- 1Department of Neurology, Headache Center North-East, University Medical Center Rostock, Rostock, Germany
- 2Institute of Medical Psychology and Medical Sociology, University Medical Center Rostock, Rostock, Germany
- 3Institute of Diagnostic and Interventional Radiology, Pediatric Radiology and Neuroradiology, University Medical Center Rostock, Rostock, Germany
Background: The care of patients with headache in the emergency department (ED) represents a diagnostic and clinical challenge. Data on the prevalence and characteristics of headache patients in purely neurological EDs are sparse. The aim of the present study is to examine patient profiles with the cardinal symptom of headache in an academic neurological ED, to analyze correlations between headache characteristics and search for differences compared to the interdisciplinary ED.
Methods: This retrospective cross-sectional study assessed all patients who presented to the ED of the Department of Neurology at Rostock University Medical Center between November 2013 and November 2016 with the main symptom of headache. Epidemiological, clinical, diagnostic data as well as key data regarding the care structure were recorded. Correlations between headache characteristics and diagnosis at discharge were analyzed and risk profiles were identified using binary logistic regression analysis.
Conclusion: This study comprehensively characterized a large collective of patients with the cardinal symptom of headache presenting to a purely neurology emergency department.
Background
Headaches are a frequent complaint and represent a major challenge in the emergency department (ED). They result in 1–4 % of all presentations in an interdisciplinary ED (1–4) and are one of the most common presenting symptoms in emergency neurological patients, accounting for 8.4–16% of visits (5). According to Goldstein et al., 2.2% of patients in American interdisciplinary EDs presented with headaches based on data of the National Hospital Ambulatory Medical Care Survey (1). In a study by Doretti et al., headaches accounted for 3.2% of visits to two EDs in Italy and Austria (6). In the interdisciplinary ED of a German university hospital, headaches were found caused 3.5% of all visits and 19% of the primary neurological presentations (7). Besides headaches, the most frequent chief neurological complaints in an interdisciplinary ED are vertigo, epileptic seizures and motor deficits (8). The prevalence of headaches in the general population is high: 5–15% for migraine, 38% for tension-type headaches, and 4% for chronic headaches (9). Only 7% of patients with migraine seek headache-specific help at the emergency department (9). As headaches
can be secondary to a serious, potentially life-threatening disease, the major challenge in the ED is to identify the patients who require further diagnostics and rapid specialist treatment from among those with the purely primary headaches. If deemed primary, the correct diagnosis according to the ICHD-3 criteria (10) is essential for correct treatment for headache specialists and neurologists, while it may be more important not to miss a secondary course for emergency physicians. Several studies have shown that primary headaches are under- and misdiagnosed in the ED inferring inadequate treatment (11–13). The proportion of secondary headaches in the ED varies from 4% to over 14% for severe headache with sudden onset (1). Various guidelines support the ED physician in the choice of additional diagnostic procedures (14–16). The concept of warning symptoms (“red flags”) has proven helpful as a decision aid. Typical “red flags” in the clarification of headaches are patient age over 50 years, immunosuppression, an abnormal neurological examination finding or additional symptoms such as fever. However, a study by Goldstein et al. 2018 also showed that a normal neurological finding in patients with headaches does not rule out a secondary headache and pathological brain imaging findings (17). The care of patients with headache in the ED represents a challenging and cost-intensive task, especially in times of increasing demand by patients (18, 19). Data on patient's characteristics in purely neurological EDs are sparse. The aim of the present study is to examine patient profiles with the main symptom of headache in a neurological ED at an academic tertiary center, and to record clinical, epidemiological as well as diagnostic data. Key data regarding the care structure are presented, correlations between headache characteristics are examined, predictors of symptomatic headaches are determined, and risk profiles for individual headache groups are developed.
Methods
This retrospective cross-sectional study assessed all patients aged at 18 years or above who presented to the neurological ED at Rostock University Medical Center between November 2013 and November 2016 with headache as main complaint. Data on administrative details were collected from the admission books for all patients. Then, the digital doctor's letters were screened for additional demographic information, previous medical history, headache characteristics, concomitant symptoms, instrumental diagnostic procedures, diagnosis at discharge. The diagnoses at discharge were categorized according to the ICHD-3 as primary and secondary headache (10). The data to be analyzed were transferred into an Excel table and a descriptive analysis of patient characteristics was conducted. The categorical data were summarized in numbers and percentages, and the continuous data according to means and standard deviations. The descriptive and exploratory statistical analyses were conducted using the statistical program SPSS 22 (IBM) and Excel (Microsoft). Differences in frequency distributions and the mean value of individual variables within comparison groups were examined using the Chi2 test or t-test. In case of ordinally scaled variables, the Kruskal-Wallis or Mann–Whitney U test were used. The statistical significance was defined as p <0.05.
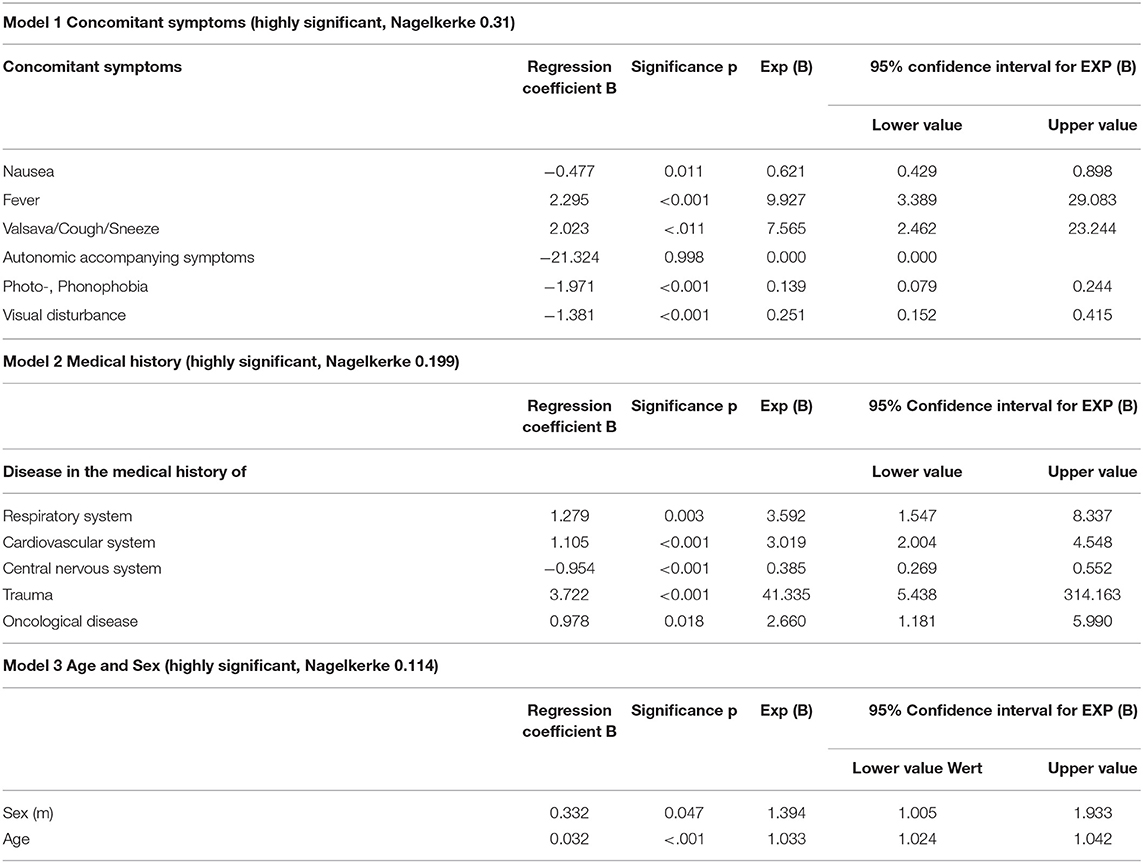
Risk profiles were developed using binary logistic regression analysis. The final diagnoses primary and secondary headache served as dependent variables as well as the independent variables age, sex, medical history (cardiovascular, oncological, autoimmune/ rheumatological, trauma, etc.), specification of headache (duration of headache, pain intensity, new onset, pain character) and concomitant symptoms (such as nausea, fever, photo-, phonophobia etc.) as possible influencing factors. The models used were highly significant with p <0.001 and had a predictive value between 0.114 and 0.311 according to Nagelkerke (R2).
The research was conducted according to the Declaration of Helsinki. The retrospective, fully anonymized analysis of data was approved by the Ethics committee of the University Medical Center Rostock (identifier: A 2018/0168).
Results
Patient Demographics and Characteristics
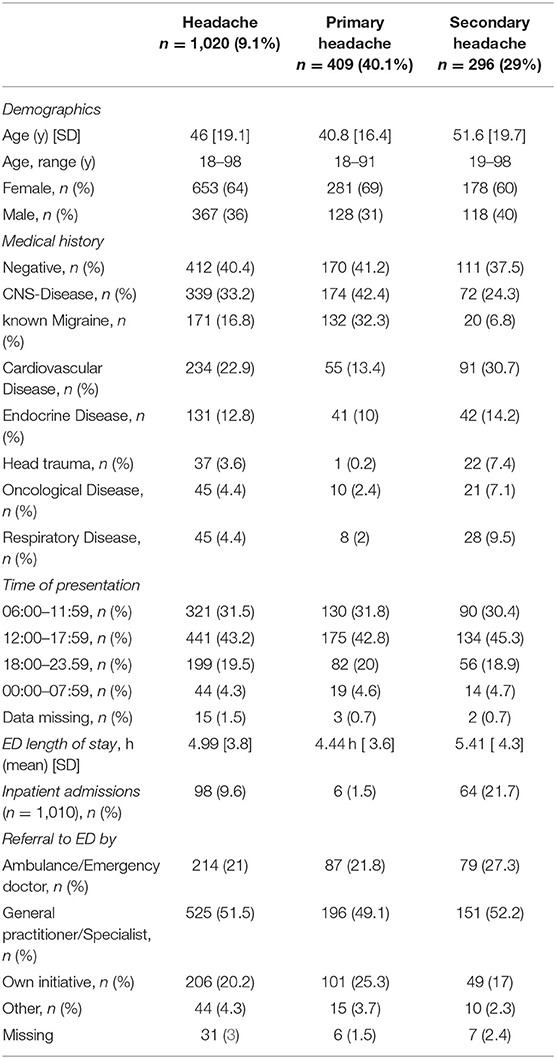
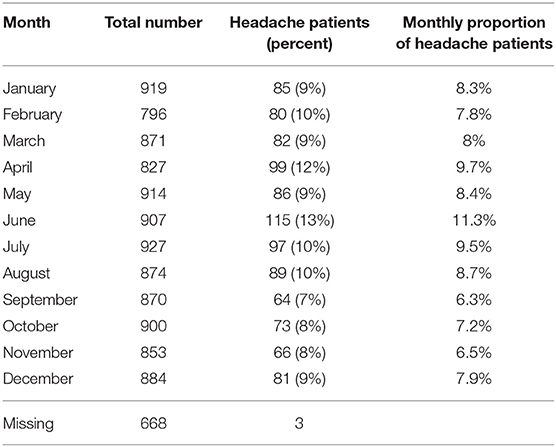
11,210 patients who presented to the neurological ED of the University Medical Center Rostock between November 2013 and November 2016 were included in the study. Thousand and twenty patients suffered from headache as their cardinal symptom. Thus, the prevalence of patients with headache in the ED was 9.1%. Their average age was 46 years (SD 19.1; range from 18 to 98) and women were more frequently affected than men (64 vs. 36%). Of the 1,020 patients, 296 (29%) had a secondary headache. These patients had a mean age of 52 years (SD 19.7 range from 19 to 88) and were older than the overall cohort of patients with headaches; 60.1% were female and 39.1% were male. Some 412 (40.4%) patients had no previous medical history. Of the various pre-existing conditions, central nervous system disorders were the most common (33.2%, n = 339), of which 171 patients (16.8%) had a known history of migraine. The second most frequent pre-existing conditions were cardiovascular diseases (22.9%; n = 234), and the third most frequent were concomitant endocrine diseases (12.8%; n = 131). The majority of patients presented to the ED with a referral or admission slip from their general practitioner/ or ambulatory-care specialist physician (51.5%, n = 525), followed by self-presentation (20.2%; n = 206) and presentations through emergency medical services (21%, n = 214). There was a significant seasonal peak of presentations to the ED in June (p = 0.005) and diurnal peak between 10 am and 1 pm (p < 0.001). The average length of stay of patients in the ED was 4.99 h (SD 3.8; median 4 h) and 9.6% (n = 98) of patients were admitted to ward for further inpatient treatment. The demographic data and medical history of patients with the cardinal symptom of headache in the ED are summarized in Table 1.
Headache Characteristics
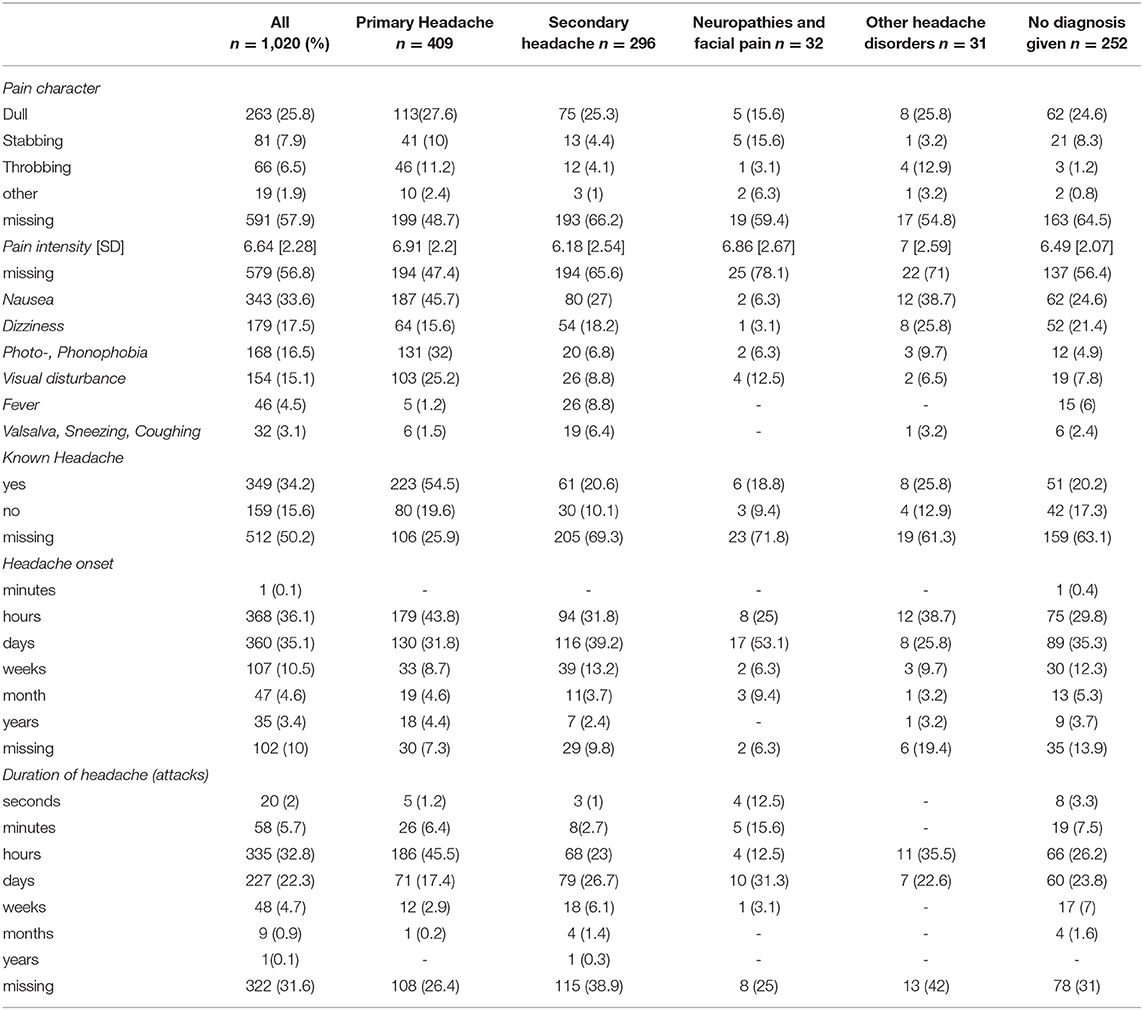
The most frequent headache characteristic was dull (25.8%, n = 263), followed by stabbing (7.9%, n = 81) and others (1.9%, n = 19), although in most cases, the character of the headache was not assessed/documented (57.9%, n = 591). The average pain intensity on the NRS (numerical rating scale) from 0 to 10 was 6.6 (SD 2.28). Stabbing headaches were significantly more frequent in the “Neuropathies and Facial pain” group (p < 0.001; for further details see Table 2). With regard to pain intensity, there was no statistically significant difference between the individual headache groups (p = 0.1). While a positive history of headaches was found in 34.2% (n = 349) patients, there was no history of headaches in 15.6% (n = 159) and no assessment respectively documentation in 50.2% (n = 512). In 78.9% (n = 805) of patients, concomitant symptoms such as nausea (33.6%, n = 343), light-headedness/vertigo (17.5%, n = 179), photo-/phonophobia (16.5%, n = 168) and visual disturbances (15.1%, n = 154) were recorded (see Table 2). The concomitant symptoms nausea, photo- and phonophobia and visual disturbances were significantly more frequent in the group with primary headache (p < 0.001).
Additional Diagnostics
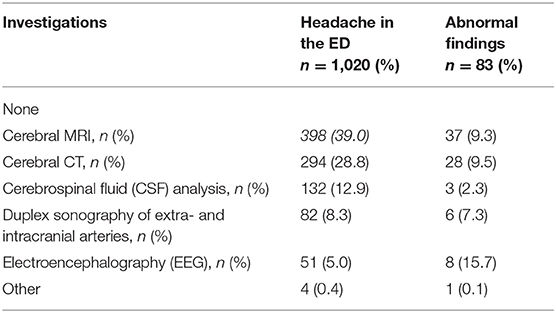
Cerebral imaging was performed in 69% (n = 704) of patients: 39 % (n = 398) received cerebral magnetic resonance imaging (head MRI) and 28.8 % (n = 294) received cerebral computed tomography (head CT). The head MRI yielded abnormal findings in 9.3 % (n = 37) of cases and the head CT yielded abnormal findings in 9.5 % (n = 28) of cases. In 12.9% (n = 132) of patients, cerebrospinal fluid (CSF) was analyzed, which was abnormal in 2.3% (n = 3) of cases. Duplex sonography of the cervical and cerebral arteries amounted to 8.3% (n = 82), with abnormal findings in six patients (7.3%), followed by electroencephalography (EEG) in 5% (n = 51) of patients with abnormal results in 8 patients (15.7%). For a summary of additional diagnostics see Table 3.
Headache Diagnoses
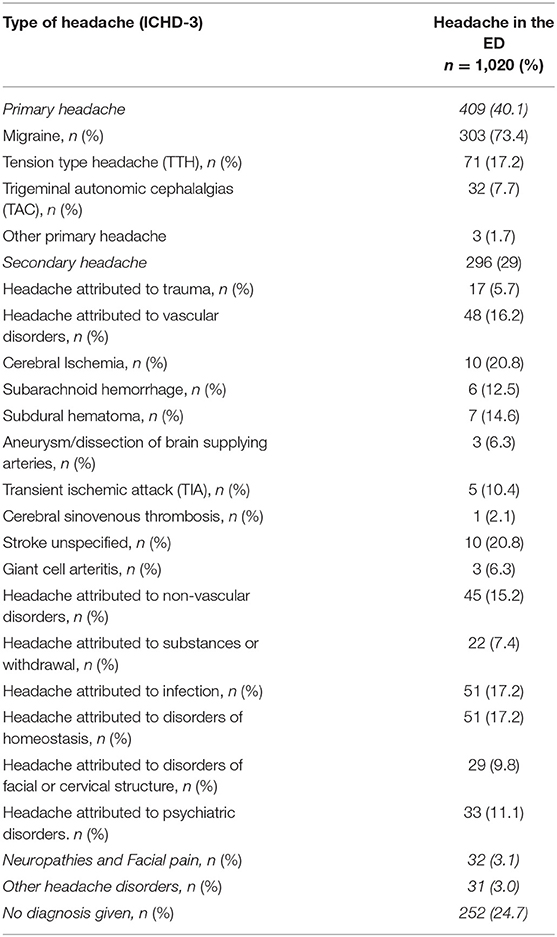
The final diagnoses according to the ICHD-3 classification are summarized in Table 4. Primary headaches were the most prevalent headache type (40.1%, n = 409), with migraine as the most frequent subtype (73.4%), followed by tension-type headache (17.2%) and trigeminal autonomic cephalalgias (7.7%). Trigeminal neuralgia was the most common type of facial pain, at 3.1% (n = 32). Patients with secondary headache formed the second-largest group, with 29% (n = 296) of patients. In 31 (3.0%) of patients, other headache disorders were diagnosed, and a total of 252 (24.7%) of patients received no final diagnosis. Of the secondary headaches, 17.2% were attributed to infection, 17.2% to disorders of electrolyte dyshomeostasis, 16.2% to vascular disorders, 15.2% to non-vascular disorders, 5.7% to trauma, 7.4% to intoxication or substance withdrawal, and 11.1% to psychiatric disorders. Among the headaches attributed to vascular diseases, 20.8% (n = 10) emerged in patients with acute cerebral ischemia, 12.5% (n = 6) in patients with subarachnoid hemorrhage, 14.6% (n = 7) in patients with subdural hematoma and 6.3% (n = 3) in patients with arterial vessel dissection.
Advanced Analyses
A comparison of age showed that patients with a primary headache were significantly younger than patients with a secondary headache (p < 0.001). Gender was unrelated to secondary headache, but in the group of primary headaches, migraines were more frequent in women (p < 0.001) while trigeminal autonomic headaches were more frequent in men (p < 0.001). With regard to the characteristics of headaches, which were only assessed in a total of 48% of the patients, it was apparent that stabbing headaches occurred significantly more frequently in the group of neuropathies and facial pain (p < 0.001). The concomitant symptoms of nausea, photo-, phonophobia and visual disturbances (p < 0.001) occurred more often in the group of primary headaches, while no significant difference was found between the groups regarding pain intensity. In patients with cardiovascular diseases, secondary headache were more prevalent (p < 0.0001). Patients with primary headache had a higher risk of having a history of CNS diseases (p < 0.0001). Of note, known migraine was also subsumed thereunder. A positive history of cerebral infarction was associated with a missing final headache diagnosis (p = 0.017). There was a significant peak of seasonal presentations to the ED in June (p = 0.005; see also Table 5) as well as diurnal presentations between 10 am and 1 pm (p < 0.001). Patients who self-presented to the ED were more likely to suffer from trigeminal neuralgia and facial pain (p = 0.001). The diagnosis of secondary headache was associated with inpatient admission of the patient (p < 0.001).
For the subsequent analysis of possible risk factors for secondary headache vs. primary headache, only patients with a formal headache diagnosis were considered. The risk of suffering from a secondary headache increased by 1.03 with every year of age (p < 0.001). A person aged 50 years or above is 2.85 times more likely to suffer from a secondary headache than someone aged below 50 years (p < 0.001), see Table 6.
Diseases of the respiratory system, cardiovascular system, oncological diseases or trauma in the medical history significantly increased the risk of secondary headaches, while a history of migraine significantly decreased it. Diseases of the respiratory system were associated with a 3.6-fold risk of secondary headache (p = 0.003), diseases of the cardiovascular system with a 3.0-fold (p < 0.001), oncological diseases with a 2.7-fold (p = 0.018) and trauma in the medical history with a 41.4-fold (p < 0.001) risk of secondary headache. For more information on the discharge diagnoses of patients with trauma in their medical history, see Supplementary Material 1. For patients with a previous neurological condition (migraine included), the risk of secondary headache was reduced by 0.39-fold (p < 0.001). Concomitant symptoms such as fever (9.93-fold, p < 0.001), aggravation of headache by sneezing/coughing or Valsalva maneuver (7.57-fold, p < 0.001) increased the risk of secondary headache, while symptoms such as nausea, photo-, phonophobia and visual disturbances were associated with a significantly lower risk (p = 0.01, p < 0.001, p < 0.001) of secondary headache, see Table 6. No significant association was found between secondary headache and data on pain character, pain intensity, suddenness of onset, duration of headache or previously experienced headache. Also, no association was found with the type of referral and presentation.
Discussion
This retrospective cross-sectional study comprehensively examined a large sample of patients presenting to a purely neurological emergency department and included 11,210 patients who presented between November 2013 and November 2016. A prevalence of 9.1% for headache as the cardinal symptom with a preponderance of female patients and an average age of 46 years was found. The prevalence reported in the literature ranged from 2.2% for North American EDs, 3.2% for hospitals in Austria and Italy, to 3% in a study from the UK (1, 6, 20). However, these frequencies pertained to interdisciplinary EDs and not a purely neurological ED as in the present study. An analysis of patient cohorts presenting to an interdisciplinary ED of a German university medical center found a headache prevalence of 3.5%, although the prevalence was substantially higher (19%) when only neurological cases were considered (7). Primary headaches were the most frequent headache type found in our study. Of these, migraine was the most frequent subtype, followed by tension-type headache and trigeminal autonomic cephalalgias. Accordingly, of all patients with headache in the ED, 29.7% suffered from migraine, which is in line with the rates of 26% (5) or 23% (21) described in other studies. A large North American epidemiological study which evaluated the data of the National Hospital Ambulatory Medical Care Survey found a higher rate of migraine patients in the ED, at 63% (1). This is probably due to the specific characteristics of the North American health system with its restricted access to outpatient care, and its reimbursement (6). The proportion of patients with secondary headache was remarkably high in our study (29%) compared to the very low secondary headache rates of 2% in interdisciplinary EDs described in the literature (1). Furthermore, a low ratio of primary to secondary headache of 9:1 was reported (7). In general, the rate of secondary headache in the ED is assumed to range between 5 and 22% (5, 22, 23). However, the reported rates are only comparable to a limited degree due to differences in the examined patient samples, corresponding health care systems, referral rates to the ED, and the differing definitions of secondary headaches in the respective studies. Nevertheless, an additional factor for the high proportion of secondary headaches in this study may be that this study was conducted in a purely neurological ED with a highly selected group of patients. Besides cerebral hemorrhage [six patients with subarachnoid hemorrhage; seven patients with subdural hematoma) there were also a high proportion of patients with cerebral ischemia (10 patients, and 10 patients with unspecified stroke as well as five patients with transient ischemic attacks (TIA)] in this group. The patients in this study with a discharge diagnosis of stroke had no obvious neurological deficits. The presenting symptom was headache. The diagnosis of stroke was made based on cerebral imaging, predominantly MRI imaging. It is a well-known finding that cerebral ischemia can be accompanied by headaches or can even be the leading clinical sign thereof. On the one hand, migraine with aura is associated with an approximately twofold increased risk of cerebral ischemia (24, 25) and on the other hand, a new-onset or concomitant secondary headache mimicking primary headaches can occur with cerebral ischemia, which is not yet sufficiently understood. The literature reports a wide range of 6–44% for the prevalence of headache associated with cerebral ischemia (26, 27). A meta-analysis by Harriott et al. found a pooled prevalence of 14%, with an increased risk of headache in the case of cerebral ischemia in the posterior circulation and for the female sex (27). An analysis of an Israeli stroke register over 2 months including 2,166 patients revealed that 8.4% had suffered from headache and cerebral ischemia, and a large proportion of 28% of patients suffered from TIA and headache (28, 29).
Detailed phenotypic data were documented in only 42% of patients, which is surprisingly low given that this information is essential for classifying the headache according to the current headache classification. This might also explain why no final diagnosis was reported in a large proportion (24.7%) of headache patients. Nevertheless, this value is still low compared to other assessments of headache patients in EDs, which reported rates of 32% (6), 36% (30) or even 44% (21) of cases in which no specific headache diagnosis was given. Primary headaches are often underdiagnosed or misdiagnosed in the ED (31). The presence/absence of important “red flags” such as thunderclap headache was also not systematically documented. Although it can be assumed that it was asked, the lack of documentation shows that standardized, structured documentation would be useful for headache patients in the ED. With regard to additional diagnostics, 69% of the patients in our study received cerebral imaging, of which 39% was made up of head MRI and 29% head CT. The high percentage of an emergency head MRI—in comparable studies 57.8% of patients received cerebral imaging but only 1.7% received head MRI (6)—is due to the high availability of MR imaging 24/7 at our department. Of the patients who underwent cerebral imaging, 9.4% had an abnormal finding, which corresponds to 6.4% of all patients with the cardinal symptom of headache. A study by Negro et al. assessing headache patients in an interdisciplinary ED in the period from 2015 to 2018 even showed that cerebral imaging was performed in 75% of cases, 6.6% of which yielded abnormal findings (32). By contrast, a large North American study which evaluated data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) found that only 14% of patients with headache who visited an ED between 1992 and 2001 underwent cerebral imaging, which yielded a pathological diagnosis in 5.5% of cases (1). In our study, after head MRI and head CT, cerebrospinal fluid diagnostics were the third most frequent diagnostics, at 12.9% (n = 132), which yielded abnormal findings in three patients (2.3%). The literature describes even lower rates of cerebrospinal fluid diagnostics in patients with headache in the ED, of 1.2% (6), and the diagnostics should be reserved for a corresponding selected group of patients. The fourth most frequent diagnostic procedure was duplex sonography of the brain-supplying arteries, which 8.3% of the patients received and which led to an abnormal finding in 7.3% of them. This examination is also useful for selected patients, e.g., to detect an arterial dissection, which was found in our study in three patients (6.3% of secondary headaches), or also in the case of a suspected giant cell arteritis, which was likewise found in three patients (6.3% of secondary headaches). Guidelines and a concept of warning symptom “red flags” are classically used to help ED physicians with the challenging task of distinguishing between primary and secondary headache. (14–16) Munoz-Ceron additionally suggests predictors of a primary headache as “green flags” (33) based on the ICHD-3 classification.
In our study we also investigated which characteristics correlate with the diagnosis of primary or secondary headache. Binary logistic regression analysis showed that the risk of suffering from a secondary headache for a patient with headache in the emergency department increases 1.03-fold (p < 0.001) with each year of age. Similar findings were obtained by Locket et al., who described a higher risk of secondary headache in patients aged over 50 years (34), as well as Munoz-Ceron et al., who found an association of secondary headaches and immunosuppression in the medical history and age over 50 years with non-primary headache (33). We also found that a history of cardiovascular diseases, disease of the respiratory system, oncological diseases or trauma in the medical history were strongly correlated with the diagnosis of secondary headache. Trauma in the medical history was even associated with a 41-fold increased risk of secondary headache. Therefore trauma, cardiovascular and respiratory diseases in patient history should also be considered “red flags,” especially since they are not yet mentioned in corresponding guidelines, except for malignancy in the medical history (14–16). Munoz-Ceron et al. assume in their study that it is not meaningful to determine frequently observed symptoms in the case of primary headache in outpatient departments, such as nausea, vertigo, photo- and phonophobia and pain intensity, and found no statistically significant correlations with concomitant symptoms (33). However, in our sample the presence of nausea, photo- and phonophobia and visual disturbances significantly correlated with primary headaches (p = 0.011 and p < 0.001). In contrast, concomitant symptoms such as fever (9.93-fold, p < 0.001), worsening of headache by sneezing/coughing or Valsalva maneuvers (7.57-fold, p < 0.001) increased the risk of secondary headache. Another important point is that, contrary to common belief, headache intensity does not differ significantly between patients with primary and secondary headaches and is not a discriminatory criterion.
Limitations
The study has several potential limitations that should be addressed. It was a retrospective cross-sectional data analysis with all problems inherent to its retrospective nature. Clinical data was collected in the ED in a busy clinical environment and documented without a uniform or standardized template in the patient record from where it extracted retrospectively. This procedure carries the risk of several systematic biases. A selection bias is, however, unlikely since the individual data records have been collected by many different doctors over a long period of time. Furthermore, this single-center study was conducted in a neurological ED in a university hospital of tertiary care and our results may not be generalized to other countries or to other EDs. Finally, a high proportion of patients presented to our neurological ED on their own initiative representing another source of bias. However, the rate of self-presentations was higher in patients with a final diagnosis of primary headaches than those with secondary headaches indicating that the patients‘ self-allocation was often purposeful.
Conclusion
This study comprehensively characterized a large sample of patients with the cardinal symptom of headache presenting to a purely neurological emergency department. The majority of patients attending the ED because of headache were suffering from primary headaches. The unusually high proportion of secondary headaches (29%) may be due to the purely neurological setting with a high prevalence of cerebrovascular disorders. Higher age and a history of cardiovascular disease, respiratory disease, oncologic disease, or head trauma, as well as distinct concomitant symptoms such as fever, worsening of headache by sneezing/coughing or Valsalva maneuvers correlated positively with the diagnosis of secondary headache.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethikkommission an der Medizinischen Fakultät der Universität Rostock St.-Georg-Str. 108 18055 Rostock. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
FR: drafted the manuscript, analysis, and interpretation and revising the manuscript. JJ: acquisition, analysis, interpretation, and revising the manuscript. PK: analysis, interpretation, and revising the manuscript. TH, AG, and UW: interpretation, and revising the manuscript. TJ: conception, analysis, interpretation and revising the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
FR served on advisory boards and/or as speaker for Allergan, Novartis, Teva, Ipsen. He has received royalties from Elsevier. PK served on advisory boards and/or as speaker for Allergan, Novartis, Teva and Lilly. UW has received speaker honoraria and travel funds from Ipsen Pharma, Merz Pharma, Allergan, Bristol-Myers Squibb, Daiichi Sankyo, Bayer Vital, Boehringer Ingelheim and Pfizer, and a research grant from Merz Pharma. He has received royalties from Thieme and Elsevier Press. He serves as editor of the European Journal of Ultrasound. TJ served on advisory boards and/or as speaker for Allergan, Autonomic Technologies, Desitin, Hormosan, Novartis, Lilly, Sanofi and Teva.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.706074/full#supplementary-material
Abbreviations
ED, Emergency department; ICHD-3, The International Classification of Headache Disorders 3rd edition; MRI, Magnetic resonance imaging; CT, Computed tomography; CSF, Cerebrospinal fluid; EEG, Electroencephalography; TIA, Transient ischemic attack; NHAMCS, National Hospital Ambulatory Medical Care Survey; ACEP, Guidelines on Acute Non-traumatic Headache Diagnosis and Management in the Emergency Department; CNS, Central nervous system; SD, Standard deviation; TTH, Tension type headache; TAC, Trigeminal autonomic cephalalgia.
References
1. Goldstein JN, Camargo CA, Pelletier AJ, Edlow JA. Headache in United States emergency departments: demographics, work-up and frequency of pathological diagnoses. Cephalalgia. (2006) 26:684–90. doi: 10.1111/j.1468-2982.2006.01093.x
2. Locker T, Mason S, Rigby A. Headache management–are we doing enough? An observational study of patients presenting with headache to the emergency department. Emerg Med J. (2004) 21:327–32. doi: 10.1136/emj.2003.012351
3. Ramirez-Lassepas M, Espinosa CE, Cicero JJ, Johnston KL, Cipolle RJ, Barber DL. Predictors of intracranial pathologic findings in patients who seek emergency care because of headache. Arch Neurol. (1997) 54:1506–9. doi: 10.1001/archneur.1997.00550240058013
4. Giamberardino MA, Affaitati G, Costantini R, Guglielmetti M, Martelletti P. Acute headache management in emergency department. A narrative review. Intern Emerg Med. (2020) 15:109–17. doi: 10.1007/s11739-019-02266-2
5. Schankin CJ, Straube A, Bassetti CL, Fischer U. Headache in the emergency department. Nervenarzt. (2017) 88:597–606. doi: 10.1007/s00115-017-0335-x
6. Doretti A, Shestaritc I, Ungaro D, Lee J-I, Lymperopoulos L, Kokoti L, et al. Headaches in the emergency department -a survey of patients' characteristics, facts and needs. J Headache Pain. (2019) 20:100. doi: 10.1186/s10194-019-1053-5
7. pubmeddev KK, et al. Differenzialdiagnose und Notfallversorgung akuter Kopfschmerzen. - PubMed - NCBI. Available online at: https://www.ncbi.nlm.nih.gov/pubmed/29621823 (accessed Feb 11, 2020).
8. Royl G, Ploner CJ, Möckel M, Leithner C. Neurological chief complaints in an emergency room. Nervenarzt. (2010) 81:1226–30. doi: 10.1007/s00115-010-3020-x
9. Friedman BW, Serrano D, Reed M, Diamond M, Lipton RB. Use of the emergency department for severe headache. A population-based study. Headache. (2009) 49:21–30. doi: 10.1111/j.1526-4610.2008.01282.x
10. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders 3rd edition. Cephalalgia. (2018) 38:1–211. doi: 10.1177/0333102417738202
11. Valade D, Lucas C, Calvel L, Plaisance P, Derouet N, Meric G, et al. Migraine diagnosis and management in general emergency departments in France. Cephalalgia. (2011) 31:471–80. doi: 10.1177/0333102410378178
12. Blumenthal HJ, Weisz MA, Kelly KM, Mayer RL, Blonsky J. Treatment of primary headache in the emergency department. Headache. (2003) 43:1026–31. doi: 10.1046/j.1526-4610.2003.03202.x
13. Gupta MX, Silberstein SD, Young WB, Hopkins M, Lopez BL, Samsa GP. Less is not more: underutilization of headache medications in a university hospital emergency department. Headache. (2007) 47:1125–33. doi: 10.1111/j.1526-4610.2007.00846.x
14. Peretz A, Dujari S, Cowan R, Minen M. ACEP guidelines on acute non-traumatic headache diagnosis and management in the emergency department, commentary on behalf of the refractory, inpatient, emergency care section of the American headache society. Headache. (2020). 60:643–6. doi: 10.1111/head.13744
15. Leitlinie_Diagnostik_Zusatzuntersuchungen_bei_Kopfschmerzen_2017.pdf. Available online at: http://www.dmkg.de/files/dmkg.de/Empfehlungen/Leitlinie_Diagnostik_Zusatzuntersuchungen_bei_Kopfschmerzen_2017.pdf (accessed Apr 21, 2020).
16. Mitsikostas DD, Ashina M, Craven A, Diener HC, Goadsby PJ, Ferrari MD, et al. European Headache Federation consensus on technical investigation for primary headache disorders. J Headache Pain. (2015) 17:5. doi: 10.1186/s10194-016-0596-y
17. Goldstein L, Laytman T, Steiner I. Is head computerized tomography indicated for the workup of headache in patients with intact neurological examination. Eur Neurol. (2018) 80:341–4. doi: 10.1159/000496805
18. Di Somma S, Paladino L, Vaughan L, Lalle I, Magrini L, Magnanti M. Overcrowding in emergency department: an international issue. Intern Emerg Med. (2015) 10:171–5. doi: 10.1007/s11739-014-1154-8
19. Hooker EA, Mallow PJ, Oglesby MM. Characteristics and trends of emergency department visits in the United States (2010-2014). J Emerg Med. (2019) 56:344–51. doi: 10.1016/j.jemermed.2018.12.025
20. Knox J, Chuni C, Naqvi Z, Crawford P, Waring W. Presentations to an acute medical unit due to headache: a review of 306 consecutive cases. Acute Med. (2012) 11:144–9. doi: 10.52964/AMJA.0563
21. Chu KH, Howell TE, Keijzers G, Furyk JS, Eley RM, Kinnear FB, et al. Acute headache presentations to the emergency department: a statewide cross-sectional study. Acad Emerg Med. (2017) 24:53–62. doi: 10.1111/acem.13062
22. Royl G, Ploner CJ, Leithner C. Headache in the emergency room: the role of immigrant background on the frequency of serious causes and diagnostic procedures. Neurol Sci. (2012) 33:793–9. doi: 10.1007/s10072-011-0830-y
23. Sahai-Srivastava S, Desai P, Zheng L. Analysis of headache management in a busy emergency room in the United States. Headache. (2008) 48:931–8. doi: 10.1111/j.1526-4610.2008.01156.x
24. Kurth T, Diener H-C. Migraine and stroke: perspectives for stroke physicians. Stroke. (2012) 43:3421–6. doi: 10.1161/STROKEAHA.112.656603
25. Mawet J, Kurth T, Ayata C. Migraine and stroke: in search of shared mechanisms. Cephalalgia. (2015) 35:165–81. doi: 10.1177/0333102414550106
26. Arboix A, Massons J, Oliveres M, Arribas MP, Titus F. Headache in acute cerebrovascular disease: a prospective clinical study in 240 patients. Cephalalgia. (1994) 14:37–40. doi: 10.1046/j.1468-2982.1994.1401037.x
27. Harriott AM, Karakaya F, Ayata C. Headache after ischemic stroke: A systematic review and meta-analysis. Neurology. (2020) 94:e75–86. doi: 10.1212/WNL.0000000000008591
28. Pollak L, Shlomo N, Korn Lubetzki I. National acute stroke israeli survey group. Headache in stroke according to National Acute Stroke Israeli Survey. Acta Neurol Scand. (2017) 135:469–75. doi: 10.1111/ane.12621
29. Lebedeva ER, Ushenin AV, Gurary NM, Gilev DV, Olesen J. Sentinel headache as a warning symptom of ischemic stroke. J Headache Pain. (2020) 21:70. doi: 10.1186/s10194-020-01140-3
30. Friedman BW, Hochberg ML, Esses D, Grosberg B, Corbo J, Toosi B, et al. Applying the International Classification of Headache Disorders to the emergency department: an assessment of reproducibility and the frequency with which a unique diagnosis can be assigned to every acute headache presentation. Ann Emerg Med. (2007) 49:409–19. doi: 10.1016/j.annemergmed.2006.11.004
31. Luciani M, Negro A, Spuntarelli V, Bentivegna E, Martelletti P. Evaluating and managing severe headache in the emergency department. Expert Rev Neurother. (2021) 21:277–85. doi: 10.1080/14737175.2021.1863148
32. Negro A, Spuntarelli V, Sciattella P, Martelletti P. Rapid referral for headache management from emergency department to headache center: four years data. J Headache Pain. (2020) 21:25. doi: 10.1186/s10194-020-01094-6
33. Munoz-Ceron J, Marin-Careaga V, Peña L, Mutis J, Ortiz G. Headache at the emergency room: Etiologies, diagnostic usefulness of the ICHD 3 criteria, red and green flags. PLoS ONE. (2019) 14:e0208728. doi: 10.1371/journal.pone.0208728
Keywords: headache, emergency department, primary headache, migraine, secondary headache
Citation: Rimmele F, Janke J, Kropp P, Grossmann A, Hamann T, Walter U and Jürgens TP (2021) Headache Characteristics in the Neurological Emergency Department: A Retrospective Study. Front. Neurol. 12:706074. doi: 10.3389/fneur.2021.706074
Received: 06 May 2021; Accepted: 28 July 2021;
Published: 19 August 2021.
Edited by:
Chirstian Wöber, Medical University of Vienna, AustriaReviewed by:
Paolo Martelletti, Sapienza University of Rome, ItalyJonathan Edlow, Beth Israel Deaconess Medical Center and Harvard Medical School, United States
Copyright © 2021 Rimmele, Janke, Kropp, Grossmann, Hamann, Walter and Jürgens. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Florian Rimmele, Zmxvcmlhbi5yaW1tZWxlQG1lZC51bmktcm9zdG9jay5kZQ==
 Florian Rimmele
Florian Rimmele Josephine Janke
Josephine Janke Peter Kropp
Peter Kropp Annette Grossmann3
Annette Grossmann3 Uwe Walter
Uwe Walter Tim P. Jürgens
Tim P. Jürgens