
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Neurol. , 18 December 2020
Sec. Movement Disorders
Volume 11 - 2020 | https://doi.org/10.3389/fneur.2020.573576
This article is part of the Research Topic Multidisciplinary Approach to Uncovering the Pathophysiology of Tourette Syndrome View all 8 articles
 Shan-shan Cen1,2†
Shan-shan Cen1,2† Jun Yu1†
Jun Yu1† Qiao Wang3
Qiao Wang3 Wissam Deeb1,4
Wissam Deeb1,4 Kai-liang Wang3
Kai-liang Wang3 Aparna Wagle Shukla1
Aparna Wagle Shukla1 Irene Malaty1
Irene Malaty1 Adolfo Ramirez-Zamora1
Adolfo Ramirez-Zamora1 Jian-guo Zhang3
Jian-guo Zhang3 Wei Hu1*
Wei Hu1* Fan-gang Meng3,5*
Fan-gang Meng3,5*Tourette syndrome (TS) is a childhood-onset, chronic neuropsychiatric disorder characterized by multiple motor and vocal tics. TS poses a considerable burden on both patients and health care providers, leading to a major detriment of educational success, occupation, and interpersonal relationships. A multidisciplinary, specialist-driven management approach is required due to the complexity of TS. However, access to such specialty care is often dramatically limited by the patients' locations and the specialists' geographic clustering in large urban centers. Telemedicine uses electronic information and communication technology to provide and support health care when distance separates participants. Therefore, we conducted this mini-review to describe the latest information on telemedicine in the assessment and management of TS and discuss the potential contributions to care for TS patients with a multidisciplinary approach. We believe that telemedicine could be a revolutionary method in improving medical access to patients with TS.
Tourette syndrome (TS) is a complex neuropsychiatric movement disorder characterized by multiple motor tics and at least one vocal/phonic tic lasting for more than 1 year. TS is common with a prevalence of 3–8 per 1,000 children, affecting males more often than females by a ratio of about 4:1 (1). It commonly manifests during childhood but affects children, adolescents, and adults worldwide. Although some tics may be mild, others can result in significant psychosocial, physical, and functional difficulties that impair social activities, academic achievements, and employment performance. Additionally, up to 90% of patients with TS exhibit one or more comorbidities, including attention deficit hyperactivity disorder (ADHD), obsessive–compulsive disorder (OCD), sleep disorders, and other behavioral and psychosocial problems (2). These comorbid conditions cause many patients with TS to suffer from varying degrees of additional functional impairment across multiple domains.
Management of TS requires a combination of therapies to treat tics and comorbid conditions. Patients with mild and non-disabling tics should receive education, counseling, and supportive care. Therapeutic strategies for impairing tics are individually tailored, including behavioral therapy—especially the Comprehensive Behavioral Intervention for Tics (CBIT)—as the first-line option, followed by various standard and emerging pharmacologic treatments, and finally, deep brain stimulation (DBS) surgery (3). Although appropriate treatment may reduce tic frequency and severity, a large proportion of patients have a significantly impaired quality of life (QoL) compared to individuals without TS. Tic severity, greater emotional and behavioral difficulties, especially OCD, ADHD, anxiety, and depression, have shown the most significant impact on QoL (4–7).
In the current care model, evaluation and management of TS require frequent travel to tertiary centers and multiple longitudinal in-person visits. Tics are usually intermittent, fluctuating, and often less pronounced when the patient is examined face to face; thus, they can be difficult to assess during regular visits. The care is usually multidisciplinary, consisting of numerous sessions with various providers. Consequently, this increases the burden on patients and caregivers and contributes to the challenges of obtaining and maintaining comprehensive specialized care. In many areas, a severe shortage of needed specialists such as neurologists, psychiatrists, and psychologists further compound the barriers to health care access, equity, and quality (8, 9). A recent survey showed that in the United States, as many as 26% of adult patients have found it challenging to find a physician that is knowledgeable about TS (10). Furthermore, a recent study has suggested that TS also poses a tremendous economic burden on patients, families, and society. The annual TS-specific costs totaled 3,404€ per patient in Germany, with 18% direct costs and 81% indirect costs (11).
Telemedicine, defined by the Institute of Medicine as “the use of electronic and communications technologies to provide and support health care when distance separates the participants,” brings benefits to patients and health care systems by facilitating timesaving and cost-effective access to tertiary care services (12). Because of the challenges mentioned above in the evaluation and management of TS, telemedicine could be an innovative and particularly attractive approach to improving health care and outcomes for patients with TS. This article aims to review the current status of telemedicine in the assessment and management of TS and discuss the potential contributions to care for TS patients with a multidisciplinary approach.
TS belongs to a spectrum of tic disorders ranging from a provisional form to those associated with general medical conditions. The diagnosis of a tic disorder is based on historical features and observation of the tics either directly or by video recording to assess tic classification and characteristics. Tics are sudden, rapid, recurrent, non-rhythmic motor movements or phonic productions and are classified into the motor and phonic categories, with each subdivided into simple and complex groups. Simple motor tics are characterized by simple muscle movements such as eye blinking, head jerking, and shoulder shrugging. In contrast, complex motor tics comprise complex patterns of activities such as smelling, touching, hitting, jumping, bending, echopraxia (imitating observed movements), and copropraxia (making obscene gestures). Simple phonic tics include various sounds and noises such as grunting, barking, and hooting. Complex phonic tics involve linguistically meaningful vocalizations and expressions, repetition of words/syllables/phrases, echolalia (repeating other people's words), palilalia (repeating one's own words), coprolalia (obscene words or profanity), or other vocal alterations (3). The severity of tics can be evaluated by The Yale Global Tic Severity Scale, a widely used assessment instrument consisting of the Total Tic Score (composed of separate ratings on the number, frequency, intensity, complexity, and interference of motor and vocal tics) and the Tic Impairment Score (based on the impact of the tic disorder on self-esteem, family life, and social acceptance). Additionally, about 90% of adults (13) and 37% of children (14) report a premonitory urge/sensation—vaguely defined as an urge, mounting internal tension, itch, or feeling—in a crescendo fashion just before a motor or phonic tic. The premonitory urge can be a useful clue to differentiate from other repetitive movements, such as stereotypes and psychogenic movement. The Premonitory Urge for Tics Scale characterizes and quantifies premonitory urges (15). For the clinical diagnosis of TS, both the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) and the Tourette Syndrome Classification Study Group criteria (16) require the presence of both multiple motor tics and one or more phonic tics with onset before age 18 years.
Of note, a patient with a tic disorder typically has a normal neurologic examination. Possible “soft” neurologic findings may include incoordination, synkinesis (involuntary muscular movements accompanying voluntary movements), and motor restlessness—especially in individuals with comorbid ADHD individuals. There is no definitive diagnostic laboratory test. Neuroimaging studies are also typically normal.
In addition to a careful review of the medical, social, and family history for tics and tic-related disorders, the evaluation of a patient with a suspected tic disorder should also include an assessment of the common presence and detrimental effect of the coexisting conditions, as 86–90% of individuals with TS have at least one comorbid neuropsychological problem (17). ADHD symptoms are reported in 21–90% of TS patients and usually precede tics onset of tics by 2–3 years (18). A lifetime comorbid diagnosis of OCD is present in about 50% of TS patients, and the obsessive–compulsive behaviors usually emerge several years after the onset of tics during early adolescence, although an earlier age of onset has also been suggested (19). Generalized anxiety disorder is reported in 19–90% of TS patients with increased rates in children and youth (20). The presence of depression has positively correlated with earlier onset and a longer duration of tics in TS (21). There is a higher prevalence of suicidal ideations and attempts in TS (22). Episodic outbursts, rage, difficulty with aggression, and other disruptive behaviors are common and reported in 25–70% of TS populations (17). Self-injurious behavior in TS correlates with impulsivity and impulse control (23). The frequencies of poor self-concept, reduced self-esteem, antisocial activities, oppositional behaviors, schizotypal traits, and personality disorders are also increased in TS (24).
These additional issues add an extra clinical burden and can cause greater functional and social impairments than that induced by the tics. Health-related QoL assessments have shown that the presence of these comorbidities, rather than tic severity, predicts clinical outcomes (5). Thus, the evaluation of TS requires a multidisciplinary team of experts, including neurologists, psychologists, psychiatrists, and behavior therapists.
Many chronic neurological conditions, including movement disorders, impair mobility, cognitive function, and driving ability. As these diseases progress, the patients' ability to access care decreases, leaving those with the greatest need for attention receiving the least care. Particularly, the supply of pediatric and adult neurologists with expertise in childhood-onset movement disorders is limited and unevenly distributed. As such, the need for teleneurology for the evaluation and management of TS and other tics disorders is immense. Telemedicine has been shown to improve specialty care access, allowing earlier evaluation and diagnosis of movement disorders and concomitant neurological, psychiatric, and medical comorbidities (25, 26).
In the realm of movement disorders, using a telemedicine approach to detect, characterize, and monitor the motor and non-motor symptoms and, in turn, reaching a diagnosis of the hypokinetic and hyperkinetic conditions has been primarily studied in the context of Parkinson's disease (PD). National randomized controlled trials (RCTs) have confirmed the feasibility of telemedicine house calls evaluating PD patients without worsening clinical outcomes or caregiver burden or increasing the number of emergency room visits or hospitalizations (27, 28). Many studies have highlighted the feasibility, reliability, and safety of telemedicine and mobile technologies, utilizing video (even just short clips), teleconferencing, wearable devices, or other novel technologies, in motor evaluation of tremors, bradykinesia, upper and lower limb functioning, posture, gait, and dyskinesia in PD patients, with satisfactory patient compliance (29–38). Notably, several studies have shown non-inferiority of teleneurology vs. in-person visits to evaluate and assess PD using the Unified Parkinson's Disease Rating Scale (UPDRS) (37, 39). Furthermore, evaluation of voice and speech impairments in PD patients has been shown to be reliable and comparable via telecommunication vs. face-to-face visits (40). Last but not least, the feasibility and concurrent validity of performing movement assessment via video clips or teleconferencing for pediatric populations have also been reported (41, 42).
While studies demonstrating the feasibility, validity, and diagnostic accuracy of TS and other tic disorders via telemedicine are lacking, one can easily speculate that an interdisciplinary telemedicine approach for evaluating and diagnosing tic disorders, particularly TS, has bright prospects. Like PD, TS is also suitable for evaluation and management via telemedicine since TS is clinically diagnosed and most of the physical exam findings are audio-visual (43) that can be reliably collected using telemedicine technologies. Some of the signs and symptoms can be difficult to adequately elicit and capture in a typical clinical setting due to the fluctuations of symptoms and severity. Specifically, tics are typically less pronounced when the patient is being examined face to face, making telemedicine and less obtrusive remote monitoring particularly appealing.
Additionally, both TS and PD patients present with comorbid emotional, behavioral, and other psychosocial problems, requiring a comprehensive patient-centered interdisciplinary care with the active involvement of Neuropsychology and Psychiatry. Feasibility and validity of cognitive screening with the Montreal Cognitive Assessment (MoCA) in patients with movement disorders via telemedicine have been published (33–38). Telepsychiatry has also been found to be a feasible and comparable alternative to face-to-face contact for evaluating the psychiatric comorbidities for patients, including those with movement disorders, with high patient satisfaction and improved access to care (44–47). Specifically, relevant to TS, ADHD has been the most common disorder treated through telepsychiatry and is considered a reasonable alternative to an in-office visit to provide evidence-based care, especially for underserved populations of youth with ADHD (48, 49). It can help facilitate collaborative models of care to empower primary care providers to manage ADHD within their practices while also ensuring those with more severe and complicated illness getting more specialized care when needed. Similarly, a small study found that telepsychiatry resulted in near-perfect interrater agreement on rating scale scores for OCD, and both in-person and telepsychiatry approaches demonstrated excellent diagnostic reliability (50). Finally, multiple studies confirmed the feasibility and diagnostic accuracy for mood disorders via the telepsychiatry approach (51, 52). Thus, telemedicine can lower barriers for access to the scarce but much-needed subspecialty expertise and bring together a comprehensive multidisciplinary care plan, improving the health and functional outcomes and possibly enhancing the QoL of TS patients and their caregivers.
After a careful initial assessment of the tics, the presence of comorbid issues, and the resulting impairment in each scenario, either in-person or via telemedicine, an effective, comprehensive therapeutic plan for individuals with tic disorders, even though there is no cure per se, consists of a systematic tiered approach of education, behavioral therapy, pharmacotherapy, and then more invasive interventions.
The first step is to educate the patients, their family, and their school and workplace about the diagnosis, potential comorbid conditions, and indications for therapy.
Children with TS usually experience negative perceptions from their peers (53, 54). Such social rejection and isolation lead to bullying and teasing (55), actively impairing their social development (56). It is critical to educate all patients and their parents, peers, and teachers about the natural course and associated comorbidities of this condition. Children with the disorder can be fully prepared with relevant information, promoting strategies to cope with the surrounding environment and retain self-esteem (57). Simultaneously, it can improve mutual relationships and alter misconceptions.
A couple of studies examined the impact of educating peers about TS have shown positive changes in the attitude and behavioral intentions of those peers toward individuals suffering from TS (58–61). Peers that attended those studies received information by watching a video or had been provided a vignette labeling TS developed in conjunction with a team of experts. On the contrary, one study used short educational statements and failed to show a difference; the reason was thought to be insufficient information delivery (54). A similar study for elementary school teachers provided a 2-h education workshop about TS results in a 5% improvement in knowledge (62). Educating teachers is valuable since they play a vital role in the early detection and initial referral of children in need of mental health care. Besides, numerous studies examined the impact of educating folks about ADHD (1). Studies indicated that providing sufficient information to peers and teachers can alter the misconceptions and change the attitude toward a patient's behavior (63–68). Also, improving parental knowledge about ADHD can enhance treatment compliance and increase enrollment (69, 70). Moreover, the positive effects of psychoeducation intervention have been substantially discussed in other psychological disorders related to TS, such as depression and OCD, etc. (71, 72).
However, the ways of delivering education vary. There are training programs, education group sessions, or just a video-taped program, providing a range of information about TS (66, 67, 69). The literature emphasizes the importance of providing sufficient information since simply giving diagnostic labeling to peers is unhelpful (73), raising the question to find the optimal way to present knowledge effectively and conveniently (74). The satisfaction and feasibility of telemedicine-delivered psychoeducation have been demonstrated by a few studies in PTSD veterans (75), hospice caregivers (76), and stem cell transplant survivors (77). Psychoeducation has also been incorporated in remote management of depression (78, 79). Recently, the International Parkinson's Disease and Movement Disorder Society have sponsored a tele-education Parkinson's disease program for health providers in Douala (Cameroon), successfully delivering lectures through synchronous video conferences. Although post-course patient access remained unchanged, medical knowledge was improved dramatically (80). These preliminary studies prove the feasibility of providing education via telecommunication technology and hint toward potential applications in other fields. Thus, tele-psychoeducation, utilizing modern technologies such as real-time videoconference, would be a reliable method to deliver sufficient information about TS and associated comorbidities with precision. Furthermore, it would allow frequent re-evaluation to monitor long-term changes in behaviors.
While supportive care is often sufficient for many individuals with milder tics, the presence of psychosocial problems, tic-induced musculoskeletal/physical difficulties, and disruption of school work settings would indicate a need to initiate behavioral or pharmacologic tic-suppressing therapy to reduce tics to a degree where they are no longer causing significant problems.
Habit reversal therapy (HRT), notably CBIT, has become the gold standard and initial intervention for managing and coping with tics (56) without the adverse effects associated with pharmacotherapies, such as cognitive blunting, depression, weight gain, and motor dysfunction (81). CBIT is a well-established therapy consisting of HRT core component—awareness training and competing response training—along with relaxation training and functional intervention (82). Multiple clinical randomized trials and meta-analysis have consistently determined its efficacy (83, 84). Unfortunately, CBIT is not widely available due to a paucity of skilled providers (84–86).
So far, a few studies have investigated the delivery of CBIT remotely, such as the use of a website interface—TicHelper.com (87). A 2012 pilot RCT study has demonstrated comparably significant tic reduction among the 10 TS patients receiving CBIT via videoconference vs. the nine patients receiving face-to-face CBIT (25). Another 2016 RCT examined the delivery of CBIT via the Voice over Internet Protocol (VoIP) approach vs. the waitlist control and found more significant reductions in clinician-rated and patient-reported tic severity among the 12 patients in the VoIP-delivered CBIT group after 10 weeks (88). Additionally, in 2019, internet-delivered behavioral therapies were again rated as highly acceptable, credible, and satisfactory in a small 23-patient pilot study (89). Jakubovski et al. (90) created a new and sophisticated internet-delivered CBIT (iCBIT) program and designed a multicenter and prospective RCT in Germany to discover the efficacy of this program, yet there were no results published so far. Studies regarding telemedicine delivered behavior therapy for tics are summarized in Table 1.
In sum, these studies suggest that tele-CBIT is a promising tool for delivering behavioral therapies for patients with TS/tic disorders and may help increase compliance and adherence by creating alternative avenues for managing tics. These studies do have limitations, however, including small sample sizes and lack of long-term follow-up, making it difficult to draw definitive conclusions on the efficacy of tele-CBIT for the treatment of tics in patients with TS or chronic tic disorders. Data on cost-effectiveness are also lacking.
Pharmacotherapy can be considered when CBIT/HRT alone is insufficient to achieve satisfactory control of the tics and comorbid conditions (1). Recommendations regarding the sequence of pharmacologic therapy vary. In general, guanfacine, clonidine, topiramate, clonazepam, and baclofen are considered tier 1 medications and recommended for milder tics. Atypical and typical antipsychotics (including aripiprazole, risperidone, olanzapine, ziprasidone, quetiapine, pimozide, fluphenazine, haloperidol, ecopipam, sulpiride, and tiapride), VMAT-2 inhibitors (including tetrabenazine, deutetrabenazine, and valbenazine), botulinum toxins, and potentially the cannabinoids are considered tier 2 medications and reserved for more difficult to control symptoms (3). The use of pharmacotherapy can be limited by side effects such as sedation, drug-induced extrapyramidal symptoms, weight gain, and metabolic problems, leading to obstacles and even cessation. Thus, prescribing medication should be thoroughly considered whether tics causing interference on physical, social, or emotional interference determine the QoL.
So far, studies regarding the efficacy of delivering medication treatment via telemedicine to TS patients are lacking. Nevertheless, since TS and psychiatric disorders overlap in medication management, especially ADHD, we can look at the efficacy of tele-pharmacotherapy in the realm of psychiatry, which is meant to be the most frequently requested service (9, 92). Myers's study brings concrete evidence on the adherence to guideline-based care to children with ADHD and demonstrates high efficacy of providing pharmacotherapy remotely (49, 93, 94). Moreover, the ability to deliver medication management via videoconferencing has been proven in variable psychological conditions, such as depression (78, 95–97), PTSD (98), and other psychiatric conditions (45, 99). There is growing acceptance that telemedicine has successfully implemented medication management in patients with psychiatric disorders (100). Thus, there are reasons to believe that telemedicine can allow TS specialists to provide guideline-based medication treatment. However, potential challenges should be addressed, such as establishing a physician–patient relationship, coordinating with the complement mental health care system, etc. (100).
In recent years, DBS has been considered a last resort treatment option for severe TS resistant to medical and behavioral therapy (2). There is currently no consensus on the optimal brain target for tics treatment; however, our studies indicated that targeting the anteromedial globus pallidus (am GPi) or thalamic centromedian-parafascicular (CM-Pf) are more likely to reduce tic severity (101). Although utilizing DBS in TS management is still investigational, DBS has reached an innovative era. A recent study shows the reliability of predicting surgical candidacy (dystonia, essential tremor, and Parkinson's disease) for DBS through telemedicine technology and saved travel and time (102). To relieve the burden of postoperative follow-up from both sides of patients and physicians (103), engineers and clinicians have established a wireless system for DBS (104, 105), enabling DBS programmers to adjust parameters of the stimulators remotely. Studies from China (106) and Canada (107) confirm the safety and feasibility of using telemedicine for DBS follow-up. According to a recent report from China, among a total of 2,126 telemedicine visits since December 2019, 1,256 teleprogramming visits have performed, mainly for Parkinson's disease, saving a mean travel distance of 1,141 km (105).
Although the benefits of offering CBIT/HRT via telemedicine for individuals with TS/tics have been established (25, 88, 89), long-term prospective RCTs are required to study tele-CBIT/HRT and to compare this to traditional face-to-face care. Moreover, scientific evidence demonstrating the feasibility, efficacy, satisfaction, and economic value of telemedicine for TS is lacking significantly. Studies should assess the feasibility of delivering TS visits via telemedicine, which will be measured by the proportion of patients completing the assigned number of visits via telemedicine vs. in person. Also, clinicians will analyze the percentage of visits completed as scheduled, the proportion of visits completed via telemedicine vs. face-to-face office visits. Research and data are desired to measure economic benefits, such as time expenditure for each study visit, travel distance, and caregiver burden. Studies should cover more aspects of tele-treatment, including the efficacy of psychoeducation and medication management, therapeutic alliance, and adherence.
Additionally, the technology issue is still the primary concern to deliver health care for TS patients via telemedicine, regardless of the rapid advancement of technology, due to the uneven distribution of broadband. This barrier has been mentioned in multiple articles (88, 108, 109). TS patients present with sudden, rapid, non-rhythmic movements (motor tics) and vocalizations (phonic tics) that wax and wane in frequency. Thus, high-quality video and audio communication are essential in the interactions between health care providers and patients through telemedicine to precisely detect physical examination findings and perform adequate psychoeducation and behavior therapy without any disruption and delaying. According to the American Telemedicine Association (ATA) (110), telemedicine service should provide at a bandwidth of a minimum of 384 kbps in each of the downlink and uplink directions. However, the 2016 broadband progress report (111) from US Federal Communications Commission still showed a dramatic disproportion in bandwidth speed and internet access in rural/urban areas, which may impede providing adequate care for patients living far away from metropolitan areas through telemedicine. 5G, the 5th generation of the wireless network, will enable high-speed virtual connection with low latency. Ideally, a wearable device could be developed to identify quantified vocal and motor tics and would be an excellent asset for TS telemedicine.
Reimbursement and licensure have always been considered a significant barrier and were evolving in recent years. In the USA, states can reimburse Medicaid covered telemedicine services (112). Notably, most TS patients are not covered by Medicaid and have to be responsible for telemedicine costs by their families. Still, the reimbursement varies from states about what telemedicine types to include, whether and where they can be covered, etc. Thus, cost-effectiveness should be specifically assessed to demonstrate whether telemedicine can save money compared to traditional visits. Regarding licensure, generally, telemedicine is prohibited from practicing out-of-states. The Interstate Medical Licensure Compact is launched to streamline the licensing process and allow physicians to practice in multiple states, supporting the use of telemedicine. Currently, 29 states, Washington D.C., and the Territory of Guam are involved in the Compact (113). Other common concerns mentioned in previous studies include privacy/safety and establishing rapport, which should carefully be addressed in future studies in TS (114).
So far, telemedicine has been studied in the realm of movement disorders, mainly evaluated in PD, and proved to be a feasible alternation to in-person visits. As PD, TS is most likely valid for evaluation and management via video conferencing, yet telemedicine has been sparsely studied in this field. Tele-CBIT holds promise, though further prospective RCTs are required to conclude. Telemedicine has potential prospects in contributing to multidisciplinary care for TS patients who face physical or economic access issues. As in Figure 1, we propose a multidisciplinary telemedicine team for the care of patients with TS, including neurologists, psychiatrists, psychologists, and behavioral therapists. They can evaluate patients, offer management plans, provide psychosocial and behavioral interventions such as CBIT, and offer education to the patients' peers, family members, and teachers remotely via videoconferencing technology.
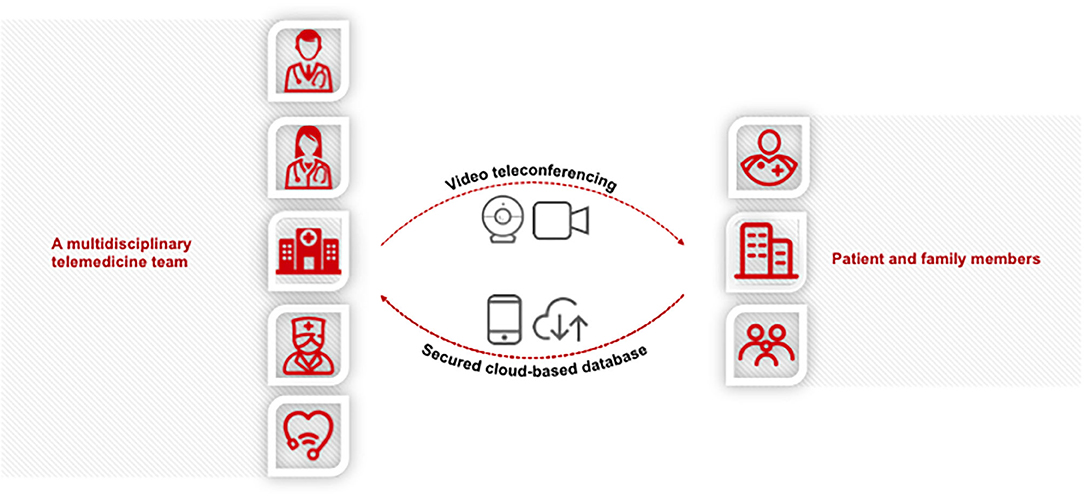
Figure 1. Schema of multidisciplinary care for the Tourette syndrome (TS) via telemedicine. Video telemedicine can be used to provide comprehensive care and support for TS patients and their families/caretakers in a timely and easily accessible fashion while ensuring patient privacy and HIPAA compliance. Neurologists and psychiatrists can evaluate the patients and offer management plans and education remotely. Behavioral therapists and psychologists can provide the Comprehensive Behavioral Intervention for Tics (CBIT), other psychosocial and behavioral interventions, and psychoeducation via telemedicine. Additional specialty service and social work needs can also be accommodated via telemedicine as appropriate. In summary, telemedicine promises to be a revolutionary approach to improve access to care for patients with TS, especially those living in more rural areas. Its feasibility, satisfaction, clinical effects, and cost-effectiveness should be assessed by further research. Potential limitations such as technological issues, reimbursement, and licensure should be addressed as well.
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Deeb W, Malaty IA and Mathews CA, Tourette disorder other tic disorders. Handb Clin Neurol. (2019) 165:123–53. doi: 10.1016/B978-0-444-64012-3.00008-3
2. Jankovic J. Treatment of tics associated with Tourette syndrome. J Neural Transm (Vienna). (2020) 127:843–50. doi: 10.1007/s00702-019-02105-w
3. Singer HS. Tics and Tourette syndrome. Continuum (Minneap Minn). (2019) 25:936–58. doi: 10.1212/con.0000000000000752
4. Evans J, Seri S, Cavanna AE. The effects of Gilles de la Tourette syndrome and other chronic tic disorders on quality of life across the lifespan: a systematic review. Eur Child Adolesc Psychiatry. (2016) 25:939–48. doi: 10.1007/s00787-016-0823-8
5. Storch EA, Merlo LJ, Lack C, Milsom VA, Geffken GR, Goodman WK, et al. Quality of life in youth with Tourette's syndrome and chronic tic disorder. J Clin Child Adolesc Psychol. (2007) 36:217–27. doi: 10.1080/15374410701279545
6. Muller-Vahl K, Dodel I, Muller N, Munchau A, Reese JP, Balzer-Geldsetzer M, et al. Health-related quality of life in patients with Gilles de la Tourette's syndrome. Mov Disord. (2010) 25:309–14. doi: 10.1002/mds.22900
7. Bernard BA, Stebbins GT, Siegel S, Schultz TM, Hays C, Morrissey MJ, et al. Determinants of quality of life in children with Gilles de la Tourette syndrome. Mov Disord. (2009) 24:1070–3. doi: 10.1002/mds.22487
8. Patel UK, Malik P, DeMasi M, Lunagariya A, Jani VB. Multidisciplinary approach and outcomes of Tele-neurology: a review. Cureus. (2019) 11:e4410. doi: 10.7759/cureus.4410
9. American Academy of C, Adolescent Psychiatry Committee on T and Issues ACoQ. Clinical Update: Telepsychiatry With Children and Adolescents. J Am Acad Child Adolesc Psychiatry. (2017) 56:875–93. doi: 10.1016/j.jaac.2017.07.008
10. Robertson MM. A personal 35 year perspective on Gilles de la Tourette syndrome: prevalence, phenomenology, comorbidities, and coexistent psychopathologies. Lancet Psychiatry. (2015) 2:68–87. doi: 10.1016/s2215-0366(14)00132-1
11. Dodel I, Reese JP, Muller N, Munchau A, Balzer-Geldsetzer M, Wasem J, et al. Cost of illness in patients with Gilles de la Tourette's syndrome. J Neurol. (2010) 257:1055–61. doi: 10.1007/s00415-010-5458-y
12. Bria WF, Finn NB. Telemedicine. In: Digital Communication in Medical Practice. Springer-Verlag London Press (2009). p. 59–73.
13. Kwak C, Dat Vuong K, Jankovic J. Premonitory sensory phenomenon in Tourette's syndrome. Mov Disord. (2003) 18:1530–3. doi: 10.1002/mds.10618
14. Banaschewski T, Woerner W, Rothenberger A. Premonitory sensory phenomena and suppressibility of tics in Tourette syndrome: developmental aspects in children and adolescents. Dev Med Child Neurol. (2003) 45:700–3. doi: 10.1017/s0012162203001294
15. Woods DW, Piacentini J, Himle MB, Chang S. Premonitory Urge for Tics Scale (PUTS): initial psychometric results and examination of the premonitory urge phenomenon in youths with Tic disorders. J Dev Behav Pediatr. (2005) 26:397–403. doi: 10.1097/00004703-200512000-00001
16. Definitions and Classification of Tic Disorders. The Tourette Syndrome Classification Study Group. Arch Neurol. (1993) 50:1013–6. doi: 10.1001/archneur.1993.00540100012008
17. Hirschtritt ME, Lee PC, Pauls DL, Dion Y, Grados MA, Illmann C, et al. Lifetime prevalence, age of risk, and genetic relationships of comorbid psychiatric disorders in Tourette syndrome. JAMA Psychiatry. (2015) 72:325–33. doi: 10.1001/jamapsychiatry.2014.2650
18. Comings DE, Comings BG. A controlled study of Tourette syndrome. I. Attention-deficit disorder, learning disorders, and school problems. Am J Hum Genet. (1987) 41:701–41.
19. Gaze C, Kepley HO, Walkup JT. Co-occurring psychiatric disorders in children and adolescents with Tourette syndrome. J Child Neurol. (2006) 21:657–64. doi: 10.1177/08830738060210081301
20. Martino D, Ganos C, Pringsheim TM. Tourette syndrome and chronic Tic disorders: the clinical spectrum beyond Tics. Int Rev Neurobiol. (2017) 134:1461–90. doi: 10.1016/bs.irn.2017.05.006
21. Rickards H, Robertson M. A controlled study of psychopathology and associated symptoms in Tourette syndrome. World J Biol Psychiatry. (2003) 4:64–8. doi: 10.3109/15622970309167953
22. Storch EA, Hanks CE, Mink JW, McGuire JF, Adams HR, Augustine EF, et al. Suicidal thoughts and behaviors in children and adolescents with chronic Tic disorders. Depress Anxiety. (2015) 32:744–53. doi: 10.1002/da.22357
23. Mathews CA, Waller J, Glidden D, Lowe TL, Herrera LD, Budman CL, et al. Self injurious behaviour in Tourette syndrome: correlates with impulsivity and impulse control. J Neurol Neurosurg Psychiatry. (2004) 75:1149–55. doi: 10.1136/jnnp.2003.020693
24. Silvestri PR, Baglioni V, Cardona F, Cavanna AE. Self-concept and self-esteem in patients with chronic tic disorders: a systematic literature review. Eur J Paediatr Neurol. (2018) 22:749–56. doi: 10.1016/j.ejpn.2018.05.008
25. Himle MB, Freitag M, Walther M, Franklin SA, Ely L, Woods DW. A randomized pilot trial comparing videoconference versus face-to-face delivery of behavior therapy for childhood tic disorders. Behav Res Ther. (2012) 50:565–70. doi: 10.1016/j.brat.2012.05.009
26. Dorsey ER, Deuel LM, Voss TS, Finnigan K, George BP, Eason S, et al. Increasing access to specialty care: a pilot, randomized controlled trial of telemedicine for Parkinson's disease. Mov Disord. (2010) 25:1652–9. doi: 10.1002/mds.23145
27. Beck CA, Beran DB, Biglan KM, Boyd CM, Dorsey ER, Schmidt PN, et al. National randomized controlled trial of virtual house calls for Parkinson disease. Neurology. (2017) 89:1152–61. doi: 10.1212/WNL.0000000000004357
28. Dorsey ER, Venkataraman V, Grana MJ, Bull MT, George BP, Boyd CM, et al. Randomized controlled clinical trial of “virtual house calls” for Parkinson disease. JAMA Neurol. (2013) 70:565–70. doi: 10.1001/jamaneurol.2013.123
29. Schoffer KL, Patterson V, Read SJ, Henderson RD, Pandian JD, O'Sullivan JD. Guidelines for filming digital camera video clips for the assessment of gait and movement disorders by teleneurology. J Telemed Telecare. (2005) 11:368–71. doi: 10.1258/135763305774472042
30. Kim HB, Lee HJ, Lee WW, Kim SK, Jeon HS, Park HY, et al. Validation of Freezing-of-Gait Monitoring Using Smartphone. Telemed J E Health. (2018) 24:899–907. doi: 10.1089/tmj.2017.0215
31. Ferraris C, Nerino R, Chimienti A, Pettiti G, Cau N, Cimolin V, et al. Feasibility of home-based automated assessment of postural instability and lower limb impairments in Parkinson's disease. Sensors (Basel). (2019) 19:1129. doi: 10.3390/s19051129
32. Sekimoto S, Oyama G, Hatano T, Sasaki F, Nakamura R, Jo T, et al. A randomized crossover pilot study of telemedicine delivered via iPads in Parkinson's disease. Parkinsons Dis. (2019) 2019:9403295. doi: 10.1155/2019/9403295
33. Abdolahi A, Bull MT, Darwin KC, Venkataraman V, Grana MJ, Dorsey ER, et al. A feasibility study of conducting the Montreal Cognitive Assessment remotely in individuals with movement disorders. Health Inform J. (2016) 22:304–11. doi: 10.1177/1460458214556373
34. Stillerova T, Liddle J, Gustafsson L, Lamont R, Silburn P. Could everyday technology improve access to assessments? A pilot study on the feasibility of screening cognition in people with Parkinson's disease using the Montreal Cognitive Assessment via Internet videoconferencing. Aust Occup Ther J. (2016) 63:373–80. doi: 10.1111/1440-1630.12288
35. Salih SA, Wootton R, Beller E, Gray L. The validity of video clips in the diagnosis of gait disorder. J Telemed Telecare. (2007) 13:333–6. doi: 10.1258/135763307782215406
36. Russell TG, Jull GA, Wootton R. The diagnostic reliability of Internet-based observational kinematic gait analysis. J Telemed Telecare. (2003) 9(Suppl. 2):S48–51. doi: 10.1258/135763303322596255
37. Hubble JP, Pahwa R, Michalek DK, Thomas C, Koller WC. Interactive video conferencing: a means of providing interim care to Parkinson's disease patients. Mov Disord. (1993) 8:380–2. doi: 10.1002/mds.870080326
38. Goetz CG, Stebbins GT, Wolff D, DeLeeuw W, Bronte-Stewart H, Elble R, et al. Testing objective measures of motor impairment in early Parkinson's disease: feasibility study of an at-home testing device. Mov Disord. (2009) 24:551–6. doi: 10.1002/mds.22379
39. Abdolahi A, Scoglio N, Killoran A, Dorsey ER, Biglan KM. Potential reliability and validity of a modified version of the Unified Parkinson's Disease Rating Scale that could be administered remotely. Parkinsonism Relat Disord. (2013) 19:218–21. doi: 10.1016/j.parkreldis.2012.10.008
40. Constantinescu G, Theodoros D, Russell T, Ward E, Wilson S, Wootton R. Assessing disordered speech and voice in Parkinson's disease: a telerehabilitation application. Int J Lang Commun Disord. (2010) 45:630–44. doi: 10.3109/13682820903470569
41. Nicola K, Waugh J, Charles E, Russell T. The feasibility and concurrent validity of performing the Movement Assessment Battery for Children - 2nd Edition via telerehabilitation technology. Res Dev Disabil. (2018) 77:40–8. doi: 10.1016/j.ridd.2018.04.001
42. Gorter H, Lucas C, Groothuis-Oudshoorn K, Maathuis C, van Wijlen-Hempel R, Elvers H. The use of video clips in teleconsultation for preschool children with movement disorders. Pediatr Phys Ther. (2013) 25:323–9. doi: 10.1097/PEP.0b013e3182983399
43. Cohen SC, Leckman JF, Bloch MH. Clinical assessment of Tourette syndrome and tic disorders. Neurosci Biobehav Rev. (2013) 37:997–1007. doi: 10.1016/j.neubiorev.2012.11.013
44. Malhotra S, Chakrabarti S, Shah R, Mehta A, Gupta A, Sharma M. A novel screening and diagnostic tool for child and adolescent psychiatric disorders for telepsychiatry. Indian J Psychol Med. (2015) 37:288–98. doi: 10.4103/0253-7176.162921
45. O'Reilly R, Bishop J, Maddox K, Hutchinson L, Fisman M, Takhar J. Is telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiatr Serv. (2007) 58:836–43. doi: 10.1176/ps.2007.58.6.836
46. Seritan AL, Heiry M, Iosif AM, Dodge M, Ostrem JL. Telepsychiatry for patients with movement disorders: a feasibility and patient satisfaction study. J Clin Mov Disord. (2019) 6:1. doi: 10.1186/s40734-019-0077-y
47. Mazhari S, Ghaffari Nejad A, Mofakhami O, Raaii F, Bahaadinbeigy K. Evaluating the diagnostic agreement between telepsychiatry assessment and face-to-face visit: a preliminary study. Iran J Psychiatry. (2019) 14:236–41.
48. Palmer NB, Myers KM, Vander Stoep A, McCarty CA, Geyer JR, Desalvo A. Attention-deficit/hyperactivity disorder and telemental health. Curr Psychiatry Rep. (2010) 12:409–17. doi: 10.1007/s11920-010-0132-8
49. Myers K, Vander Stoep A, Zhou C, McCarty CA, Katon W. Effectiveness of a telehealth service delivery model for treating attention-deficit/hyperactivity disorder: a community-based randomized controlled trial. J Am Acad Child Adolesc Psychiatry. (2015) 54:263–74. doi: 10.1016/j.jaac.2015.01.009
50. Baer L, Cukor P, Jenike MA, Leahy L, O'Laughlen J, Coyle JT. Pilot studies of telemedicine for patients with obsessive-compulsive disorder. Am J Psychiatry. (1995) 152:1383–5. doi: 10.1176/ajp.152.9.1383
51. Hubley S, Lynch SB, Schneck C, Thomas M, Shore J. Review of key telepsychiatry outcomes. World J Psychiatry. (2016) 6:269–82. doi: 10.5498/wjp.v6.i2.269
52. Chakrabarti S. Usefulness of telepsychiatry: a critical evaluation of videoconferencing-based approaches. World J Psychiatry. (2015) 5:286–304. doi: 10.5498/wjp.v5.i3.286
53. Boudjouk PJ, Woods DW, Miltenberger RG, Long ES. Negative peer evaluation in adolescents: effects of Tic disorders and trichotillomania. Child Family Behav Ther. (2000) 22:17–28. doi: 10.1300/J019v22n01_02
54. Friedrich S, Morgan SB, Devine C. Children's attitudes and behavioral intentions toward a peer with Tourette syndrome. J Pediatr Psychol. (1996) 21:307–19. doi: 10.1093/jpepsy/21.3.307
55. Cutler D, Murphy T, Gilmour J, Heyman I. The quality of life of young people with Tourette syndrome. Child Care Health Dev. (2009) 35:496–504. doi: 10.1111/j.1365-2214.2009.00983.x
56. Pringsheim T, Okun MS, Muller-Vahl K, Martino D, Jankovic J, Cavanna AE, et al. Practice guideline recommendations summary: treatment of tics in people with Tourette syndrome and chronic tic disorders. Neurology. (2019) 92:896–906. doi: 10.1212/WNL.0000000000007466
57. Verdellen C, van de Griendt J, Hartmann A, Murphy T, ESSTS Guidelines Group. European clinical guidelines for Tourette syndrome and other tic disorders. Part III: behavioural and psychosocial interventions. Eur Child Adolesc Psychiatry. (2011) 20:197–207. doi: 10.1007/s00787-011-0167-3
58. Holtz KD, Tessman GK. Evaluation of a peer-focused intervention to increase knowledge and foster positive attitudes toward children with tourette syndrome. J Dev Phys Disabil. (2007) 19:531–42. doi: 10.1007/s10882-007-9042-z
59. Woods DW. The impact of Tic severity on the effects of peer education about tourette's syndrome. J Dev Phys Disabil. (2002) 14:51–62. doi: 10.1023/a:1013563713146
60. Woods DW, Koch M, Miltenberger RG. The effect of video-based peer education on the social acceptability of adults with Tourette's syndrome. J Dev Phys Disabil. (2003) 15:67–78. doi: 10.1023/a:1021456321200
61. Woods DW, Marcks BA. Controlled evaluation of an educational intervention used to modify peer attitudes and behavior toward persons with Tourette's Syndrome. Behav Modif. (2005) 29:900–12. doi: 10.1177/0145445505279379
62. White SW, Sukhodolsky DG, Rains AL, Foster D, McGuire JF, Scahill L. Elementary school teachers' knowledge of Tourette Syndrome, obsessive-compulsive disorder, & attention-deficit/hyperactivity disorder: effects of teacher training. J Dev Phys Disabil. (2010) 23:5–14. doi: 10.1007/s10882-010-9209-x
63. Koonce DA, Cruce MK, Aldridge JO, Langford CA, Sporer AK, Stinnett TA. The ADHD label, analogue methodology, and participants' geographic location on judgments of social and attentional skills. Psychol Sch. (2004) 41:221–34. doi: 10.1002/pits.10150
64. Jones HA, Chronis-Tuscano A. Efficacy of teacher in-service training for attention-deficit/hyperactivity disorder. Psychol Sch. (2008) 45:918–29. doi: 10.1002/pits.20342
65. Jastrowski KE, Berlin KS, Sato AF, Davies WH. Disclosure of attention-deficit/hyperactivity disorder may minimize risk of social rejection. Psychiatry. (2007) 70:274–82. doi: 10.1521/psyc.2007.70.3.274
66. Cornett-Ruiz S, Hendricks B. Effects of labeling and ADHD behaviors on peer and teacher judgments. J Educ Res. (1993) 86:349–55. doi: 10.1080/00220671.1993.9941228
67. Barbaresi WJ, Olsen RD. An ADHD educational intervention for elementary schoolteachers: a pilot study. J Dev Behav Pediatr. (1998) 19:94–100. doi: 10.1097/00004703-199804000-00006
68. Syed EU, Hussein SA. Increase in teachers' knowledge about ADHD after a week-long training program: a pilot study. J Atten Disord. (2010) 13:420–3. doi: 10.1177/1087054708329972
69. Corkum P, Rimer P, Schachar R. Parental knowledge of attention-deficit hyperactivity disorder and opinions of treatment options: impact on enrollment and adherence to a 12-month treatment trial. Can J Psychiatry. (1999) 44:1043–8. doi: 10.1177/070674379904401011
70. Svanborg P, Thernlund G, Gustafsson PA, Hagglof B, Schacht A, Kadesjo B. Atomoxetine improves patient and family coping in attention deficit/hyperactivity disorder: a randomized, double-blind, placebo-controlled study in Swedish children and adolescents. Eur Child Adolesc Psychiatry. (2009) 18:725–35. doi: 10.1007/s00787-009-0031-x
71. Donker T, Griffiths KM, Cuijpers P, Christensen H. Psychoeducation for depression, anxiety and psychological distress: a meta-analysis. BMC Med. (2009) 7:79. doi: 10.1186/1741-7015-7-79
72. Zareei Mahmoodabadi H, Sardadvar N, Nasirian M. Effectiveness of psycho-educational intervention in improving symptoms of patients with obsessive-compulsive disorder and general family functioning of companions. Iran Red Crescent Med J. (2018) 20:e58377. doi: 10.5812/ircmj.58377
73. Law GU, Sinclair S, Fraser N. Children's attitudes and behavioural intentions towards a peer with symptoms of ADHD: does the addition of a diagnostic label make a difference? J Child Health Care. (2007) 11:98–111. doi: 10.1177/1367493507076061
74. Nussey C, Pistrang N, Murphy T. How does psychoeducation help? A review of the effects of providing information about Tourette syndrome and attention-deficit/hyperactivity disorder. Child Care Health Dev. (2013) 39:617–27. doi: 10.1111/cch.12039
75. Niles BL, Klunk-Gillis J, Ryngala DJ, Silberbogen AK, Paysnick A, Wolf EJ. Comparing mindfulness and psychoeducation treatments for combat-related PTSD using a telehealth approach. Psychol Trauma Theory Res Practi Policy. (2012) 4:538–47. doi: 10.1037/a0026161
76. Oliver DP, Demiris G. Comparing face-to-face and telehealth-mediated delivery of a psychoeducational intervention: a case comparison study in hospice. Telemed J E Health. (2010) 16:751–3. doi: 10.1089/tmj.2010.0013
77. Lounsberry JJ, Macrae H, Angen M, Hoeber M, Carlson LE. Feasibility study of a telehealth delivered, psychoeducational support group for allogeneic hematopoietic stem cell transplant patients. Psychooncology. (2010) 19:777–81. doi: 10.1002/pon.1617
78. Ruskin PE, Silver-Aylaian M, Kling MA, Reed SA, Bradham DD, Hebel JR, et al. Treatment outcomes in depression: comparison of remote treatment through telepsychiatry to in-person treatment. Am J Psychiatry. (2004) 161:1471–6. doi: 10.1176/appi.ajp.161.8.1471
79. Garcia-Lizana F, Munoz-Mayorga I. Telemedicine for depression: a systematic review. Perspect Psychiatr Care. (2010) 46:119–26. doi: 10.1111/j.1744-6163.2010.00247.x
80. Cubo E, Doumbe J, Njiengwe E, Onana P, Garona R, Alcalde J, et al. A Parkinson's disease tele-education program for health care providers in Cameroon. J Neurol Sci. (2015) 357:285–7. doi: 10.1016/j.jns.2015.07.019
81. Scahill L, Erenberg G, Berlin CM Jr, Budman C, Coffey BJ, Jankovic J, et al. Contemporary assessment and pharmacotherapy of Tourette syndrome. NeuroRx. (2006) 3:192–206. doi: 10.1016/j.nurx.2006.01.009
82. McGuire JF, Ricketts EJ, Piacentini J, Murphy TK, Storch EA, Lewin AB. Behavior therapy for Tic disorders: an evidenced-based review and new directions for treatment research. Curr Dev Disord Rep. (2015) 2:309–17. doi: 10.1007/s40474-015-0063-5
83. McGuire JF, Piacentini J, Brennan EA, Lewin AB, Murphy TK, Small BJ, et al. A meta-analysis of behavior therapy for Tourette Syndrome. J Psychiatr Res. (2014) 50:106–12. doi: 10.1016/j.jpsychires.2013.12.009
84. Piacentini J, Woods DW, Scahill L, Wilhelm S, Peterson AL, Chang S, et al. Behavior therapy for children with Tourette disorder: a randomized controlled trial. JAMA. (2010) 303:1929–37. doi: 10.1001/jama.2010.607
85. Wilhelm S, Peterson AL, Piacentini J, Woods DW, Deckersbach T, Sukhodolsky DG, et al. Randomized trial of behavior therapy for adults with Tourette syndrome. Arch Gen Psychiatry. (2012) 69:795–803. doi: 10.1001/archgenpsychiatry.2011.1528
86. Ben-Pazi H, Browne P, Chan P, Cubo E, Guttman M, Hassan A, et al. The promise of telemedicine for movement disorders: an interdisciplinary Approach. Curr Neurol Neurosci Rep. (2018) 18:26. doi: 10.1007/s11910-018-0834-6
87. Conelea CA, Wellen BCM. Tic treatment goes tech: a review of TicHelper.com. Cogn Behav Pract. (2017) 24:374–81. doi: 10.1016/j.cbpra.2017.01.003
88. Ricketts EJ, Goetz AR, Capriotti MR, Bauer CC, Brei NG, Himle MB, et al. A randomized waitlist-controlled pilot trial of voice over Internet protocol-delivered behavior therapy for youth with chronic tic disorders. J Telemed Telecare. (2016) 22:153–62. doi: 10.1177/1357633X15593192
89. Andren P, Aspvall K, Fernandez de la Cruz L, Wiktor P, Romano S, Andersson E, et al. Therapist-guided and parent-guided internet-delivered behaviour therapy for paediatric Tourette's disorder: a pilot randomised controlled trial with long-term follow-up. BMJ Open. (2019) 9:e024685. doi: 10.1136/bmjopen-2018-024685
90. Jakubovski E, Reichert C, Karch A, Buddensiek N, Breuer D, Muller-Vahl K. The ONLINE-TICS study protocol: a randomized observer-blind clinical trial to demonstrate the efficacy and safety of internet-delivered behavioral treatment for adults with chronic Tic disorders. Front Psychiatry. (2016) 7:119. doi: 10.3389/fpsyt.2016.00119
91. Himle MB, Olufs E, Himle J, Tucker BTP, Woods DW. Behavior therapy for tics via videoconference delivery: an initial pilot test in children. Cogn Behav Pract. (2010) 17:329–37. doi: 10.1016/j.cbpra.2010.02.006
92. Yellowlees P, Shore J, Roberts L, American Telemedicine Association. Practice guidelines for videoconferencing-based telemental health - October 2009. Telemed J E Health. (2010) 16:1074–89. doi: 10.1089/tmj.2010.0148
93. Rockhill CM, Tse YJ, Fesinmeyer MD, Garcia J, Myers K. Telepsychiatrists' medication treatment strategies in the children's attention-deficit/hyperactivity disorder telemental health treatment study. J Child Adolesc Psychopharmacol. (2016) 26:662–71. doi: 10.1089/cap.2015.0017
94. Pliszka SR, Crismon ML, Hughes CW, Corners CK, Emslie GJ, Jensen PS, et al. The Texas Children's Medication Algorithm Project: revision of the algorithm for pharmacotherapy of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. (2006) 45:642–57. doi: 10.1097/01.chi.0000215326.51175.eb
95. Fortney JC, Pyne JM, Edlund MJ, Williams DK, Robinson DE, Mittal D, et al. A randomized trial of telemedicine-based collaborative care for depression. J Gen Intern Med. (2007) 22:1086–93. doi: 10.1007/s11606-007-0201-9
96. Moreno FA, Chong J, Dumbauld J, Humke M, Byreddy S. Use of standard Webcam and Internet equipment for telepsychiatry treatment of depression among underserved Hispanics. Psychiatr Serv. (2012) 63:1213–7. doi: 10.1176/appi.ps.201100274
97. Fortney JC, Pyne JM, Mouden SB, Mittal D, Hudson TJ, Schroeder GW, et al. Practice-based versus telemedicine-based collaborative care for depression in rural federally qualified health centers: a pragmatic randomized comparative effectiveness trial. Focus (Am Psychiatr Publ). (2017) 15:361–72. doi: 10.1176/appi.focus.15306
98. Fortney JC, Pyne JM, Kimbrell TA, Hudson TJ, Robinson DE, Schneider R, et al. Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. (2015) 72:58–67. doi: 10.1001/jamapsychiatry.2014.1575
99. De Las Cuevas C, Arredondo MT, Cabrera MF, Sulzenbacher H, Meise U. Randomized clinical trial of telepsychiatry through videoconference versus face-to-face conventional psychiatric treatment. Telemed J E Health. (2006) 12:341–50. doi: 10.1089/tmj.2006.12.341
100. Cain S, Sharp S. Telepharmacotherapy for child and adolescent psychiatric patients. J Child Adolesc Psychopharmacol. (2016) 26:221–8. doi: 10.1089/cap.2015.0039
101. Xu W, Zhang C, Deeb W, Patel B, Wu Y, Voon V, et al. Deep brain stimulation for Tourette's syndrome. Transl Neurodegener. (2020) 9:4. doi: 10.1186/s40035-020-0183-7
102. Witek N, Heath SL, Ouyang B, Tanner CM, Galifianakis NB. Remote telemedicine evaluation of deep brain stimulation candidacy: retrospective cohort analysis. Neurol Clin Pract. (2020) 10:199–205. doi: 10.1212/CPJ.0000000000000723
103. Chen Y, Hao H, Chen H, Li L. The study on a telemedicine interaction mode for Deep Brain Stimulation postoperative follow-up. Conf Proc IEEE Eng Med Biol Soc. (2015) 2015:186–9. doi: 10.1109/EMBC.2015.7318331
104. Chen Y, Hao H, Chen H, Tian Y, Li L. The study on a real-time remote monitoring system for Parkinson's disease patients with deep brain stimulators. Conf Proc IEEE Eng Med Biol Soc. (2014) 2014:1358–61. doi: 10.1109/EMBC.2014.6943851
105. Keesara S, Jonas A, Schulman K. Covid-19 and health care's digital revolution. N Engl J Med. (2020) 382:e82. doi: 10.1056/NEJMp2005835
106. Li D, Zhang C, Gault J, Wang W, Liu J, Shao M, et al. Remotely programmed deep brain stimulation of the bilateral subthalamic nucleus for the treatment of primary Parkinson Disease: a randomized controlled trial investigating the safety and efficacy of a novel deep brain stimulation system. Stereotact Funct Neurosurg. (2017) 95:174–82. doi: 10.1159/000475765
107. Jitkritsadakul O, Rajalingam R, Toenjes C, Munhoz RP, Fasano A. Tele-health for patients with deep brain stimulation: the experience of the Ontario Telemedicine Network. Mov Disord. (2018) 33:491–2. doi: 10.1002/mds.27230
108. Silva GS, Farrell S, Shandra E, Viswanathan A, Schwamm LH. The status of telestroke in the United States: a survey of currently active stroke telemedicine programs. Stroke. (2012) 43:2078–85. doi: 10.1161/STROKEAHA.111.645861
109. LeRouge C, Garfield MJ. Crossing the telemedicine chasm: have the U.S. barriers to widespread adoption of telemedicine been significantly reduced? Int J Environ Res Public Health. (2013) 10:6472–84. doi: 10.3390/ijerph10126472
110. American Telemedicine Association. Telehealth is Health (2020). Available online at: http://www.americantelemed.org/ (accessed November 28, 2020).
111. FCC. 2016 Broadband Progress Report (2020). Available online at: https://www.fcc.gov/reportsresearch/reports/broadband-progressreports/2016-broadband-progressreport (accessed November 28, 2020).
112. Medicaid. Telemedicine (2020). https://www.medicaid.gov/medicaid/benefits/telemedicine/index.html (accessed November 28, 2020).
113. The Interstate Medical Licensure Compact. A Faster Pathway to Physician Licensure (2020). Available online at: https://www.imlcc.org/ (accessed November 28, 2020).
Keywords: Tourette syndrome, telemedicine, movement disorder, CBIT, tics
Citation: Cen S-s, Yu J, Wang Q, Deeb W, Wang K-l, Shukla AW, Malaty I, Ramirez-Zamora A, Zhang J-g, Hu W and Meng F-g (2020) Multidisciplinary Telemedicine Care for Tourette Syndrome: Minireview. Front. Neurol. 11:573576. doi: 10.3389/fneur.2020.573576
Received: 17 June 2020; Accepted: 16 November 2020;
Published: 18 December 2020.
Edited by:
Takashi Morishita, Fukuoka University, JapanReviewed by:
Davide Martino, University of Calgary, CanadaCopyright © 2020 Cen, Yu, Wang, Deeb, Wang, Shukla, Malaty, Ramirez-Zamora, Zhang, Hu and Meng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Hu, d2VpLmh1QHVmbC5lZHU=; Fan-gang Meng, bWVuZ2ZnQGNjbXUuZWR1LmNu
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.