- 1Department of Neurology, Tianjin Medical University General Hospital, Tianjin, China
- 2Laboratory of Epidemiology, Tianjin Neurological Institute, Tianjin, China
- 3Key Laboratory of Post-neuroinjury Neuro-repair and Regeneration in Central Nervous System, Tianjin Neurological Institute, Ministry of Education and Tianjin City, Tianjin, China
- 4Department of Cardiology, Tianjin Medical University General Hospital, Tianjin, China
- 5Department of Neurology, North China University of Science and Technology Affiliated Hospital, Tangshan, China
- 6Department of Internal Medicine, Tianjin Jizhou People's Hospital, Tianjin, China
- 7Department of Neurosurgery, Tianjin Jizhou People's Hospital, Tianjin, China
This study aimed to explore trends in the burden from stroke associated with home quarantine during the COVID-19 pandemic. Patients with a first-ever stroke registered between January 1 and April 20 from 2010 to 2020 were included in this study. We compared the incidence and the rates of mortality, hospitalization, and diagnosis by neuroimaging for first-ever stroke among a low-income population in rural China during the study periods. Overall, 377 first-ever stroke patients were analyzed in this study period; men accounted for 59.2%. Compared with 2019, the incidence of first-ever stroke was 73.5% lower in 2020 (P < 0.001). The incidence of first-ever stroke was lower by 64.18% in 2020 than in the previous 5 years (P = 0.002) and by 65.42% in 2020 than in the previous 10 years (P = 0.001). Mortality from first-ever stroke in 2020 was not significantly different from that in 2019, but it was noticeably lower than that for the previous 5 and 10 years. However, rates of hospitalization and diagnosis by neuroimaging remained stable across the study period. These findings suggest that the home quarantine helped reduce outdoor activities at low temperatures, restrict gatherings, reduce alcoholism and high-fat diet, and lower pollution caused by factories. These changes were advantageous for helping high-risk groups to reduce the burden of stroke.
Introduction
The World Health Organization officially classified the novel COVID-19 outbreak as a global pandemic on March 11, 2020. As of April 22, 2020, the cumulative number of affected patients worldwide was more than 2.3 million. Not only has COVID-19 had a serious impact on health and the economy worldwide, but it has also brought about major changes in people's lives. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is extremely contagious. Over the last several months, governments across the world have issued self-isolation orders as a result of the COVID-19 outbreak. In China, the government issued a rule on January 23, 2020 to seal off the city of Wuhan, with a subsequent nationwide compulsory isolation order. These actions played an impressive role in blocking the spread of SARS-CoV-2.
Some studies have reported that patients with existing cardiovascular diseases may be at greater risk of developing severe COVID-19 (1, 2). An Italian study reported that cases of ischemic stroke decreased in the casualty department during the COVID-19 epidemic (3). However, the impact of isolation during the pandemic on chronic non-communicable diseases remains unknown, especially in low-income populations. Thus, we aimed to assess the effects of compulsory isolation during the COVID-19 pandemic on the burden of stroke in a low-income population in rural China.
Methods
Participants and Study Design
The study population came from the Tianjin Brain Study (4, 5), which began in 1985 as an on-going population-based study conducted in Tianjin, China, a township of Jizhou District that contains 18 administrative villages. The total population of this township was 14,285 in 2010 and 14,534 as of April 20, 2020; 95% are low-income farmers whose annual per capita income was <100 USD in 1991 and <1,000 USD in 2010.
Since January 23, 2020, strict measures for controlling the COVID-19 epidemic have been enforced and strengthened after the lock-down strategy implemented in Wuhan, China (6). On January 24, 2020, a first-level public health emergency response was carried out in Tianjin and the counties under its jurisdiction (7). Tourist attractions, entertainment venues, libraries, and schools were ordered to shut down. It was recommended that healthy residents stay at home and avoid mass gatherings to reduce the spread of the virus. People returning home from other provinces and cities were required to be in a centralized quarantine facility and to undergo medical observation for more than 14 days. Symptomatic patients and those suspected to be infected were required to receive treatment in an isolation ward (8, 9).
Tianjin is one of four municipalities in China, which includes 15 administrative districts. Overall, 136 patients were diagnosed with SARS-CoV-2 infections from 13 administrative districts in Tianjin during the study period. However, Jizhou District is one of two districts with zero infection cases of SARS-CoV-2 in Tianjin.
The research protocol was approved by Tianjin Medical University General Hospital Ethics Committee, and all patients provided written informed consent.
Data Collection
Information on stroke patients was collected by the stroke surveillance network, which has been described previously (4). Briefly, in the Tianjin Brain Study, local licensed village physicians report stroke cases to physicians in community hospitals within 24 h of stroke onset. Physicians from the community hospital then visit the stroke patients' homes to confirm the stroke event and obtain information about the characteristics and clinical features. They then report confirmed and suspected stroke cases monthly to Tianjin Medical University General Hospital. Then, neurologists from Tianjin Medical University General Hospital use interviews to identify possible stroke events. The local licensed village physicians and the physicians from the community hospital are trained annually by a qualified neurologist.
Information was obtained by questionnaire about patients' age and education. Data regarding stroke subtypes, whether a diagnosis was made using computed tomography, and whether patients were hospitalized were collected within 24 h after patient admission was obtained by related medical records. In this study, patients were divided into three age groups: <45, 45–64, and ≥65 years. Education levels used years as the unit of measurement. Patients were divided into three education level groups: 0, 1–6, and ≥7 years.
Definition of Stroke Events
First-ever stroke was defined as the first occurrence (i.e., without a history of stroke) of a rapidly developed focal (or global) disorder of cerebral function of vascular origin that lasted more than 24 h (10).
Stroke was categorized into three subtypes: hemorrhagic stroke, ischemic stroke (IS), and uncategorized stroke. Hemorrhagic stroke was defined as an intracerebral hemorrhage (ICH) or subarachnoid hemorrhage. IS was defined as a thrombotic brain infarction due to temporary or permanent occlusion of a feeding artery or of venous thrombosis. Uncategorized stroke was defined when patients' strokes could not be categorized as hemorrhagic stroke or IS or when there was a lack of evidence of neuroimaging. Patients with transient ischemic attacks, subarachnoid hemorrhage, and silent stroke, a kind of stroke detected only by imaging, were excluded in this study. Stroke was diagnosed by a professional neurologist based on typical clinical symptoms combined with imaging findings. Patients without neuroimaging in this study were diagnosed as having full clinical strokes with significant clinical symptoms and signs. For this study, all-cause mortality of stroke patients was used for mortality data.
Statistical Analyses
Patients with a first-ever stroke who were registered between January 1 and April 20 for the years 2010 through 2020 were included in this study. Moreover, patients who died from stroke each year (i.e., 2010 through 2020) between January 1 and April 20 were also included in this study. Continuous variables, including age and education level, were analyzed with Student's t-tests and presented as means and standard deviations. Categorical variables are presented as frequencies and 95% confidence intervals (CIs); differences between groups were compared using chi-squared tests. All participants were categorized into three age groups (<45, 45–64, and ≥65 years) and three education groups based on the number of years of formal education (0, 1–6, and ≥7 years). The incidence of first-ever stroke events every year from 2010 to 2020 were calculated separately using the corresponding person-years. The age-standardized incidences were calculated with the direct method using the world standard population by 10 age groups: <35, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, and ≥75 years (11).
Changes in rates were calculated as follows: (rate in 2020—rate in reference years)/rate of reference years, and results are expressed as percentages. Differences in the incidence and rates of mortality, hospitalization, and diagnosis by neuroimaging between 2010 and 2020 were analyzed using the chi-squared test. Statistical significance was defined as P < 0.05. SPSS version 19.0 for Windows (IBM Corp., Armonk, NY) was used for analyses.
Results
Demographic and Clinical Characteristics of Patients With the First-Ever Stroke
Overall, there were 377 new cases between January 1 and April 20 for 2010 through 2020; men accounted for 59.2% (n = 223) of subjects. The average age was 65.7 years old overall (65.21 years for men and 66.42 years for women). The mean education level was 4.32 years (4.92 years for men and 3.44 years for women). There were 309 cases of IS (accounting for 82.0% of cases) and 62 cases of ICH (accounting for 16.4% of cases). Of these cases, 86.5% of patients were diagnosed by neuroimaging, but the rate of hospitalization was only 43% (Table 1).
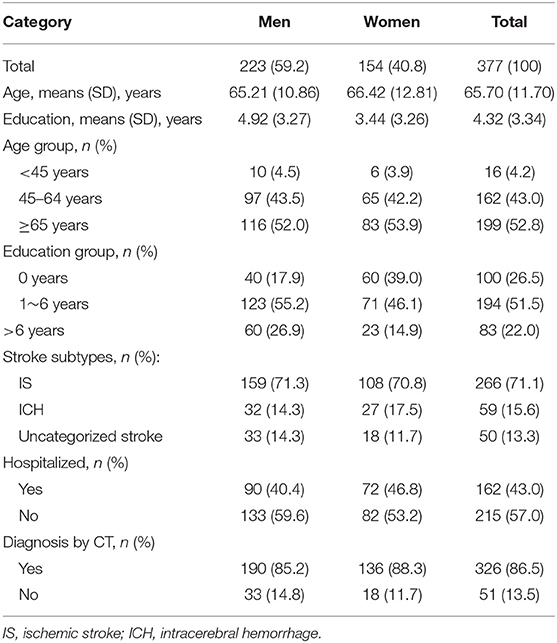
Table 1. Characteristics of the first-ever stroke from January 1st to April 20th during 2010 to 2020 in Tianjin Brain Study.
Incidence of and Mortality From First-Ever Stroke for 2010 Through 2020
Table 2 shows that the incidence of first-ever stroke in 2020 was 61.92/100,000 person-years overall (77.73 for men and 44.02 for women). The highest incidence was among those people aged 65 years and older (344.12/100,000 person-years). The incidence of IS was 43.68/100,000 person-years and of ICH was 5.66/100,000 person-years. Simultaneously, mortality per 100,000 person-years in this period was 6.88 overall (12.96 for men, 68.82 for people aged 65 years and older). There was a noticeably lower incidence in 2020 than in any other time from 2010 through 2019 (Figure 1). Similar trends were observed for mortality.
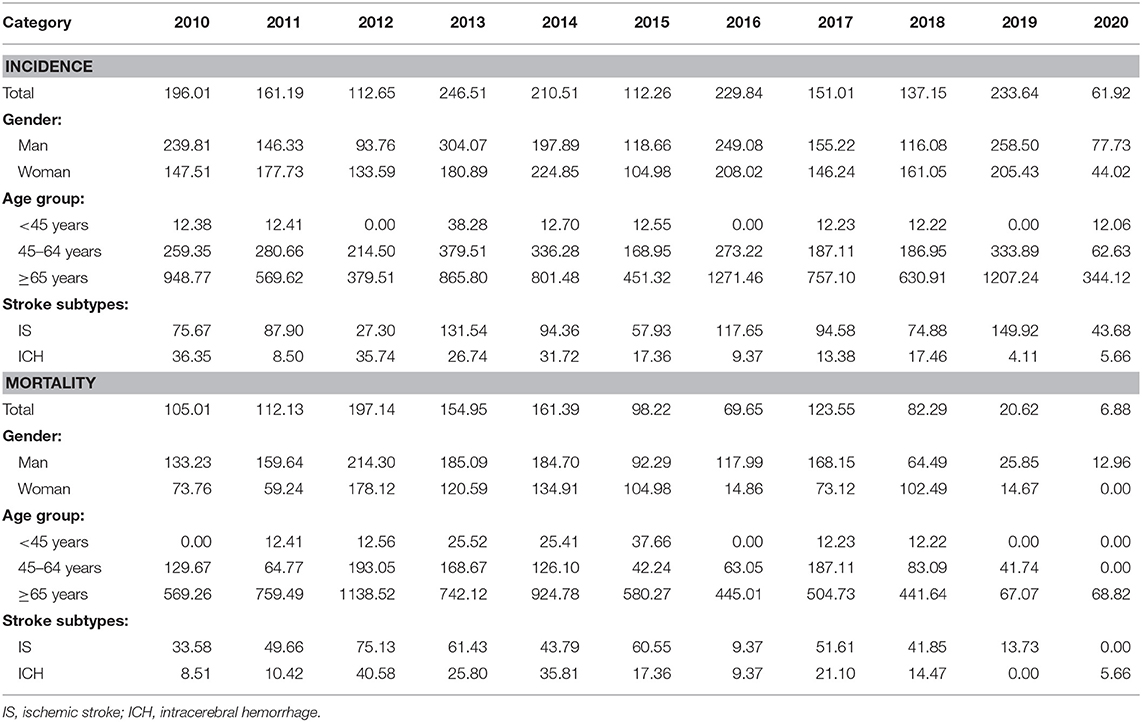
Table 2. The incidence and mortality of first-ever stroke from 1st January to 20th April during 2010 to 2020 (per 100 000 person-year).
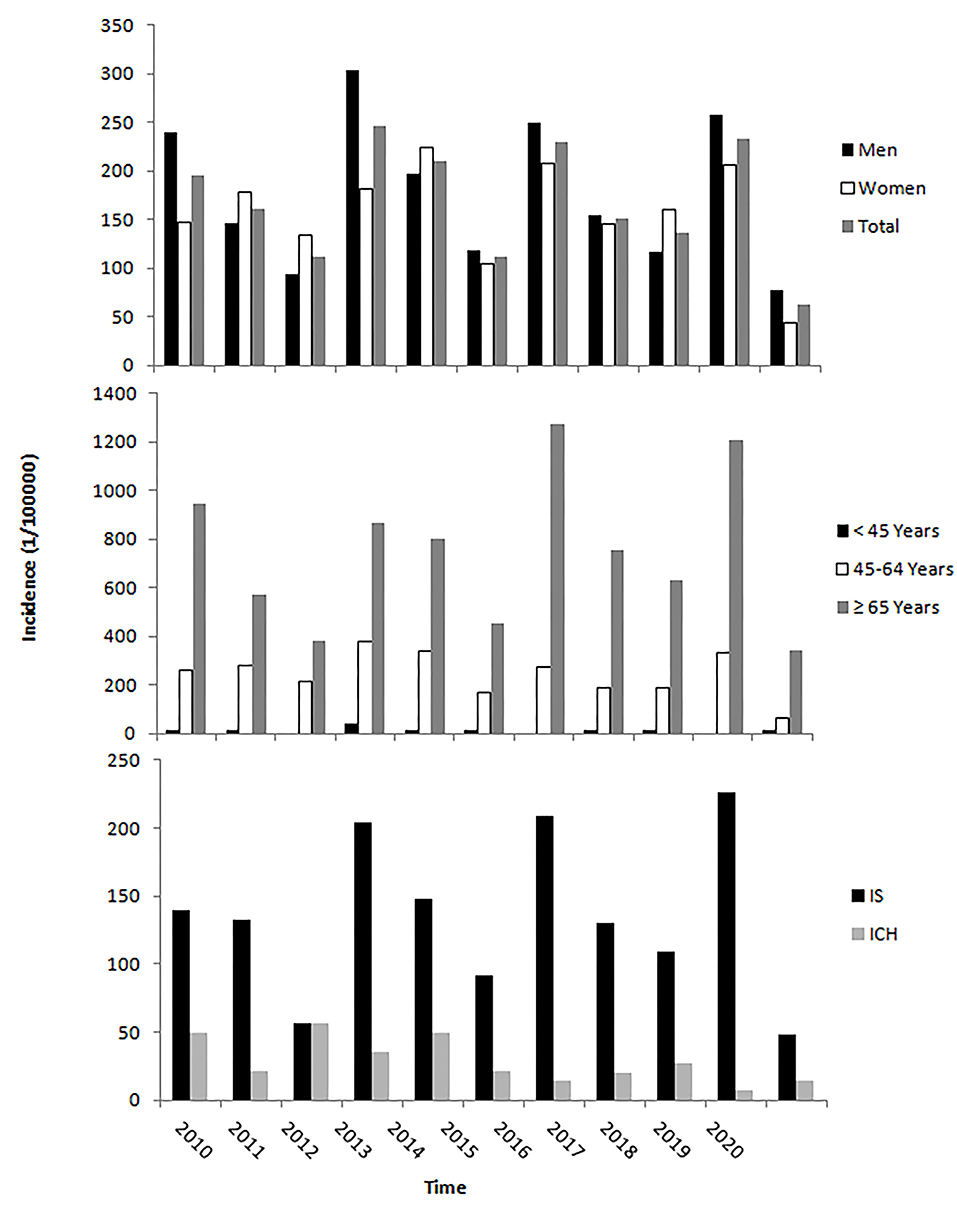
Figure 1. The incidence of the first-ever stroke from January 1 to April 20 during 2010 to 2020. The incidence of the first-ever stroke from 1st January to 20th April in 2020 was lower than that in the same time in previous years across sex, age, and stroke types.
Hospitalization and Diagnosis by Neuroimaging for 2010 to 2020
Table 3 shows that the hospitalization rate for first-ever stroke in 2020 was 77.78%; overall, 83.33% were men and 66.67% were women. The hospitalization rate was 100% in patients aged <45 years old. Moreover, the rate of diagnosis by neuroimaging in 2020 was 100% across sex, age, and stroke subtype groups.
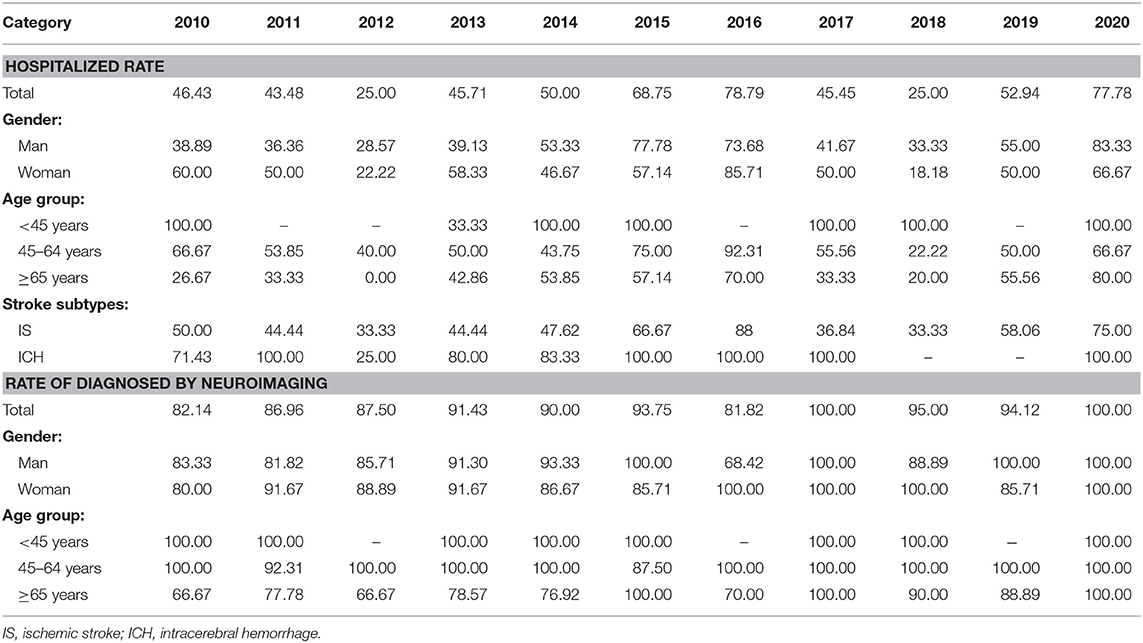
Table 3. Trends in the hospitalized rate and diagnosed by neuroimaging of first-ever stroke from 1st January to 20th April during 2010 to 2020 (%).
Variation in Stroke Burden for 2020 vs. 2010–2019
Compared with the incidence of first-ever stroke in 2019, that in 2020 was 73.5% lower overall [P < 0.001; 69.93% for men [P = 0.006] and 78.57% for women [P = 0.008]]. There were similar trends in incidence for 2020 compared with that in the previous 5 years (2015–2019) and the previous 10 years (2010–2019), all P < 0.05. The overall incidence of first-ever stroke was significantly lower in 2020 than in the previous 5 years (64.18% lower; P = 0.002) and in the previous 10 years (65.42% lower; P = 0.001). These decreases were observed in both men (56.70 and 58.65% lower, respectively) and women (74.72 and 73.95% lower, respectively), but there was a greater difference observed for women. Moreover, the decreasing tendency was observed among those patients aged 45 years and over and with ischemic stroke across times. Of these, the greatest decrease was observed in patients aged 45–64 years, with a decrease of 81.24% from that in 2019 (P = 0.003). However, during the study period, the incidence of first-ever stroke remained stable for those patients aged <45 years and for those with ICH. There were no significant changes in mortality from first-ever stroke between 2019 and 2020, but mortality was noticeably lower than that for the previous 5 and 10 years across the sexes, age groups, and stroke types, except for patients aged <45 years and those with ICH.
The rates of hospitalization and diagnosis by neuroimaging remained stable across the study period (Table 4).
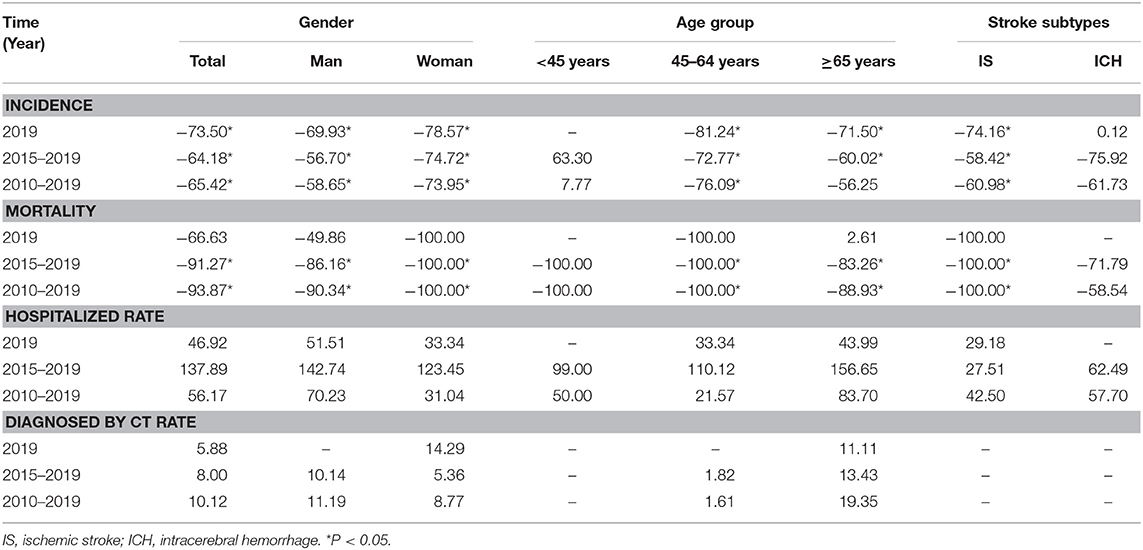
Table 4. Changes of the stroke burden from January 1st to April 20th in 2020 comparing to the same periods during 2010 to 2019 (%).
Discussion
In this study, we assessed the effects of compulsory isolation during the COVID-19 pandemic on the burden of stroke in rural China in a low-income population. We compared the current incidence and rates of mortality, hospitalization, and diagnosis by neuroimaging for first-ever stroke during the COVID-19 pandemic in 2020 to those for previous years among a low-income population in rural China. We found that the incidence in 2020 was much lower than that in other time periods from 2010 through 2019 both in men and in women, in those aged 45 years and older, and for IS regardless of whether the reference was 2019, 2015–2019, and 2010–2019. Similar results were observed in mortality for 2015–2019 and 2010–2019. However, the rates of hospitalization and diagnosis by neuroimaging remained stable across the study period.
As the main cause of death worldwide, epidemiological trends of stroke have been receiving much attention. With the development of treatment and nursing technology, the fatality rate of stroke will gradually decrease and the patient's prognosis will be improved. In addition, the popularization of medical insurance will increase the detection rate of mild strokes. From 2010 to 2020, China's economy and medical level indeed have achieved rapid development. However, our previous research in this population found that first-ever stroke incidence increased by an average of 10.7% per 1,000 USD increase in overall per capita gross domestic product adjusted for purchasing power parity and by 12.0% per 1,000 Yuan increase in per capita net income (12). Moreover, the incidence of first-ever stroke in this study population showed an increasing trend from 1992 to 2018 (13–15). However, the burden of stroke from January to April 2020 was contrary to previous research trends, and the present study showed that the incidence and mortality of stroke decreased dramatically during the COVID-19 pandemic.
It is well-known that drinking alcohol and consuming a high-fat diet are risk factors for stroke (16–18). However, a previous study showed that drinking alcohol had positive effects on stroke onset (16). Another study reported that the cardiovascular benefits of low-moderate alcohol consumption perhaps might have been overestimated and that alcohol consumption may have no positive health effects (19). In addition, an animal experiment confirmed that prolonged consumption of a high-fat diet aggravates the condition of stroke (20). An Iranian case-control study demonstrated that the risk of stroke increased as high-fat diet consumption increased (21).
The Spring Festival is the biggest festival in China and occurs on the first day in the lunar calendar. The longest vacations in China are during Spring Festival, which often continues for 7 days. During that time, whole families not only hold a dinner party every day, but they also visit relatives, neighbors, and friends to pay a New Year call. This visitation and reunion results in drinking alcohol, consuming a high-fat diet, and extra excitement and tension. Consequently, Spring Festival is the peak time of stroke onset every year. Thus, home quarantine to a large extent caused people to avoid other people, drinking alcohol, and consuming a high-fat diet, which has been shown to be a risk factor for stroke (16–18).
Moreover, outdoor temperature seems to be related to cerebrovascular events risk. A previous study reported that the mortality of stroke was related with temperature, and cold temperatures were the main cause of increased stroke burden (22). Another national study in China also reported that both low and high temperature may increase the risk of stroke mortality, while the potential effect of cold temperature might last more than 2 weeks (23). Moreover, even a moderate decrease in temperature can increase the risk of ischemic stroke (24). The outdoor temperature in Tianjin from January to April is −3 to 4°C (25), which is the winter in Tianjin. Therefore, limiting outdoor activity and augmenting time spent indoors may contribute to the decreased incidence of first-ever stroke by inhibiting elevations in blood pressure. In addition, factories cut production or even shut down entirely during the COVID-19 pandemic, which indirectly reduced pollutant emissions. In the first half of 2020, the PM 2.5 concentration in Tianjin was 53 μg/m3, a year-on-year decrease of 7.0% (26). The risk of stroke has been shown to increase among people with long-term exposure to particulate matter PM 2.5 (27). Short-term exposure to particulates in air pollution has been shown to be associated with increased mortality from ischemic heart disease (2). Therefore, shutting down factories and production so that pollutant emissions are reduced may indirectly decrease stroke incidence and mortality.
Finally, a previous study has reported that viral infections can increase the risk of stroke and that the risk of stroke decreases by 24% after influenza vaccination (28, 29). A Spanish study demonstrated that hospitalization and mortality rates for stroke increased as influenza rates increased (30). Moreover, some studies have shown that the risks of morbidity and mortality were higher among older adults infected with viruses (31, 32), especially in January and February in North China. However, the spread of common influenza was effectively reduced due to compulsory isolation during the COVID-19 pandemic. In the present study, the incidence of first-ever stroke in 2020 was 81.24% lower in those aged 45–64 years and 71.5% lower in those aged 65 years and older compared with those for the preceding years.
During the period of the COVID-19 pandemic, the primary health care system in China played an important role in blocking transmission. Local rural physicians measured body temperature, handed out disinfection materials, and propagated the knowledge of prevention daily door-to-door. This practice was implemented to find new stroke patients early during this special period and thereby avoid delays in medical services due to isolation and allow patients to obtain timely medical treatment. In this study, it was observed that, compared with the same 4-months period in the past 10 years, the rates of hospitalization and diagnosis by neuroimaging in 2020 did not decrease during the COVID-19 pandemic. This result shows that home quarantine did not affect medical care-seeking behavior for stroke patients.
There are several limitations of this study. First, the study population was from 18 villages in Tianjin, which is not representative of the whole population in China. However, the large population study design and long study period may have reduced the impact of limited representation on the study results. Second, the observation period in 2020 only included the first 4 months. Thus, this result is not representative of the whole year. We would like to continue to follow to the end of the year and assess the whole impact of the pandemic on the burden of stroke in 2020. Finally, the data were analyzed using only descriptive statistics; we did not adjust for any potential confounders that could have affected the estimates of these changes. This statistical method could have partially affected results in this study.
Conclusions
This paper is the first report to demonstrate trends in the incidence and mortality of stroke associated with home quarantine during the COVID-19 pandemic in a low-income population in China. The incidence of first-ever stroke in 2020 was much lower than that from 2010 to 2019. A similar trend was observed for mortality when compared with that in 2015–2019 and 2010–2019. Moreover, the rates of hospitalization and diagnosis by neuroimaging in 2020 remained stable across the study period. Thus, home quarantine may play a beneficial role in preventing stroke in rural China. In addition, even though COVID-19 was a huge challenge for the health system, medical services have not been affected in China. These findings suggest that the home quarantine helped reduce outdoor activities at low temperatures, the restrict gatherings, reduction alcoholism and high-fat diet, and decrease pollution caused by factories, etc. These changes may have been advantageous for helping high-risk groups to reduce the burden of stroke. It is crucial to explore simple and valid approaches to reduce the burden of chronic non-communicable diseases.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Tianjin Medical University General Hospital Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
XN, JLi, and JW were involved in conception and design and data interpretation for this article. JLiu, QY, XZ, QL, YY, DG, WM, JT, and ZL were involved in data collection, case diagnosis, and confirmation for this article. JLiu, QY, and XZ were involved in manuscript drafting. JW was involved in data analysis for this article. JW and XN were involved in the critical review in for this article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank all participants of the Tianjin Brain Study and local medical care professionals for their valuable contributions. We pay the highest respect to all medical personnel fighting on the front line of fighting the COVID-19 epidemic.
References
1. Khosravani H, Rajendram P, Notario L, Chapman MG, Menon BK. Protected code stroke: hyperacute stroke Management during the coronavirus disease 2019 (COVID-19) pandemic. Stroke. (2020) 51:1891–5. doi: 10.1161/STROKEAHA.120.029838
2. Aggarwal G, Lippi G, Michael Henry B. Cerebrovascular disease is associated with an increased disease severity in patients with coronavirus disease 2019 (COVID-19): a pooled analysis of published literature. Int J Stroke. (2020) 15:385–9. doi: 10.1177/1747493020921664
3. Morelli N, Rota E, Terracciano C, Immovilli P, Spallazzi M, Colombi D, et al. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 Era. Eur Neurol. (2020) 83:213–5. doi: 10.1159/000507666
4. Wang J, An Z, Li B, Yang L, Tu J, Gu H, et al. Increasing stroke incidence and prevalence of risk factors in a low-income Chinese population. Neurology. (2015) 84:374–81. doi: 10.1212/WNL.0000000000001175
5. Wang J, Ning X, Yang L, Tu J, Gu H, Zhan C, et al. Sex differences in trends of incidence and mortality of first-ever stroke in rural Tianjin, China, from 1992 to 2012. Stroke. (2014) 45:1626–31. doi: 10.1161/STROKEAHA.113.003899
6. Wuhan COVID-19 Prevention and Control Headquarters Issued Circular No. 3. Available online at: http://www.xinhuanet.com/politics/ (accessed April 23, 2020).
7. Tianjin Initiates First-Level Public Health Emergency Response To COVID-19. Available online at: http://www.chinanews.com/gn/ (accessed April 23, 2020).
8. Firm Confidence to Win the War of Prevention and Control of Epidemic Situation—The Decision-Making and Deployment of the Politburo Standing Committee Meeting of the Cpc Central Committee Triggered a Strong Response from the Cadres and the Masses. Available online at: http://www.locpg.gov.cn/jsdt/ (accessed April 23, 2020)
9. Tianjin Municipal Health Commission. Notice on Issuing the Implementation Plan (Trial) of Community Prevention and Control of COVID-19 in Tianjin. Available online at: http://wsjk.tj.gov.cn/art/2020/1/30/art_92_71078.html (accessed April 20, 2020).
10. Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T. Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ. (1980) 58: 113–30.
11. Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M. Age Standardization of Rates: A New Who World Standard. (GPE Discussion Paper Series, No 31). EIP/GPE/EBD, WHO, Geneva (2001).
12. Zhao P, Liu J, Hao Y, Lin Q, Gao Y, Tu J, et al. Macroeconomic Development and dramatic increase in stroke burden in rural China: a 25-year population-based study. Front Neurol. (2020) 11: 385. doi: 10.3389/fneur.2020.00385
13. Ning X, Sun J, Jiang R, Lu H, Bai L, Shi M, et al. Increased Stroke burdens among the low-income young and middle aged in rural China. Stroke. (2017) 48: 77–83. doi: 10.1161/STROKEAHA.116.014897
14. Lu H, Guo Z, Liu J, Zhang H, Zhao W, Wu Y, et al. Trends in stroke incidence among elderly low-income residents of rural China: a population-based study from 1992 to 2016. Aging (Albany NY). (2018) 10:3438–49. doi: 10.18632/aging.101657
15. Wang J, Bai L, Shi M, Yang L, An Z, Li B, et al. Trends in Age of first-ever stroke following increased incidence and life expectancy in a low-income Chinese population. Stroke. (2016) 47:929–35. doi: 10.1161/STROKEAHA.115.012466
16. Wood AM, Kaptoge S, Butterworth AS, Willeit P, Warnakula S, Bolton T, et al. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. (2018) 391: 1513–23. doi: 10.1016/S0140-6736(18)30134-X
17. Liu G, Li Y, Hu Y, Zong G, Li S, Rimm EB, et al. Influence of Lifestyle on incident cardiovascular disease and mortality in patients with diabetes mellitus. J Am Coll Cardiol. (2018) 71:2867–76. doi: 10.1016/j.jacc.2018.04.027
18. Kraus WE, Bhapkar M, Huffman KM, Pieper CF, Krupa Das S, Redman LM, et al. 2 years of calorie restriction and cardiometabolic risk (CALERIE): exploratory outcomes of a multicentre, phase 2, randomised controlled trial. Lancet Diabetes Endocrinol. (2019) 7:673–83. doi: 10.1016/S2213-8587(19)30151-2
19. Chiva-Blanch G, Badimon L. Benefits and risks of moderate alcohol consumption on cardiovascular disease: current findings and controversies. Nutrients. (2019) 12:108. doi: 10.3390/nu12010108
20. Fifield KE, Rowe TM, Raman-Nair JB, Hirasawa M, Vanderluit JL. Prolonged high fat diet worsens the cellular response to a small, covert-like ischemic stroke. Neuroscience. (2019) 406:637–52. doi: 10.1016/j.neuroscience.2019.01.050
21. Boroujeni HK, Saadatnia M, Shakeri F, Keshteli AH, Saneei P, Esmaillzadeh A. Dairy consumption and risk of stroke: a case-control study. Int J Prev Med. (2016) 7:2. doi: 10.4103/2008-7802.173792
22. Yang J, Yin P, Zhou M, Ou C, Li M, Li J, et al. The burden of stroke mortality attributable to cold and hot ambient temperatures: epidemiological evidence from China. Environ Int. (2016) 92–93:232–8. doi: 10.1016/j.envint.2016.04.001
23. Chen R, Wang C, Meng X, Chen H, Thach TQ, Wong CM, et al. Both low and high temperature may increase the risk of stroke mortality. Neurology. (2013) 81:1064–70. doi: 10.1212/WNL.0b013e3182a4a43c
24. Hong YC, Rha JH, Lee JT, Ha EH, Kwon HJ, Kim H. Ischemic stroke associated with decrease in temperature. Epidemiology. (2003) 14:473–8. doi: 10.1097/01.ede.0000078420.82023.e3
25. Whether China. Tianjin Weather for 12 Months. Available online at: http://www.weather.com.cn/forecast/history.shtml?areaid=101030100&month=12
26. Tianjin Ecological Security Bureau. Available online at: http://sthj.tj.gov.cn/ (accessed November 21, 2020).
27. Qiu H, Sun S, Tsang H, Wong CM, Lee RS, Schooling CM, et al. Fine particulate matter exposure and incidence of stroke: a cohort study in Hong Kong. Neurology. (2017) 88:1709–17. doi: 10.1212/WNL.0000000000003903
28. Warren-Gash C, Blackburn R, Whitaker H, McMenamin J, Hayward AC. Laboratory-confirmed respiratory infections as triggers for acute myocardial infarction and stroke: a self-controlled case series analysis of national linked datasets from Scotland. Eur Respir J. (2018) 51:1701794. doi: 10.1183/13993003.01794-2017
29. Siriwardena AN, Asghar Z, Coupland CC. Influenza and pneumococcal vaccination and risk of stroke or transient ischaemic attack-matched case control study. Vaccine. (2014) 32:1354–61. doi: 10.1016/j.vaccine.2014.01.029
30. López-Fernández L, López-Messa J, Andrés-de Llano J, Garmendia-Leiza JR, García-Cruces J, García-Crespo J. Relationship between seasonal influenza rates and hospitalization and mortality rates due to acute cardiovascular diseases in a Spanish region. Med Clin (Barc). (2019) 153:133–40. doi: 10.1016/j.medcle.2019.06.008
31. Widmer K, Zhu Y, Williams JV, Griffin MR, Edwards KM, Talbot HK. Rates of hospitalizations for respiratory syncytial virus, human metapneumovirus, and influenza virus in older adults. J Infect Dis. (2012) 206:56–62. doi: 10.1093/infdis/jis309
32. van Asten L, van den Wijngaard C, van Pelt W, van de Kassteele J, Meijer A, van der Hoek W, et al. Mortality attributable to 9 common infections: significant effect of Influenza A, respiratory syncytial virus, influenza B, norovirus, and parainfluenza in elderly persons. J Infect Dis. (2012) 206:628–39. doi: 10.1093/infdis/jis415
Keywords: stroke, epidemiology, incidence, burden, COVID-19
Citation: Liu J, Yang Q, Zhang X, Lin Q, Yang Y, Guo D, Mao W, Tu J, Liu Z, Li J, Ning X and Wang J (2021) A Sharp Decline in Burden of Stroke in Rural China During COVID-19 Pandemic. Front. Neurol. 11:596871. doi: 10.3389/fneur.2020.596871
Received: 20 August 2020; Accepted: 28 December 2020;
Published: 25 January 2021.
Edited by:
Cheng-Yang Hsieh, Sin-Lau Christian Hospital, TaiwanReviewed by:
Helen L. Po, MacKay Memorial Hospital, TaiwanHuang-tz Ou, National Cheng Kung University, Taiwan
Copyright © 2021 Liu, Yang, Zhang, Lin, Yang, Guo, Mao, Tu, Liu, Li, Ning and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinghua Wang, amh3ODc5OUB5YWhvby5jb20=; andhbmczQHRtdS5lZHUuY24=; Xianjia Ning, eG5pbmdAdG11LmVkdS5jbg==; Jidong Li, amRfbGlfZG9jdG9yQDE2My5jb20=
†These authors have contributed equally to this work
 Jie Liu
Jie Liu Qiaoxia Yang
Qiaoxia Yang Xin Zhang
Xin Zhang Qiuxing Lin
Qiuxing Lin Dandan Guo
Dandan Guo Wenjing Mao5
Wenjing Mao5 Xianjia Ning
Xianjia Ning Jinghua Wang
Jinghua Wang