Furthermore, the efficiency of treatment and neurological function improved significantly after the implementation of telestroke.
These findings are consistent with those of previous studies that have reported significant improvements in thrombolytic therapy after the implementation of telemedicine networks in other countries and territories (14, 17–19). Previous studies and systematic reviews have already verified the safety, efficacy, and reliability of intravenous rtPA delivery through telestroke networks (15); therefore, international guidelines for stroke recommend the use of telemedicine (8, 20). Our results support the promotion of such guidelines in Western China. Although the increase of intravenous thrombolysis rate was insignificant in this pilot study, there was an upward trend and an obvious improvement in the time efficiency, which is a key element for the early management of patients with AIS (8). In actual, the insignificance of thrombolysis increase might be mainly attributed to the data change in the hub center, which decreased after initiation of the telestroke program. This may be because West China Hospital is located in the city center of Chengdu, the capital of Sichuan province, and has the heaviest traffic conditions. Therefore, a relatively small number of patients with potential AIS can arrive within the 4.5-h time window. Instead, a number of patients only received thrombectomy in this tertiary medical center: some of them arrived beyond the 4.5-h window or had contraindications to thrombolysis, while others were transferred from other hospitals to receive the bridging therapy after intravenous rtPA. The rate of thrombectomy among all patients with AIS in West China Hospital was 9.3% (156/1,684) during the year 2020, an increase from the rate of 7.9% (149/1,891) in 2019. With new evidence regarding the benefit of endovascular thrombectomy alone in patients with AIS from large-vessel occlusion (21, 22), this rate may further increase in such central hospitals. Therefore, in the development and improvement of telestroke networks, attention should be directed toward consultations for the potential thrombectomy or bridging therapy and to the optimization of the transport process among hospitals.
We further assessed the impact of the COVID-19 pandemic on this newly established telemedicine network and found that operation of the system was hardly affected during this special circumstance. A slight growth in the volume of patient admissions was observed 1 year after the COVID-19 outbreak. This result differs from those reported in some prior studies, which noted obvious reductions in stroke admissions and a more than 25% drop in thrombolysis and thrombectomy procedures (23, 24). The Mayo Clinic reported a 50% reduction in total telemedicine activations for potential cases of stroke between 1 month before and 1 month after the declaration of the COVID-19 pandemic by the WHO (10). The main reason for this difference may be our relatively longer study period. We collected data for the full year after the COVID-19 outbreak. Importantly, in the latter half of the year, the epidemic has been better controlled across the country. The numbers of cumulative confirmed cases of COVID-19 in China were 83,534 and 3,537 in the first and second halves of the year, respectively. Among these, 595 and 258 cases occurred in Sichuan Province (data from the official website of the National Health Commission of China). We indeed observed a drop in stroke admissions in the first month of 2020 in our study, as several strict measures were implemented to contain the spread of the virus, which may have affected the rate of hospital visits. However, a stroke is a severe acute disease that must be given priority in the consultation and treatment. Following control of the epidemic in China, especially with the resumption of work and restoration of transportation, the total number of IS admissions rapidly increased and remained relatively stable. This increase is consistent with the trend of stroke incidence and prevalence in China in recent years (2, 5, 6). Furthermore, three spoke hospitals (located in Wangcang, Pingshan, and Ganzi) began to administer intravenous thrombolytic treatment for potential cases of AIS as the telestroke program progressed. These hospitals have thus received and cured more patients with stroke since the end of 2019.
Our findings showed higher rates of intravenous thrombolysis after implementation of the telestroke network, especially in the spoke hospitals. Sichuan Province, located in the southwest of China, covers an area of 485,000 km2 and has a population of more than 88 million. It is reputed as “a land of abundance,” but it is among the regions with the highest mortality-to-incidence ratio among patients with stroke in China (2, 3). Healthcare resources are relatively deficient in Western China, and highly qualified doctors and advanced technologies are often unavailable or severely lacking in rural and remote regions (9). Such imbalanced distribution of medical resources is present in several other regions of China (2). The long distance required for transfer to specialized centers may be the most important barriers to appropriate acute treatment, such as intravenous thrombolysis (7). Our present telestroke and telemedicine network includes regions throughout Sichuan in all directions, especially in areas with poor economic status (Figure 1). A convenient and effective medicine network can bring neurological expertise to the patient instead of requiring transfer of the patient to advanced hospitals, which can save time from symptom onset to the initiation of treatment. This telestroke treatment mode might be replicated and promoted in other regions with deficiency of medical resources. Online consultation and training can increase the knowledge and availability of a practitioner, allowing more patients to receive immediate, quality care close to home.
In the context of a pandemic or other public health emergency, telemedicine is advantageous given its ability to provide long-distance medical care and relieve local pressure (25). In our study, the rate of thrombolysis in patients with stroke was similar between the relatively severe phase and better-controlled phase of the COVID-19 epidemic, highlighting the stability of the telestroke network during the pandemic. Interestingly, the mean DNT was much shorter during the COVID-19 pandemic phase, possibly due to lower total patient volume in most hospitals and smoother access to investigations and treatments. However, the epidemic has not been resolved yet, meaning that the present data cannot perfectly capture the impact of COVID-19 on the implementation of the telestroke program in Sichuan. Our group will further collect and analyze relevant data following resolution of the pandemic.
Our study had some limitations. First, the data were retrospectively collected and reported by each hospital based on their clinical practice, so the quality of assessment and treatment may have varied among hospitals. Second, since some hospitals in the network had no special department of neurology, there were some missing or incomplete records in these sites before implementation of the telestroke program. Such data deficiency may have resulted in overestimation of the thrombolysis rate in the pre-telestroke phase (when they had not yet administered thrombolysis therapy), while underestimating the advantages of the telestroke network. The database established for the Sichuan telestroke program will allow for the collection of additional data that can be used to accurately reflect the effects of telestroke implementation in Western China. Third, we did not perform crosswise comparisons in the present study, meaning that the influence of other factors on improvements in AIS management cannot be ruled out. Furthermore, because of the limited data, we could not calculate the rate of thrombolysis among patients arriving within the time window or identify the reasons why they had not received thrombolytic treatment; therefore, the present study was unable to clarify the specific advantages of the telestroke network for patients with stroke.
Despite these limitations, the results of the current study support the implementation and promotion of telemedicine for patients with stroke in Western China, especially in special circumstance, such as the COVID-19 pandemic.
Telemedicine is effective for improving the thrombolysis administration in patients with AIS in Western China. Implementation of the telestroke network should be promoted, especially when access to care is affected by public health emergencies, such as the COVID-19 pandemic.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
NC, XW, MZ, RY, DC, ML, YD, ZH, DZ, and LH: acquisition, analysis, or interpretation of data for the work, drafting the work or revising it critically for important intellectual content, and final approval of the version to be published. All authors contributed to the article and approved the submitted version.
The present study was supported by the Sichuan Science and Technology Program (2019YFH0196), the National Key Research and Development Program of China (2018YFC1311400), and the Project of Health Commission of Sichuan Province (19PJ048).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank Dr. Stefan Schwab, Dr. Lorenz Breuer, and Mr. Mateusz Scibor for counseling and guidance during the establishment and implementation of the telestroke network in Sichuan.
1. Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
2. Wu S, Wu B, Liu M, Chen Z, Wang W, Anderson CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. (2019) 18:394–405. doi: 10.1016/S1474-4422(18)30500-3
3. Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in china: results from a nationwide population-based survey of 480 687 adults. Circulation. (2017) 135:759–71. doi: 10.1161/CIRCULATIONAHA.116.025250
4. Phipps MS, Cronin CA. Management of acute ischemic stroke. BMJ. (2020) 368:l6983. doi: 10.1136/bmj.l6983
5. Wang YJ, Li ZX, Gu HQ, Zhai Y, Jiang Y, Zhao XQ, et al. China stroke statistics 2019: a report from the national center for healthcare quality management in neurological diseases, china national clinical research center for neurological diseases, the Chinese stroke association, national center for chronic and non-communicable disease control and prevention, Chinese center for disease control and prevention and institute for global neuroscience and stroke collaborations. Stroke Vasc Neurol. (2020) 5:211–39. doi: 10.1136/svn-2020-000457
6. Chao BH, Yan F, Hua Y, Liu JM, Yang Y, Ji XM, et al. Stroke prevention and control system in China: CSPPC-stroke program. Int J Stroke. (2021) 16:265–72. doi: 10.1177/1747493020913557
7. Messe SR, Khatri P, Reeves MJ, Smith EE, Saver JL, Bhatt DL, et al. Why are acute ischemic stroke patients not receiving IV tPA? Results from a national registry. Neurology. (2016) 87:1565–74. doi: 10.1212/WNL.0000000000003198
8. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. (2019) 50:e344–418. doi: 10.1161/STR.0000000000000211
9. Hong Z, Li N, Li D, Li J, Li B, Xiong W, et al. Telemedicine during the COVID-19 pandemic: experiences from western China. J Med Internet Res. (2020) 22:e19577. doi: 10.2196/19577
10. Huang JF, Greenway MRF, Nasr DM, Chukwudelunzu FE Sr., Demaerschalk BM, et al. Telestroke in the time of COVID-19: the mayo clinic experience. Mayo Clin Proc. (2020) 95:1704–8. doi: 10.1016/j.mayocp.2020.06.007
11. The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA project principal investigators. J Clin Epidemiol. (1988) 41:105–14. doi: 10.1016/0895-4356(88)90084-4
12. World Health Organization. ICD-11 for Mortality and Morbidity Statistics. 08 Diseases of the Nervous System. (2021). Available online at: https://icd.who.int/dev11/l-m/en (accessed November 17, 2021).
13. Liu L, Chen W, Zhou H, Duan W, Li S, Huo X, et al. Chinese stroke association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of ischaemic cerebrovascular diseases. Stroke Vasc Neurol. (2020) 5:159–76. doi: 10.1136/svn-2020-000378
14. Handschu R, Scibor M, Wacker A, Stark DR, Köhrmann M, Erbguth F, et al. Feasibility of certified quality management in a comprehensive stroke care network using telemedicine: STENO project. Int J Stroke. (2014) 9:1011–6. doi: 10.1111/ijs.12342
15. Kepplinger J, Barlinn K, Deckert S, Scheibe M, Bodechtel U, Schmitt J. Safety and efficacy of thrombolysis in telestroke: a systematic review and meta-analysis. Neurology. (2016) 87:1344–51 doi: 10.1212/WNL.0000000000003148
16. Brott T, Adams Jr HP, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. (1989) 20:864–70. doi: 10.1161/01.STR.20.7.864
17. Amorim E, Shih MM, Koehler SA, Massaro LL, Zaidi SF, Jumaa MA, et al. Impact of telemedicine implementation in thrombolytic use for acute ischemic stroke: the University of Pittsburgh Medical Center telestroke network experience. J Stroke Cerebrovasc Dis. (2013) 22:527–31. doi: 10.1016/j.jstrokecerebrovasdis.2013.02.004
18. Lopez-Cancio E, Ribo M, Cardona P, Serena J, Purroy F, Palomeras E, et al. Telestroke in catalonia: increasing thrombolysis rate and avoiding interhospital transfers. Cerebrovasc Dis. (2018) 46:66–71. doi: 10.1159/000492124
19. Muller-Barna P, Hubert GJ, Boy S, Bogdahn U, Wiedmann S, Heuschmann PU, et al. TeleStroke units serving as a model of care in rural areas: 10-year experience of the TeleMedical project for integrative stroke care. Stroke. (2014) 45:2739–44. doi: 10.1161/STROKEAHA.114.006141
20. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. (2018) 49:e46–110. doi: 10.1161/STR.0000000000000158
21. Zi W, Qiu Z, Li F, Sang H, Wu D, Luo W, et al. Effect of endovascular treatment alone vs. intravenous alteplase plus endovascular treatment on functional independence in patients with acute ischemic stroke: the DEVT randomized clinical trial. JAMA. (2021) 325:234–43. doi: 10.1001/jama.2020.23523
22. Yang P, Zhang Y, Zhang L, Zhang Y, Treurniet KM, Chen W, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med. (2020) 382:1981–93. doi: 10.1056/NEJMoa2001123
23. Leadership AASC. Temporary emergency guidance to US stroke centers during the coronavirus disease 2019 (COVID-19) pandemic: on behalf of the American heart association/American stroke association stroke council leadership. Stroke. (2020) 51:1910–2. doi: 10.1161/STROKEAHA.120.030023
24. Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. (2020) 51:1996–2001. doi: 10.1161/STROKEAHA.120.030225
Keywords: coronavirus, Covid-19, telemedicine, telestroke, stroke, thrombolysis
Citation: Chen N, Wu X, Zhou M, Yang R, Chen D, Liao M, Deng Y, Hong Z, Zhou D and He L (2022) Telestroke for the Treatment of Ischemic Stroke in Western China During the COVID-19 Pandemic: A Multicenter Observational Study. Front. Neurol. 12:822342. doi: 10.3389/fneur.2021.822342
Received: 25 November 2021; Accepted: 29 December 2021;
Published: 31 January 2022.
Edited by:
Christoph Gumbinger, Heidelberg University, GermanyReviewed by:
Tomaz Velnar, Maribor University Medical Centre, SloveniaCopyright © 2022 Chen, Wu, Zhou, Yang, Chen, Liao, Deng, Hong, Zhou and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dong Zhou, emhvdWRvbmc2NkB5YWhvby5kZQ==; Li He, aGVsaTIwMDNuZXdAMTI2LmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.