
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Neurol. , 28 July 2020
Sec. Stroke
Volume 11 - 2020 | https://doi.org/10.3389/fneur.2020.00780
This article is part of the Research Topic Consequences of the COVID-19 Pandemic on Care for Neurological Conditions View all 77 articles
Stroke is a significant cause of admission to Singapore's acute care hospitals. Because of the current COVID-19 pandemic, there have been major changes in the stroke care system. On calling for the public ambulance, those suspected to have COVID-19 infection are taken to the National Center for Infectious Diseases. Otherwise, on arrival at the emergency room, all cases with fever or respiratory symptoms [COVID-19 suspect patients (CSPs)] are evaluated separately by staff wearing full personal protective equipment (PPE). Triage is not delayed. CSPs needing hyperacute therapies are sent to a specially prepared scanner; if not, imaging is deferred to the latter part of the day. CSPs are managed in isolation rooms, and sent to the acute stroke unit (ASU) if two consecutive COVID-19 swabs are negative. Investigation and rehabilitation are done within the room. ASU rounds are attended by essential members, communication by electronic means. Multidisciplinary team rounds have largely ceased, and discussions are via electronic platforms. Patient transfer and staff movement are minimized. All hospital staff wear face-masks, infection control is strictly enforced. Visitors are not allowed; staff make daily calls to update families. Mild stroke patients may be sent home with rehabilitation advice. Out-patient rehabilitation centers are closed. Patients return for out-patient visits only if needed; medications are sent to their home, and nurses make essential home visits. Stroke support and rehabilitation activities have started on-line. Continuing medical education activities are mainly by webinars. Stroke research has been severely hampered. Overall, evidence-based stroke care is delivered in a re-organized manner, with a clear eye on infection control.
The current COVID-19 pandemic has had a significant impact on global economic, political, social, emotional, and medical health. Stroke is a major cause of death and disability throughout the world (1), especially in Asia (2). Stroke occurs in 5.9% of COVID-19 patients, largely ischemic, but with a few hemorrhagic strokes (3, 4). Among patients with COVID-19, cerebrovascular disease is associated with increased mortality and severe COVID-19 infection (5); patients with prior stroke have a more severe COVID-19 infection (6, 7). While there is current interest in hypercoagulable states, vasculitis, and cardioembolism from cardiomyopathy as the mechanism for the stroke, others including large artery atherosclerosis, small artery disease, and other cardioembolic sources such as atrial fibrillation should not be forgotten (8, 9). There has been a noticeable drop in the number of stroke patients arriving at Emergency Rooms (10–12), or they come late (12, 13), or when they are more severe (14). This could be possibly out of fear of entering an environment where there may be COVID-19 patients (15), or due to the reduced availability of ambulances or prompt medical services due to resource diversion to managing COVID-19. All these impact on the provision of evidence-based stroke care that have been proven to reduce death, disability, and stroke recurrence (16).
Singapore is a small tropical island city-state of 5.7 million people situated in the heart of South-East Asia. Stroke is a major cause of death and disability, with an incidence of 1.8/1,000, prevalence of 3.65% among those aged above 50 years, and is among the top 10 causes of hospitalization to our acute care government-funded restructured hospitals that provide heavily subsidized care for more than 95% of acute stroke patients (17).
The number of people diagnosed with COVID-19 in Singapore has been rising (18). The Singapore government quickly established a high-level Multi-Ministry Taskforce on 22 January 2020. It comprises 10 members, all ministers, and is co-chaired by the Minister of Health and the Minister of National Development, with the Deputy Prime Minister as its Advisor. The Taskforce's roles are to direct the national whole-of-government response to the novel coronavirus outbreak; coordinate the community response to protect Singaporeans and stay vigilant against the spread of the disease; and work with the international community to respond to the outbreak. This has resulted in a seamless collaborative response, tapping on the resources of many ministries, so as to swiftly and effectively respond to the infection.
Prior to the COVID-19 pandemic, patients calling for the national ambulance service who were assessed as possibly having a stroke were transported directly to one of three thrombolysis/thrombectomy centers if they met the time windows, or, if not, to the nearest of the seven restructured hospitals or a collaborating private hospital scattered throughout the country. The few patients who arrived via their own transportation means and who met the time windows would receive thrombolysis at whichever center they arrived at, but if they needed thrombectomy, they were then transported to one of the three thrombectomy centers; a small number of thrombectomies were performed at a few private hospitals. Intravenous thrombolysis and thrombectomy services were available 24 h a day. In all hospitals, after emergent triage, patients were, where possible, neuro-imaged while still in the emergency department, before being sent to the acute stroke unit (ASU) of that hospital to be managed by a multidisciplinary stroke team. Those requiring in-patient rehabilitation were transferred to the rehabilitation department or to a nearby community hospital. On discharge, they were followed up by the specialist if necessary, or by the primary care physician. Community-based resources were available including out-patient rehabilitation, home medical and nursing and rehabilitation (19). Stroke support was provided by the Singapore National Stroke Association (SNSA), the oldest national-level support group for stroke survivors and their carers (20, 21).
There have been a few publications with details on how the stroke care has been reorganized due to the COVD-19 situation. Some are hospital-based (22, 23) some only address a specific issue e.g., thrombectomy in that hospital (24). There are no publications on stroke care re-organization at a regional or national level, to my knowledge. In Singapore's response to the COVID-19 epidemic, there were significant changes to the well-coordinated stroke care system, bolstered by lessons learnt from the 2002–2003 SARS-CoV-1 epidemic. This paper aims to present these changes, and what efforts have been made to maintain the provision of high-quality care for those with acute stroke and after discharge, as well as ancillary stroke activities at a national level. The information may be valuable to clinicians, administrators and policy makers involved in stroke care coordination beyond a single hospital, involving hospital and care networks.
At a national level, on calling for the public ambulance, patients are screened for possible COVID-19 infection or if they are at high risk of having COVID-19 (HrCP). The definition includes return from a country with high numbers of COVID-19 patients, in close contact with persons who have COVID-19 (e.g., same household as, cared for, or exposed for more than 30 min within two meters of a COVID-19 patient), or have been served a quarantine, leave of absence or stay-home order due to contact with a COVID-19 patient. These HrCP are taken directly to the National Center for Infectious Diseases (NCID) where they are assessed and isolated for further care. This policy of sending HrCP to the NCID may be reviewed if the center gets overloaded with patients. There have been no noticeable delays in emergency service response times—the public ambulance service is centrally coordinated and has adequate staff and necessary ambulances; the provision for dealing with large numbers of ambulance requests has been in place for many years, probably based on prior experiences with large disasters and tragedies causing mass casualties. All others who meet the criteria for intravenous thrombolysis or thrombectomy are still taken to the three dedicated centers; if they do not meet the criteria, they are taken to any of the restructured hospitals, as before. Ambulance staff wear full PPE at all times. Each ambulance is fully equipped with adequate stores so that this can be achieved. The staff are all trained on how to quickly don their PPE with minimal delay. Patients may still choose to use their own transportation means for getting to their preferred hospital. There is no practice change here.
At a hospital level, existing stroke pathways had to be modified in each hospital to meet the needs for strict infection control. In all hospitals, on arrival at the emergency room, all cases are screened again for possible COVID-19 infection and fever; those who are HrCPs are immediately sent to NCID—again this policy may be amended. The NCID is located next to the National Neuroscience Institute (NNI); the neurologist is able to see the stroke patient immediately. NCID has a designated CT scan negative-pressure room that is staffed 24 h a day and used only for COVID-19 patients. By protocol, all thrombectomy patients are prophylactically intubated and sent to a pre-specified operating theater which has negative pressure and a separate ventilation system. They are subsequently managed in the NCID Intensive Care Unit, and later in the NCID wards. The NNI neurologist consults on the patient on a daily basis to collaborate on stroke patient care. It is unlikely that acute stroke therapy was delayed by pre-triage to or subsequent management in NCID (25).
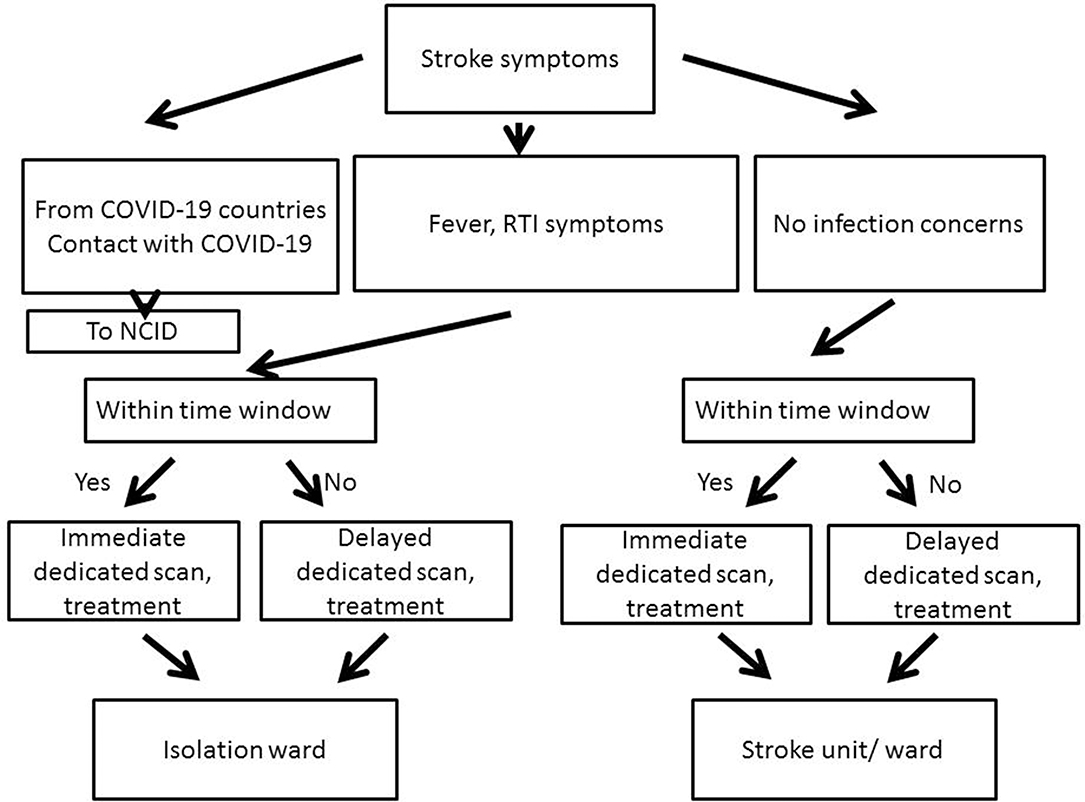
Figure 1. Workflow in the Emergency Department. All patients arriving within the time window for hyperacute therapy are sent for immediate imaging; those who arrive beyond the time window are scanned later at the next available slot, usually later that same day. This applies to both with and without infection concerns (NCID, National Center for Infectious Diseases; RTI, Respiratory Tract Infection).
Those with fever or respiratory tract infection symptoms (e.g., cough, breathlessness, sore throat, runny nose) are defined as COVID-19 suspect patients (CSPs) and are evaluated separately in an area set aside for this purpose, with staff wearing PPE, and the patient in a face mask (FM). Triage, assessment for urgent therapies, imaging are performed without delay for all CSPs and non-CSPs as per the hospital stroke protocol. CSPs needing hyperacute therapies are sent to a scan machine in a minimally equipped room prepared for them, and the scanning room is thoroughly disinfected after each patient; if not for hyperacute therapy, the imaging is delayed to the latter part of the day. The three hospitals with the dedicated thrombolysis-thrombectomy services are able to reserve a scan room just for CSPs. Telemedicine is used where possible to reduce staff members entering this area.
Intravenous thrombolysis commences in the scan room, if possible, for all patients. CSPs who need thrombectomy are prepared in a negative-pressure room if available, and aerosol-generating activities are minimized. Non-CSPs are managed in the usual manner. There is a pool of interventional radiologists and trained staff, allowing for multiple thrombectomy teams in each of the three dedicated centers, in order to cater for the eventuality that if one EVT team unfortunately encounters a confirmed COVID-19 case without adequate protection, that whole team may need to be quarantined for many days.
CSPs in all hospitals are managed in isolation rooms, usually within a ‘fever ward' or if possible within the acute stroke unit (ASU), with staff in PPE, patients in FM. CSPs are swabbed for COVID-19 daily, and only sent out to the ASU for further care if two consecutive swabs are negative—the results of each swab are ready within 24 h; if positive, the patient is transferred to the NCID. Venepunctures, x-rays, neurosonology, echocardiography, arrhythmia monitoring, and rehabilitation are done within the isolation room by dedicated technicians and staff, based on the clinical need, but may be deferred until the patient has been moved to the ASU if it's less urgent. If repeat imaging is needed, the CSP is transported wearing a FM to the specially-prepared scanner, with imaging performed in the latter part of the day whenever possible. Non-CSPs are managed as usual in the ASU, and have their investigations performed in the usual venues e.g., radiology department, neurosonology laboratory, cardiac laboratory (Table 1).
ASU daily rounds are attended only by essential members, communication is by electronic means wherever possible, as all hospitals have electronic medical records including review of imaging and laboratory test results. Multidisciplinary team rounds have largely ceased; discussions are held via electronic platforms. Patient transfer and staff movement are minimized, with ward-based teams where possible. All hospital staff wear FM, infection control is strictly enforced especially hand-washing; social distancing enforced as far as is practicable. Care pathways continue to be followed. Non-urgent surgeries have been postponed.
Visitors are not allowed, except perhaps if the patient is in intensive care (one named visitor throughout hospital stay), or if caregiver training is being provided pre-discharge. Doctors and nurses call the patient's family daily with updates, patients are allowed easy access to ward telephones, wi-fi is provided free where possible. Hospital visits by volunteer befrienders from the SNSA have been halted, but communication over the phone may continue.
Rehabilitation is provided as before, but with social distancing, with patients kept at least one meter apart in the gyms. Transfers to rehabilitation units and community hospitals may be delayed by repeat screening for COVID-19 infection; mild strokes may be sent home with rehabilitation advice.
Out-patient rehabilitation centers are closed, which may increase functional limitations and hinder recovery (26). Online rehabilitation services are being tried, but elderly patients are usually unable to manage the required steps, further challenged by their physical disabilities. Traditional Chinese Medicine services have ceased. At the patient level, patients return for out-patient visits only if needed; many are fearful. They may still visit their family physicians. Home visits by nurses are performed where necessary (e.g., to change nasogastric tubes, urine catheters and dressings). Doctors call selected patients to determine progress. Medications are sent to the patient's home for a small fee to maintain compliance. Teleconsultation is available but not actively taken up by elderly patients. Some stroke support activities by SNSA have started on-line e.g., exercises, aphasia therapy, but again disabled elderly who are not familiar with the use of online services may not participate.
All healthcare professionals are regularly recertified by their respective professional boards (e.g., Singapore Medical Council for doctors), usually by participating in continuing medical education (CME) activities (27). Professional recertification requirements have not been relaxed—full-practice doctors still need to earn at least 50 points over 2 years. But the availability of CME activities by electronic means via webinars has greatly increased; COVID-19 CMEs are popular and well-attended. Stroke research has been severely hampered as subjects are fearful to come to hospital, movements around the hospital is strictly controlled. But some researchers are taking the opportunity provided by reduced out-patient work to write their previously-shelved papers.
There have been a number of publications of stroke systems of care during the COVID-19 epidemic. Pre-hospital triage, advance notice by the ambulance to the Emergency Room, adequate training and use of PPE to reduce staff infection, adequate respiratory management en-route, care in appropriately equipped hospitals, and minimizing transfers is important (28, 29). Existing stroke pathways may need to be revised (23), including for endovascular therapy (30, 31). Rehabilitation should not be neglected (32, 33). It can be managed with stream-lined protocols, use of telemedicine/telerehabilitation, attending to COVID-19-related adverse events (such as fever and respiratory symptoms), enforcing social distancing and adequate sterilization of equipment (34, 35). While trying to provide the best of care to patients, staff safety cannot be neglected (36). A protocol specifically for the management of stroke among patients with COVID-19 may be helpful (22) and needs to be practiced (37). In effect, the entire system of care may needs to be reorganized (38). Guidelines and suggestions for stroke care have been proposed (39–44), but each center had best develop its own or tailor existing guidelines to meet and fit its needs. Consent for research, usually performed face-to-face, may be taken remotely (45), either electronically or by phone; follow-ups may need to be by phone (46). Challenges for stroke care are even greater in developing countries (47).
The COVID-19 pandemic has posed some challenges to the provision of stroke care in Singapore. There is no overall change in pre-hospital and hyperacute stroke care policies, but CSPs are cared for in isolation; stroke support services and stroke research are majorly affected. Still, evidence-based stroke care is delivered in a re-organized manner, with a clear eye on infection control. The future is likely to see the greater use of electronic communication and telemedicine.
NV wrote the paper and agrees to be accountable for the content of the work.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. (2019) 18:439–58. doi: 10.1016/S1474-4422(18)30499-X
2. Venketasubramanian N, Yoon BW, Pandian J, Navarro JC. Stroke epidemiology in south, east, and south-east Asia: a review. J Stroke. (2017) 19:286–94. doi: 10.5853/jos.2017.00234
3. Li Y, Li M, Wang M, Zhou Y, Chang J, Xian Y, et al. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Stroke Vasc Neurol. (2020). doi: 10.1136/svn-2020-000431
4. Mao L, Wang M, Chen S, He Q, Chang J, Hong C, et al. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. JAMA Neurol. (2020) 77:1–9. doi: 10.1001/jamaneurol.2020.1127
5. Pranata R, Huang I, Lim MA, Wahjoepramono PEJ, July J. Impact of cerebrovascular and cardiovascular diseases on mortality and severity of COVID-19 - systematic review, meta-analysis, and meta-regression. J Stroke Cerebrovasc Dis. (2020) 29:104949. doi: 10.1016/j.jstrokecerebrovasdis.2020.104949
6. Larson AS, Savastano L, Kadirvel R, Kallmes DF, Hassan AE, Brinjikji W. COVID-19 and the cerebro-cardiovascular systems: what do we know so far? J Am Heart Assoc. (2020) 9:e016793. doi: 10.1161/JAHA.120.016793
7. Aggarwal G, Lippi G, Michael Henry B. Cerebrovascular disease is associated with an increased disease severity in patients with Coronavirus Disease 2019 (COVID-19): a pooled analysis of published literature. Int J Stroke. (2020) 15:385–9. doi: 10.1177/1747493020921664
8. Hess DC, Eldahshan W, Rutkowski E. COVID-19-related stroke. Transl Stroke Res. (2020) 11:322–5. doi: 10.1007/s12975-020-00818-9
9. Venketasubramanian N. Hennerici MG. Stroke in coronavirus disease 2019 (COVID-19) and severe acute respiratory syndrome (SARS). Cerebrovasc Dis. (2020) 26:1–2. doi: 10.1159/000508370
10. Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center: cover title: falling stroke rates during COVID-19. J Stroke Cerebrovasc Dis. (2020) 29:104953. doi: 10.1016/j.jstrokecerebrovasdis.2020.104953
11. Morelli N, Rota E, Terracciano C, Immovilli P, Spallazzi M, Colombi D, et al. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 Era. Eur Neurol. (2020) 1–3. doi: 10.1159/000507666
12. Pop R, Quenardelle V, Hasiu A, Mihoc D, Sellal F, Dugay MH, et al. Impact of the COVID-19 outbreak on acute stroke pathways - insights from the Alsace region in France. Eur J Neurol. (2020) 11:1073–9. doi: 10.1111/ene.14316
13. Teo KC, Leung WCY, Wong YK, Liu RKC, Chan AHY, Choi OMY, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. (2020) 51:2228–31. doi: 10.1161/STROKEAHA.120.030105
14. Yaghi S, Ishida K, Torres J, Mac Grory B, Raz E, Humbert K, et al. SARS2-CoV-2 and stroke in a New York healthcare system. Stroke. (2020) 51:2002–11. doi: 10.1161/STROKEAHA.120.030335
15. Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. (2020) 51:1996–2001. doi: 10.1161/STROKEAHA.120.030225
16. Markus HS, Brainin M. COVID-19 and stroke-a global World Stroke Organization perspective. Int J Stroke. (2020) 15:361–4. doi: 10.1177/1747493020923472
17. Venketasubramanian N, Chen CL. Burden of stroke in Singapore. Int J Stroke. (2008) 3:51–4. doi: 10.1111/j.1747-4949.2008.00181.x
18. Singapore: Ministry of Health. Available online at: https://covidsitrep.moh.gov.sg/ (accessed May 24, 2020).
19. Venketasubramanian N, Chan BP, Lim E, Hafizah N, Goh KT, Lew YJ, et al. Stroke disease management–a framework for comprehensive stroke care. Ann Acad Med Singapore. (2002) 31:452–60.
20. Singapore National Stroke Association. Available online at: http://www.snsa.org.sg/ (accessed May 24, 2020).
21. Venketasubramanian N, Yin A, Lee LB, De Silva DA. Two decades of nation-wide community-based stroke support - The Singapore National Stroke Association. Int J Stroke. (2017) 12:297–301. doi: 10.1177/1747493016676620
22. Wang X, Chen Y, Li Z, Wang D, Wang Y. Providing uninterrupted care during COVID-19 pandemic: experience from Beijing Tiantan Hospital. Stroke Vasc Neurol. (2020) 5:180–4. doi: 10.1136/svn-2020-000400
23. Baracchini C, Pieroni A, Viaro F, Cianci V, Cattelan AM, Tiberio I, et al. Acute stroke management pathway during Coronavirus-19 pandemic. Neurol Sci. (2020) 41:1003–5. doi: 10.1007/s10072-020-04375-9
24. Alqahtani SA, Alnaami I, Alhazzani A. Protected stroke mechanical thrombectomy code during the coronavirus (COVID-19) pandemic: southwestern part of Saudi Arabia stroke unit local protocol. Cureus. (2020) 12:e7808. doi: 10.7759/cureus.7808
25. Christopher SYH, Carol TH, Yu-lin W. Challenges in adapting existing hyperacute protocols by a tertiary neuroscience centre for patients with COVID-19 in Singapore. Int J Cerebrovasc Dis Stroke. (2020) 3:125. doi: 10.29011/2688-8734.000025
26. Boldrini P, Garcea M, Brichetto G, Reale N, Tonolo S, Falabella V, et al. Living with a disability during the pandemic. “Instant paper from the field” on rehabilitation answers to the COVID-19 emergency. Eur J Phys Rehabil Med. (2020). doi: 10.23736/S1973-9087.20.06373-X. [Epub ahead of print].
27. Singapore Medical Council. Available online at: https://www.healthprofessionals.gov.sg/smc/continuing-medical-education-(cme)-for-doctors (accessed May 24, 2020).
28. Goyal M, Ospel JM, Southerland AM, Wira C, Amin-Hanjani S, Fraser JF, et al. AHA/ASAstroke council science subcommittees: emergency neurovascular Care(ENCC), the Telestroke and the Neurovascular Intervention Committees. Prehospital triage of acute stroke patients during the COVID-19 pandemic. Stroke. (2020) 51:2263–7. doi: 10.1161/STROKEAHA.120.030340
29. Khosravani H, Rajendram P, Notario L, Chapman MG, Menon BK. Protected code stroke: hyperacute stroke management during the coronavirus disease 2019 (COVID-19) pandemic. Stroke. (2020) 51:1891–5. doi: 10.1161/STROKEAHA.120.030243
30. Smith MS, Bonomo J, Knight WA 4th, Prestigiacomo CJ, Richards CT, Ramser E, et al. Endovascular therapy for patients with acute ischemic stroke during the COVID-19 pandemic: a proposed algorithm. Stroke. (2020) 51:1902–9. doi: 10.1161/STROKEAHA.120.029863
31. Nguyen TN, Abdalkader M, Jovin TG, Nogueira RG, Jadhav AP, Haussen DC, et al. Mechanical thrombectomy in the Era of the COVID-19 pandemic: emergency preparedness for neuroscience teams: a guidance statement from the society of vascular and interventional neurology. Stroke. (2020) 51:1896–901. doi: 10.1161/STROKEAHA.120.030629
32. Leocani L, Diserens K, Moccia M, Caltagirone C. Disability through COVID-19 pandemic: neurorehabilitation cannot wait. Eur J Neurol. (2020). doi: 10.1111/ene.14320. [Epub ahead of print].
33. Carda S, Invernizzi M, Bavikatte G, Bensmaïl D, Bianchi F, Deltombe T, et al. COVID-19 pandemic. What should PRM specialists do? A clinician's perspective. Eur J Phys Rehabil Med. (2020). doi: 10.23736/S1973-9087.20.06317-0. [Epub ahead of print].
34. Bikson M, Hanlon CA, Woods AJ, Gillick BT, Charvet L, Lamm C, et al. Guidelines for TMS/tES clinical services and research through the COVID-19 pandemic. Brain Stimul. (2020) 13:1124–49. doi: 10.31234/osf.io/82bmu
35. Chang MC, Boudier-Revéret M. Usefulness of telerehabilitation for stroke patients during the COVID-19 pandemic. Am J Phys Med Rehabil. (2020) 99:582. doi: 10.1097/PHM.0000000000001468
36. Leira EC, Russman AN, Biller J, Brown DL, Bushnell CD, Caso V, et al. Preserving stroke care during the COVID-19 pandemic: potential issues and solutions. Neurology. (2020). doi: 10.1212/WNL.0000000000009713
37. Kurz MW, Ospel JM, Daehli Kurz K, Goyal M. Improving stroke care in times of the COVID-19 pandemic through simulation: practice your protocols! Stroke. (2020) 51:2273–5. doi: 10.1161/STROKEAHA.120.030091
38. Sheth SA, Wu TC, Sharrief A, Ankrom C, Grotta JC, Fisher M, et al. Early Lessons from world war COVID: reinventing our stroke systems of care. Stroke. (2020) 51:2268–72. doi: 10.1161/STROKEAHA.120.030154
39. Rodríguez-Pardo J, Fuentes B, Alonso de Leciñana M, Campollo J, Calleja Castaño P, Carneado Ruiz J, et al. en nombre del Grupo Multidisciplinar del Plan Ictus Madrid. Acute stroke care during the COVID-19 pandemic. Ictus Madrid Program recommendations. Neurologia. (2020) 35:258–63. doi: 10.1016/j.nrleng.2020.04.007
40. Qureshi AI, Abd-Allah F, Alsenani F, Aytac E, Borhani-Haghighi A, Ciccone A, et al. Management of acute ischemic stroke in patients with COVID-19 infection: report of an international panel. Int J Stroke. (2020). doi: 10.1177/1747493020923234. [Epub ahead of print].
41. AHA/ASA Stroke Council Leadership. Temporary emergency guidance to us stroke centers during the coronavirus disease 2019 (COVID-19) pandemic: on behalf of the American Heart Association/American Stroke Association Stroke Council Leadership. Stroke. (2020) 51:1910–2. doi: 10.1161/STROKEAHA.120.030023
42. Dafer RM, Osteraas ND, Biller J. Acute stroke care in the coronavirus disease 2019 pandemic. J Stroke Cerebrovasc Dis. (2020) 29:10488. doi: 10.1016/j.jstrokecerebrovasdis.2020.104881
43. Zhao J, Rudd A, Liu R. Challenges and potential solutions of stroke care during the coronavirus disease 2019 (COVID-19) outbreak. Stroke. (2020) 51:1356–7. doi: 10.1161/STROKEAHA.120.029701
44. Bhatia R, Sylaja PN, Srivastava MVP, Khurana D, Pandian JD, Suri V, et al. Consensus statement - suggested recommendations for acute stroke management during the COVID-19 pandemic: expert group on behalf of the Indian Stroke Association. Ann Indian Acad Neurol. (2020) 23(Suppl 1):S15–S23. doi: 10.4103/aian.AIAN_302_20
45. Rai AT, Frei D. A rationale and framework for seeking remote electronic or phone consent approval in endovascular stroke trials - special relevance in the COVID-19 environment and beyond. J Neurointerv Surg. (2020) 12:654–7. doi: 10.1136/neurintsurg-2020-016221
46. Meschia JF, Barrett KM, Brown RD Jr, Turan TN, Howard VJ, Voeks JH, et al. The CREST-2 experience with the evolving challenges of COVID-19: a clinical trial in a pandemic. Neurology. (2020) 95:29–36. doi: 10.1212/WNL.0000000000009698
Keywords: stroke, services, COVID-19, Singapore, stroke unit
Citation: Venketasubramanian N (2020) Stroke Care Services in Singapore During COVID-19 Pandemic—A National Perspective. Front. Neurol. 11:780. doi: 10.3389/fneur.2020.00780
Received: 24 May 2020; Accepted: 25 June 2020;
Published: 28 July 2020.
Edited by:
Cheng-Yang Hsieh, Sin-Lau Christian Hospital, TaiwanReviewed by:
Po-Yu Lin, National Cheng Kung University Hospital, TaiwanCopyright © 2020 Venketasubramanian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Narayanaswamy Venketasubramanian, ZHJudnJhbWFuaUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.