
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurol. , 07 February 2022
Sec. Neurotrauma
Volume 12 - 2021 | https://doi.org/10.3389/fneur.2021.723424
Background: Urinary retention is one of the most frequent complications of spinal cord injuries (SCI) and negatively impacts patient satisfaction and quality of life. Acupuncture as an integral part of traditional Chinese medicine (TCM) has recently drawn widespread attention for its potential in the management of urinary retention. However, there are many different styles of acupuncture-related techniques, and the optimal choice of acupuncture for urinary retention after SCI is still unclear. Hence, this study uses a Bayesian network meta-analysis (NMA) to compare the efficacy of different types of acupuncture therapies using both direct and indirect evidence.
Methods: Randomized controlled trials of acupuncture-related techniques for treating urinary retention after SCI were retrieved from the following electronic databases: Pubmed, Cochrane Library, Web of Science, China National Knowledge Infrastructure (CNKI), the Chinese Biomedical Literature Service System (SinoMed), the Wan-Fang database, and the Chinese Scientific Journals Database (VIP). The retrieval time was from inception to November 2020. Clinical effective rate (CER) was the primary outcome indicator and residual urine volume (RUV) was the secondary outcome indicator. A Bayesian NMA was performed using the Markov chain Monte Carlo method in R software (version 3.6.1) interfacing with JAGS software (version 4.3.0). The node-splitting method was used to identify inconsistencies. In addition, a comparative adjusted funnel plot was used to assess publication bias.
Results: A total of 26 randomized controlled trials involving 1,652 patients were included. Bayesian NMA showed that electroacupuncture combined with moxibustion ranks first in both CER and RUV. In addition, in terms of cumulative probability, electro-acupuncture combined with moxibustion ranked first in CER. The results of the node splitting method revealed that direct and indirect evidence were consistent (P > 0.05). In addition, publication bias was detected.
Conclusion: A Bayesian NMA that combined direct and indirect comparisons showed that electro-acupuncture combined with moxibustion had a better effect on urinary retention due to SCI. However, it still needs a large sample size and high-quality randomized controlled trials to verify this finding.
Systematic Review Registration: https://inplasy.com/, identifier: INPLASY2021110005.
Urinary retention is impaired voiding despite a full bladder, leading to a post-void residual (PVR) (1). It is one of the most frequent results of spinal cord injury (SCI) and negatively impacts patient satisfaction and quality of life. Urinary retention after SCI refers to dysfunction of the urinary bladder due to damaged bladder neural circuits following SCI. Studies have found that the bladder wall appears ischemic following SCI, affecting bladder metabolic function and resulting in the inability to discharge urine (2). Urinary retention has been closely associated with adverse outcomes including urinary tract infections, overdistension of the urinary bladder, and high mortality rates (3–5). Urethral catheterization and bladder function training are currently the main treatments for urinary retention among those SCI patients whose normal bladder function is altered. However, urethral catheterization is strongly associated with urinary tract infection (UTI), and the risk of a UTI increases with how long the patient catheterizes (6). Catheter-associated UTIs are the most common nosocomial infections. Catheter-associated UTIs affect men and women, and long-term urinary catheterization always and inevitably leads to bacteria in the urine of both sexes. Long-term catheterization typically results in a daily risk of 3–7% for the development of symptomatic catheter-associated UTI (7). In contrast, bladder function training leads to limited functional improvement. There is therefore a strong demand for novel and effective therapies for urinary retention after SCI.
Acupuncture as an integral part of traditional Chinese medicine (TCM) has recently drawn widespread attention for its potential in the management of urinary retention. It has consequently been the subject of research works on the topic (8–12). Advantages of acupuncture, as non-pharmacological therapy, including safety, convenience, and minimal side effect profile (13, 14). In China, many domains of acupuncture such as manual acupuncture, electro-acupuncture, moxibustion therapy, auricular acupuncture, and acupoint patching are widely used in the treatment of urinary retention after SCI. A previous traditional pairwise meta-analysis indicated that acupuncture has a positive effect on urinary retention due to SCI (15). However, there are many different styles of acupuncture, and the optimal acupuncture intervention is still unclear. Network meta-analysis (NMA) based on the traditional pairwise meta-analysis is an increasingly popular tool that can simultaneously synthesize direct and indirect evidence by summarizing different interventions for the same disease (16, 17). NMA can also assess the efficacy of different treatments and estimate the relative efficacy of such interventions (18, 19). Therefore, this study aimed to use NMA to explore the efficacy of different acupuncture therapy types in the treatment of urinary retention after SCI. This work may help provide guidelines for acupuncture therapy in the treatment of urinary retention after SCI and serve as the basis of future work.
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (20), and the study protocol has been registered on the website of https://inplasy.com/ (Registration number: INPLASY2021110005).
Literature inclusion: The PICOS framework (participants, interventions, comparisons, outcome, and study design) was used to identify literature appropriate for inclusion in this work. Eligible literature were randomized controlled trials (RCTs): (1) Study design: only articles referring to RCTs were included; (2) Participants: diagnosed with spinal cord injury, survived the shock period, not limited by age, gender, race, or nationality; (3) Intervention and control measures: using a similar study as the reference (21), acupuncture-related techniques were defined as acupoint-based therapy (e.g., manual acupuncture, electro-acupuncture, auricular acupuncture, moxibustion, acupoint patching, acupoint injection, acupoint embedding, and warm needling moxibustion) in this systematic review, regardless of stimulation method. The control group received conventional therapy or conventional therapy combined with some other therapy. The current conventional-therapies strategy for urinary retention after SCI consists of intermittent catheterization and bladder function training. (4) Outcome indicators: The primary outcome was Clinical effective rate (CER). Based on the presence of clinical symptoms and objective indicators, efficacy was divided into valid and invalid categories. No improvement in clinical symptoms, including those that worsen, was considered invalid. CER = (total number – invalid number)/total number × 100% (22). The secondary outcome was residual urine volume (RUV). The level of urinary retention was evaluated by the amount of RUV.
Literature exclusion: (1) Treatment measures in the experimental group included non-acupuncture-related therapies such as Chinese medicine and Western medicine; (2) The trial data was wrong; (3) The trial data was repeated; (4) The full text could not be obtained; (5) The outcome was not relevant.
RCTs of acupuncture-related techniques for the treatment of urinary retention after SCI were extracted from the following electronic databases: China National Knowledge Internet (CNKI), Wan-fang Database, Chinese Scientific Journals Database (VIP), the Chinese Biomedical Literature Service System (SinoMed), PubMed, Cochrane Library, and Web of Science. The retrieval period was from inception to November 2020. Terms such as “acupuncture,” “manual acupuncture,” “electro-acupuncture,” “scalp needle,” “elongated needle,” “moxibustion,” “warm needling,” “acupuncture plus moxibustion,” “acupoint injection,” “acupoint patching,” “auricular acupuncture,” “ear acupuncture,” “spinal cord injury,” “urinary retention,” and “neurogenic bladder” were used as subject words, keywords, free-text terms, or MeSH (Medical Subject Heading) terms to identify potentially eligible studies. The search strategy was adjusted for each database. There were no restrictions on blinding methods, language, and year of publication.
Relevant data from the eligible studies were extracted by two independent reviewers, and Microsoft Excel 2019 (Microsoft Corp, Redmond, WA, USA) was used to manage the data. A standard form table was constructed that included publication information (authors, publish date), demographic data (gender, age, ASIA grading, sample size, the course of SCI onset), intervention measures (experimental group: acupuncture treatments plus conventional therapy; control group: conventional therapy or conventional therapy plus other acupuncture therapy), and outcome (CER, RUV). The independent reviewers assessed the quality of the included trials using the Cochrane risk of bias tool (23). The Cochrane Risk of Bias tool includes seven items: (1) random sequence generation; (2) allocation concealment; (3) blinding of participants and personnel; (4) blinding of outcome assessment; (5) incomplete outcome data; (6) selective reporting; (7) other sources of bias. Each trail was graded as either “low,” “high,” or “unclear” risk. During trial selection when data extraction and quality assessment scores were inconsistent, discrepancies were resolved by a third reviewer.
Given the potential sources of clinical heterogeneity among the included studies, a random effect model was adopted to merge the datasets. The Bayesian meta-analysis was performed using R software (version 3.6.3; http://www.Rproject.org) and JAGS software (version 4.3.0, https://nchc.dl.sourceforge.net/project/mcmc-jags/JAGS/4.x/Windows/JAGS-4.3.0.exe), using the Bayesian hierarchical model and the Markov Chain Monte Carlo algorithm (24). We used 200,000 iterations, and the first 5,000 iterations were regarded as burn-in for annealing to eliminate the influence of the initial value. The combined results were presented as odds ratios (ORs) with 95% confidence intervals (95% CIs) for dichotomous outcomes. Due to the limitations of dichotomous outcomes, the description of “healing,” “remarkable effect,” and “effective” described in the study were combined into valid. The combined results were presented as mean differences (MDs) with 95% CIs for continuous outcomes. If 95% CIs of ORs did not contain 1 and 95% CIs of MDs did not contain 0, the corresponding ORs or MDs were considered to indicate a statistically significant difference. The surface under the cumulative ranking area (SUCRA) was used to rank the probabilities for different interventions. The SUCRA values range from 0 to 100%, assigned to the worst and best treatments (25), respectively. Publication bias and small-study effects among the included RCTs for the primary outcome were compared using an adjusted funnel plot (26).
A total of 1,199 references were identified (375 references from CNKI, 405 references from Wanfang, 188 references from VIP, 190 references from SinoMed, 8 references from Pubmed, 19 references from Cochrane Library, and 14 references from Web of Science) and imported into Endnote X9 (Clarivate Analytics, Philadelphia, PA, USA). After eliminating duplicates, 419 articles remained. Following the exclusion of reviews, case reports, animal experiments, and other irrelevant content, 125 studies remained. Non-randomized methodologies, data duplication, mixed interventions, and outcome indicators that did not include CER or RUV were also excluded. A total of 26 RCTs were ultimately included after evaluating the full text. A detailed flowchart depicting the article screening process is shown in Figure 1.

Figure 1. Flow diagram depicting the selection process of eligible studies. CNKI, China national knowledge infrastructure; VIP, Chinese Scientific Journals Database; SinoMed, Chinese Biomedical Literature Service System; n, number of publications.
A total of 26 articles were included, of which 25 trials (27–51) were double-arm RCTs and one trial (11) was three-arm RCTs. The total sample consisted of 1,652 patients (805 in the control group and 847 in the treatment group). Eight studies did not mention American Spinal Injury Association (ASIA) grade. Six studies did not report the course of SCI. Three studies did not mention the gender ratio of the participants. Two studies only reported the overall gender ratio. Three studies did not report patient age. The interventions in the control group included conventional therapy (CT) combined with electro-acupuncture (EA), CT combined with drug, CT combined with warm needle moxibustion (WNM), and CT combined with manual acupuncture (MA). The interventions in the experimental group included CT combined with EA, CT combined with Moxibustion (MOX), CT combined with MA, CT combined with acupoint patching (AP), CT combined with MOX, and Dong Shi Qi Point (DSQP), CT combined with auricular acupuncture (AA), CT combined with EA and MOX, CT combined with MOX and Wrist-ankle acupuncture (WAA). The shortest treatment course was 7 days and the longest was 2 months. Twenty-one trials reported CER and 20 trials reported RUV. Detailed study summaries are shown in Table 1.
Figure 2 depicts the risk of bias. For random sequence generation, 13 trials used random number tables, three trials used network programming software, six trials did not provide randomization details, and four trials used a wrong random method. Two trials involved allocation concealment and were assigned a low risk of bias. Only one trial mentioned single blindness and was assigned a low risk of bias. Only one trial reported two cases dropped out and the influence of incomplete outcome data was assigned a low risk of bias. All trials that did not mention study protocol and the influence of selective reporting were assigned an “uncertain” risk of bias. Only one trial reported disclosure of conflict of interest and the influence of other sources of bias was assigned a low risk of bias.
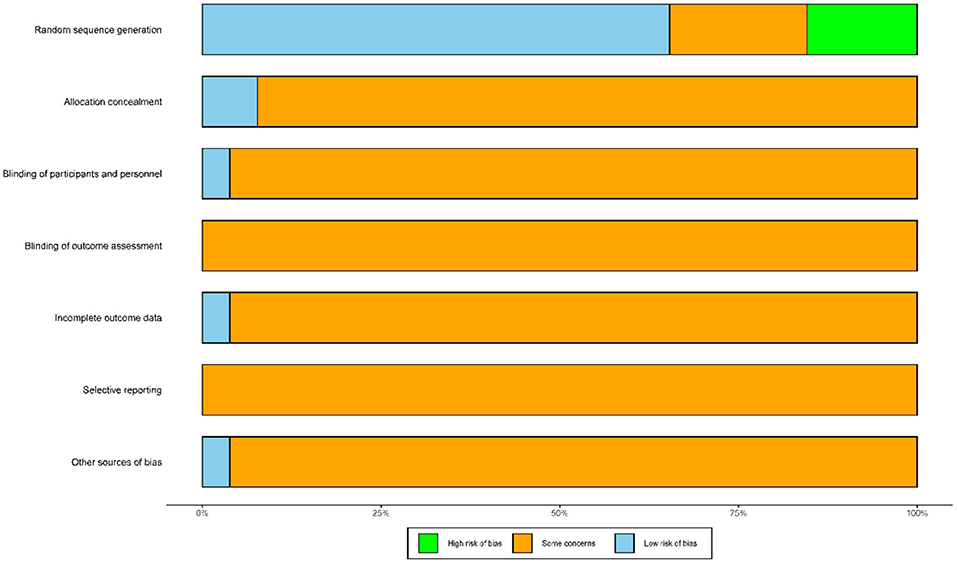
Figure 2. Risk of bias of the included studies. The vertical axis represents the quality evaluation items and the horizontal axis represents the number of studies.
Figure 3 shows 12 direct comparisons: CT vs. CT+MA (n = 2), CT vs. CT+EA (n = 2), CT vs. CT+MOX (n = 5), CT vs. CT+AA (n = 1), CT vs. CT+AP (n = 1), CT vs. CT+DSQP+MOX (n = 1), CT vs. CT+WAA (n = 1), CT+Drug vs. CT+MA (n = 1), CT+Drug vs. CT+EA (n = 1), CT+EA vs. CT+EA+MOX (n = 2), CT+MOX vs. CT+WNM (n = 1), CT vs. CT+multiple acupuncture (n = 1). Figure 4 shows the ranked and SUCRA values. CT+EA+MOX ranked first. CT+EA+ MOX (97%) had the highest SUCRA value in CER followed by CT+EA (74%), CT+MA (66%), CT+MOX (64%), CT+AP (63%), CT+multiple acupuncture (59%), CT+WAA+MOX (54%), CT+DSQP+MOX (54%), CT+Drug (24%), CT+WNM (21%), CT (21%), and CT+AA (4%). Table 2 shows the Odds ratio (95%CIs) of all treatments. Compared with CT, CT+MA, CT+EA, CT+MOX, and CT+EA+MOX were associated with significantly higher probabilities of CER.
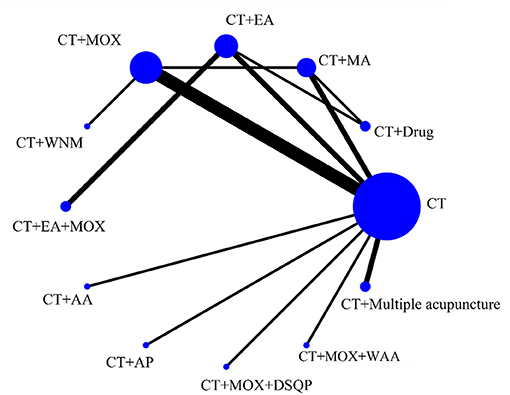
Figure 3. Network of eligible comparisons for the network meta-analysis of CER. Each node represents an intervention and the size of each node represents the number of randomly assigned participants. Each line represents a direct comparison between interventions and the width of the lines represents the number of studies.
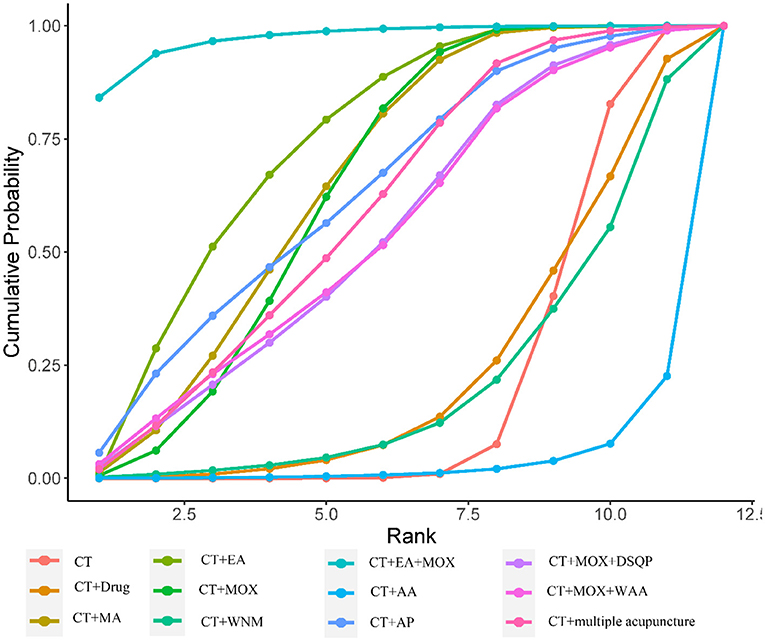
Figure 4. Cumulative probability ranking curve of different interventions for CER. The vertical axis represents cumulative probabilities, while the horizontal axis represents ranks.
Figure 5 presents 11 direct comparisons: CT vs. CT+MA (n = 3), CT vs. CT+EA (n = 2), CT vs. CT+MOX (n = 6), CT vs. CT+SA (n = 1), CT vs. CT+AA (n = 1), CT vs. CT+AP (n = 1), CT vs. CT+DSQP+MOX (n = 1), CT vs. CT+WAA (n = 1), CT+Drug vs. CT+EA (n = 1), CT+EA vs. CT+EA+MOX (n = 2), CT+EA vs. CT+SA (n = 1). Figure 6 presents the ranked and SUCRA value. CT+EA+MOX ranked first in terms of RUV and, the SUCRA value followed by CT+MA (79%), CT+EA+MOX (78%), CT+MOX (76%), CT+EA (62%), CT+AP (52%), CT+MOX +DSQP (42%), CT+WAA+MOX (41%), CT+Drug (40%), CT+AA (37%), CT+SA (23%), and CT (17%). Table 3 presents the mean differences (95%CIs) of all therapeutic measures. Compared with CT (control group), CT+MA, CT+EA, CT+MOX, and CT+EA+MOX were associated with significantly higher probabilities of RUV.
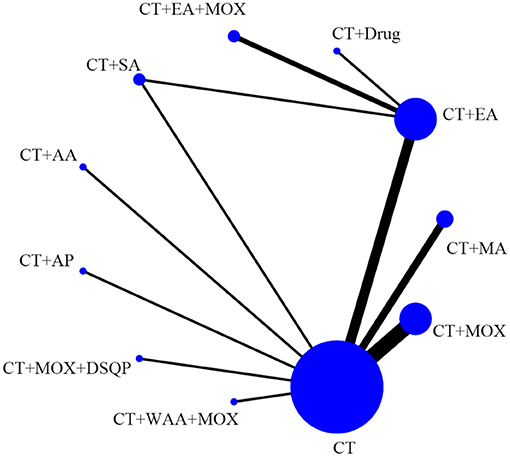
Figure 5. Network of eligible comparisons for the network meta-analysis of RUV. Each node represents an intervention and the size of each node represents the number of randomly assigned participants. Each line represents a direct comparison between interventions and the width of the lines represents the number of studies.
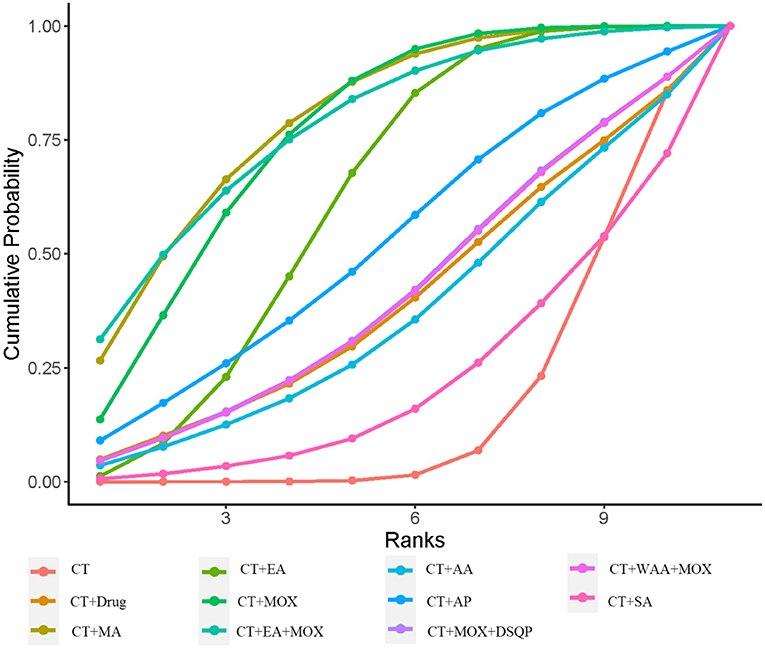
Figure 6. Cumulative probability ranking curve of different interventions for RUV. The vertical axis represents cumulative probabilities, while the horizontal axis represents ranks.
A comparative adjusted funnel plot was used to assess CER publication bias. When the distribution points in the funnel plot are symmetric, there is no publication bias (52). As shown in Figure 7, all points on the funnel plot were asymmetric and two points were at the bottom of the funnel plot, which represents a potential publication bias.
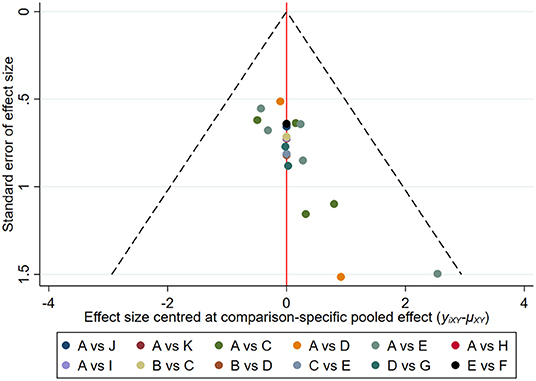
Figure 7. Comparison-adjusted funnel plots for the CER network. The vertical axis represents “standard error of effect size” and the horizontal axis represents “effect size centered at the comparison-specific pooled effect (yixy− uxy).” (A, CT; B, CT+Drug; C, CT+MA; D, CT+EA; E, CT+MOX; F, CT+WNM; G, CT+EA+MOX; H, CT+AA; I, CT+AP; J, CT+MOX+DSQP; K, CT+WAA+ MOX; L, CT+multiple acupuncture).
The node-splitting method was used to assess the inconsistency of the model between direct and indirect evidence (53, 54). Closed loops within the network were divided into direct and indirect comparison results. As shown in Figure 8, the results of node splitting revealed that direct and indirect evidence were consistent (P > 0.05).
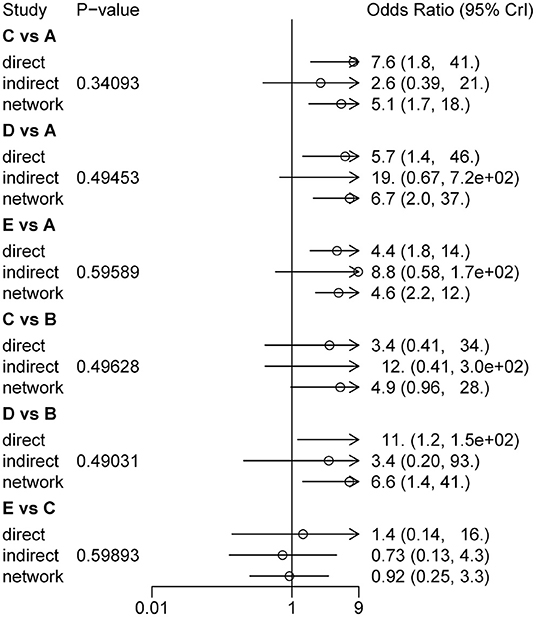
Figure 8. Consistency test results assessed different treatment measures of CER (A, CT; B, CT+ Drug; C, CT+MA; D, CT+EA; E, CT+MOX).
To the best of our knowledge, this is the first Bayesian NMA of acupuncture-related techniques in the treatment of urinary retention in patients with SCI. This study included 26 RCTs. The results of CER in NMA demonstrated that EA combined with MOX, EA, MOX, and MA have significantly increased treatment effects compared with CT. RUV in NMA demonstrated that EA combined with MOX, EA, MOX, and MA have significantly increased positive effects compared with CT. In terms of ranking probability, EA combined with MOX ranked first in both CER and RUV. In terms of cumulative probability, EA combined with MOX ranked first in CER. CER was assessed based on the degree of improvement of TCM clinical symptoms before and after treatment. This evaluation criterion was widely used to evaluate the efficacy of TCM (55–57). Further, the node splitting method showed that the direct and indirect evidence supporting treatment efficacy was consistent. Therefore, EA combined with MOX may be the best acupuncture intervention in patients with urinary retention secondary to an SCI.
The outcomes of the works included in this meta-analysis highlight several important factors, the most important of which is that EA combined with MOX may have better therapeutic efficacy in the treatment of urinary retention due to SCI. There is a good deal of evidence to support this view. An earlier study performed by our team indicated that acupuncture contributed to the recovery of neurologic function after SCI (58), and EA was the most frequently used technique. Another systematic review also suggests that acupuncture was helpful in the treatment of urinary retention after SCI, and EA was also primarily used (15). EA has been found to promote the recovery of bladder function in the setting of multiple pathologies (59, 60). Experimental studies showed that the mechanism of action of EA on bladder function includes apoptosis inhibition, nerve cell protection, and promotion of recovery of injured nerves (61). MOX is also an important part of acupuncture therapy, and has been widely used since ancient times in China. MOX exerts a warm stimulation effect by burning the herb Artemisia vulgaris over an acupoint and is widely considered a type of acupuncture treatment (62). Previous studies have shown that MOX can be used to treat urinary dysfunction caused by a stroke, SCI, or other factor (29, 63–65). Furthermore, EA combined with MOX is commonly used in research and clinical practice (66, 67). It is therefore noteworthy that the cumulative probability of EA combined with MOX did not show a significant advantage over EA alone in terms of RUV. Due to individual variation, RUV may not be the most suitable method for evaluating the clinical efficacy of TCM.
One important factor that needs to be taken into consideration is the selection of a Bayesian method or frequency analysis. The Bayesian method integrates overall information, sample information, and prior information of unknown parameters. According to Bayes' theorem, the posterior distribution of unknown parameters is obtained and unknown parameters are statistically inferred. This flexibility permits the wide use of Bayesian methodology in scientific research. Bayesian NMA also fully considers the uncertainty of parameters and can describe them with direct probabilities (for example, the probability that one intervention is better than another). Compared with frequency methods, Bayesian methods are more valuable when dealing with complex or sparse data (20). Finally, the comparison-adjusted funnel plot was used to detect publication bias in this study. The comparison-adjusted funnel plot appeared to have a degree of asymmetry, suggesting that potential publication bias existed in which “negative” studies were less likely to be reported. Prioritizing the publication of only articles that demonstrated differences between groups might be due to the rejection by journal editors of studies in this research field that report negative findings and seriously limits the quality of the evidence that addresses the effectiveness of acupuncture treatment.
Many other factors are also evident based on the studies we analyzed. First, most studies did not mention the ASIA grade of the SCIs. According to a previous study, ASIA grade on admission affected recovery in both univariate and multivariate analyses (68). We therefore could not explore the homogeneity of the ASIA grade included in these patients. Second, an outstanding question was the course of SCI-mediated urinary retention, as only 20 of our included studies mentioned the specific course of the SCI. Therefore, we were unable to compare differences between the acute and chronic phases. Third, most studies do not report on the long-term efficacy of acupuncture treatments. We therefore could not compare the long-term efficacy of acupuncture treatments. In addition, we could not assess the effect of acupoints on urinary retention due to SCI.
First, the currently available evidence on acupuncture and SCI-related urinary retention is insufficient due to small available sample sizes, limited numbers of patients in each trial, and limited analysis of CER and RUV data. Second, this study did not evaluate the safety of acupuncture because there was a lack of adverse event reporting in most of the included trials. Third, although a comprehensive literature search was performed using multiple online databases, it remains possible that some eligible studies may still have been missed.
The results of this NWM show that EA combined with MOX may be the most effective acupuncture technique for urinary retention after SCI. Our study may provide an important clinical reference value for clinical investigations of acupuncture in the treatment of neurogenic urinary retention and provide essential information to decision-makers. However, there are too many differences between the designs of the included studies to draw a definitive and clinical recommendation. High quality, large sample size, multicenter clinical trials are needed.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author/s.
KH and XL were involved in writing and draft preparation. BQ and LJ were involved in literature inclusion and exclusion. RM was involved in writing, draft preparation, and supervision. All authors critically revised the manuscript and approved its final version.
This work was supported by the Zhejiang Chinese Medical University Research Fund (Nos. 2019ZG17 and 2018ZY17 to KH); Chinese Medicine Research Program of Zhejiang Province (No. 2019ZZ013 to RM); Zhejiang Provincial Natural Science Foundation of China (No. LQ19H270003 to KH; No. LY19H270009 to RM); National Natural Science Foundation of China (No. 82174487 to RM).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
CT, conventional therapy; EA, electro-acupuncture; MA, manual acupuncture; WNM, warm needle moxibustion; AA, auricular acupuncture; AP, acupoint patching; DSQP, dong shi qi point; WAA, wrist-ankle acupuncture; SA, sham acupuncture; SCI, spinal cord injury.
1. Baldini G, Bagry H, Aprikian A, Carli F. Postoperative urinary retention: anesthetic and perioperative considerations. Anesthesiology. (2009) 110:1139–57. doi: 10.1097/ALN.0b013e31819f7aea
2. Bablumyan A, Kamalov A, Kirpatovski V, Srapyan A. [Relationship of acute urinary retention, bladder ischemia and metabolic changes in bladder wall and urine during infravesical obstruction due to benign prostatic hyperplasia]. Georgian Med News. (2011) 11:18–20.
3. Simforoosh N, Dadkhah F, Hosseini SY, Asgari MA, Nasseri A, Safarinejad MR. Accuracy of residual urine measurement in men: comparison between real-time ultrasonography and catheterization. J Urol. (1997) 158:59–61. doi: 10.1097/00005392-199707000-00016
4. Smith NK, Albazzaz MK. A prospective study of urinary retention and risk of death after proximal femoral fracture. Age Ageing. (1996) 25:150–4. doi: 10.1093/ageing/25.2.150
5. Torres B, Serakides R, Caldeira F, Gomes M, Melo E. The ameliorating effect of dantrolene on the morphology of urinary bladder in spinal cord injured rats. Pathol Res Pract. (2011) 207:775–9. doi: 10.1016/j.prp.2011.10.004
6. Suetens C, Latour K, Kärki T, Ricchizzi E, Kinross P, Moro ML, et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Euro Surveill. (2018) 23:1800516. doi: 10.2807/1560-7917.ES.2018.23.46.1800516
7. Saint S, Meddings JA, Calfee D, Kowalski CP, Krein SL. Catheter-associated urinary tract infection and the medicare rule changes. Ann Intern Med. (2009) 150:877–84. doi: 10.7326/0003-4819-150-12-200906160-00013
8. Chen S, Sun H, Xu H, Zhang Y, Wang H. Effects of acupuncture on hospitalized patients with urinary retention. Evid Based Complement Altern Med. (2020) 2020:2520483. doi: 10.1155/2020/2520483
9. Lauterbach R, Ferrer Sokolovski C, Rozenberg J, Weissman A. Acupuncture for the treatment of post-partum urinary retention. Eur J Obstet Gynecol Reprod Biol. (2018) 223:35–38. doi: 10.1016/j.ejogrb.2018.01.029
10. Yi WM, Pan AZ, Li JJ, Luo DF, Huang QH. Clinical observation on the acupuncture treatment in patients with urinary retention after radical hysterectomy. Chin J Integr Med. (2011) 17:860–3. doi: 10.1007/s11655-011-0800-5
11. Gu XD, Wang J, Yu P, Li JH, Yao YH, Fu JM. Effects of electroacupuncture combined with clean intermittent catheterization on urinary retention after spinal cord injury: a single blind randomized controlled clinical trial. Int J Clin Exp Med. (2015) 8:19757–63.
12. Sudhakaran P. Urinary retention in pregnancy and puerperium: acupuncture treatment. Med Acupunc. (2019) 31:269–73. doi: 10.1089/acu.2019.1363
13. Lin JG, Chen YH, Gao XY, Lao L, Lee H, Litscher G. Clinical efficacy, mechanisms, and safety of acupuncture and moxibustion. Evid Based Complement Altern Med. (2014) 2014:356258. doi: 10.1155/2014/356258
14. Zhao H, Li D, Li Y, Yang Y, Liu Y, Li J, et al. Efficacy and safety of acupuncture for hypertension: an overview of systematic reviews. Complement Ther Clin Pract. (2019) 34:185–94. doi: 10.1016/j.ctcp.2018.12.003
15. Wang J, Zhai Y, Wu J, Zhao S, Zhou J, Liu Z. Acupuncture for chronic urinary retention due to spinal cord injury: a systematic review. Evid Based Complement Altern Med. (2016) 2016:9245186. doi: 10.1155/2016/9245186
16. Grant RL. The uptake of Bayesian methods in biomedical meta-analyses: a scoping review (2005-2016). J Evid Based Med. (2019) 12:69–75. doi: 10.1111/jebm.12326
17. Zhang D, Wu J, Duan X, Wang K, Ni M, Liu S, et al. Network meta-analysis of chinese herbal injections plus the FOLFOX regimen for the treatment of colorectal cancer in China. Integr Cancer Ther. (2019) 18:1534735419827098. doi: 10.1177/1534735419827098
18. Greco T, Biondi-Zoccai G, Saleh O, Pasin L, Cabrini L, Zangrillo A, et al. The attractiveness of network meta-analysis: a comprehensive systematic and narrative review. Heart Lung Vessels. (2015) 7:133–42.
19. Rouse B, Chaimani A, Li T. Network meta-analysis: an introduction for clinicians. Intern Emerg Med. (2017) 12:103–11. doi: 10.1007/s11739-016-1583-7
20. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/M14-2385
21. Cheng P, Chi Z, Xiao Y, Xie W, Zhu D, Yu T, et al. The acupuncture-related therapy for post-stroke urinary incontinence: a protocol for systematic review and network meta-analysis. Medicine. (2020) 99:e22865. doi: 10.1097/MD.0000000000022865
22. Ministry of Health of People's Republic of China. Guidelines of TCM Clinical Research, 1st Edn. Beijing: People's Health Publishing House (1993).
23. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
24. Shim SR, Kim SJ, Lee J, Rücker G. Network meta-analysis: application and practice using R software. Epidemiol Health. (2019) 41:e2019013. doi: 10.4178/epih.e2019013
25. Cope S, Jansen JP. Quantitative summaries of treatment effect estimates obtained with network meta-analysis of survival curves to inform decision-making. BMC Med Res Methodol. (2013) 13:147. doi: 10.1186/1471-2288-13-147
26. Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS ONE. (2013) 8:e76654. doi: 10.1371/journal.pone.0076654
27. Zhu M, Chu JM, Zeng YH, Chen SX. Heat-sensitive moxibustion combined with acupuncture for treatment of 20 cases of retention after spinal cord injury urinary, Jiangsu J Trad Chinese Med. (2013) 45:54–55. doi: 10.3969/j.issn.1672-397X.2013.05.032
28. Zhao MH. Observation on curative effect of jiaji point drainage needle combined with warm needling on urinary retention after incomplete spinal cord injury. Shanghai J Acupunct Moxibust. (2015) 34:1162–1164.
29. Zhang CF, Sheng YF, Zhang HY. Efficacy of the herbal cake-separated moxibustion with new-type moxibustion device on urinary retention after spinal cord injury. Chinese Acupunct Moxibust. (2019) 39:953–6. doi: 10.13703/j.0255-2930.2019.09.010
30. Yang K. Clinical Research on the urinary retention after SCI by fulmigating the navel with Chinese herbs Beneth the Moxa cone and comprehensive rehabilitation training. Shandong Trad Chinese Med Univ. (2011).
31. Wu BT, Li JJ. Treatment of 68 cases of urinary retention after spinal cord injury by electroacupuncture combined with intermittent urinary catheterization. Traditional Chinese Med Res. (2012) 25:68–70.
32. Wang ZQ, Min YJ. Observation of effect on thermal moxibustion treatment of incomplete spinal cord injury urinary retention. J Chengdu Univ TCM. (2013) 36:60–3.
33. Wang L, An N. Acupuncture and moxibustion combined with intermittent catheterization in the treatment of spinal cord injury urinary retention for 18 cases. Chinese Med Modern Dist Educ China. (2017) 15:107–9.
34. Tong Z, Zhou SC, Zhu BB, Zhao CY, Li SM. Clinical observation of electroacupuncture of pair-point on neurogenic bladder urinary retention due to spinal cord injury. Shanxi J Trad Chinese Med. (2016) 32:27–9.
35. Su R. Observation on the Clinical Effect of “Zhibian Penetrating Shuidao” Acupuncture on Spinal Cord Injury Urinary Retention. Shanxi University of Chinese Medicine (2020).
36. Su J. Electro-Acupuncture Treatment Baliao Points Primarily Early Treatment of Thoracolumbar Fractures With Spinal Cord Injury Post-Operative Urinary Retention Clinical Research. Fujian University of Traditional Chinese Medicine (2012).
37. Sheng YF, Zhang C, Zhang CF, Zhu M. Clinical study of aconite moxibustion combined with bladder function training for treating urinary retention after incomplete spinal cord injury. China J Tradit Chinese Med Pharm. (2020) 35:3758–61.
38. Ma ST. The Clinical Research of Yiyuan Moxibustion on Neurogenic Bladder Urinary Retention After Spinal Cord Injury. Henan University of Chinese Medicine (2017).
39. Luo J. Effect of acupuncture and intermittent catheterization on bladder function in patients with urinary retention after spinal cord injury. Chinese Foreign Med Res. (2020) 18:130–2. doi: 10.14033/j.cnki.cfmr.2020.19.053
40. Li JL, He XH, Yang T, Li HS. Effect of acupuncture and intermittent catheterization in patients with urinary retention after spinal cord injury. China Foreign Med Treat. (2010) 29:84.
41. Li JH, Zhao DM, Ma BQ, Zhang LP, Wang Y. Curative effect of ginger-separated moxibustion combined with wrist-ankle acupuncture on neurogenic bladder uroschesis after spinal cord injury. Clin J Chinese Med. (2020) 12:80–2. doi: 10.3969/j.issn.1674-7860.2020.24.030
42. Kuang X, Zhou F. Moxibustion combined with rehabilitation functional training in the treatment of urinary retention in patients with spinal cord injury. Med Innov China. (2020) 17:77–80. doi: 10.3969/j.issn.1674-4985.2020.27.020
43. Jiang YX, Chen RX, Jiao L, Xiong J. Clinical effects of heat-sentive moxibustion therapy on urinary retention induced by spinal cord injury. China J Tradit Chinese Med Pharm. (2016) 31:324–6.
44. Huo JT, Zhang WR, Yang HX, Wei J. Clinical effect analysis of acupoint magnetic sticking application on patients with urinary retention after spinal cord injury. Intern Med. (2019) 12:92–9.
45. Hu Y, Wang HY. Clinical observation on treatment of spinal cord injury urinary retention with acupuncture Shenshu and Ciliao. Nei Mongol J Tradit Chinese Med. (2014) 7:59.
46. Hou Z, Luo KM, Qi TC, Kou JW, Bu AX. Clinical observation on 32 cases of urinary retention after spinal cord injury treated with salt-separated moxibustion at Dong's Qi and Shenque point. Chinese J Ethnomed Ethnopharm. (2019) 28:95–8.
47. Guo LQ. Clinical Study on Electroacupuncture associated With Neurogenic Bladder Dysfunction After Spinal Cord Injury Treated Intermittent Catheterization. Henan College of Traditional Chinese Medicine (2015).
48. Gao YL, Cheng X, Xia M. Acupuncture on the points of the Ren and Du Meridian Meridian for incompleteness effects of urinary retention after spinal cord injury. Tradit Chinese Med J. (2013) 12:46–7.
49. Gao YL, Chen X, Cheng X, Lai JH. Effects of electroacupuncture at acupoints ren and du channels on urinary retention of patients with incomplete spinal cord injury. J Med Theor Pract. (2017) 30:2355–6.
50. Gao XF, Cai BC. Intermittent catheterization combined with mild moxibustion to treat 30 cases of urinary retention after spinal cord injury. Chinese Med Modern Dist Educ China. (2014) 12:77–8. doi: 10.3969/j.issn.1672-2779.2014.20.044
51. Bu AX, Wang LG, Hou Z. Clinical study on treatment of acute spinal cord injury by penetrating auricular acupuncture along the skin and Baihui Point. Lishizhen Med Mater Med Res. (2017) 28:653–5.
52. Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. (2011) 342:d549. doi: 10.1136/bmj.d549
53. Spineli LM. An empirical comparison of Bayesian modelling strategies for missing binary outcome data in network meta-analysis. BMC Med Res Methodol. (2019) 19:86. doi: 10.1186/s12874-019-0731-y
54. van Valkenhoef G, Dias S, Ades AE, Welton NJ. Automated generation of node-splitting models for assessment of inconsistency in network meta-analysis. Res Synth Methods. (2016) 7:80–93. doi: 10.1002/jrsm.1167
55. Yang X, Hu C, Wang S, Chen Q. Clinical efficacy and safety of Chinese herbal medicine for the treatment of patients with early diabetic nephropathy: a protocol for systematic review and meta-analysis. Medicine. (2020) 99:e20678. doi: 10.1097/MD.0000000000020678
56. Wang L, Zhang L, Feng X, Xing L, Zhang W, Jiang K, et al. The functional difference of dendritic cells in HBeAg negative chronic Hepatitis B patients with three different spleen deficiency syndromes and the therapeutic evaluation of Chinese medicine intervention based on syndrome differentiation. Evid Based Complement Alternat Med. (2014) 2014:802402. doi: 10.1155/2014/802402
57. Jin J, Zhang H, Li D, Jing Y, Sun Z, Feng J, et al. Effectiveness of Xin Jia Xuan Bai Cheng Qi Decoction in treating acute exacerbation of chronic obstructive pulmonary disease: study protocol for a multicentre, randomised, controlled trial. BMJ Open. (2019) 9:e030249. doi: 10.1136/bmjopen-2019-030249
58. Ma R, Liu X, Clark J, Williams GM, Doi SA. The impact of acupuncture on neurological recovery in spinal cord injury: a systematic review and meta-analysis. J Neurotrauma. (2015) 32:1943–57. doi: 10.1089/neu.2014.3866
59. Chen H, Wang C, Zhou M, Yan Chan P, Lo Yam L, Lok Lam W, et al. Electroacupuncture for post-stroke overactive bladder: a multi-centre pilot randomized controlled trial. Acupunct Med. (2021) 39:175–83. doi: 10.1177/0964528420925488
60. Yu HJ, Zhu JG, Shen P, Shi LH, Shi YC, Chen F. Electroacupuncture decreases the urinary bladder pressure in patients with acute gastrointestinal injury. Genet Mol Res. (2015) 14:34–9. doi: 10.4238/2015.January.15.5
61. Zhang T, Yu J, Huang Z, Wang G, Zhang R. Electroacupuncture improves neurogenic bladder dysfunction through activation of NGF/TrkA signaling in a rat model. J Cell Biochem. (2019) 120:9900–5. doi: 10.1002/jcb.28272
62. Dimitrova A, Murchison C, Oken B. Acupuncture for the treatment of peripheral neuropathy: a systematic review and meta-analysis. J Altern Complement Med. (2017) 23:164–79. doi: 10.1089/acm.2016.0155
63. Liu HL, Wang LP. [Randomized controlled study on ginger-salt-partitioned moxibustion at shenque (CV 8) on urination disorders poststroke]. Zhongguo Zhen Jiu. (2006) 26:621–4.
64. Zhang JL, Yang J, Wang C, Pan W, Wang F. [Clinical trials of treatment of post-stroke neurogenic bladder by plum-blossom needle tapping plus moxibustion]. Zhen Ci Yan Jiu. (2019) 44:363–6. doi: 10.13702/j.1000-0607.180155
65. Feng XD, Ren YF, Wei DW, Liu CM. [Clinical observation on moxibustion combined with intermittent urethral catheterization for treatment of neurogenic vesical dysfunction]. Zhongguo Zhen Jiu. (2009) 29:91–4.
66. Wang L, Qiu L, Zheng X, Ouyang J, Zhang M, He L, et al. Effectiveness of electroacupuncture at Jiaji acupoints (EX-B2), plus moxibustion and intermediate on postherpetic neuralgia: a randomized controlled trial. J Tradit Chin Med. (2020) 40:121–7.
67. Huang X. Treatment of urinary retention with acupuncture and moxibustion. J Tradit Chin Med. (1991) 11:187–8.
Keywords: acupuncture, urinary retention, network meta-analysis, spinal cord injury, clinical efficacy
Citation: He K, Li X, Qiu B, Jin L and Ma R (2022) Comparative Efficacy of Acupuncture-Related Techniques for Urinary Retention After a Spinal Cord Injury: A Bayesian Network Meta-Analysis. Front. Neurol. 12:723424. doi: 10.3389/fneur.2021.723424
Received: 10 June 2021; Accepted: 27 December 2021;
Published: 07 February 2022.
Edited by:
Ahmed Negida, Zagazig University, EgyptReviewed by:
Ali Hammed, Tishreen University, SyriaCopyright © 2022 He, Li, Qiu, Jin and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ruijie Ma, bWFyaWE3ODc4QHNpbmEuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.