
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 27 April 2021
Sec. Neuromuscular Disorders and Peripheral Neuropathies
Volume 12 - 2021 | https://doi.org/10.3389/fneur.2021.627183
 Juanjuan Zhang1†
Juanjuan Zhang1† Dandan Xie2†
Dandan Xie2† Yanfeng Zou3†
Yanfeng Zou3† Xuen Yu4
Xuen Yu4 Yang Ji5
Yang Ji5 Chengyou Wang6
Chengyou Wang6 Xinyi Lv7
Xinyi Lv7 Nong Zhou1
Nong Zhou1 Xiao Jiang8
Xiao Jiang8 Kai Wang1,8,9,10,11*
Kai Wang1,8,9,10,11* Yanghua Tian1*
Yanghua Tian1*Background: Nitrous oxide (N2O), commonly known as laughing gas, is inhaled recreationally because it produces the feelings of euphoria and freedom from pain. The risk of neurological dysfunction secondary to N2O abuse and its clinical diagnosis are, however, not yet sufficiently recognized, especially in China. Here, we have summarized the key clinical characteristics of N2O-induced neurological disorders.
Materials and Methods: We recruited 20 patients with N2O-induced neurological disorders and analyzed their clinical features, laboratory data, magnetic resonance imaging and electromyography. We also carried out a literature review and compared 99 previously reported patients with our case series to confirm our results. Subgroup analysis was performed to explore the difference in demographical and clinical characteristics of N2O abuse between Asian and non-Asian patients.
Results: The most common initial symptoms of N2O-induced neurological disorders were weakness and/or paresthesia. Most patients presented with myelopathy and/or peripheral neuropathy. The most commonly involved segment of the spinal cord was the cervical spinal cord, extending over 4–6 vertebral levels, but more than half of the patients with myelopathy had no sensory change at the corresponding spinal level. Homocysteine was found to be the most sensitive and practical indicator for diagnosis. Subgroup analysis showed that the Asian patients (median: 22.0 years old, Q1–Q3:19.0–26.0 years old) with N2O abuse were younger than non-Asian patients [26.0 (22.3–31.0) years old, P = 2.8 × 10−4]. The incidence of myelopathy combined with peripheral neuropathy was significantly higher in Asian patients than in non-Asian patients, who had myelopathy or peripheral neuropathy (P = 2 × 10−5).
Conclusions: Key clinical characteristics of N2O abuse are longitudinally extensive cervical myelopathy and peripheral neuropathy. Recognition of these traits in young people in the age group of 20–30 years will provide important guidance for accurate diagnosis of neurological disease associated with N2O abuse. The clinical manifestations differ in Asian patients and non-Asian patients.
Nitrous oxide (N2O), an odorless and colorless gas, which is also known as laughing gas, is widely used in anesthesia and as a propellant in the food industry (1, 2). Unfortunately, because of its legitimation, convenience and low cost, N2O is recreationally inhaled by people for the feelings of euphoria and freedom from pain (3, 4). N2O abuse has now become a common societal and medical problem in many countries, including the USA, UK and China (1, 3, 5) According to the Global Drug Survey of 2016, N2O is the seventh most commonly used recreational drug (6). Since the first Chinese case was reported in 2016, there has been a rapid annual increase in published papers related to recreational abuse of N2O in China (3). The risks associated with N2O abuse and its clinical diagnosis are, however, not yet sufficiently recognized, especially in China.
Alterations in vitamin B12 (methylcobalamin and adenosylcobalamin) metabolism were speculated to underlie the neurotoxic effects of N2O (4, 7–9). Methylcobalamin converts homocysteine to methionine as part of the methylation cycle. The process might be disturbed by N2O via irreversible oxidation of the cobalt atom of vitamin B12, which leads to low levels of vitamin B12, hyperhomocysteinemia, demyelination, axonal degeneration, and megaloblastic anemia (10). Adenosylcobalamin is a cofactor for L-methylmalonyl coenzyme A (MMCoA) mutase, which catalyzes the conversion of methylmalonyl-CoA to succinyl-CoA in mitochondria. Inactivation of adenosylcobalamin results in reduced levels of succinyl-CoA, and high levels of methylmalonic acid (MMA) which also leads to demyelination (9).
Individuals who abuse N2O may present with numbness, weakness, ataxia, decreased deep sensation, urinary retention, sleep disorders, hallucinations or even death (4, 7, 11–13). However, these neurological symptoms secondary to N2O abuse are non-specific and often mimic other diseases (14). If the patient conceals, or the neurologist ignores, recreational N2O abuse, the patient may be wrongly diagnosed with autoimmune diseases, such as Guillain-Barre syndrome (GBS) and receive unnecessary treatments (i.e., intravenous immunoglobulin, IVIG). It is thus important that clinicians recognize the clinical features of neurological disease associated with N2O abuse.
Here, we recruited 20 patients diagnosed with N2O-induced neurological disorders and summarized their clinical features, laboratory data, magnetic resonance imaging (MRI) and electromyography (EMG). We also carried out a literature review and compared 99 previously reported patients with our case series to confirm our results. Homocysteine metabolism is involved in vitamin B12 metabolism and might differ among various populations. To explore the demographical and clinical characteristics of N2O abuse between Asian and non-Asian patients, we pooled the data for our 20 patients and the previously reported 99 patients to conduct subgroup analysis (15).
This retrospective hospital-based case series study was conducted in the First Affiliated Hospital of Anhui Medical University, the Affiliated Anqing Hospital of Anhui Medical University, the Institute of Neurology of Anhui University of Chinese Medicine, the First Affiliated Hospital of the University of Science and Technology of China and the Affiliated Tongling Hospital of Anhui Medical University. We searched the hospital medical records from October 2018 to May 2020 to identify patients (≥14 years old) with a history of N2O abuse and symptoms suggestive of neurological disease using an institutional search tool. Patients with myelopathy and/or peripheral neuropathy caused by infection, autoimmunity, trauma, vascular disease, other toxic/metabolic causes, tumor, heredity and systemic disease were excluded. One patient had a pre-existing diagnosis of N2O-induced subacute degeneration of the spinal cord (SCD) and had re-inhaled N2O before this admission (case 20). None of the patients were vegetarian or had undergone gastrectomy and so were unlikely to have vitamin B12 deficiency. It was not possible to obtain consent from all patients since current contact details were unavailable and all cases were, therefore, anonymized. The Clinical Research Ethics Committee of Anhui Medical University approved this study protocol, which was in accordance with the Declaration of Helsinki. Patients gave written informed consent.
Details of clinical symptoms, examinations and treatment and prognosis of these patients were collected. Because standard techniques and routine treatment varied between the different hospitals, some data were missing.
To further demonstrate clinical characteristics of N2O abuse, we performed a systematic literature review through searches of MEDLINE and EMBASE, with the key words (nitrous oxide or laughing gas or N2O) AND (neurological disease or myelopathy or peripheral neuropathy or Guillain-Barre syndrome or GBS or subacute degeneration of the spinal cord or SCD or degeneration or spinal cord or neurotoxicity), with the studies limited to human and case reports limited to the period January 1998 to July 2020. Cases before 1998 were not included due to undocumented spinal cord MRI. Studies without detailed documentation of patients' clinical features were excluded, even if they had a large sample size. Exclusion criteria were: non-English language publication, patients younger than 14 years old, symptoms caused by infection, autoimmunity, trauma, vascular disease, other toxic/metabolic causes (such as N2O anesthesia or vegetarian diet), tumor, heredity and systemic disease. The search yielded previously reported 99 patients were recruited. We extracted the following information: gender, age, clinical manifestations, examinations, treatment and prognosis. Two investigators (Zhang and Ji) independently reviewed the retrieved articles to choose potentially relevant articles and extracted data.
We pooled the data from our own 20 patients and the 99 previously reported patients then divided them into two groups: Asian patients from Asian countries and non-Asian patients from European, North American, and Oceanian countries. We created two more subgroups from pooling the data of our own 20 patients and 23 patients of published cases from China. These two groups were patients from mainland China and patients from Taiwan. After reassigning the cases, we performed analyses to explore the differences in demographical and clinical characteristics of N2O abuse between each grouping pair (Asian vs. non-Asian and mainland China vs. Taiwan).
All statistical analyses were conducted using IBM SPSS (version 25.0). Normally distributed continuous variables were expressed as the mean ± standard deviation (SD) and compared with the independent sample t-test. Continuous variables that were not normally distributed were expressed as the median (Q1–Q3) and compared with the Mann-Whitney U test. The chi-squared test was used for comparisons of categorical variables. A probability level of <5% (two-sided) was regarded as significant.
Clinical features of 20 patients are summarized in Supplementary Table 1 and Table 1. All patients were young (median: 22.5 years old, Q1–Q3: 20.3–27.8 years old). Eleven were female and nine were male. The duration of N2O abuse was between 3 days and 2 years.
All 20 patients initially presented with weakness or numbness. Eleven patients presented with both weakness and numbness. Six patients presented with only numbness. Three patients presented with only weakness, including one patient who did not complain of paresthesia but presented with abnormal deep sensation on physical examination and one patient who complained of paroxysmal numbness of distal parts of all four limbs but presented with normal sensation on physical examination. In half of the patients, weakness was present in all four limbs. In 30% of patients, weakness was present only in the lower limbs. In other patients, the whole body (1/20) or only one leg (1/20) was affected. Besides weakness and paresthesia, eleven patients presented with ataxia and eight of them with disturbances in proprioception over the course of the disease. Unsteady gait and pain were complained of in four and two patients, respectively. Psychiatric symptoms, sleep disturbance, bowel and bladder dysfunction, arterial thrombosis and memory impairment were also observed (cases 6, 12, 15, 18, 20). The cognition of patients was evaluated by mini-mental state examination, Montreal cognitive assessment, Stroop test, verbal fluency test, digit span test and Chinese auditory vocabulary learning test.
Laboratory tests and ancillary examinations of 20 patients are summarized in Supplementary Table 1 and Table 1. The average hemoglobin (Hb) level was 133 ± 20 g/L. Three female patients showed anemia (normal: female >110 g/L; male >120 g/L). Mean corpuscular volume (MCV) was 96 ± 9 fl. Elevated MCV was found in five patients (normal <100 fl). Only five patients had deceased levels of vitamin B12 (normal: 197–771 pg/mL). High homocysteine levels were found in 14 patients (normal: 5–13.9 μmol/L).
MRI of the spinal cord was performed in 19 patients. T2 hyperintensity of the posterior column in the spinal cord was found in 15 patients. The common segment involved started at C2 and terminated at C6 or C7. One patient (case 5) presented with myelopathy in the whole spinal cord. One patient (case 13) had several MRI scans of the spinal cord and changes in the MRI signal resolved after 4 months of treatment with mecobalamin and hyperbaric oxygen (Figure 1). It is noteworthy that, although abnormal spinal cord signals were seen in 15 patients, 13 patients presented with no sensory changes at the corresponding spinal level.
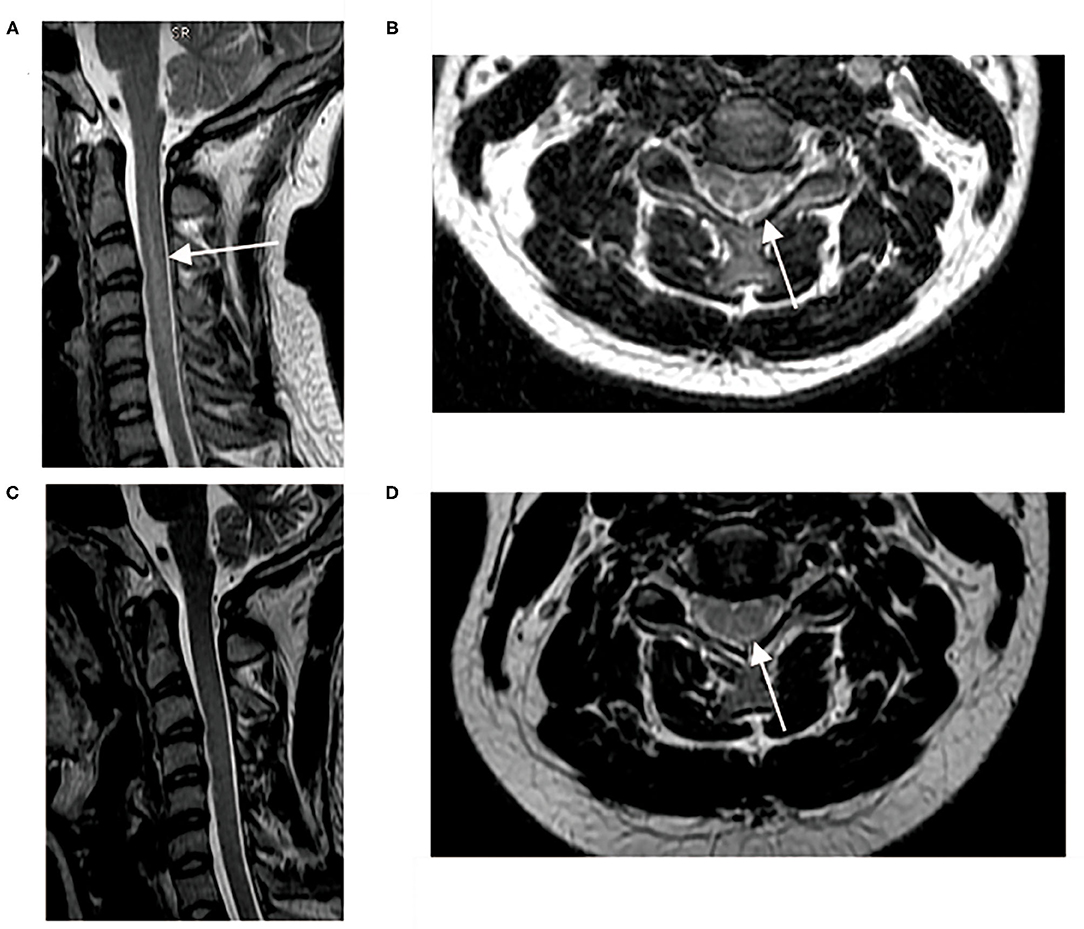
Figure 1. Spinal cord MRI pre- and after-treatment. (A,B) T2 hyperintensity of posterior column from C2–C6 pre-treatment; (C) Sagittal T2-hyperintensity of posterior column from C2–C6 resolved 4 months after treatment with mecobalamine and hyperbaric oxygen; (D) Axial inverted “V” T2-hyperintensity was blurred 4 months after treatment.
Eighteen patients underwent EMG, which showed demyelination and axonal damage in peripheral nerves in 16 patients. Twelve patients had both abnormal signals in the spinal cord and abnormal EMGs. The most common manifestations in our series were N2O-induced cervical myelopathy and peripheral neuropathy.
All patients ceased inhaling N2O and received supplements of cobamamide, mecobalamin or cyanocobalamin by intramuscular or intravenous injection (0.5–2 mg/day, Supplementary Table 2) for 13.7 ± 7.3 days, followed by oral medication. Five patients received glucocorticoid therapy, either to relieve edema of the spinal cord or because the patients did not admit to N2O abuse and a diagnosis of autoimmune disease was considered. Failure to admit to N2O abuse also resulted in two patients receiving IVIG. Five patients received hyperbaric oxygen therapy. Sixteen patients improved on discharge (Supplementary Table 2). After discharge, 16 patients recovered in 0.5–3.5 months, three patients were lost to follow-up and one patient still walked slowly and suffered from numb toes and memory loss.
Data for 99 previously published patients with detailed medical records were collected (Table 1 and Supplementary Table 3). Men and women were almost equally represented, and the patients had a median age of 24.0 (Q1–Q3: 21.0–29.0) years old. Myelopathy was the most common presentation (42/99), followed by combined myelopathy and peripheral neuropathy (33/99) and peripheral neuropathy (11/99). Sixty-six patients presented with paresthesia or numbness as the initial symptoms, and 30 patients experienced gait instability. Over the course of the disease, 68 patients presented with weakness of the limbs, half of the lower limbs (31/69). During physical examination, 79 patients showed decreased deep sensory perception and 66 showed ataxia. Lhermitte's sign was rare (8/99). Reported abnormal laboratory data included elevated levels of homocysteine (93.2%) and MMA (94.1%), decreased levels of vitamin B12 (53.8%), elevated MCV (37.7%) and decreased Hb (31.3%). Spinal cord involvement was seen in 76 patients, most of which was in the cervical segment (52/76). Cervical and thoracic segments were involved in 20 patients. Only one patient had lesions in the thoracic segment. Notably, 50 patients did not present with changes in sensory perception at the corresponding spinal level, even though they had lesions in the spinal cord. Almost half of the patients had abnormal EMGs (45/99). Almost all the patients were treated with vitamin B12 (95/99). Most of the patients (73/99) improved following N2O cessation and vitamin B12 supplementation. One patient, whose medical history was concealed, deteriorated. One patient died because of re-abuse of N2O, combined with abuse of psychotropic drugs.
In addition, we analyzed the length of lesions in the spinal cord both in our own 20 patients and in 99 previously reported patients (Figure 2). In 25.3% of patients, the lesions extended over five or six vertebral levels, followed by four (17.3%), seven (8.0%) and three levels (6.7%).
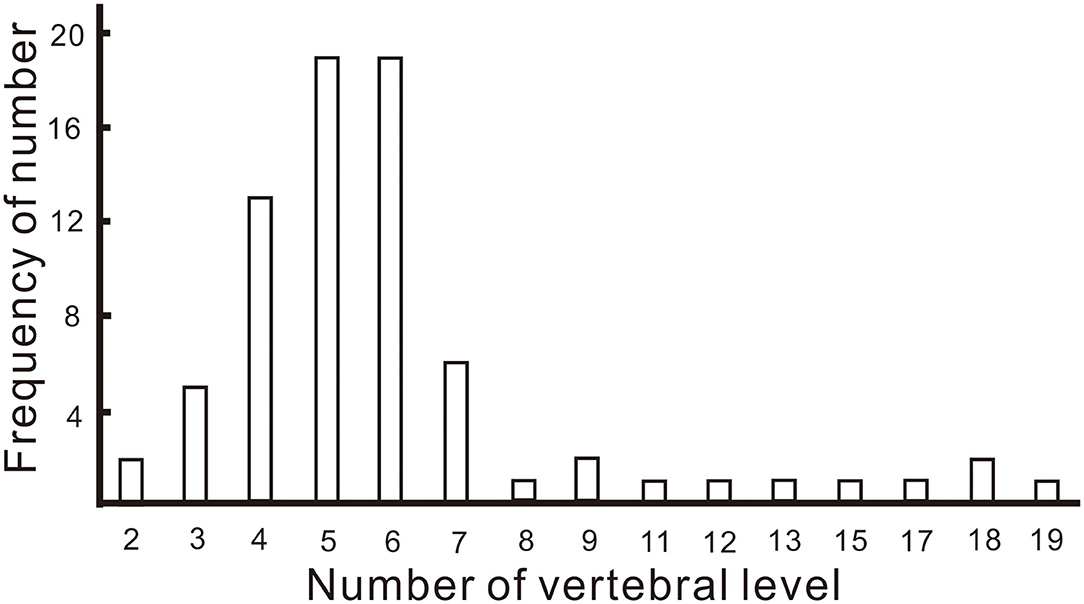
Figure 2. Frequency of the number of vertebral levels over which lesions of the spinal cord extended.
The comparison between Asian patients and non-Asian patients is shown in Table 2. There were 56 Asian patients and 63 non-Asian patients. More Asian females abused N2O, whereas more non-Asian males abused N2O (χ2:8.868, P = 0.003). The Asian patients were significantly younger than non-Asian patients (Z = −3.632, P = 2.8 × 10−4). More non-Asian patients had a history of polysubstance or intravenous drug abuse (χ2: 5.521, P = 0.02). The average period of N2O abuse by Asian patients was significantly shorter than that of non-Asian patients (Z = −2.072, P = 0.04). Most Asian patients (41/56) had myelopathy combined with symptoms of, or EMG-confirmed peripheral injuries (combined injuries). Six patients had only myelopathy and seven had only peripheral injuries. Most non-Asian patients (26/63) had only myelopathy, followed by only peripheral injuries (7/63) and combined injuries (18/63). The proportions of the type of injury differed significantly between Asian and non-Asian patients (χ2: 21.398, P = 2 × 10−5, Figure 3 and Table 2). No significant differences in levels of Hb, MCV, vitamin B12 and homocysteine were found between Asian and non-Asian patients (P > 0.05). The comparison between mainland patients and Taiwan patients is shown in Table 3. No significant differences in the age, gender, the proportion of polysubstance or intravenous drug abuse, time of N2O abuse, levels of Hb, MCV, vitamin B12, homocysteine and the type of injuries were found between them.
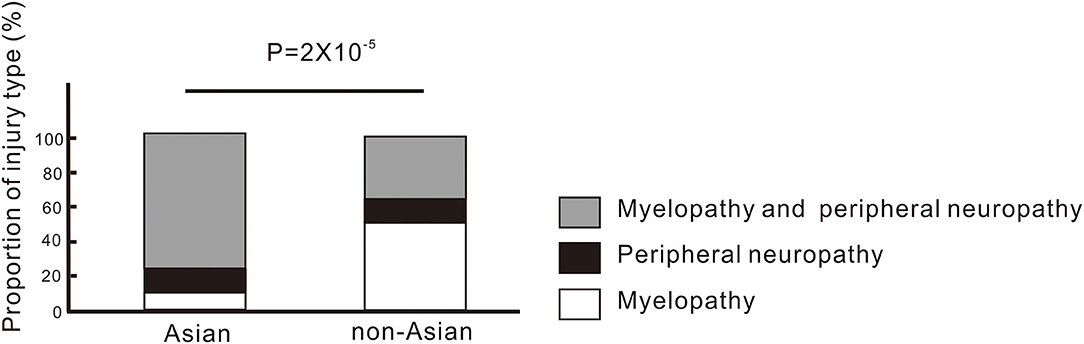
Figure 3. Type of injuries involved in N2O-induced neurological disorders in Asian and non-Asian patients.
In this study, we found that the most common initial symptoms of N2O-induced neurological disorders were weakness and/or paresthesia. Longitudinally extensive cervical myelopathy, with or without peripheral neuropathy, is the most common manifestation, but most patients with myelopathy had no sensory change at the corresponding spinal level. The most common number of vertebral levels involved in lesions was five and six. The most reliable and practical laboratory indicator for diagnosis was homocysteine. The Asian patients with N2O abuse were younger than non-Asian patients. The incidence of myelopathy combined with peripheral neuropathy was significantly higher in Asian patients than in non-Asian patients, who mainly had myelopathy or peripheral neuropathy.
One of the common manifestations of neurological disorders caused by N2O is SCD, which is characterized by decreased deep sensation, symmetrical T2-weighted hypersensitivity in the posterior column of spinal cord and vitamin B12 deficiency (9). However, attention must be given to the cause of differences between neurological disorders caused by N2O compared to those caused by vitamin B12 deficiency. In both our case series and previous cases, the cervical segment is much more vulnerable in patients who abuse N2O (3, 16). Zheng et al. found that 32 patients had lesions in the cervical spinal cord and one patient had lesions in both cervical and thoracic spinal cord in 33 patients with N2O abuse who performed MRI (3). Bao et al. found that, in 16 patients who abused N2O, the most commonly impaired vertebral levels were C3–C5 (50.6%), followed by C2 (41.6%) and C6 (37.2%) (16). Lan et al. suggested that the vulnerability of the cervical segment to N2O neurotoxicity is attributable to the higher density of myelinated fibers of fasciculus gracilis in the cervical segment compared with the thoracic segment (17, 18). In contrast, the upper thoracic segments of the spinal cord are affected in more patients with SCD secondary to vitamin B12 deficiency than in patients who abuse N2O (17, 19). In addition to the involvement of different segments of the spinal cord, differences in both nerve excitability and MRI T2 signals have been reported in N2O abuse and vitamin B12 deficiency (20). We also found that, in 25.3% of patients, the lesions in the spinal cord extended over five or six vertebral levels, followed by four levels. This means that the lesions in the spinal cord secondary to N2O abuse are longitudinally extensive myelitis. The extended vertebral levels in our study were a little longer than those in the study by Bao et al. (16) and similar to those in the study by Zheng et al. (3). An interesting observation is that, despite lesions in the cervical segment of the spinal cord, many patients had no sensory change at the corresponding spinal level. A low proportion of patients with sensory change at the spinal level was also seen by Bao et al. (16). Vasconcelos et al. considered that an absence of sensory change at the spinal level might be associated with better clinical resolution since the absence of sensory change at the spinal level indicated that transmission of sensory impulses to higher centers is preserved (18). Another explanation might be that dysfunction of the spinal cord is subclinical, although the lesions in the spinal cord seem extensive.
We found that, except for MMA levels, the biggest change in laboratory indicators was hyperhomocysteinemia, followed by levels of vitamin B12. Neither low Hb nor high MCV occurred frequently. Since N2O affects both methionine synthase and MMCoA mutase pathways, low Hb, elevated MCV, low vitamin B12 levels, high homocysteine and MMA levels, can be tested and helpful for differential diagnosis, although the specificity and sensibility of these indicators varies. Anemia was found in 66.2% of patients with SCD secondary to vitamin B12 deficiency in the study by Cao et al. (21). By contrast, anemia was found in only 15% of patients in our case series and 31.3% in previous cases. The low incidence of anemia in patients with symptoms secondary to N2O abuse indicates the involvement of mechanisms other than disturbed vitamin B12 metabolism, such as cytotoxicity of homocysteine toward cortical astrocytes and N2O-catalyzed production of hydroxyl radicals (22, 23). Low levels of vitamin B12 were seen in more patients than low levels of Hb. Theoretically, vitamin B12 should be a good indicator, but it is, on the contrary, a confusing indicator. On the one hand, some patients had taken vitamin B12 before hospitalization. On the other hand, in some patients, the serum vitamin B12 level is normal but with abnormal vitamin B12-related metabolism (functional vitamin B12 deficiency) (4). Both availability of folate and vitamin B12 deficiency affect levels of homocysteine, whereas levels of MMA are not affected by other vitamins (9). MMA is, therefore, an accurate and specific biomarker of functional vitamin B12 deficiency. Although the incidence of high levels of MMA in previous cases was 94.1%, only 34.3% of patients had an MMA test. This means that MMA is not a suitable indictor for practical use and the most sensitive and practical indicator for the diagnosis of N2O-induced neurological disorders is homocysteine.
In general, young people tend to abuse N2O for recreational purpose. Asian patients who abused N2O were younger than non-Asian patients. The Asian patients were mostly from China and Korea, where recreational N2O abuse is popular among young people (age range: 16–41). By contrast, in non-Asian countries, more middle-aged people abuse N2O, with even one 60-year-old women inhaling N2O (age range: 17–60) (24). The difference in age might be explained by different cultures and economies.
Our data showed that Asian patients were prone to combined injuries, whereas more non-Asian patients had single injury-lesions in the spinal cord. Neurological dysfunction secondary to N2O abuse is related to disturbed metabolism of vitamin B12, folate and homocysteine (9). MTHFR (methylenetetrahydrofolate reductase) is one of genes that participates in homocysteine metabolic pathways. Mutation of MTHFR attenuates the activity of MTHFR, resulting in hyperhomocysteinemia (15). The frequency of different genotypes of MTHFR differs among populations (15), and the strength of the association between MTHFR and risk of coronary heart disease was found to vary in eastern and western populations (25). The differences in types of injury seen in neurological disorders caused by N2O abuse in different populations may, therefore, be explained by differences in genetic background. Additionally, Asian people eat less meat than European or North American people, which may influence basal serum levels of vitamin B12 since dietary vitamin B12 is mainly derived from animal sources (26). It has been reported that symptoms secondary to N2O abuse may be related to basal serum levels of vitamin B12 and the difference may, therefore, also be associated with different dietary habits (27). Our data also showed that there were no significant differences in demographical and clinical characteristics of N2O abuse between mainland patients and Taiwan patients. The results of mainland patients were almost parallel with that of the previous study on Taiwan patients, except for N2O exposure time, proportion of multiple illicit substance abuse, and serum vitamin B12 (28). These differences may be attributed to social factors and vitamin B12 supplement before hospitalization.
N2O-induced neurological disorders are mostly regarded as SCD, but there are some differences between the two. If longitudinally extensive cervical myelopathy with peripheral neuropathy is found in young patients with a normal diet, clinicians should consider the possibility of N2O abuse in either Neurology or Emergency departments, regardless of presence of amenia or low serum vitamin B12. The present study has some limitations. Firstly, the sample size in the retrospective study was small. We plan to conduct a large sample study with follow-up. Secondly, not all of necessary laboratory tests and ancillary examinations were performed on all of our patients. This means that there are some gaps in our results, which influence our interpretation. Lastly, since not all of our patients were followed-up regularly, and follow-up consisted mainly of telephone interviews, dynamic changes in symptoms, MRI and EMG were not observed regularly.
N2O abuse is increasing rapidly among young people in a number of countries. It is very important that all frontline clinicians are aware of the damage caused by N2O, and of the various clinical presentations of neurotoxicity related to abuse of N2O. The key clinical manifestations associated with N2O abuse are longitudinally extensive cervical myelopathy and peripheral neuropathy in young patients, which should enable a quick and accurate diagnosis. The type of injury differs in Asian patients and non-Asian patients, which makes differential diagnosis more difficult.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Clinical Research Ethics Committee of Anhui Medical University. The patients/participants provided their written informed consent to participate in this study.
JZ, YT, and KW contributed to the study design. JZ, DX, XY, CW, and XL contributed to the data collection. JZ, YZ, YJ, YT, and NZ contributed to the data analysis and interpretation. JZ, YT, YJ, and XJ contributed to the manuscript preparation. All authors contributed to the article and approved the submitted version.
This study was supported by the National Natural Science Foundation of China (81901135, 32071054) and the 2019 Natural Science Foundation of Universities of Anhui Province (KJ2019A0243).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.627183/full#supplementary-material
1. Kaar SJ, Ferris J, Waldron J, Devaney M, Ramsey J, Winstock AR. Up: the rise of nitrous oxide abuse. An international survey of contemporary nitrous oxide use. J Psychopharmacol. (2016) 30:395–401. doi: 10.1177/0269881116632375
2. van Amsterdam J, Nabben T, van den Brink W. Recreational nitrous oxide use: prevalence and risks. Regul Toxicol Pharmacol. (2015) 73:790–6. doi: 10.1016/j.yrtph.2015.10.017
3. Zheng D, Ba F, Bi G, Guo Y, Gao Y, Li WS. The sharp rise of neurological disorders associated with recreational nitrous oxide use in China: a single-center experience and a brief review of Chinese literature. J Neurol. (2020) 267:422–9. doi: 10.1007/s00415-019-09600-w
4. Keddie S, Adams A, Kelso ARC, Turner B, Schmierer K, Gnanapavan S, et al. No laughing matter: subacute degeneration of the spinal cord due to nitrous oxide inhalation. J Neurol. (2018) 265:1089–95. doi: 10.1007/s00415-018-8801-3
5. Oussalah A, Julien M, Levy J, Hajjar O, Franczak C, Stephan C, et al. Global burden related to nitrous oxide exposure in medical and recreational settings: a systematic review and individual patient data meta-analysis. J Clin Med. (2019) 8:551. doi: 10.3390/jcm8040551
6. Winstock A, Barratt M, Ferris J, Maier L. Global overview and highlights. Global Drugs Survey. (2017). Available online at: https://www.globaldrugsurvey.com/past-findings/gds2017-launch/
7. Buizert A, Sharma R, Koppen H. When the laughing stops: subacute combined spinal cord degeneration caused by laughing gas use. J Addict Med. (2017) 11:235–6. doi: 10.1097/ADM.0000000000000295
8. Reynolds E. Vitamin B12, folic acid, and the nervous system. Lancet Neurol. (2006) 5:949–60. doi: 10.1016/S1474-4422(06)70598-1
9. Nouri A, Patel K, Montejo J, Nasser R, Gimbel DA, Sciubba DM, et al. The role of vitamin B12 in the management and optimization of treatment in patients with degenerative cervical myelopathy. Global Spine J. (2019) 9:331–7. doi: 10.1177/2192568218758633
10. Fang X, Li W, Gao H, Ma Y, Dong X, Zheng D, et al. Skin hyperpigmentation: a rare presenting symptom of nitrous oxide abuse. Clin Toxicol. (2020) 58:476–81. doi: 10.1080/15563650.2019.1665181
11. Yuan JL, Wang SK, Jiang T, Hu WL. Nitrous oxide induced subacute combined degeneration with longitudinally extensive myelopathy with inverted V-sign on spinal MRI: a case report and literature review. BMC Neurol. (2017) 17:222–5. doi: 10.1186/s12883-017-0990-3
12. Dong X, Ba F, Wang R, Zheng D. Imaging appearance of myelopathy secondary to nitrous oxide abuse: a case report and review of the literature. Int J Neurosci. (2019) 129:225–9. doi: 10.1080/00207454.2018.1526801
13. Hirvioja J, Joutsa J, Wahlsten P, Korpela J. Recurrent paraparesis and death of a patient with 'whippet' abuse. Oxf Med Case Rep. (2016) 2016:41–3. doi: 10.1093/omcr/omw012
14. Algahtani H, Shirah B, Abdelghaffar N, Abuhawi O, Alqahtani A. Nitrous oxide recreational abuse presenting with myeloneuropathy and mimicking Guillain-Barre syndrome. Intractable Rare Dis Res. (2020) 9:54–7. doi: 10.5582/irdr.2020.01007
15. Sukla KK, Raman R. Association of MTHFR and RFC1 gene polymorphism with hyperhomocysteinemia and its modulation by vitamin B12 and folic acid in an Indian population. Eur J Clin Nutr. (2012) 66:111–8. doi: 10.1038/ejcn.2011.152
16. Bao L, Li Q, Li Q, Chen H, Zhang R, Shi H, et al. Clinical, electrophysiological and radiological features of nitrous oxide-induced neurological disorders. Neuropsychiatr Dis Treat. (2020) 16:977–84. doi: 10.2147/NDT.S236939
17. Xiao CP, Ren CP, Cheng JL, Zhang Y, Li Y, Li BB, et al. Conventional MRI for diagnosis of subacute combined degeneration (SCD) of the spinal cord due to vitamin B-12 deficiency. Asia Pac J Clin Nutr. (2016) 25:34–8. doi: 10.6133/apjcn.2016.25.1.04
18. Vasconcelos OM, Poehm EH, McCarter RJ, Campbel WW, Quezado ZMN. Potential outcome factors in subacute combined degeneration: review of observational studies. J Gen Intern Med. (2006) 21:1063–8. doi: 10.1111/j.1525-1497.2006.00525.x
19. Sun HY, Lee JW, Park KS, Wi JY, Kang HS. Spine MR imaging features of subacute combined degeneration patients. Eur Spine J. (2014) 23:1052–8. doi: 10.1007/s00586-014-3191-4
20. Tani J, Weng HY, Chen HJ, Chang TS, Sung JY, Lin CS. Elucidating unique axonal dysfunction between nitrous oxide abuse and vitamin B12 deficiency. Front Neurol. (2019) 10:704. doi: 10.3389/fneur.2019.00704
21. Cao J, Su ZY, Xu SB, Liu CC. Subacute combined degeneration: a retrospective study of 68 cases with short-term follow-Up. Eur Neurol. (2018) 79:247–55. doi: 10.1159/000488913
22. Maler JM, Seifert W, Hüther G, Wiltfang J, Rüther E, Kornhuber J, et al. Homocysteine induces cell death of rat astrocytes in vitro. Neurosci Lett. (2003) 347:85–8. doi: 10.1016/S0304-3940(03)00655-4
23. Singh SK, Misra UK, Kalita J, Bora HK, Murthy RC. Nitrous oxide related behavioral and histopathological changes may be related to oxidative stress. Neurotoxicology. (2015) 48:44–9. doi: 10.1016/j.neuro.2015.03.003
24. Anderson M, Hollatz T. “Whippet” into your differential. Chest. In: Conference: CHEST 2015. Montreal, QC: Conference Publication (2015).
25. Lewis SJ, Ebrahim S, Smith GD. Meta-analysis of MTHFR 677C->T polymorphism and coronary heart disease: does totality of evidence support causal role for homocysteine and preventive potential of folate? BMJ. (2005) 331:1053. doi: 10.1136/bmj.38611.658947.55
26. Fedosov SN, Brito A, Miller JW, Green R, Allen LH. Combined indicator of vitamin B12 status: modification for missing biomarkers and folate status and recommendations for revised cut-points. Clin Chem Lab Med. (2015) 53:1215–25. doi: 10.1515/cclm-2014-0818
27. Zhao B, Zhao L, Li Z, Zhao R. Subacute combined degeneration induced by nitrous oxide inhalation: two case reports. Medicine. (2020) 99:e19926. doi: 10.1097/MD.0000000000019926
Keywords: nitrous oxide, vitamin B12, homocysteine, spinal cord disease, peripheral nervous system diseases
Citation: Zhang J, Xie D, Zou Y, Yu X, Ji Y, Wang C, Lv X, Zhou N, Jiang X, Wang K and Tian Y (2021) Key Characteristics of Nitrous Oxide-Induced Neurological Disorders and Differences Between Populations. Front. Neurol. 12:627183. doi: 10.3389/fneur.2021.627183
Received: 08 November 2020; Accepted: 01 April 2021;
Published: 27 April 2021.
Edited by:
Xin-Ming Shen, Mayo Clinic, United StatesReviewed by:
Xiaochu Zhang, University of Science and Technology of China, ChinaCopyright © 2021 Zhang, Xie, Zou, Yu, Ji, Wang, Lv, Zhou, Jiang, Wang and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanghua Tian, YXlmeXR5aEAxMjYuY29t; Kai Wang, d2FuZ2thaTE5NjRAMTI2LmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.