- Department of Sports Medicine, Goethe-University Frankfurt, Frankfurt, Germany
Background: Physical activity and sleep quality are both major factors for improving one's health. Knowledge on the interactions of sleep quality and the amount of physical activity may be helpful for implementing multimodal health interventions in older adults.
Methods: This preliminary cross-sectional study is based on 64 participants [82.1 ± 6.4 years (MD ± SD); 22 male: 42 female]. The amount of physical activity was assessed by means of an accelerometer (MyWellness Key). Self-reported sleep parameters were obtained using the Pittsburgh Sleep Quality Index. The Barthel Index was used for physical disability rating. Bivariate correlations (Spearman's Rho) were used to explore relationships between the amount of physical activity and sleep quality. To analyse differences between categorial subgroups univariate ANOVAs were applied; in cases of significance, these were followed by Tukey-HSD post-hoc analyses.
Results: No linear association between physical activity and sleep quality was found (r = 0.119; p > 0.05). In subgroup analyses (n = 41, Barthel Index ≥90 pts, free of pre-existing conditions), physical activity levels differed significantly between groups of different sleep duration (≥7 h; ≥6 to <7 h; ≥5 to <6 h; <5h; p = 0.037).
Conclusion: There is no general association between higher activity levels and better sleep quality in the investigated cohort. However, a sleep duration of ≥5 to <6 h, corresponding to 7.6 h bed rest time, was associated with a higher level of physical activity.
Background
Regular physical activity of a sufficient extent provides a broad range of health benefits. Sufficient physical activity is defined as weekly 150 min of moderate activity, or 75 min of vigorous activity, or a combination of both (1–4). Besides the generally recommended strengthening exercises twice per week, older adults (≥65 years) are also advised to include balance exercises. Physical activity is able to reduce the risk of various non-communicable diseases such as diabetes, cancer, osteoporosis, depression, cardiovascular diseases and metabolic diseases (5, 6). Moreover, sufficient physical activity enhances mobility and the ability to perform activities of daily living (ADLs) in older adults whilst also reducing the risk of falls and delaying, or preventing, care dependency (7). As a measure of independency, the Barthel Index rates the ability to perform ADLs as well as physical activity (8, 9).
Another major contributing factor to health and well-being in older adults is sleep quality. Good sleep impacts on the regeneration of the immune system and the metabolic brain processes (10–13). As well as throughout life, sleep quality determines the quality of health at higher age to a certain extent (14). However, sleep duration as one component of sleep quality decreases with increasing age, while the sleep itself shows augmented interruptions (15). Periods of deep sleep and Rapid-Eye-Movement (REM) sleep decline proportionally to the overall sleep duration. Sleep efficiency diminishes due to rising sleep latency and more frequent interruptions of sleep at old age (15). In nursing homes more than half of all inhabitants suffer from sleep disturbances (16).
Even though physical activity and sleep quality both contribute to the status of health, the underlying physiological mechanisms differ greatly. Nevertheless, there appear to be clinically important mutual relationships between these two factors (17). Therefore, changes in one factor may affect the health outcomes of both. A deeper understanding of the association between sleep parameters and physical activity may lead to advanced health promotion. It has yet to be clarified whether healthy doses of sleep and activity, as well as their health benefits, are combinable or if they possibly interfere.
Previous studies have examined associations of regular and acute bouts of physical activity with sleep parameters (18–21). Although a great variety of investigated types of physical activities and sleep parameters have led to an equally numerous variety of outcomes, there exists a consensus among the literature that physical activity increases sleep quality (22). As a crosscheck for the above-mentioned outcomes, sleep disturbances were associated with a limitation in physical activity in a cohort of cancer patients (23). However, in the case for sleep duration, there appears to be disagreement among the literature on the arguable association with physical activity (24–26).
Therefore, investigating the relation between physical activity and sleep parameters such as sleep duration may add to the current state of knowledge. A deeper understanding of the relation between these two factors might contribute to future research on their mutual health effects. Older adults generally exhibit decreased sleep quality and physical activity. Furthermore, the urgency of geriatric health promotion increases along with demographic change. Hence, the present study investigates the association between habitual physical activity and sleep parameters in older adults.
Methods
Ethical Standards and Study Design
This preliminary cross-sectional study was approved by the local review board (Goethe University, Department of Psychology and Sports Sciences, Ethics Committee; Approval-Number 2019-22) and conducted in accordance to the Declaration of Helsinki. Start date was in 2019. After agreement from the participating institutions' managements, the study design was presented at residents' meetings prior to recruitment via personal contact. All participants signed informed consent before inclusion.
Participants
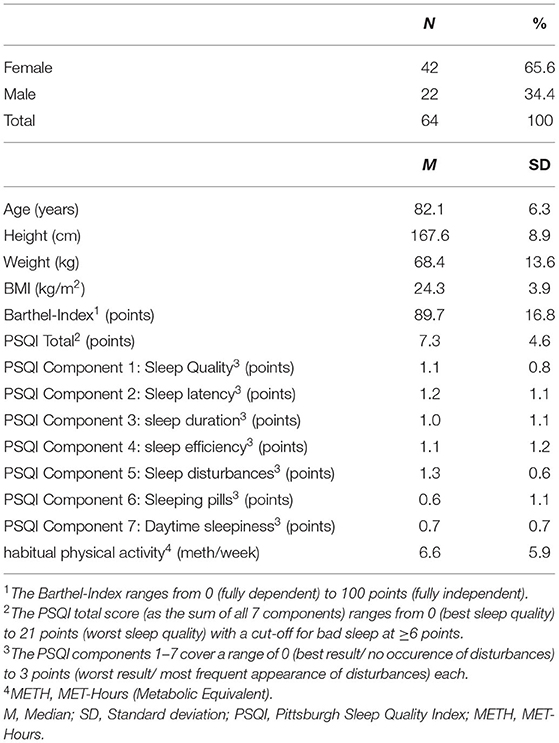
Residents (males and females) of nursing homes, assisted living institutions and senior residences aged over 65 were included. Exclusion criteria comprised acute infections or injuries, being bedridden and dementia [Montreal Cognitive Assessment—MoCA <17 (27)]. Participants were recruited by personal contact within institutions interested in the study. Overall, 64 older adults participated in the study (Table 1).
Study Flow
After recruitment, as described above, all participants wore an accelerometer for seven consecutive days. After the 7 days of activity measurement, all participants completed the Pittsburgh Sleep Quality Index (PSQI), MoCA and Barthel Index in an interview. Since physical activity was assessed for the past 7 days and sleep quality for the past 4 weeks at this point, there was a data overlap of 1 week.
Measurements and Data Processing
The Barthel Index was used for physical disability rating. The questionnaire captures self-reliance in 10 different activities of daily living. The rating works in intervals of five points, starting at 0 going up to 5–15 points depending on the item. Adding up the score of each item, the Barthel-Index ranges from 0 to 100 points. It classifies participants from completely dependent (0) to completely independent (100). Dementia was checked by means of the MoCA. The MoCA is a screening tool for mild cognitive impairment, examining executive function, language abilities, short-term memory and visuospatial processing (28). The cut-off for dementia was a score of <17 points (27).
The amount of physical activity was assessed by means of an accelerometer (MyWellness Key, Technogym, Gambettola, IT). The uniaxial accelerometer captures different intensities of acceleration expressed in a proprietary metric called “Moves.” The different intensities are categorized as “Run” [≥6 MET (Metabolic equivalent)], “Play” (3.0–5.9 MET) and “Free” (1.8–2.9 MET) (29). By means of defined category MET-values, the captured activity was translated into MET-hours prior to further processing. The MyWellness Key exhibits sufficient measurement properties (validity: Pearson's r = 0.895–0.944, p < 0.001; reliability: ICC > 0.93) (29, 30). All participants were instructed to wear the devices in a horizontal position near the hip for 7 consecutive days. Only accelerometer-datasets of at least 4 completely captured days [10 h wear time each day (31)] were included in the analysis. Datasets of 3 or fewer days were excluded in favor of reliability of the computed average daily activity (31). Accelerometer wear time was captured by a self-administered diary by the participants. Firstly, the proprietary metric of the devices was translated into MET-hours for further analysis. The conversion to MET-values was executed by multiplying the median MET-value of each intensity range with the registered minutes of activity at the corresponding intensity levels (29). Following the WHO definition of sufficient physical activity, a cut-off of 7.5 MET-h/week (150 min = 2.5 h; 2.5 h * 3MET = 7.5 MET-h) marks the minimum recommended activity level (4). Measurement properties of the accelerometers utilized have been validated satisfactory against indirect calorimetry, as well as crossvalidated for usage in cohorts of older adults (29, 30, 32–34).
Self-reported sleep quality, efficiency, duration and bed rest time were obtained using the Pittsburgh Sleep Quality Index (PSQI). The PSQI captures data on sleep for the last 4 weeks until completion in 19 items (35). The items partially offer open questions (Items 1–4) and partially offer scales, from 0 to 3, mostly defining the frequency of occurrence of sleep complaints (Items 5–14 and 16–17). The total score consists of seven components: (1) subjective sleep quality, (2) sleep latency, (3) sleep duration, (4) sleep efficiency, (5) sleep disturbances, (6) sleeping-pill intake and (7) daytime sleepiness (35). The rating of the subscores is based on the instructions from Smith and Wegener (36), yielding values of 0–3 points for each subscore. The sum of all subscores equals the total score of the PSQI, which is referenced as overall sleep quality hereinafter. The total score ranges from 0 points (highest sleep quality) to 21 points (lowest sleep quality) with a cut-off for poor sleep quality above 5 points (35). Sleep efficiency (Time spent in bed/sleep duration = sleep efficiency) is expressed as a percentage with 100% representing a perfect sleep efficiency. The questionnaire exhibits sufficient reliability (r = 0.45–0.84) as well as internal consistency (Cronbach's α = 0.69) (35–37). All PSQI subscores, as well as the total score, were digitalized and checked for plausibility. “Healthy” sleep duration was defined as a period of 6–7 h as this value is found to be an intersection present in the literature (11, 14, 24, 38–40).
Data Analysis
For statistical analyses, SPSS for Windows (Version 22, IBM, SPSS Inc., Chicago, IL, USA) and BIAS for Windows (Version 9.05, Goethe-University Frankfurt, Germany) were used. A p-value of 5% was considered as a relevant cut-off for significance testing. Normal distribution was checked by means of the Shapiro-Wilk-Test (p > 0.05). The Levene-Test served for checking homoscedasticity which was given (p > 0.05). Linearity was checked by visual inspection. Group differences (sex) were examined by means of t-tests for independent samples. Bivariate correlations (Spearman's Rho) were used to explore potential relationships between the amount of physical activity and the sleep quality as PSQI total scores and subscores. In order to minimize confounding factors on physical activity, a subcohort of n = 41 participants was created by solely including participants exhibiting a Barthel Index of 90 points or more, free of pre-existing conditions (41). Subsequently, the subcohort was split into four subgroups by the participants' habitual sleep duration. The subgroups were categorized in (1) <5 h of sleep, (2) ≥5 to <6 h of sleep, (3) ≥6 to <7 h of sleep, and (4) ≥7 h of sleep. To analyze differences between the subgroups' physical activity levels univariate ANOVAs were applied, followed by Tukey-HSD post-hoc analyses in cases of significance.
Results
Complete datasets of 64 participants were captured. No participant withdrew his/her consent and no participant was excluded. Participants characteristics are shown in Table 1.
Physical activity levels of the older adults ranged from 3.7 to 35.6 MET-h per week. Only a small proportion met the recommended physical activity levels (3.1%). Participants moved mainly at low-intensity levels (84.5% of overall captured activity), while they were active at medium intensity-levels to a much lesser extent (15.3%) with high-intensity movements being virtually non-existent (0.2%).
The PSQI data show an average total score of 7.2 ± 4.6 points for all participants. Measured scores ranged from 1 to 19 points. Less than half of the cohort (42.2%) can be classified as “good sleepers” by the PSQI total score (≤5 points). Men tended to sleep better according to the present data. Women report a higher incidence in sleep disturbances (Scale of 0 to 3: ♀ = 1.81 ± 1.31 points; ♂ = 1.32 ± 1.43 points; F = 1.611, p > 0.05), whereas men exhibited higher values regarding sleep efficiency [♀ 76.0 ± 17.7% (range 39.1–100%); ♂ 84.3 ± 11.3% (range 61.1–100%); p = 0.026].
No linear association between physical activity (Accelerometer data) and sleep quality (PSQI total score) was found in the total sample (r = 0.119; p > 0.05). In the subcohort analysis (only participants with a Barthel Index ≥90 points and free of pre-existing conditions; n = 41), the physical activity levels differed significantly (p = 0.037) between groups of different sleep duration (Group 1, n = 7, <5 h of sleep; Group 2, n = 11, ≥5 to <6 h of sleep; Group 3, n = 10, ≥6 to <7 h of sleep; Group 4, n = 13, ≥7 h of sleep) (Figure 1). More precise, the average MET-hours per week were 13.5 ± 7.4 (M ± SD) for participants sleeping <5 h (Group 1), 23.5 ± 9.7 for participants sleeping up to 6 h (Group 2), 16.8 ± 4.3 for participants sleeping up to 7 h (Group 3) and 15.0 ± 7.5 for participants sleeping 7 h or more (Group 4).
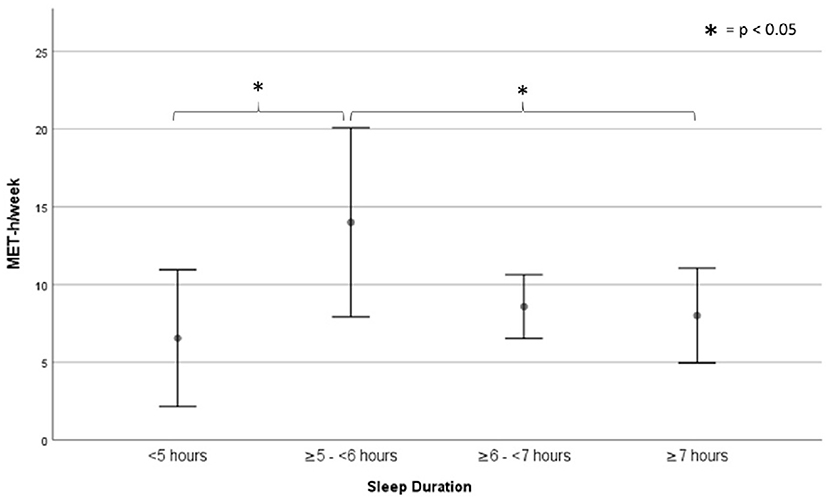
Figure 1. Sub-cohorts' activity levels based on sleep duration subgroups. Data are displayed as means and 95% confidence intervals.
Participants sleeping ≥5 to <6 h/night differed from participants exhibiting other sleep durations (≥7, ≥6 to <7, and <5 h) in the activity per week (p = 0.005) and in the sleep efficiency (p < 0.05).
Discussion
Habitual physical activity and sleep duration appear to be linked in the present cohort. However, we found no accordance between higher activity levels and better sleep quality in the investigated cohort per se. A self-reported sleep duration of ≥5 to <6 h, corresponding to 7.6 h bed rest time, is, however, associated with a higher level of physical activity.
Besides low activity levels among the cohort, the measured intensity values align with the values determined by a similar study (42). Only 3.1% of the cohort reached the recommended extent of physical activity above an intensity of ≥3 MET. Since the MyWellness Key calculates “Moves” solely from captured acceleration, regardless of sex, age, weight and height of the wearer, we hypothesize that there is some discrepancy between measured and experienced exercise intensity. The accelerometer data seem to underestimate the intensity experienced by our geriatric cohort. The need to adjust the accelerometer data for the intensity experienced in older adults has already been addressed in the literature (43, 44). Even though there is disagreement among the literature whether accelerometry reliably reflects experienced intensity in older adults, there are indications that the generalized limits of the intensity levels need age-appropriate cut-off points. For instance, even a slow walking speed (1.5 mph) was associated with moderate-intensity energy expenditure in a cohort of older adults (45). Contrary to the accelerometer's raw data, we thus assume our participants to be more active than equivalent-aged reference populations.
Our findings regarding a higher incidence of sleep disturbances and lower sleep quality in women align with related studies' results (46–48).
There is agreement on the health risks caused by “too” long or short sleep durations, such as increased all-cause mortality, cardiovascular mortality and lower cognition capability (39, 40). The discussion regarding healthy sleep duration remains controversial; estimates vary from 3 to 5 h as being too short, while 8–10 h is regarded as being too extended for sleep duration (38, 49). By reporting an average sleep duration of 6.7 ± 1.8 h, the present cohort shows a healthy sleep duration, irrespective of the quoted source.
The fact that the present cohort almost exclusively moved at lower intensity levels assumingly contributes to the missing correlations between physical activity and sleep parameters. It is feasible that there may still be a relationship between higher intensity activity and sleep parameters that has remained concealed in the present study. Despite the existing relationship of low intensity activity to health, an explanation for any missing correlation of low intensity activity with sleep parameters is absent in the literature (18, 50, 51).
However, regardless of the intensity levels, the present data indicate a trend towards a relationship between activity extent and self-reported sleep duration. Participants reporting ≥5 to <6 h of sleep move more than any group reporting different sleep durations and, consequently, when taking activity of all intensity levels into account, are more likely to be sufficiently physically active in terms of current guidelines. As majoritarian literature quantifies “healthy” sleep duration as ≥6 to ≤7 h (38, 49, 52), the most advantageous sleep duration may diverge, depending on the underlying criteria. Consequently, the sleep duration resulting in the greatest health benefits may not be the same as the one resulting in the highest amount of physical activity. Furthermore, sleep duration is assumed to depend on physical activity behavior (53), leading to a presumably mutual interference of both. The assumption that the combination of shorter sleep durations with higher activity levels is derived from gained time to move is refuted by the similar overall bedtimes adopted across all activity groups. Additionally, the most active group exhibits the lowest sleep efficiency; this highlights that increased physical activity is not, per se, a warrantor for high sleep quality. All in all, present data indicate an inverted U-shaped curvilinear relationship of physical activity and sleep duration.
Present study is not free of limitations. Regarding the findings of our statistical analysis a larger sample size would consolidate validity and generalizability of our results. Furthermore, an additional objective measurement of sleep parameters would enhance data quality compared to a solely subjective assessment tool. Measurements of physical activity may gain additional quality from usage of multiaxial accelerometers over the uniaxial instruments used in present investigation. Some modern devices allow the measurement of both, physical activity and sleep, within a single instrument.
The dominant direction of influence is still questionable in the mutual interference between sleep and physical activity. The questions: “Which of these two factors has the stronger impact on health?” and “Are these factors combinable for a maximum benefit on old age health status?” still remain. To explore these health-relevant issues, future studies should address both factors and, ideally, should also assess the direction of the causal connection. We recommend a cohort exhibiting corresponding activity levels in order to analyze the relationship of higher intensity activity with sleep parameters. For this purpose, it might be appropriate to recruit participants e.g., in sports clubs and sports facilities rather than from general population. Besides existing recommendations on physical activity, the implementation of recommendations and information on healthy sleep behavior might benefit older adults. Since both affect health over the long term, raising awareness to optimize physical activity and sleep in this particular population group, may be of more value than brief interventions.
Conclusion
Even if there is no linear association between sleep quality and physical activity, both factors appear to be linked. Differing activity levels between groups of various self-reported sleep durations indicate a coherence of sleep and activity extents. A deeper understanding of these factors' relationship may enable research on the compatibility of their health benefits and, therefore, contribute to the improvement of general and geriatric health promotion.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee, Goethe-University Department 05, Faculty of Psychology and Sport Sciences. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
LV, OV, and IE-R: study concept and design. OV and IE-R: acquisition of data. DN and JW: analysis and interpretation of data. OV, DN, JW, IE-R, and LV: preparation of manuscript. All authors have read and approved the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ADL, Activity of Daily Living; ICC, Intra Class Correlation; M, Mean; MET, Metabolic Equivalent; MoCA, Montreal Cognitive Assessment; PSQI, Pittsburgh Sleep Quality Index; REM-sleep, Rapid Eye Movement-sleep; SD, Standard Deviation; WHO, World Health Organization.
References
1. Haskell WL, Lee I-M, Pate RR, Powell KE, Blair SN, Franklin BA et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. (2007) 39:1423–34. doi: 10.1249/mss.0b013e3180616b27
2. Kahlmeier S, Wijnhoven TMA, Alpiger P, Schweizer C, Breda J, Martin BW. National physical activity recommendations: systematic overview and analysis of the situation in European countries. BMC Public Health. (2015) 15:133. doi: 10.1186/s12889-015-1412-3
3. Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. (2018) 320:2020. doi: 10.1001/jama.2018.14854
4. World Health Organization. Global Recommendations on Physical Activity for Health. Geneva: WHO (2010).
5. Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. (2009) 41:1510–30. doi: 10.1249/MSS.0b013e3181a0c95c
6. Bouchard C, Blair SN, Haskell WL. Physical Activity and Health. 2nd ed. Leeds: Human Kinetics (2012).
7. Landesinstitut für Gesundheit und Arbeit des Landes Nordrhein-Westfalen. Gesundheit durch Bewegung fördern: Empfehlungen für Wissenschaft und Praxis. Düsseldorf: Landesinst. für Gesundheit und Arbeit des Landes Nordrhein-Westfalen (2011). (LIGA.Fokus; vol 12). Available online at: https://bkk-wf.bgm-bkk.de/uploads/media/LIGA_Fokus_12.pdf#page=47 (accessed July 4, 2020).
8. Cuesta-Vargas AI, Pérez-Cruzado D. Relationship between Barthel index with physical tests in adults with intellectual disabilities. SpringerPlus. (2014) 3:543. doi: 10.1186/2193-1801-3-543
9. Wade DT, Collin C. The Barthel ADL index: a standard measure of physical disability? Int Disab Stud. (1988) 10:64–7. doi: 10.3109/09638288809164105
10. Diekelmann S, Born J. The memory function of sleep. Nat Rev Neurosci. (2010) 11:114–26. doi: 10.1038/nrn2762
11. Ferrara M, Gennaro L de. How much sleep do we need? Sleep Med Rev. (2001) 5:155–79. doi: 10.1053/smrv.2000.0138
12. Schuld A, Haack M, Hinze-Selch D, Mullington J, Pollmächer T. Experimentelle Untersuchungen der Interaktion zwischen Schlaf und Immunsystem beim Menschen. Psychother Psych Med. (2005) 55:29–35. doi: 10.1055/s-2004-834561
13. Scullin MK, Bliwise DL. Sleep, cognition, and normal aging: integrating a half century of multidisciplinary research. Perspect Psychol Sci. (2015) 10:97–137. doi: 10.1177/1745691614556680
14. Hall MH, Smagula SF, Boudreau RM, Ayonayon HN, Goldman SE, Harris TB et al. Association between sleep duration and mortality is mediated by markers of inflammation and health in older adults: the Health, Aging and Body Composition Study. Sleep. (2015) 38:189–95. doi: 10.5665/sleep.4394
15. Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. (2004) 27:1255–73. doi: 10.1093/sleep/27.7.1255
16. Neikrug AB, Ancoli-Israel S. Sleep disturbances in nursing homes. J Nutr Health Aging. (2010) 14:207–11. doi: 10.1007/s12603-010-0051-8
17. Atkinson G, Davenne D. Relationships between sleep, physical activity and human health. Physiol Behav. (2007) 90:229–35. doi: 10.1016/j.physbeh.2006.09.015
18. Chen K-M, Chen M-H, Lin M-H, Fan J-T, Lin H-S, Li C-H. Effects of yoga on sleep quality and depression in elders in assisted living facilities. J Nurs Res. (2010) 18:53–61. doi: 10.1097/JNR.0b013e3181ce5189
19. Martin JL, Marler MR, Harker JO, Josephson KR, Alessi CA. A multicomponent nonpharmacological intervention improves activity rhythms among nursing home residents with disrupted sleep/wake patterns. J Gerontol A Biol Sci Med Sci. (2007) 62:67–72. doi: 10.1093/gerona/62.1.67
20. Montgomery P. A systematic review of non-pharmacological therapies for sleep problems in later life. Sleep Med Rev. (2004) 8:47–62. doi: 10.1016/S1087-0792(03)00026-1
21. Richards KC, Lambert C, Beck CK, Bliwise DL, Evans WJ, Kalra GK et al. Strength training, walking, and social activity improve sleep in nursing home and assisted living residents: randomized controlled trial. J Am Geriatr Soc. (2011) 59:214–23. doi: 10.1111/j.1532-5415.2010.03246.x
22. Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. (2015) 38:427–49. doi: 10.1007/s10865-015-9617-6
23. Loh KP, Pandya C, Zittel J, Kadambi S, Flannery M, Reizine N, et al. Associations of sleep disturbance with physical function and cognition in older adults with cancer. Support Care Cancer. (2017) 25:3161–9. doi: 10.1007/s00520-017-3724-6
24. Bellavia A, Åkerstedt T, Bottai M, Wolk A, Orsini N. Sleep duration and survival percentiles across categories of physical activity. Am J Epidemiol. (2014) 179:484–91. doi: 10.1093/aje/kwt280
25. Khan MKA, Chu YL, Kirk SFL, Veugelers PJ. Are sleep duration and sleep quality associated with diet quality, physical activity, and body weight status? A population-based study of Canadian children. Can J Public Health. (2015) 106:e277–82. doi: 10.17269/cjph.106.4892
26. Ortega FB, Ruiz JR, Labayen I, Kwak L, Harro J, Oja L et al. Sleep duration and activity levels in Estonian and Swedish children and adolescents. Eur J Appl Physiol. (2011) 111:2615–23. doi: 10.1007/s00421-011-1883-6
27. Freitas S, Simões MR, Alves L, Vicente M, Santana I. Montreal cognitive assessment (MoCA): validation study for vascular dementia. J Int Neuropsychol Soc. (2012) 18:1031–40. doi: 10.1017/S135561771200077X
28. Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. (2005) 53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x
29. Sieverdes JC, Wickel EE, Hand GA, Bergamin M, Moran RR, Blair SN. Reliability and validity of the my wellness key physical activity monitor. Clin Epidemiol. (2013) 5:13–20. doi: 10.2147/CLEP.S38370
30. Bergamin M, Ermolao A, Sieverdes JC, Zaccaria M, Zanuso S. Validation of the mywellness key in walking and running speeds. J Sports Sci Med. (2012) 11:57–63.
31. Gabrys L, Thiel C, Tallner A, Wilms B, Müller C, Kahlert D, et al. Akzelerometrie zur erfassung körperlicher aktivität. Sportwissenschaft. (2015) 45:1–9. doi: 10.1007/s12662-014-0349-5
32. Colbert LH, Matthews CE, Havighurst TC, Kim K, Schoeller DA. Comparative validity of physical activity measures in older adults. Med Sci Sports Exerc. (2011) 43:867–76. doi: 10.1249/MSS.0b013e3181fc7162
33. Gardiner PA, Clark BK, Healy GN, Eakin EG, Winkler EAH, Owen N. Measuring older adults' sedentary time: reliability, validity, and responsiveness. Med Sci Sports Exerc. (2011) 43:2127–33. doi: 10.1249/MSS.0b013e31821b94f7
34. Herrmann SD, Hart TL, Lee CD, Ainsworth BE. Evaluation of the MyWellness Key accelerometer. Br J Sports Med. (2011) 45:109–13. doi: 10.1136/bjsm.2009.062182
35. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
36. Smith MT, Wegener ST. Measures of sleep: the insomnia severity index, medical outcomes study (MOS) sleep scale, Pittsburgh sleep diary (PSD), and Pittsburgh sleep quality index (PSQI). Arthritis Care Res. (2003) 49:S184–96. doi: 10.1002/art.11409
37. Spira AP, Beaudreau SA, Stone KL, Kezirian EJ, Lui L-Y, Redline S, et al. Reliability and validity of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older men. J Gerontol A Biol Sci Med Sci. (2012) 67:433–9. doi: 10.1093/gerona/glr172
38. Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Opler MG, et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep. (2008) 31:1087–96.
39. Silva AAd, Mello RGB de, Schaan CW, Fuchs FD, Redline S, Fuchs SC. Sleep duration and mortality in the elderly: a systematic review with meta-analysis. BMJ Open. (2016) 6:e008119. doi: 10.1136/bmjopen-2015-008119
40. Devore EE, Grodstein F, Schernhammer ES. Sleep duration in relation to cognitive function among older adults: a systematic review of observational studies. Neuroepidemiology. (2016) 46:57–78. doi: 10.1159/000442418
41. Hartigan I. A comparative review of the Katz ADL and the Barthel Index in assessing the activities of daily living of older people. Int J Older People Nurs. (2007) 2:204–12. doi: 10.1111/j.1748-3743.2007.00074.x
42. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. (2008) 40:181–8. doi: 10.1249/mss.0b013e31815a51b3
43. Schlicht W. Körperlich aktiv altern. Weinheim: Beltz Juventa (Grundlagentexte Gesundheitswissenschaften) (2013).
44. Evenson KR, Wen F, Herring AH, Di C, LaMonte MJ, Tinker LF et al. Calibrating physical activity intensity for hip-worn accelerometry in women age 60 to 91 years: the Women's health initiative OPACH calibration study. Prev Med Rep. (2015) 2:750–6. doi: 10.1016/j.pmedr.2015.08.021
45. Hall KS, Howe CA, Rana SR, Martin CL, Morey MC. METs and accelerometry of walking in older adults. Med Sci Sports Exerc. (2013) 45:574–82. doi: 10.1249/MSS.0b013e318276c73c
46. Buysse DJ, Hall ML, Strollo PJ, Kamarck TW, Owens J, Lee L, et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. (2008) 4:563–71. doi: 10.5664/jcsm.27351
47. Middelkoop HA, Smilde-van den Doel DA, Neven AK, Kamphuisen HA, Springer CP. Subjective sleep characteristics of 1,485 males and females aged 50-93: effects of sex and age, and factors related to self-evaluated quality of sleep. J Gerontol A Biol Sci Med Sci. (1996) 51:M108–15. doi: 10.1093/gerona/51A.3.M108
48. Sutter C, Zöllig J, Allemand M, Martin M. Sleep quality and cognitive function in healthy old age: the moderating role of subclinical depression. Neuropsychology. (2012) 26:768–75. doi: 10.1037/a0030033
49. Xu L, Jiang CQ, Lam TH, Liu B, Jin YL, Zhu T, et al. Short or long sleep duration is associated with memory impairment in older chinese: the Guangzhou Biobank cohort study. Sleep. (2011) 34:575–80. doi: 10.1093/sleep/34.5.575
50. Hosseini H, Esfirizi MF, Marandi SM, Rezaei A. The effect of Ti Chi exercise on the sleep quality of the elderly residents in Isfahan, Sadeghieh elderly home. Iran J Nurs Midwifery Res. (2011) 16:55–60.
51. Naylor E, Penev PD, Orbeta L, Janssen I, Ortiz R, Colecchia EF et al. Daily social and physical activity increases slow-wave sleep and daytime neuropsychological performance in the elderly. Sleep. (2000) 23:1–9. doi: 10.1093/sleep/23.1.1f
52. Woodward M. Sleep in older people. Rev Clin Gerontol. (2012) 22:130–49. doi: 10.1017/S0959259811000232
Keywords: accelerometry, Pittsburgh Sleep Quality Index, nursing home, old age health, sleep quality
Citation: Vogel O, Niederer D, Wilke J, El-Rajab I and Vogt L (2021) Habitual Physical Activity and Sleep Duration in Institutionalized Older Adults. Front. Neurol. 12:706340. doi: 10.3389/fneur.2021.706340
Received: 12 May 2021; Accepted: 28 June 2021;
Published: 27 July 2021.
Edited by:
Maurice M. Ohayon, Stanford University, United StatesReviewed by:
Barbara Galland, University of Otago, New ZealandAxel Steiger, Ludwig Maximilian University of Munich, Germany
Copyright © 2021 Vogel, Niederer, Wilke, El-Rajab and Vogt. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Oliver Vogel, dm9nZWxAc3BvcnQudW5pLWZyYW5rZnVydC5kZQ==
 Oliver Vogel
Oliver Vogel Daniel Niederer
Daniel Niederer Jan Wilke
Jan Wilke Inaam El-Rajab
Inaam El-Rajab Lutz Vogt
Lutz Vogt