
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Neurol., 25 March 2021
Sec. Neurorehabilitation
Volume 12 - 2021 | https://doi.org/10.3389/fneur.2021.646902
This article is part of the Research TopicCOVID-19: The Neurorehabilitation PerspectiveView all 26 articles
 Marta Matamala-Gomez1*
Marta Matamala-Gomez1* Sara Bottiroli2,3
Sara Bottiroli2,3 Olivia Realdon1
Olivia Realdon1 Giuseppe Riva4,5
Giuseppe Riva4,5 Lucia Galvagni6
Lucia Galvagni6 Thomas Platz7,8
Thomas Platz7,8 Giorgio Sandrini3,9
Giorgio Sandrini3,9 Roberto De Icco3,9
Roberto De Icco3,9 Cristina Tassorelli3,9
Cristina Tassorelli3,9In catastrophic situations such as pandemics, patients' healthcare including admissions to hospitals and emergency services are challenged by the risk of infection and by limitations of healthcare resources. In such a setting, the use of telemedicine interventions has become extremely important. New technologies have proved helpful in pandemics as a solution to improve the quality of life in vulnerable patients such as persons with neurological diseases. Moreover, telemedicine interventions provide at-home solutions allowing clinicians to telemonitor and assess patients remotely, thus minimizing risk of infection. After a review of different studies using telemedicine in neurological patients, we propose a telemedicine process flow for healthcare of subjects with chronic neurological disease to respond to the new challenges for delivering quality healthcare during the transformation of public and private healthcare organizations around the world forced by COVID-19 pandemic contingency. This telemedicine process flow represents a replacement for in-person treatment and thereby the provision equitable access to the care of vulnerable people. It is conceptualized as comprehensive service including (1) teleassistance with patient counseling and medical treatment, (2) telemonitoring of patients' health conditions and any changes over time, as well as (3) telerehabilitation, i.e., interventions to assess and promote body functions, activities, and consecutively participation. The hereby proposed telemedicine process flow could be adopted on a large scale to improve the public health response during healthcare crises like the COVID-19 pandemic but could equally promote equitable health care independent of people's mobility or location with respect to the specialized health care center.
On 20 March 2020, the World Health Organization (WHO) declared the pandemic state due to the spread of SARS-CoV-2 (1). In December 2020, more than 72 million subjects had been diagnosed with COVID-19 over the world, and more than 1.5 million of them had died (2). Due to the lack of an effective medical treatment to fight against the SARS-CoV-2, the healthcare measures mainly focused on symptomatic treatment, social distancing, use of device for individual protection, and the mandatory quarantine after being in close contact with an infected person (2). In this setting, medical visits, non-urgent treatments, and non-urgent medical issues, particularly for vulnerable subjects such as persons with neurological disorders, were initially interrupted and then re-assumed but frequently with a reduced scope. These measures have inevitably created long waiting lists and delays on medical visits, thus ultimately affecting patients' quality of life. Nevertheless, some preliminary efforts for maintaining the standard of care in the field of neurorehabilitation have been proposed (3, 4). Notably, the pandemic has also posed ethical questions for the healthcare system and the clinicians themselves (5). For instance, doctors had to face the dilemma of who can be treated at the hospital or at home, or who can be admitted to the limited number of beds in the intensive care units (ICU). Ultimately, in some areas, the most difficult question became how to fairly distribute scarce life-supporting clinical resources with implications for COVID-19 survivals. People with a severe chronic neurological condition who depend on a caregiver for their needs and/or to carry out their daily life routine had to face a difficult situations during the pandemic (5). COVID-19 is particularly lethal for the elderly with pre-existing conditions such as neurodegenerative and neuropsychiatric disorders, as they are a vulnerable population needing continuous supervision (6–8).
In times of stressed healthcare resources, the public health guidelines endorse the priority of treatment to those who are at short-term risk of death (9, 10). Moreover, the argument exists that young people should have priority over elderly people, even though whether and how this rule should be implemented is still controversial (10, 11). It must be noted that only a minority of people testing positive for SARS-CoV-2 become severely ill (12). Most people affected by COVID-19 present with mild symptoms and recover over a few days or weeks. From a healthcare point of view, this situation demands new ways to monitor the clinical situation of a large number of subjects at home. In addition, COVID-19 persons may develop a post-intensive care syndrome, presenting motor, cognitive, and emotional disorders, requiring an intensive rehabilitation program and a long-term supervision (13, 14). In patients with neurological disorders, the chronic persistence of COVID-19 have led to re-organized neurorehabilitation services accordingly (15, 16). In this regard, the use of new telecommunication technologies integrating telemedicine systems represents an alternative solution to facilitate the exchange between the healthcare providers and the patients (17, 18). Recently, some investigations reported the effectiveness of telemedicine services in remotely assisting, monitoring, and treating COVID-19 subjects or other diseases (17, 19–27). Indeed, a well-organized network could have the potential to reduce case fatality or at least provide a better management and supervision of the clinical conditions of vulnerable patients, such as those with neurological disorders, during the COVID-19 pandemic (28).
In this perspective article, we propose a telemedicine process flow representing a viable alternative to respond to the new challenges for patient care forced by the transformation of public and private healthcare organizations due to the COVID-19 pandemic. This network will represent a replacement for in-person treatment, providing equitable access to care for vulnerable people, including subjects with chronic neurological disorders. Such a network, which can be time- and cost-saving in normal situations, may feature two important added values: (1) safety and (2) access to care for a wider number of subjects.
In the ‘70s, Thomas Bird introduced the term “telemedicine,” meaning “healing at a distance,” which implies the delivery of healthcare services by using telecommunication technologies (29–31). Specifically, telemedicine interventions aim to facilitate healthcare treatment, limiting or avoiding hospitalization (29). More recently, WHO described “telemedicine” or “e-Health” as the use of technology related to informatics and telecommunication, i.e., information and communication technologies (ICT), directed to provide a positive effect in the patient’s health status (32). The main goals of telemedicine are to (1) improve the access to health care for rural areas, (2) give the physicians better access to tertiary consultation, (3) allow physicians to conduct remote examinations, (4) reduce health-care costs, (5) provide health-care services to a larger geographic region and or population, (6) reduce the need to transfer patients to the care centers, and (7) improve patient care (33).
During the COVID-19 pandemic, telemedicine represents an additional solution for healthcare services, allowing to deliver them directly at patient's home, reducing risks of possible infections, and enabling virtual triage to mitigate the negative psychological effects of social isolation (34). Then, with the current limitations in assisting patients at the hospital, the use of new telecommunication technologies by means of integrating telemedicine systems into the clinical routine may facilitate the maintenance of the remote relationship between healthcare providers and neurological patients (17, 35, 36). In this framework, the concept of “telemedicine” involves three treatment categories allowing to assist, monitor, and counseling patient remotely: (1) tele-assistance, (2) telemonitoring, and (3) telerehabilitation (37, 38). In the following section, we will discuss the three concepts embedded in the “telemedicine” overarching concept.
The concept of tele-assistance refers to the use of new technologies for patients' counseling at a distance. There are different modalities for providing tele-assistance: video-conferencing, e-mail, on-line chat sessions, forums, telephone calls, and mobile phone messages (39). A large number of studies have demonstrated the effectiveness of tele-assistance when dealing with patients with chronic disorders, such as cancer (40), diabetes (41), chronic respiratory failure (42), cystic fibrosis (43), brain injury (44), chronic pain (45), and stroke (46). For instance, a recent study demonstrated the effectiveness of tele-assistance at improving quality of life in people suffering from neuromuscular diseases (39). In this study, 24 participants with neuromuscular diseases were assisted through video-conferencing sessions in an on-line psychosocial program lasting 3 months. Participants reported benefits in some psychosocial variables as “getting along with people,” “psychosocial domain,” and “life activities” when compared to a control group (39). Others used a tele-assistance integrated care intervention to monitor patients with amyotrophic lateral sclerosis by using telephone calls, showing important time- and cost-saving benefits (47). One of the most useful features of tele-assistance is the possibility to support patients comprehensively from symptom onset to medical treatment delivery. For instance, a tele-assistance protocol—consisting in phone and video-conferencing connection between the ICU ambulance and the clinicians at the hospital—reduced the waiting time from symptom onset to treatment delivery in patients with stroke (48). This approach could be particularly useful at the time of the COVID-19, allowing the clinicians to assist and counsel patients at a distance, sending the clinical staff for the treatment delivery directly at their homes if and when necessary, thus avoiding the presence of the patients at the hospital.
The concept of telemonitoring is defined as the use of information provided by the technology to monitor the patient's health state at a distance (49, 50). Telemonitoring systems are promising approaches able to reduce clinical complications in chronic patients (49), as in case of neurological disorders. For instance, it has been effectively used in patients with neuromuscular diseases (51, 52) and multiple sclerosis (MS) (53). Telemonitoring systems consist in the biometric tracking and transmission to the clinicians of physiological and/or behavioral data of the patients (e.g., heart rate, breathing rate, gait pattern, motor functions, etc.) in synchronous or asynchronous videoconferencing (54). Telemonitoring has also been proposed to deliver new data necessary for differential diagnosis or to stage illnesses in a health telematic network (55). Recently, telemonitoring has been used in patients with confirmed or suspected COVID-19 remotely, allowing for the timely identification of worsening symptoms (56). This approach seems particularly useful for telemonitoring COVID-19 patients with other chronic or high-risk pathologies (e.g., multiple sclerosis, Parkinson's disease, and myasthenia gravis) as it would limit the number of hospitalizations, optimize healthcare resources, and reduce the risk of virus transmission.
Telerehabilitation (TR) is a young telemedicine subfield consisting in the use of new telecommunication-based practices for controlling and conducting rehabilitation at a distance (57). TR can be used in all those situations in which the patient and the therapist cannot be in the same location. TR allows to begin the rehabilitation process as soon as possible after hospital discharge and increases the care access to individuals who are home-forced or geographically remote from their healthcare service (58–60). Hence, TR-based systems represent solid solutions to treat patients with an alternative way compared to the traditional face-to-face approach (58), providing benefits for the healthcare system and patients in terms of cost-effectiveness and feasibility for large-scale implementations. To this end, TR can use different types of technologies, such as sensor-based technology, tele/video-conference, specific ad hoc software, or virtual reality (61). Moreover, it has been shown that through telerehabilitation systems it is possible to foster patient motivation and participation in their own rehabilitation process (62), thus improving their well-being (63). TR may be useful for the treatment of motor, cognitive, or psychological deficits. Preliminary evidence indeed suggests its application in stroke, cerebral palsy, traumatic brain injury, multiple sclerosis (MS), and Parkinson's disease (PD), in particular as for treating motor- and speech-related impairments (54–58). TR has also been used for cognitive deficits (64) associated to neurological diseases, such as stroke, MS, brain tumors, Alzheimer's disease, and mild cognitive impairment (60–63, 65, 66).
In line with the necessary adaptation of healthcare services to the COVID-19, TR technological solutions are increasingly considered as potentially effective options for continuing the rehabilitation process at a distance (45, 67–70). Currently, many efforts are now focused on the treatment of subjects recovering from COVID-19 (71–74), but it seems extremely important to implement TR protocols also in non-COVID subjects in various settings of neurological care, in order to provide a continuity of care during this pandemic contingency and possibly in the future (75–78). During the COVD-19 pandemic, we have tested an innovative TR approach for the remote treatment of cognitive deficits in neurodegenerative diseases (79, 80) called HomeCoRe (Home Cognitive Rehabilitation) (81). HomeCoRe is a patient-tailored intervention stimulating many cognitive abilities, which is the home-based version of a previously tested computer-based cognitive training program (CoRe) (82–85), devised for the hospital setting. The system proved useful for providing continuity of care after hospital discharge in a condition of safety and distance and thus can be incorporated into clinical routine protocols.
Even though telemedicine interventions clearly have limitations compared to a hands-on approach in medicine (86, 87), the development of new technologies has also advantages over face-to-face health care, e.g., it allows the clinicians to follow the patients in a synchronous or asynchronous way. Synchronous telemedicine refers to the intervention performed in real time through a video call that can be conducted through a smartphone or a webcam connected to the computer (88). Asynchronous telemedicine interventions refer to the “store-and-forward” technologies, which allow monitoring and collection of physiological and/or behavioral data through wearable or implantable devices connected to an online or virtual platform and then sending the information to a clinical center for review and consultation (88, 89). The most common technological solutions used to provide telemedicine interventions are smartphones, tablets, and wearable sensors (90), including digital applications for self-exercises or monitoring the behavioral or physiological state of the patients (91). However, in the last 20 years, some telemedicine interventions have integrated the use of virtual reality (VR) platforms to deliver personalized rehabilitation training or clinical interventions at a distance (92–94). In some instances, VR can provide full-immersed virtual environments where the patient can feel present (being there) inside the virtual environment (95, 96). In the proposed process flow, VR can be used as an advanced communication interface, in which the patient can interact with different sensory information coming from different modalities, while performing specific rehabilitation tasks within the VR environment. VR systems enable a more intuitive mode of interacting with information, for the clinicians and the patients (63, 92, 97–100).
One of the main advantages of VR is that, through the use of virtual avatars, it is possible to induce virtual body ownership illusions toward the virtual body (physical possession of the virtual body) (101). During the last years, some investigations attempted to use virtual body ownership illusion for rehabilitation purposes in chronic patients (102–111). Some investigations proposed the integration of virtual body ownership illusions within a VR training for telemedicine purposes (100, 112). However, to the best of our knowledge, a comprehensive integrated telemedicine platform that provides synchronous and asynchronous interventions by means of VR, virtual body ownership illusions, and wearable sensors for real-time telemonitoring has neither been created nor tested. In the next paragraph, we propose an integrated telemedicine system for assisting, monitoring, and treating subjects with chronic neurological diseases during this pandemic situation and beyond.
Telemedicine services have the potential to provide medical service at a distance and in some instances even to save lives, while allowing patients and clinicians to be in touch safely (113). For this reason, many public health systems worldwide have been seeking for qualified and certified digital medical services to provide a continuity of care at a distance (114). However, most of the countries were unprepared for managing patients with a modern digital approach (113, 115–117). To facilitate the process, at the beginning of 2020, the American Medical Association wrote a telehealth implementation playbook with the definitions of “telehealth” or “telemedicine” as follows: (1) real-time video-conferencing between the patients and the clinicians being in different locations; (2) image and data collection stored and forwarded for the later data interpretation; (3) remote patient's monitoring through the use of mobile health tools, wearable sensors, and devices; and (4) virtual checks through phone calls, messaging, or videoconferencing (118). It must be noted that the definition did not include motor or cognitive rehabilitation based on digital platforms during and beyond the COVID-19.
Based in the above-commented literature and after a review of different studies using telemedicine for remote monitoring and intervention in patients with neurological disorders, here, we propose a telemedicine process flow for remotely managing patients with neurological disorders by including the following components: (1) tele-assistance or patient counseling: weekly or monthly videoconferencing with a health care provider that is tailored for the patient disorder; (2) telerehabilitation: reminder and performance of physical, communicative, and/or cognitive rehabilitation assessment and training through the digital platform; (3) telemonitoring: remote monitoring of the behavioral or physiological responses through the wearable sensors connected to the digital platform; (4) interpretation of stored data by the clinicians; and (5) virtual follow-up: virtual checks between the patients and the healthcare provider for adjusting the healthcare routine based on data interpretation. All these components will create a closed-loop telemedicine process flow, where the clinicians are enabled to visit and monitor a large number of patients with a virtual face-to-face approach through videoconferencing, thus reducing the need of transportation (of people with mobility restrictions) and avoiding the risk of infection on both ends in case of particular emergencies (Figure 1). Moreover, the telemedicine process flow can facilitate the active involvement of both the patients themselves and their caregivers in the healthcare process, which is a crucial element when dealing with telemedicine solutions for managing vulnerable populations in need of continuous supervision. The proposed telemedicine process flow would also enable clinicians to detect early sign or symptoms of COVID-19. The telemedicine process flow should be based on easy-to-use and accessible technology such as smartphones or tablets, integrated with a VR platform to conduct the healthcare routine. The same devices could also be used for telemonitoring patients' physiological or behavioral responses. Even though the proposed telemedicine intervention would be very helpful for managing patients during the COVID-19 pandemic, this telemedicine process flow can be also applied in normal circumstances avoiding or reducing patients' need for transportation or hospitalization and allowing clinicians to follow their patients at a distance, where in-person evaluations can be also considered as a complement of the telemedicine intervention. This could implement patients' engagement and activation (119).
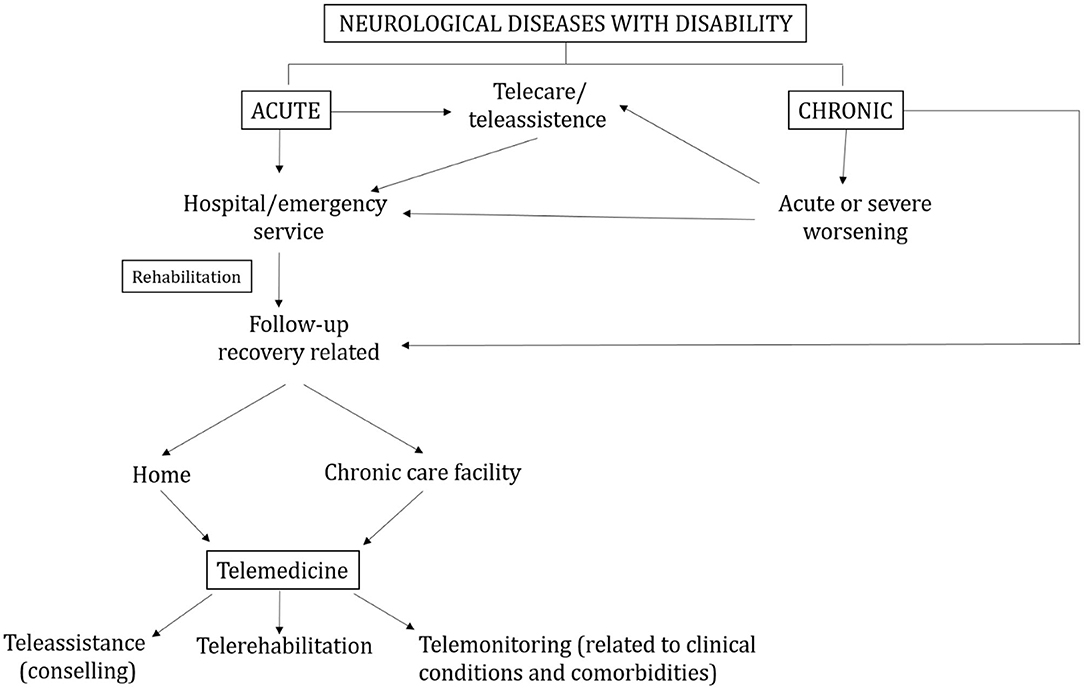
Figure 1. Flow chart of the clinical and telemedicine pathways in patients with acute or chronic neurological diseases.
Even though the proposed telemedicine intervention can be an optimal solution for monitoring and treating patients at a distance during a pandemic situation, the proposed telemedicine process flow still presents some limitations. A limitation is the availability of easy-to-use technology to deliver tele-consultations or for monitoring the patient's behavioral or physiological responses. Such limitations have been also suggested in earlier studies (36). Moreover, the performance of the training routine alone can represent some risk for the patients such as patient's falls or a bad performance of the exercises. Further, still, there is a lack of standardized tools to be used for virtual reality training and remote monitoring.
The COVID-19 pandemic has created new challenges to patient care, imposing adaptation of healthcare facilities. ICT can be extremely useful in this adaptation process and also to maintain people connected with the world (120). These adaptations should be extended to the delivery of care for neurological diseases. Here, we proposed a telemedicine process flow for healthcare of subjects with chronic neurological disease. In the future, this telemedicine process flow could be implemented and applied on a large scale not only to improve the public health capacity and to allow clinicians to deliver good quality care in case of particular emergencies such as COVID-19 but also to provide equitable health care for patients with mobility restrictions or living remotely from specialized health care centers. Even though the proposed telemedicine process flow could lead to an improvement of the public health management, some limitations should be considered.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
GS, MM-G, and SB contributed to the conceptualization of the manuscript and bibliographic review. MM-G, SB, and RD contributed to the writing. GR and OR contributed to the bibliographic review and writing of the manuscript. LG contributed to the bibliographic suggestions and the revision of the manuscript. CT, GS, and TP contributed to the supervision of the manuscript. All authors approved the final version of the manuscript for submission.
This work was funded by the Current Research Fund of the Italian Ministry of Health to the National Neurological Institute C. Mondino Foundation (Ricerca Corrente 2020) and supported by the BDH Bundesverband Rehabilitation e.V. (charity for neuro-disabilities) by a non-restricted personal grant to TP.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. WHO. WHO Director-General's Opening Remarks at the Mission Briefing on COVID-19 (2020). Available online at: https://www.who.int/directorgeneral/speeches/detail/who-director-general-s-opening-remarks-at-themission-briefing-on-covid-19---12-march-2020 (accessed March 12, 2020)
2. Centers for Disease Control and Prevention. Public Health Recommendations for Community-Related Exposure. (2020). Available online at: www.cdc.gov/coronavirus/2019-ncov/php/public-health-recommendations.html (cited July 23, 2020).
3. Buonomo A, Brescia Morra V, Zappulo E, Lanzillo R, Gentile I, Montella E, et al. COVID-19 prevention and multiple sclerosis management: The SAFE pathway for the post-peak. Multiple Scleros Relat Disord. (2020) 44:102282. doi: 10.1016/j.msard.2020.102282
4. Leocani L, Diserens K, Moccia M, Caltagirone C. Disability through COVID-19 pandemic: neurorehabilitation cannot wait. Eur J Neurol. (2020) 27:e50–1. doi: 10.1111/ene.14320
5. Kim SYH, Grady C. Ethics in the time of COVID: what remains the same and what is different. Neurology. (2020) 94:1007–8. doi: 10.1212/WNL.0000000000009520
6. Banerjee D. “Age and ageism in COVID-19:” Elderly mental health-care vulnerabilities and needs. Asian J Psychiatry. (2020) 51:102154. doi: 10.1016/j.ajp.2020.102154
7. Banerjee D. The impact of Covid-19 pandemic on elderly mental health. Int J Geriatr Psychiatry. (2020) 35:1466–7. doi: 10.1002/gps.5320
8. Korczyn AD. Dementia in the COVID-19 Period. J Alzheimer's Dis. (2020) 75:1253–61. doi: 10.3233/JAD-200609
9. Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. (2020) 382:2049–55. doi: 10.1056/NEJMsb2005114
10. White DB, Katz MH, Luce JM, Lo B. Who should receive life support during a public health emergency? Using ethical principles to improve allocation decisions. Ann Intern Med. (2009) 150:132–8. doi: 10.7326/0003-4819-150-2-200901200-00011
11. Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet. (2009) 373:423–31. doi: 10.1016/S0140-6736(09)60137-9
12. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX. WHO-China-Joint-Mission. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Anaesthesiol Intensive Ther. (2020) 382:56–63.
13. Bryant SE, McNabb K. Postintensive Care Syndrome. Crit Care Nurs Clin N Am. (2019) 31:507–16. doi: 10.1016/j.cnc.2019.07.006
14. Morone G, Matamala-Gomez M, Sanchez-Vives M V, Paolucci S, Iosa M. Watch your step! Who can recover stair climbing independence after stroke? Eur J Phys Rehabil Med. (2018) 54:811–8. doi: 10.23736/S1973-9087.18.04809-8
15. Bartolo M, Intiso D, Lentino C, Sandrini G, Paolucci S, Zampolini M, et al. Urgent measures for the containment of the coronavirus (Covid-19) epidemic in the neurorehabilitation/rehabilitation departments in the phase of maximum expansion of the epidemic. Front Neurol. (2020) 11:423. doi: 10.3389/fneur.2020.00423
16. Salvia A, Morone G, Iosa M, Balice MP, Paolucci S, Grasso MG, et al. An Italian neurorehabilitation hospital facing the SARS-CoV-2 pandemic: data from 1207 patients and workers. Front Neurol. (2020) 11:1218. doi: 10.3389/fneur.2020.584317
17. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. (2020) 382:1679–81. doi: 10.1056/NEJMp2003539
18. Sene A, Kamsu-Foguem B, Rumeau P. Telemedicine framework using case-based reasoning with evidences. Comput Methods Programs Biomed. (2015) 121:21–35. doi: 10.1016/j.cmpb.2015.04.012
19. Matamala-Gomez M, De Icco R, Sandrini G. Telemedicina e realtà virtuale ai tempi della pandemia da Covid-19. Confinia Cephalal Neurol. (2020) 30:79–83.
20. Tozzi AE, Gesualdo F, D'Ambrosio A, Pandolfi E, Agricola E, Lopalco P. Can digital tools be used for improving immunization programs? Front Public Health. (2016) 4:36. doi: 10.3389/fpubh.2016.00036
21. Woodall T, Ramage M, LaBruyere JT, McLean W, Tak CR. Telemedicine services during COVID-19: considerations for medically underserved populations. J Rural Health. (2020) 37:231–4. doi: 10.1111/jrh.12466
22. Soares WB, Silvestre IT, Lima AM, de O, de Almondes KM. The influence of telemedicine care on the management of behavioral and psychological symptoms in dementia (BPSD) Risk factors induced or exacerbated during the COVID-19 pandemic. Front Psychiatry. (2020) 11:577629. doi: 10.3389/fpsyt.2020.577629
23. Maresca G, Maggio MG, De Luca R, Manuli A, Tonin P, Pignolo L, et al. Tele-neuro-rehabilitation in italy: state of the art and future perspectives. Front Neurol. (2020) 11:563375. doi: 10.3389/fneur.2020.563375
24. Seifert A, Batsis JA, Smith AC. Telemedicine in long-term care facilities during and beyond COVID-19: challenges caused by the digital divide. Front Public Heal. (2020) 8:601595. doi: 10.3389/fpubh.2020.601595
25. Anthony Jnr B. Implications of telehealth and digital care solutions during COVID-19 pandemic: a qualitative literature review. Inf Health Soc Care. (2020) 46:68–83. doi: 10.1080/17538157.2020.1839467
26. Bokolo AJ. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Irish J Med Sci. (2020) 190:1–10. doi: 10.1007/s11845-020-02299-z
27. Bokolo AJ. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. (2020) 44:1–8. doi: 10.1007/s10916-020-01596-5
28. Savulescu J, Persson I, Wilkinson D. Utilitarianism and the pandemic. Bioethics. (2020) 34:620–32. doi: 10.1111/bioe.12771
29. Strehle EM, Shabde N. One hundred years of telemedicine: does this new technology have a place in paediatrics? Arch Dis Childhood. (2006) 91:956–9. doi: 10.1136/adc.2006.099622
30. Chirra M, Marsili L, Wattley L, Sokol LL, Keeling E, Maule S, et al. Telemedicine in neurological disorders: opportunities and challenges. Telemed e-Health. (2019) 25:541–50. doi: 10.1089/tmj.2018.0101
31. Nesbitt TS, Hilty DM, Kuenneth CA, Siefkin A. Development of a telemedicine program. West J Med. (2000) 173:169–74. doi: 10.1136/ewjm.173.3.169-a
33. Moghadas A, Jamshidi M, Shaderam M. Telemedicine in Healthcare System. 2008 World Automation Congress, WAC 2008 (2008).
34. Leite H, Hodgkinson IR, Gruber T. New development:'Healing at a distance'-telemedicine and COVID-19. Taylor Fr. (2020) 40:483–5. doi: 10.1080/09540962.2020.1748855
35. Miele G, Straccia G, Moccia M, Leocani L, Tedeschi G, Bonavita S, et al. Telemedicine in Parkinson's disease: how to ensure patient needs and continuity of care at the time of COVID-19 pandemic. Telemed e-Health. (2020) 26:1533–6. doi: 10.1089/tmj.2020.0184
36. Moccia M, Lanzillo R, Brescia Morra V, Bonavita S, Tedeschi G, Leocani L, et al. Assessing disability and relapses in multiple sclerosis on tele-neurology. Neurol Sci. (2020) 41:1369–71. doi: 10.1007/s10072-020-04470-x
37. Palsbo SE, Bauer D. Telerehabilitation: managed care's new opportunity. Manag Care Q. (2000) 8:56–64.
38. Fernández JM, Solà M, Steblin A, Vargiu E, Miralles F. The relevance of providing useful and personalized information to therapists and caregivers in tele. Stud Comput Intell. (2017) 668:97–117. doi: 10.1007/978-3-319-46135-9_6
39. Martínez O, Jometón A, Pérez M, Lázaro E, Amayra I, López-Paz JF, et al. Effectiveness of teleassistance at improving quality of life in people with neuromuscular diseases. Span J Psychol. (2014) 17:E86. doi: 10.1017/sjp.2014.89
40. Kroenke K, Theobald D, Wu J, Norton K, Morrison G, Carpenter J, et al. Effect of telecare management on pain and depression in patients with cancer: a randomized trial. JAMA. (2010) 304:163–71. doi: 10.1001/jama.2010.944
41. Polisena J, Tran K, Cimon K, Hutton B, McGill S, Palmer K. Home telehealth for diabetes management: a systematic review and meta-analysis. Diabetes Obes Metab. (2009) 11:913–30. doi: 10.1111/j.1463-1326.2009.01057.x
42. Vitacca M, Bianchi L, Guerra A, Fracchia C, Spanevello A, Balbi B, et al. Tele-assistance in chronic respiratory failure patients: a randomised clinical trial. Eur Respir J. (2009) 33:411–8. doi: 10.1183/09031936.00005608
43. Hubbard PA, Broome ME, Antia LA. Pain, coping, and disability in adolescents and young adults with cystic fibrosis: a Web-based study. Pediatr Nurs. (2005) 31:82–6.
44. Rotondi AJ, Sinkule J, Spring M. An interactive web-based intervention for persons with TBI and their families: use and evaluation by female significant others. J Head Trauma Rehabil. (2005) 20:173–85. doi: 10.1097/00001199-200503000-00005
45. Scuteri D, Matamala-Gomez M, Bottiroli S, Corasaniti MT, De Icco R, Bagetta G, et al. Pain assessment and treatment in dementia at the time of coronavirus disease covid-19. Front Neurol. (2020) 11:890. doi: 10.3389/fneur.2020.00890
46. Chumbler NR, Rose DK, Griffiths P, Quigley P, McGee-Hernandez N, Carlson KA, et al. Study protocol: home-based telehealth stroke care: a randomized trial for veterans. Trials. (2010) 11:74. doi: 10.1186/1745-6215-11-74
47. Vitacca M, Comini L, Assoni G, Fiorenza D, Gilè S, Bernocchi P, et al. Tele-assistance in patients with amyotrophic lateral sclerosis: Long term activity and costs. Disabil Rehabil Assist Technol. (2012) 7:494–500. doi: 10.3109/17483107.2011.652999
48. Torres Zenteno AH, Fernández F, Palomino-García A, Moniche F, Escudero I, Jiménez-Hernández MD, et al. Mobile platform for treatment of stroke: a case study of tele-assistance. Health Informatics J. (2016) 22:676–90. doi: 10.1177/1460458215572925
49. Meystre S. The current state of telemonitoring: a comment on the literature. Telemed J e-Health. (2005) 11:63–9. doi: 10.1089/tmj.2005.11.63
50. Paré G, Jaana M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: the evidence base. J Am Med Inf Assoc. (2007) 14:269–77. doi: 10.1197/jamia.M2270
51. Portaro S, Calabrò RS, Bramanti P, Silvestri G, Torrisi M, Conti-Nibali V, et al. Telemedicine for facio-scapulo-humeral muscular dystrophy: a multidisciplinary approach to improve quality of life and reduce hospitalization rate? Disabil Health J. (2018) 11:306–9. doi: 10.1016/j.dhjo.2017.09.003
52. Trucco F, Pedemonte M, Racca F, Falsaperla R, Romano C, Wenzel A, et al. Tele-monitoring in paediatric and young home-ventilated neuromuscular patients: a multicentre case-control trial. J Telemed Telecare. (2019) 25:414–24. doi: 10.1177/1357633X18778479
53. Marziniak M, Brichetto G, Feys P, Meyding-Lamadé U, Vernon K, Meuth SG. The use of digital and remote communication technologies as a tool for multiple sclerosis management: narrative review. J Med Internet Res. (2018) 20:e5. doi: 10.2196/rehab.7805
54. Takahashi PY, Pecina JL, Upatising B, Chaudhry R, Shah ND, Van Houten H, et al. A randomized controlled trial of telemonitoring in older adults with multiple health issues to prevent hospitalizations and emergency department visits. Arch Intern Med. (2012) 172:773–9. doi: 10.1001/archinternmed.2012.256
55. Folea S, Avram C, Vidican S, Astilean A. Telemonitoring system of neurological signs in a health telematique network. Int J E-Health Med Commun. (2010) 1:14–34. doi: 10.4018/jehmc.2010100102
56. Silven AV, Petrus AHJ, Villalobos-Quesada M, Dirikgil E, Oerlemans CR, Landstra CP, et al. Telemonitoring for patients with COVID-19: recommendations for design and implementation. J Med Internet Res. (2020) 22:e20953. doi: 10.2196/20953
57. Zampolini M, Todeschini E, Guitart MB, Hermens H, Ilsbroukx S, Macellari V, et al. Tele-rehabilitation: present and future. Ann Ist Super Sanita. (2008) 44:125–34.
58. Carey JR, Durfee WK, Bhatt E, Nagpal A, Weinstein SA, Anderson KM, et al. Comparison of finger tracking versus simple movement training via telerehabilitation to alter hand function and cortical reorganization after stroke. Neurorehabil Neural Repair. (2007) 21:216–32. doi: 10.1177/1545968306292381
59. Giordano A, Bonometti G, Pietro, Vanoglio F, Paneroni M, Bernocchi P, Comini L, et al. Feasibility and cost-effectiveness of a multidisciplinary home-telehealth intervention programme to reduce falls among elderly discharged from hospital: study protocol for a randomized controlled trial. BMC Geriatr. (2016) 16:1–7. doi: 10.1186/s12877-016-0378-z
60. Tressoldi PE, Brembati F, Donini R, Iozzino R, Vio C. Treatment of dyslexia in a regular orthography: efficacy and efficiency (Cost-effectiveness) comparison between home vs clinic-based treatments. Eur J Psychol. (2012) 8:375–90. doi: 10.5964/ejop.v8i3.442
61. Peretti A, Amenta F, Tayebati SK, Nittari G, Mahdi SS. Telerehabilitation: review of the state-of-the-art and areas of application. JMIR Rehabil Assist Technol. (2017) 4:e7. doi: 10.2196/rehab.7511
62. Matamala-Gomez M, Maisto M, Montana JI, Mavrodiev PA, Baglio F, Rossetto F, et al. The role of engagement in teleneurorehabilitation: a systematic review. Front Neurol. (2020) 11:354. doi: 10.3389/fneur.2020.00354
63. Montana JI, Gomez MM, Maisto M, Mavrodiev PA, Cavalera CM, Diana B, et al. The Benefits of emotion regulation interventions in virtual reality for the improvement of wellbeing in adults and older adults : a systematic review. J Clin Med. (2020) 9:1–22. doi: 10.3390/jcm9020500
64. Caltagirone C, Zannino GD. Telecommunications technology in cognitive rehabilitation. Funct Neurol. (2008) 23:195–9.
65. Golomb MR, McDonald BC, Warden SJ, Yonkman J, Saykin AJ, Shirley B, et al. In-home virtual reality videogame telerehabilitation in adolescents with hemiplegic cerebral palsy. Arch Phys Med Rehabil. (2010) 91:1–8.e1. doi: 10.1016/j.apmr.2009.08.153
66. Rogante M, Grigioni M, Cordella D, Giacomozzi C. Ten years of telerehabilitation: a literature overview of technologies and clinical applications. Neurorehabilitation. (2010) 27:287–304. doi: 10.3233/NRE-2010-0612
67. Mantovani E, Zucchella C, Bottiroli S, Federico A, Giugno R, Sandrini G, et al. Telemedicine and virtual reality for cognitive rehabilitation: a roadmap for the COVID-19 pandemic. Front Neurol. (2020) 11:926. doi: 10.3389/fneur.2020.00926
68. Scherrenberg M, Frederix I, De Sutter J, Dendale P. Use of cardiac telerehabilitation during COVID-19 pandemic in Belgium. Acta Cardiol. (2020) 1–4. doi: 10.1080/00015385.2020.1786625
69. Riva G, Bernardelli L, Browning MHEM, Castelnuovo G, Cavedoni S, Chirico A, et al. COVID feel good-an easy self-help virtual reality protocol to overcome the psychological burden of coronavirus. Front Psychiatry. (2020) 11:563319. doi: 10.3389/fpsyt.2020.563319
70. Turolla A, Rossettini G, Viceconti A, Palese A, Geri T. Musculoskeletal physical therapy during the COVID-19 pandemic: is telerehabilitation the answer? Phys Ther. (2020) 100:1260–4. doi: 10.1093/ptj/pzaa093
71. Negrini S, Kiekens C, Bernetti A, Capecci M, Ceravolo MG, Lavezzi S, et al. Telemedicine from research to practice during the pandemic “instant paper from the field” on rehabilitation answers to the COVID-19 emergency. Eur J Phys Rehabil Med. (2020) 56:327–30. doi: 10.23736/S1973-9087.20.06331-5
72. Andrenelli E, Negrini F, De Sire A, Arienti C, Patrini M, Negrini S, et al. Systematic rapid living review on rehabilitation needs due to COVID-19: update to May 31st, 2020. Eur J Phys Rehabil Med. (2020) 56:508–14. doi: 10.23736/S1973-9087.20.06329-7
73. Curci C, Pisano F, Bonacci E, Camozzi DM, Ceravolo C, Bergonzi R, et al. Early rehabilitation in post-acute COVID-19 patients: Data from an Italian COVID-19 Rehabilitation Unit and proposal of a treatment protocol. Eur J Phys Rehabil Med. (2020). 56:633–41. doi: 10.23736/S1973-9087.20.06339-X
74. Sivan M, Halpin S, Hollingworth L, Snook N, Hickman K, Clifton IJ. Development of an integrated rehabilitation pathway for individuals recovering from COVID-19 in the community. J Rehabil Med. (2020) 52:jrm00089. doi: 10.2340/16501977-2727
75. Motolese F, Magliozzi A, Puttini F, Rossi M, Capone F, Karlinski K, et al. Parkinson's disease remote patient monitoring during the COVID-19 lockdown. Front Neurol. (2020) 11:567413. doi: 10.3389/fneur.2020.567413
76. Assenza G, Lanzone J, Brigo F, Coppola A, Di Gennaro G, Di Lazzaro V, et al. Epilepsy care in the time of COVID-19 pandemic in Italy: risk factors for seizure worsening. Front Neurol. (2020) 11:737. doi: 10.3389/fneur.2020.00737
77. Stipa G, Gabbrielli F, Rabbito C, Di Lazzaro V, Amantini A, Grippo A, et al. The Italian technical/administrative recommendations for telemedicine in clinical neurophysiology. Neurol Sci. (2020) 1–9. doi: 10.1007/s10072-020-04732-8
78. Ramalho R, Adiukwu F, Gashi Bytyçi D, El Hayek S, Gonzalez-Diaz JM, Larnaout A, et al. Telepsychiatry during the COVID-19 pandemic: development of a protocol for telemental health care. Front Psychiatry. (2020) 11:552450. doi: 10.3389/fpsyt.2020.552450
79. Realdon O, Rossetto F, Nalin M, Baroni I, Cabinio M, Fioravanti R, et al. Technology-enhanced multi-domain at home continuum of care program with respect to usual care for people with cognitive impairment: The Ability-TelerehABILITation study protocol for a randomized controlled trial. BMC Psychiatry. (2016) 16:425. doi: 10.1186/s12888-016-1132-y
80. Manenti R, Gobbi E, Baglio F, Macis A, Ferrari C, Pagnoni I, et al. Effectiveness of an innovative cognitive treatment and telerehabilitation on subjects with mild cognitive impairment: a multicenter, randomized, active-controlled study. Front Aging Neurosci. (2020) 12:585988. doi: 10.3389/fnagi.2020.585988
81. Quaglini S, Panzarasa S, Alloni A, Sacchi M, Sinforiani E, Bottiroli S, et al. HomeCore: bringing cognitive rehabilitation at home. Stud Health Technol Inf. (2019) 264:1755–6. doi: 10.3233/SHTI190632
82. Alloni A, Sinforiani E, Zucchella C, Sandrini G, Bernini S, Cattani B, et al. Computer-based cognitive rehabilitation: the CoRe system. Disabil Rehabil. (2017) 39:407–17. doi: 10.3109/09638288.2015.1096969
83. Alloni A, Quaglini S, Panzarasa S, Sinforiani E, Bernini S. Evaluation of an ontology-based system for computerized cognitive rehabilitation. Int J Med Inform. (2018) 115:64–72. doi: 10.1016/j.ijmedinf.2018.04.005
84. Bernini S, Alloni A, Panzarasa S, Picascia M, Quaglini S, Tassorelli C, et al. A computer-based cognitive training in Mild Cognitive Impairment in Parkinson's Disease. Neurorehabilitation. (2019) 44:555–67. doi: 10.3233/NRE-192714
85. Bernini S, Panzarasa S, Barbieri M, Sinforiani E, Quaglini S, Tassorelli C, et al. A double-blind randomized controlled trial of the efficacy of cognitive training delivered using two different methods in mild cognitive impairment in Parkinson's disease: preliminary report of benefits associated with the use of a computerized tool. Aging Clin Exp Res. (2020) 1–9. doi: 10.1007/s40520-020-01665-2
86. Gentry MT, Lapid MI, Rummans TA. Geriatric telepsychiatry: systematic review and policy considerations. Am J Geriatr Psychiatry. (2019) 27:109–27. doi: 10.1016/j.jagp.2018.10.009
87. Standing C, Standing S, McDermott ML, Gururajan R, Kiani Mavi R. The paradoxes of telehealth: a review of the literature 2000-2015. Syst Res Behav Sci. (2018) 35:90–101. doi: 10.1002/sres.2442
88. Marin A. Technology Feature| Telemedicine takes center stage in the era of COVID-19. Science (80-) [Internet]. (2020) 6517:731–3. Available from: https://science.sciencemag.org/content/370/6517/731.summary
89. Patterson V, Hoque F, Vassallo D, Farquharson Roberts M, Swinfen P, Swinfen R. Store-and-forward teleneurology in developing countries. J Telemed Telecare. (2001) 7(Suppl 1):52–3. doi: 10.1177/1357633X010070S121
90. Dorsey ER, Glidden AM, Holloway MR, Birbeck GL, Schwamm LH. Teleneurology and mobile technologies: the future of neurological care. Nat Rev Neurol. (2018) 14:285–97. doi: 10.1038/nrneurol.2018.31
91. Sánchez Rodríguez MT, Collado Vázquez S, Martín Casas P, Cano de la Cuerda R. Neurorehabilitation and apps: a systematic review of mobile applications. Neurologia. (2018) 33:313–26. doi: 10.1016/j.nrleng.2015.10.002
92. Riva G, Gamberini L. Virtual reality in telemedicine. Telemed J. (2000) 6:327–40. doi: 10.1089/153056200750040183
93. Tuena C, Pedroli E, Trimarchi PD, Gallucci A, Chiappini M, Goulene K, et al. Usability issues of clinical and research applications of virtual reality in older people: a systematic review. Front Hum Neurosci. (2020) 14:93. doi: 10.3389/fnhum.2020.00093
94. Perez-Marcos D. Virtual reality experiences, embodiment, videogames and their dimensions in neurorehabilitation. J Neuroeng Rehabil. (2018) 15:113. doi: 10.1186/s12984-018-0461-0
95. Slater M, Sanchez-Vives MV. Enhancing our lives with immersive virtual reality. Front Robot AI. (2016) 3:74. doi: 10.3389/frobt.2016.00074
96. Tuena C, Serino S, Dutriaux L, Riva G, Piolino P. Virtual enactment effect on memory in young and aged populations: a systematic review. J Clin Med. (2019) 8:620. doi: 10.3390/jcm8050620
97. Riva G, Gamberini L. Virtual reality as telemedicine tool: Technology, ergonomics and actual applications. Technol Health Care. (2000) 8:113–27. doi: 10.3233/THC-2000-8203
98. Ji H, Jing W, Gao J, Liu X. Research on telemedicine technology and implement based on Virtual Reality. In: Proceedings of 2016 IEEE Advanced Information Management, Communicates, Electronic and Automation Control Conference, IMCEC 2016. Xi'an (2017). p. 1581–6.
99. Carbone M, Freschi C, Mascioli S, Ferrari V, Ferrari M. A wearable augmented reality platform for telemedicine. In: De Paolis L, Mongelli A, editors. Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). Cham: Springer (2016). p. 92–100.
100. Perez-Marcos D, Solazzi M, Steptoe W, Oyekoya O, Frisoli A, Weyrich T, et al. A fully immersive set-up for remote interaction and neurorehabilitation based on virtual body ownership. Front Neurol. (2012) 3:110. doi: 10.3389/fneur.2012.00110
101. Slater M, Perez-Marcos D, Ehrsson HH, Sanchez-Vives M V. Towards a digital body: the virtual arm illusion. Front Hum Neurosci. (2008) 2:6. doi: 10.3389/neuro.09.006.2008
102. Matamala-Gomez M, Malighetti C, Cipresso P, Pedroli E, Realdon O, Mantovani F, et al. Changing body representation through full body ownership illusions might foster motor rehabilitation outcome in patients with stroke. Front Psychol. (2020) 11:1962. doi: 10.3389/fpsyg.2020.01962
103. Matamala-Gomez M, Diaz Gonzalez AM, Slater M, Sanchez-Vives MV. Decreasing pain ratings in chronic arm pain through changing a virtual body: different strategies for different pain types. J Pain. (2019) 20:685–97. doi: 10.1016/j.jpain.2018.12.001
104. Chirico A, Malighetti C, Serino S, Cipresso P, Pedroli E, Tuena C, et al. Towards an advancement of multisensory integration deficits in anorexia nervosa: exploring temporal discrimination processing of visuo-auditory stimuli. Annu Rev CyberTherapy Telemed. (2019) 17:53–8. Available online at: http://hdl.handle.net/10807/147119
105. Serino S, Scarpina F, Keizer A, Pedroli E, Dakanalis A, Castelnuovo G, et al. A novel technique for improving bodily experience in a non-operable super-super obesity case. Front Psychol. (2016) 7:837. doi: 10.3389/fpsyg.2016.00837
106. Serino S, Polli N, Riva G. From avatars to body swapping: The use of virtual reality for assessing and treating body-size distortion in individuals with anorexia. J Clin Psychol. (2019) 75:313–22. doi: 10.1002/jclp.22724
107. Pozeg P, Palluel E, Ronchi R, Solcà M, Al-Khodairy AW, Jordan X, et al. Virtual reality improves embodiment and neuropathic pain caused by spinal cord injury. Neurology. (2017) 89:1894–903. doi: 10.1212/WNL.0000000000004585
108. Solcà M, Ronchi R, Bello-Ruiz J, Schmidlin T, Herbelin B, Luthi F, et al. Heartbeat-enhanced immersive virtual reality to treat complex regional pain syndrome. Neurology. (2018) 91:e1–11. doi: 10.1212/WNL.0000000000005905
109. Donati ARC, Shokur S, Morya E, Campos DSF, Moioli RC, Gitti CM, et al. Long-term training with a brain-machine interface-based gait protocol induces partial neurological recovery in paraplegic patients. Sci Rep. (2016) 6:30383. doi: 10.1038/srep30383
110. Matamala-Gomez M, Nierula B, Donegan T, Slater M, Sanchez-Vives M V. Manipulating the perceived shape and color of a virtual limb can modulate pain responses. J Clin Med. (2020) 9:291. doi: 10.3390/jcm9020291
111. Malighetti C, Serino S, Riva G, Cipolletta S. Inside and outside the self. Virtual reality and repertory grids in the spatial analysis of anorexic patients' meanings. Annu Rev CyberTherapy Telemed. (2016) 14:78–83. Available online at: http://hdl.handle.net/10807/119674
112. Riva G, Gamberini L. Virtual reality in telemedicine (Chapter 15: Studies in new technologies and practices in communication BT - Communications through virtual technologies: Identity, community and technology in the communication age). In: Riva G, Davide F, editors. Communications Through Virtual Technologies: Identity, Community and Technology in the Communication Age. Amsterdam: IOS Press (2001). p. 101–17; 273 p. Available online at: https://search.proquest.com/docview/619693531?accountid=16562
113. Kaplan B. REVISITING HEALTH INFORMATION TECHNOLOGY ETHICAL, LEGAL, and SOCIAL ISSUES and EVALUATION: TELEHEALTH/TELEMEDICINE and COVID-19. Int J Med Inf. (2020) 143:104239. doi: 10.1016/j.ijmedinf.2020.104239
114. Shook JR, Galvagni L, Giordano J. Cognitive enhancement kept within contexts: neuroethics and informed public policy. Front Syst Neurosci. (2014) 8:228. doi: 10.3389/fnsys.2014.00228
115. Wang TT, Li JM, Zhu CR, Hong Z, An DM, Yang HY, et al. Assessment of utilization and cost-effectiveness of telemedicine program in western regions of China: a 12-year study of 249 hospitals across 112 cities. Telemed e-Health. (2016) 22:909–20. doi: 10.1089/tmj.2015.0213
116. Hong Z, Li N, Li D, Li J, Li B, Xiong W, et al. Telemedicine during the COVID-19 pandemic: experiences from Western China. J Med Internet Res. (2020) 22:e19577. doi: 10.2196/preprints.19577
117. Omboni S. Telemedicine during the COVID-19 in Italy: a missed opportunity? Telemed E-Health. (2020) 26:973–5. doi: 10.1089/tmj.2020.0106
118. Association AM. Telehealth Implementation Playbook. American Medical Association. (2020). Available online at: https://www.ama-assn.org/terms-use
119. Miller KL. Patient centered care: apath to better health outcomes through engagement and activation. Neurorehabilitation. (2016) 39:465–70. doi: 10.3233/NRE-161378
Keywords: telemedicine, healthcare, virtual reality, neurorehabilitation, COVID-19
Citation: Matamala-Gomez M, Bottiroli S, Realdon O, Riva G, Galvagni L, Platz T, Sandrini G, De Icco R and Tassorelli C (2021) Telemedicine and Virtual Reality at Time of COVID-19 Pandemic: An Overview for Future Perspectives in Neurorehabilitation. Front. Neurol. 12:646902. doi: 10.3389/fneur.2021.646902
Received: 28 December 2020; Accepted: 03 February 2021;
Published: 25 March 2021.
Edited by:
Andrea Martinuzzi, Eugenio Medea (IRCCS), ItalyReviewed by:
Marcello Moccia, University of Naples Federico II, ItalyCopyright © 2021 Matamala-Gomez, Bottiroli, Realdon, Riva, Galvagni, Platz, Sandrini, De Icco and Tassorelli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marta Matamala-Gomez, bWFydGEubWF0YW1hbGExMEBnbWFpbC5jb20=; bWFydGEubWF0YW1hbGFnb21lekB1bmltaWIuaXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.