- 1Department of Neurology, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, China
- 2Department of Neurology, Dushu Lake Hospital Affiliated to Soochow University, Suzhou, China
Background and Purpose: Convulsive seizures related to posterior circulation stroke are considered rare. However, some patients with acute basilar artery occlusion (BAO) can present with convulsive movements. Misdiagnosed as seizures may delay the reperfusion therapy for acute BAO. In this study, we have summarized the clinical features and possible mechanisms of BAO presenting with convulsive movements.
Methods: We performed an Institutional Review Board-approved institutional database query from 2015 to 2020 and a literature search of the online database PubMed. Clinical data were collected and analyzed.
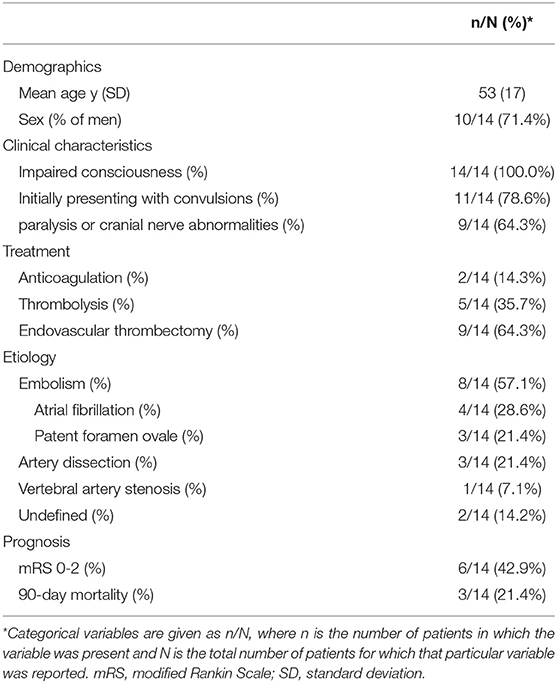
Results: In total, 14 patients with acute BAO presented with convulsions. There were 10 men and 4 women, with a mean age of 53 (range, 23–77) years. All of these patients had different degrees of impaired consciousness (100.0%, 14/14). Convulsive movements were the initial symptoms in 78.6% (11/14) of patients. Further, 64.3% (9/14) of patients presented with paralysis or cranial nerve abnormalities, and 85.7% (12/14) of patients were treated with reperfusion therapy (thrombolysis, 35.7% [5/14]; endovascular thrombectomy, 64.3% [9/14]). The BAO etiology and mechanism were related to embolism, vessel dissections, and severe stenosis of the right vertebral artery in 57.1% (8/14), 21.4% (3/14), and 7.1% (1/14) of patients, respectively; they were undefined in 14.3% (2/14) of patients. Moreover, 42.9% (6/14) of patients had a 90-day modified Rankin Scale score of 0–2, and the mortality rate was 21.4% (3/14).
Conclusions: Acute BAO, especially that related to embolism or vessel dissection, may present with convulsive movements. Acute BAO is a devastating, but treatable disease if diagnosed in time. Considering the possibility of BAO is important when dealing with patients presenting with acute-onset convulsive movements. Prompt diagnosis and reperfusion therapy may help achieve a better prognosis.
Introduction
Convulsive seizures can occur in acute ischemic stroke, with an incidence of approximately 5% (1). The risk factors include cortical involvement, multifocal areas of ischemia, anterior circulation or temporal lobe stroke, large infarct size, and ischemic-to-hemorrhagic transformation (1, 2). Generally, seizures occur mainly with cortical infarcts in the anterior circulation or supratentorial lesions; however, seizures related to a posterior circulation infarct are considered rare (3). Acute basilar artery occlusion (BAO) is a potentially fatal, but treatable disease. However, its diagnosis may be challenging due to the heterogeneity of symptoms and signs, especially when the presenting symptom is “seizures.” Occasionally, it may be misdiagnosed as a seizure with Todd's palsy, causing a delay in the treatment of ischemic stroke and leading to a poor prognosis. This study aimed to investigate the clinical characteristics and outcomes of acute BAO presenting with convulsive movements.
Methods
Data for all consecutive patients with BAO were collected from Sir Run Run Shaw Hospital, PR China between January 1, 2015, and September 1, 2020. This study was approved by the Institutional Review Board Committee, which waived the requirement of written informed consent due to the retrospective study design.
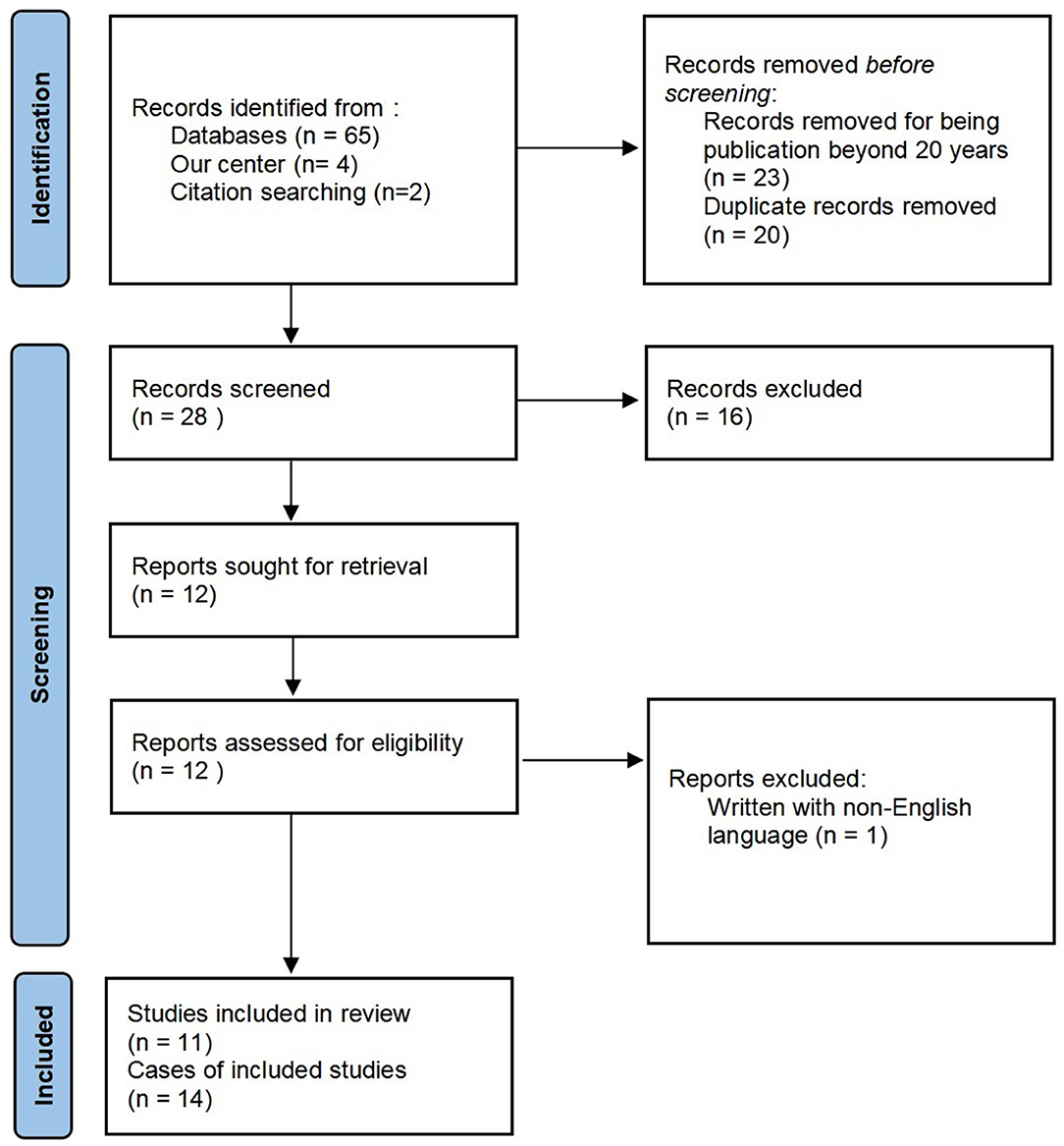
In addition, we performed a literature search of the online database PubMed in June 2021 using Endnote-web with the terms “basilar artery occlusion” combined with “seizure,” “convulsion,” “convulsive,” or “epilepsy.” The reference lists of the included articles were screened for additional relevant articles. Considering the development of neuroimaging technology and treatment options, only articles published in the past 20 years were included. Patients with angiography-proven acute BAO, initially presenting with convulsive movements, were included. Asymptomatic patients, patients with chronic BAO, and patients aged <18 years were excluded. Articles without full text available, written in languages other than English, or without sufficient clinical data were excluded. An adapted Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram is shown in Figure 1.
The full texts of potentially relevant articles were reviewed independently by two authors (DZ and YGC). The following information was extracted from each article: (1) age at onset, (2) sex, (3) initial symptoms and signs, (4) stroke risk factors and comorbidity, (5) infarct regions, (6) result of electroencephalogram (EEG), (7) reperfusion treatment, and (8) prognosis (Table 1).
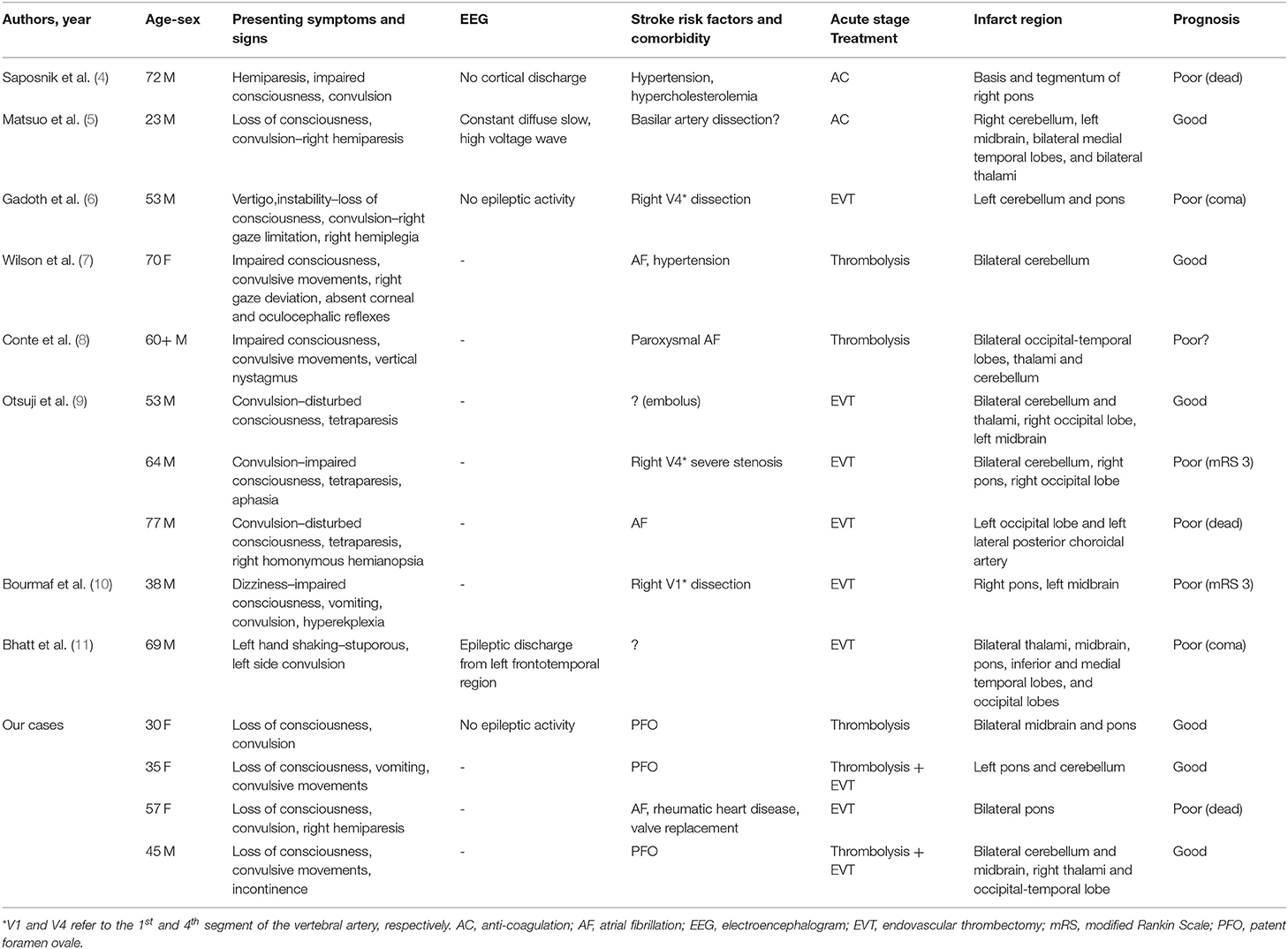
Table 1. Clinical data of 14 acute basilar artery occlusion patients presenting with a convulsive movement.
Results
Over the 5-year study period, 40 patients were diagnosed with BAO at our hospital, among which 28 had acute BAO with new-onset neurological symptoms and signs. Furthermore, 4 patients presented with convulsive movements.
The literature review yielded additional 10 cases of patients with acute BAO presenting with convulsions from eight reports (Table 1). There were 10 men and 4 women, with a mean age of 53 (range, 23–77) years (Table 2). All patients had different degrees of impaired consciousness (100%, 14/14). Further, 78.6% (11/14) of patients initially presented with convulsions or convulsive movements, and 64.3% (9/14) of patients presented with paralysis or cranial nerve abnormalities. However, some patients did not present with focal symptoms, signs, or clear laterality. Electroencephalogram (EEG) results were available for five patients, among which four patients displayed no epileptic activity, and one patient presented with epileptic discharge from the left frontotemporal region.
In terms of treatment in the hyper-acute stage, all patients, except two patients treated with anticoagulation, received reperfusion therapy (thrombolysis, 35.7% [5/14]; endovascular thrombectomy (EVT), 64.3% [9/14]). Among them, two patients underwent intravenous thrombolysis and bridging artery thrombectomy. Acute endovascular intervention treatment was performed in all patients after 2015. However, EVT was not successful because of a tortuous vertebral artery in one patient (8). In one patient from our center, a 30-year-old woman, digital subtraction angiography was performed after thrombolysis revealed recanalization of the basilar artery.
Regarding the etiology and mechanism of BAO, (1) 57.1% (8/14) of patients had embolism (atrial fibrillation, 28.6% [4/14]; patent foramen ovale, 21.4% [3/14]; unidentified source, 7.1% [1/14]) (9), (2) 21.4% (3/14) of patients had vessel dissections (vertebral artery dissection, 14.3% [2/14]; basilar artery dissection, 7.1% [1/14]), (3) 7.1% (1/14) of patients had basilar occlusion owing to severe right vertebral artery stenosis, and (4) 14.3% (2/14) of patients had an undefined etiology.
Furthermore, 42.9% (6/14) of patients had a 90-day modified Rankin Scale score of 0–2. The all-cause 90-day mortality rate was 21.4% (3/14).
Discussion
Acute basilar artery occlusion is responsible for approximately 1% of all ischemic strokes, with high rates of mortality and morbidity (12, 13). However, if recognized early, the prognosis may improve with reperfusion therapies such as intravenous thrombolysis and EVT (14, 15). However, in clinical practice, the heterogeneity of presenting symptoms and signs, ranging from a decreased level of consciousness, weakness, cranial nerve abnormalities, and tetraplegia/quadriplegia to locked-in syndrome, can make the diagnosis challenging (7, 16).
Involuntary movements of the limbs are occasionally seen in acute stroke, including fasciculation-like, shivering, jerky, intermittent shaking, and tonic-clonic activities (4). Cortical involvement is the best-characterized risk factor for early seizure after ischemic stroke, which is supported by studies with largely different designs (2, 17). However, seizures related to posterior circulation infarcts are considered rare. According to the cases in our study and the literature, patients with acute BAO may present with convulsions. Moreover, convulsions could even be the initial symptoms in some cases. Patients with acute BAO and pyramidal tract involvement may present with hemiparesis. However, palsy can occur after convulsive seizures, known as Todd's palsy. Therefore, when convulsions are present, especially when convulsion is the initial symptom, hemiparesis may be considered as Todd's palsy (5). This assumption may delay the diagnosis and treatment of acute BAO, and may directly affect prognosis (14, 18). Therefore, when dealing with patients with acute convulsions in the emergency department, the existence of sustained neurological signs should be evaluated. If possible, cranial computed tomography angiography should be performed to assess the possibility of stroke, especially acute BAO. This fatal condition may be treated if diagnosed in time.
The pathophysiology and mechanism of such convulsive movements in patients with posterior circulation stroke are unclear. Traditionally, when explaining the generation of seizures, the leading role is often given to the cerebral cortex. Nonetheless, Penfield et al. postulated a “centrencephalic system” to characterize a group of neurons located in the brainstem reticular formation that functioned as a pacemaker for seizures (4, 19, 20). In rat and cat models, stimulation of the reticular formation of the midbrain, pontine, or medulla results in tonic activity followed by short-lasting clonic jerks (4). However, this theory is still controversial. Other studies have proposed that the disruption of inhibitory projections from the cortex to the brainstem can result in decerebrate posturing (1, 21). These decerebrate spasms tend to be regarded as convulsive seizures. Ischemia of the descending pathways, including the corticospinal, vestibulospinal, and reticulospinal tracts, may be related (21, 22). Zhang et al. recorded epileptic discharges from the brainstem, but not from the hippocampus or cortex, even in middle cerebral artery occlusion induced convulsive seizures (1). Mader et al. reported a patient with bilateral paramedian thalamic infarcts and BAO, followed by paramedian midbrain infarcts 12 days later, who experienced seizures witnessed by caregivers and recorded by EEG (1). Such evidence suggests the role of the brainstem in generating convulsive movements or seizures. However, the posterior circulation also provides blood supply to the occipital and temporal lobes and thalamus. A study on seizures and epilepsy in patients with a posterior circulation infarct demonstrated that > 50% of patients with seizures had infarcts in the territory of the posterior cerebral artery, which supplies the medial surface of the occipital and temporal lobes (3). Therefore, ruling out the role of the occipital and temporal lobes or thalamus in generating such convulsive movements in BAO is difficult (5, 6, 8).
In animal models, stimulation of the brain stem produces tonic-clonic activities without concurrent cortical discharges classically recorded with cortical seizures on scalp EEG (23). The EEG results available in our study demonstrated no epileptic activity, except in one patient, showing epileptic discharge from the left frontotemporal region. This might, in part, be explained that postictal or interictal EEG could be normal in this scenario. Another explanation is that scalp EEG may not demonstrate electric activity from the brainstem or medial temporal lobe. In summary, it is still controversial whether these convulsive movements are seizures or seizure mimics.
In general, the most common mechanism of BAO is in situ atherosclerosis. However, most cases of acute BAO with convulsions on presentation were related to embolism or vascular dissection; they were rarely related to atherosclerosis. According to the results of some clinical and autopsy studies, seizures are more common with cardioembolic infarct than other subtypes of ischemic stroke; however, clinical data showing a clear relationship between embolism and seizures are lacking (17). Embolism or vascular dissection may cause sudden ischemia and subsequent pathophysiological changes to more brain structures without providing sufficient time for collateral circulation to compensate. Posterior circulation strokes caused by atherosclerosis may also present with convulsions (24).
Poor prognosis has been reported in > 80% of patients with acute BAO (12, 13). Since 2015, several large randomized clinical trials have demonstrated the safety and efficacy of EVT in large vessel occlusions in the anterior circulation. However, it is uncertain whether patients with large vessel occlusions in the posterior circulation would also benefit from EVT. Several studies have demonstrated improvement in mortality and disability rates in patients with acute BAO receiving endovascular treatment (14, 25, 26). However, the current data are insufficient for generating high-class evidence-based guidelines. EVT, especially combined with intravenous thrombolysis, if possible, seems to be the most effective therapy for the treatment of acute BAO. Studies have also suggested that EVT within the early therapeutic time window is associated with better functional outcomes and reduced mortality (14, 26). Therefore, in patients with acute BAO presenting with convulsive movements, prompt recognition and diagnosis are crucial.
The limitations of the present study include the restricted number of patients and the incomplete availability of clinical data for some patients. Only articles published in English during the last 20 years were included. EEG results were not available for most patients. In addition, it was unclear whether some available EEG results were ictal or postictal. Moreover, due to reperfusion therapies in the hyper-acute stage, the final stroke regions demonstrated in the following diffusion-weighted imaging may be inconsistent with ischemic regions during disease onset. Therefore, it is difficult to attribute the origin of the convulsion to the brainstem, thalami, or occipital and temporal lobes.
Conclusion
Acute BAO, especially that related to embolism or vessel dissection, can present with convulsive movements. The pathophysiology and underlying mechanisms are unclear. Therefore, defining this phenomenon as a seizure or seizure mimic is difficult. However, acute BAO is a devastating, but treatable disease. The possibility of acute BAO in patients with acute-onset convulsive movements should be considered.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
DZ collected relative data and drafted the manuscript. YC and YH helped with data collection and direct patient care. XHu and XHe revised the manuscript for intellectual content. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Health Commission of Zhejiang Province, Medical and Health Project (2021KY727), and Hangzhou Municipal Health Commission, Medical and Health Science Project (A20210510).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Dr. Qiaowei Zhang and Dr. Xiaojing Yu for their intellectual discussions.
References
1. Mader EC, Losada V, Baity JC, McKinnies EM, Branch LA. Stroke-onset seizures during midbrain infarction in a patient with top of the basilar syndrome. J Investig Med High Impact Case Rep. (2020) 8:2324709620940497. doi: 10.1177/2324709620940497
2. Doria JW. and Forgacs PB. Incidence, implications, and management of seizures following ischemic and hemorrhagic stroke. Curr Neurol Neurosci Rep. (2019) 19:37. doi: 10.1007/s11910-019-0957-4
3. De Reuck JL. and Van Maele G. Seizures and epilepsy in patients with a posterior circulation infarct. J Stroke Cerebrovasc Dis. (2012) 211:1–4. doi: 10.1016/j.jstrokecerebrovasdis.2010.03.012
4. Saposnik G. and Caplan LR. Convulsive-like movements in brainstem stroke. Arch Neurol. (2001) 58:654–7. doi: 10.1001/archneur.58.4.654
5. Matsuo K, Fujii C, Fuse I, Nakajima M, Takada M, Miyata K. Top of the basilar syndrome in a young adult initially presenting with a convulsive seizure. Intern Med. (2011) 50:1425–8. doi: 10.2169/internalmedicine.50.4801
6. Gadoth A, Hallevi H. Basilar artery occlusion presenting as a tonic-clonic seizure. Isr Med Assoc J. (2011) 13:314–5.
7. Wilson LK, Benavente OR, Woolfenden AR, Asdaghi N. Spontaneous limb movements and posturing secondary to acute basilar artery occlusion: a potentially devastating seizure mimic. Pract Neurol. (2014) 14:42–4. doi: 10.1136/practneurol-2013-000585
8. Conte WL, Gill CE, Biller J. Top of the basilar syndrome presenting with convulsions. JAMA Neurol. (2017) 74:248–9. doi: 10.1001/jamaneurol.2016.3449
9. Otsuji R, Uno J, Motoie R, Karashima S, Ren N, Nagaoka S, et al. Basilar artery occlusion with “Seizures” as a presenting symptom: three cases treated using mechanical thrombectomy. World Neurosurg. (2018) 117:32–9. doi: 10.1016/j.wneu.2018.05.227
10. Bourmaf M, Katyal R, Al-Awwad A. Top of basilar syndrome presenting with hyperekplexia initially diagnosed as a convulsive status epilepticus. J Emerg Med. (2020) 59:e53–6. doi: 10.1016/j.jemermed.2020.04.038
11. Bhatt SK, Dawit S, Okazaki EM, Noe KH. Refractory left focal motor status epilepticus as initial clinical presentation of acute basilar artery thrombosis. Mayo Clin Proc Innov Qual Outcomes. (2021) 5:511–5. doi: 10.1016/j.mayocpiqo.2020.12.002
12. Israeli-korn SD, Schwammenthal Y, Yonash-Kimchi T, Bakon M, Tsabari R, Orion D, et al. Ischemic stroke due to acute basilar artery occlusion: proportion and outcomes. Isr Med Assoc J. (2010) 12:671–5.
13. Schonewille WJ, Algra A, Serena J, Molina CA, Kappelle LJ. Outcome in patients with basilar artery occlusion treated conventionally. J Neurol Neurosurg Psychiatry. (2005) 76:1238–41. doi: 10.1136/jnnp.2004.049924
14. Uno J, Kameda K, Otsuji R, Ren N, Nagaoka S, Maeda K, et al. Mechanical thrombectomy for acute basilar artery occlusion in early therapeutic time window. Cerebrovasc Dis. (2017) 44:217–24. doi: 10.1159/000479939
15. Kaneko J, Ota T, Unemoto K, Shigeta K, Inoue M, Aoki R, et al. Endovascular treatment of acute basilar artery occlusion: Outcomes, influencing factors and imaging characteristics from the Tama-REgistry of acute thrombectomy (TREAT) study. J Clin Neurosci. (2021) 86:184–9. doi: 10.1016/j.jocn.2020.12.034
16. Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G. Basilar artery occlusion. Lancet Neurol. (2011) 10:1002–14. doi: 10.1016/S1474-4422(11)70229-0
17. Camilo O, Goldstein LB. Seizures and epilepsy after ischemic stroke. Stroke. (2004) 35:1769–75. doi: 10.1161/01.STR.0000130989.17100.96
18. Gory B, Mazighi M, Blanc R, Labreuche J, Piotin M, Turjman F, et al. Mechanical thrombectomy in basilar artery occlusion: influence of reperfusion on clinical outcome and impact of the first-line strategy (ADAPT vs stent retriever). J Neurosurg. (2018) 129:1482–91. doi: 10.3171/2017.7.JNS171043
19. Browning RA. Role of the brain-stem reticular formation in tonic-clonic seizures: lesion and pharmacological studies. Fed Proc. (1985) 44:2425–31.
20. Penfield W. Epileptic automatism and the centrencephalic integrating system. Res Publ Assoc Res Nerv Ment Dis. (1952) 30:513–28.
21. Degtyarenko AM, Zavadskaya TV, Baev KV. Mechanisms of supraspinal correction of locomotor activity generator. Neuroscience. (1993) 52:323–32. doi: 10.1016/0306-4522(93)90160-H
22. Bauer G, Gerstenbrand F, Hengl W. Involuntary motor phenomena in the locked-in syndrome. J Neurol. (1980) 223:191–8. doi: 10.1007/BF00313183
23. Kreindler A, Zuckermann E, Steriade M, Chimion D. Electro-clinical features of convulsions induced by stimulation of brain stem. J Neurophysiol. (1958) 21:430–6. doi: 10.1152/jn.1958.21.5.430
24. Yamashiro K, Furuya T, Noda K, Urabe T, Hattori N, Okuma Y. Convulsive movements in bilateral paramedian thalamic and midbrain infarction. Case Rep Neurol. (2011) 3:289–93. doi: 10.1159/000334754
25. Sun X, Tong X, Gao F, Lao H, Miao Z. Endovascular treatment for acute basilar artery occlusion: a single center retrospective observational study. BMC Neurol. (2019) 19:315. doi: 10.1186/s12883-019-1551-8
Keywords: acute ischemic stroke, basilar artery occlusion, posterior circulation stroke, convulsion, seizure
Citation: Zhang D, Chen Y, Hao Y, Hu X and He X (2022) Acute Basilar Artery Occlusion Presenting With Convulsive Movements: A Systematic Review. Front. Neurol. 12:803618. doi: 10.3389/fneur.2021.803618
Received: 28 October 2021; Accepted: 09 December 2021;
Published: 07 January 2022.
Edited by:
Simone Beretta, San Gerardo Hospital, MexicoReviewed by:
Jeanne Teitelbaum, McGill University, CanadaSmit Patel, UCLA Health System, United States
Copyright © 2022 Zhang, Chen, Hao, Hu and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xudong He, eHVkb25naGV6akB6anUuZWR1LmNu
 Dan Zhang
Dan Zhang Yigang Chen1
Yigang Chen1 Yonggang Hao
Yonggang Hao Xingyue Hu
Xingyue Hu Xudong He
Xudong He