- 1IRCCS Istituto delle Scienze Neurologiche di Bologna, Bologna, Italy
- 2Department of Biomedical and Neuromotor Sciences, Alma Mater Studiorum—University of Bologna, Bologna, Italy
- 3Neuroradiology Department, IRCCS Istituto delle Scienze Neurologiche di Bologna, Bologna, Italy
Background: Transverse sinus stenosis is a common brain MRI finding in chronic migraine (CM) and chronic tension-type headache (CTTH) patients in clinical practice; however, its clinical and diagnostic role is unclear. The aim of the study is to determine the frequency of transverse sinus stenosis in these headache patients resistant to preventive treatments and to verify whether this is a useful finding for identifying patients with intracranial hypertension.
Methods: This is an observational study. Patients with refractory CM and CTTH underwent a 3T-magnetic resonance venography (MRV) before cerebrospinal fluid (CSF) opening pressure measurement. Transverse sinus stenosis was determined using the combined conduit score. Patients with opening pressure >200 repeated MRV study 1 month after CSF withdrawal to evaluate changes in neuroimaging findings.
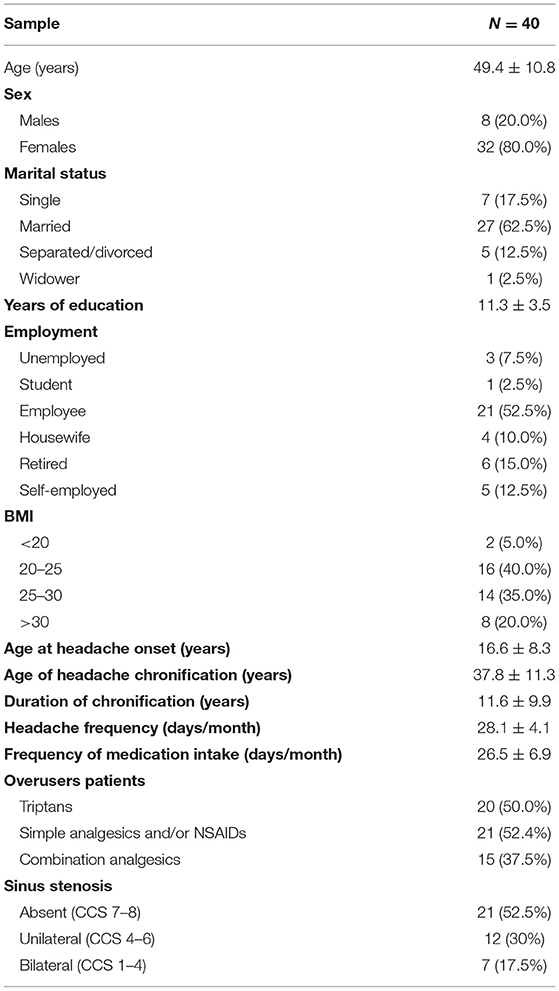
Results: We analyzed MRV studies of 40 patients (32 F, 8 M; mean age, 49.4 ± 10.8; mean body mass index, 26.7 ± 6.4; 39 CM and 1 CTTH with concomitant episodic migraine). Nineteen cases (47.5%) had evidence of transverse sinus stenosis: bilateral in seven patients (17.5%) and unilateral in 12 cases (30%). No statistically significant differences in transverse sinus stenosis distribution were found between patients with opening pressure <200 mmH2O and those with opening pressure >200 mmH2O. On Spearman bivariate test, there was no correlation between opening pressure and combined conduit score. No changes in neuroimaging findings were found 1 month after CSF withdrawal.
Conclusion: Transverse sinus stenosis is a frequent radiological finding (47.5%) in CM and CTTH patients refractory to preventive treatments. However, this finding is not suggestive of intracranial hypertension. Whether transverse sinus stenosis may be a possible risk factor for chronic headache or a comorbidity needs to be evaluated in larger epidemiological studies.
Introduction
Transverse sinus stenosis is a common brain MRI finding in chronic migraine and chronic tension-type headache patients in clinical practice, although a few studies evaluated it systematically (1–4). Previously reported transverse sinus stenosis prevalence ranges from 9% in a series of chronic tension-type patients to 92.8% in 44 refractory chronic migraine patients (1, 3). The importance of investigating the presence of transverse sinus stenosis in these patients, especially when refractory to medical treatments, arises from the need to rule out a condition of idiopathic intracranial hypertension without papilledema (IIHWOP). Headache attributed to IIHWOP may mimic chronic migraine or chronic tension-type headache, and the discrimination can be clinically difficult (5, 6). The diagnosis of IIHWOP can be suggested not only by elevated cerebrospinal fluid (CSF) opening pressure but also by the presence of at least three of the following neuroimaging findings: empty sella, distention of the perioptic subarachnoid space with or without a tortuous optic nerve, flattening of the posterior sclerae, and transverse venous sinus stenosis (Table 1) (7). Among these radiological features, transverse sinus stenosis is accepted as the most sensitive hallmark of the diagnosis, having a sensitivity of 84.4% [95% confidence interval (95% CI), 65.9–93.9%] and a specificity of 94.9% (95% CI, 91.7–96.9%) (8). Although, a possible bidirectional correlation between transverse venous sinus stenosis and IIHWOP has been previously reported (9), the role of transverse sinus stenosis in headache patients is still controversial. Moreover, transverse sinus stenosis may also be found in about one-third of the general population (10, 11). Indeed, 31% of 100 people with normal MR imaging findings had magnetic resonance venography (MRV) evidence of a transverse flow gap (10). More recently, using CT angiography, the prevalence of transverse sinus stenosis was 38% in 355 consecutive “healthy” subjects (11).
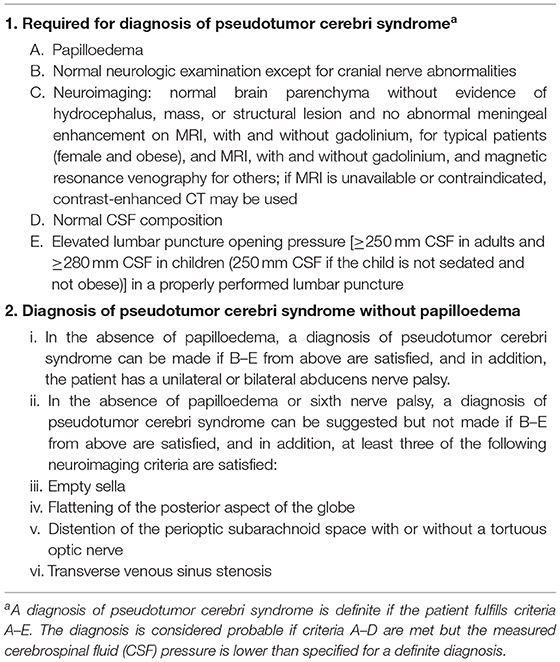
Table 1. Diagnostic criteria for pseudotumor cerebri syndrome (7).
The aim of this study was to clarify the clinical frequency and diagnostic role of sinus stenosis on MRV to identify patients with intracranial hypertension among chronic migraine and chronic tension-type headache patients resistant to prophylactic therapies.
Materials and Methods
Outcome Measures
The primary endpoint of the study was to analyze the frequency of transverse sinus stenosis in a series of consecutive refractory chronic headache (chronic migraine and chronic tension-type headache) patients.
The secondary endpoint was to evaluate the correlation between transverse sinus stenosis and CSF opening pressure to identify patients with intracranial hypertension and to evaluate changes in transverse sinus stenosis after CSF withdrawal.
Standard Protocol Approvals and Patient Consents
This prospective study was conducted in agreement with principles of good clinical practice, and the study protocol was approved by the Local Ethics Committee of the local health service of Bologna, Italy (no. 12017/CE). All patients gave their written informed consent to study participation.
Participants
Forty patients with refractory chronic headache (chronic migraine and chronic tension-type headache) prospectively underwent MRV at the tertiary Headache Center of IRCCS Institute of Neurological Sciences of Bologna, Italy, from September 2013 to February 2016, as part of a previous study (12). Diagnosis of the type of headache was established according to the International Classification of Headache Disorders-3 beta version criteria and also confirmed according the new International Classification of Headache Disorders-3 version criteria (13, 14). Refractoriness was defined as the failure of at least three trials of preventive therapies at adequate doses and at least one detoxification attempt in case of medication overuse. Inadequate response was defined as absence of clinically meaningful improvement after at least 3 months of therapy at a stable dose considered appropriate for migraine or tension-type prevention according to accepted guidelines (15, 16). As previously reported, detailed information about the clinical features of headache and associated symptoms potential-related comorbidities and concomitant medications were collected by face-to-face structured interviews (12).
Study Protocol
In this prospective study, each patient underwent MRV before CSF opening pressure measurement. Complete details of the lumbar puncture procedure, and results were described elsewhere in detail (12). Briefly, according to previous findings that suggest that CSF withdrawal may result in a sustained remission of chronic migraine, we performed CSF withdrawal in patients with opening pressure values above 200 mmH2O: intracranial pressure measurements were repeated every 2 ml of extracted CSF, up to ~100 mmH2O (3, 12). We found 9 of 40 patients (22.5%) with opening pressure >200 mmH2O, two of them above 250 mmH2O (12). Each patient with opening pressure >200 repeated the MRV study 1 month after CSF withdrawal to evaluate changes in neuroimaging findings.
Subjects were examined with a 3T MR system (Signa 3T GE) with an eight-channel brain array coil. All the examinations included T1- and T2-weighted sequences and MRV studies. MRV studies were performed using two-dimensional time-of-flight sequence acquired in the coronal plane and by a three-dimensional contrast-enhanced ultrafast gradient-echo angiographic sequence with elliptic centric ordering of k-space collection (Time Resolved Imaging of Contrast Kinetics). The Time Resolved Imaging of Contrast Kinetics sequences acquisition was in the sagittal image plane, covering the whole head. Venous phase correct time delay was calculated administering a small 2-ml test bolus of gadolinium chelates followed by 10 ml bolus of normal saline (12). The angiographic sequence was then acquired after the injection of a 30-ml bolus of gadolinium chelate contrast agent at a rate of 2 ml/s followed by 30 ml saline flush at 2 ml/s (12).
Two neuroradiologists (F.T. and L.C.), who were blinded to the patient's clinical features, reviewed source images from contrast-enhanced MRV on a PACS viewing workstation. Sagittal source images and reformatted images of the volume using 1–2 mm thick section in the coronal and axial plane and three-dimensional maximum intensity projection reconstructions were reviewed. Vascular stenosis was determined using the combined conduit score (CCS) (17). The CCS is defined as the sum of the right and left scores that is the highest degree of stenosis from the torcular to the distal sigmoid sinus, rated on a 0–4 scale as follows: 0, discontinuity; 1, hypoplasia or severe stenosis estimated as <25% of the cross-sectional diameter of the lumen; 2, moderate stenosis (25–50%); 3, mild stenosis (50–75%); and 4, no significant narrowing seen (75–100%) (17). Stenosis was defined as a CCS score <3. The sum of the right and left side scores provided the CCS (17). Stenosis was also defined as bilateral, unilateral, or absent. Disagreements were resolved by consensus. The degree of sinus stenosis was correlated to clinical features including opening pressure, body mass index (BMI), and disease duration.
We evaluated effect of CSF withdrawal at 1, 3, and 6 months follow-up. Patients recorded all headache attacks and drugs treatments on a clinical diary, over the whole study period (12).
Statistics
All data were analyzed using the SPSS software package (version 21, IBM Analytics). t-test or Mann–Whitney test, as appropriate, was used to compare continuous variables, while chi-square test was adopted for categorical variables. Results were expressed by mean ± standard deviation, median with interquartile range or percentage. The Spearman bivariate test was used to detect the strength of correlation between selected variables. Values of p < 0.05 were considered statistically significant. A Bonferroni correction was applied for multiple comparisons.
Results
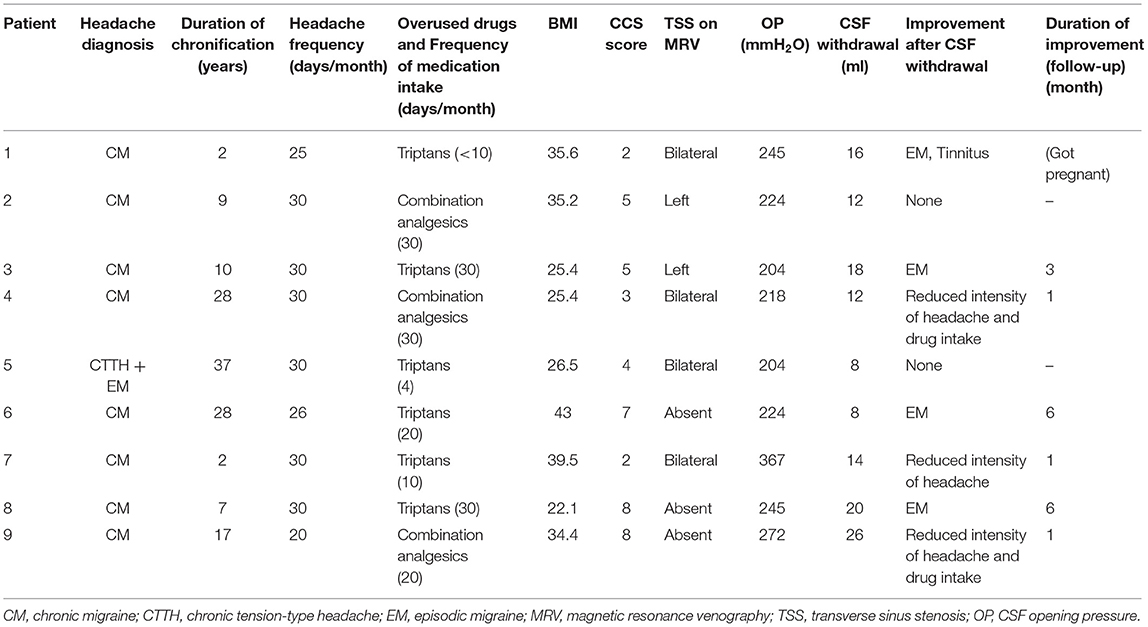
Analyses were conducted in 40 patients (32 F, 8 M; mean age, 49.4 ± 10.8; mean BMI, 26.7 ± 6.4). Thirty-nine patients had chronic migraine, and one patient had chronic tension-type headache with concomitant episodic migraine. Demographic and baseline clinical features are reported in Table 2. All patients had normal brain parenchyma. Nineteen cases (47.5%) had MRV evidence of transverse sinus stenosis: bilateral in seven patients (17.5%; CCS ranging from 1 to 4) and unilateral in 12 cases (30%, 11 on the left side, and one on the opposite) (CCS ranging from 4 to 6). The remaining 21 MRV studies (52.5%) revealed no transverse sinus stenosis (CCS, 7 or 8) (Table 2). Patients with opening pressure <200 mmH2O and those with opening pressure >200 mmH2O showed no statistically significant differences in demographic and clinical features, CCS score, and presence or not of unilateral/bilateral stenosis (Table 3). Details on the distribution of transverse sinus stenosis findings according to opening pressure are shown in Table 4. In particular, among the two patients with opening pressure >250 mmH2O, one had bilateral sinus stenosis and the other no evidence of stenosis. On Spearman bivariate test, there was no correlation between opening pressure and CCS score. There was no statistically significant difference (p = 0.616) in BMI values among groups with absent (mean, 25.85; SD, 5.90), unilateral (mean, 27.92; SD, 7.11), or bilateral (mean, 27.44; SD, 7.29) stenosis. Moreover, no association was detected between BMI and disease duration. No changes of neuroimaging findings and CCS scores were found on neuroimaging in the nine patients with opening pressure >200 mmH2O 1 month after CSF withdrawal. At the 1 month follow-up visit, seven of the nine patient reported clinical improvement after withdrawal. Effect of CSF withdrawal on headache up to 6-month follow-up is briefly reported in Table 5 and also in detail elsewhere (12).
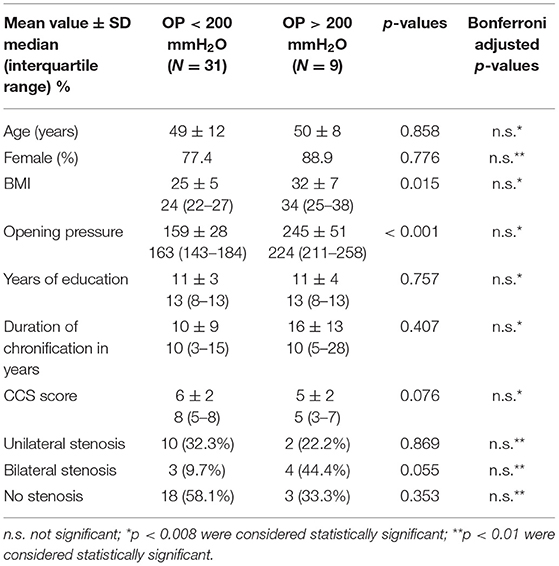
Table 3. Comparisons of features of patients with opening pressure (OP) < 200 mmH2O and patients with OP > 200 mmH2O (groups 1 and 2).
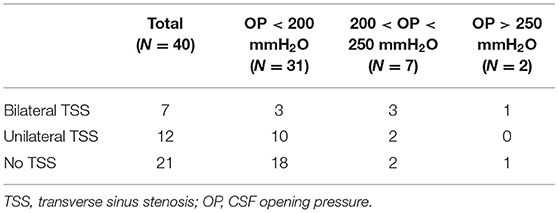
Table 4. Distribution of transverse sinus stenosis in our sample, based on opening pressure measurement.
Discussion
In our study, we found a relatively high frequency (47.5%) of transverse sinus stenosis in chronic headache (chronic migraine and chronic tension-type headache) patients refractory to preventive treatments. Previously reported transverse sinus stenosis frequency ranges from 9% in a series of 198 chronic tension-type headache patients to 92.8% in 44 unresponsive chronic migraine patients (1–4) (Table 6). Undoubtedly, our findings are significantly lower than previously described in this latter series of refractory chronic migraine patients, but similar to those found in a series of 83 unselected chronic migraine patients (50.6%) (3, 4). These heterogeneous results may in part be explained by a lack of homogeneity in the MRV technique used among studies.
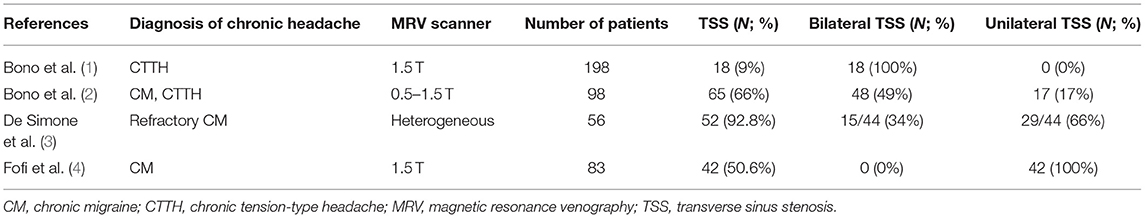
Table 6. Summary of previous studies investigating transverse sinus stenosis in chronic headache patients.
Furthermore, our results confirm that in chronic migraine and chronic tension-type headache patients, independent of opening pressure, transverse sinus stenosis may be bilateral (17.5%) or unilateral (30%). Interestingly, unilateral transverse sinus stenosis prevalence in our sample is in line with the 33% reported in the general population (11). On the contrary, our bilateral transverse sinus stenosis prevalence (17.5%) was significantly higher than the 5% found in healthy subjects (11).
Overall, our results suggest that transverse sinus stenosis is a frequent radiological feature in refractory patients, even though the role is still unknown. We speculate that this neuroimaging feature may be a risk factor for chronic migraine or a comorbidity. On the contrary, this finding alone should not be considered an isolated hallmark of intracranial hypertension in chronic migraine and chronic tension-type headache patients. In fact, we found no correlation between CCS score and CSF opening pressure. Moreover, in our series, transverse sinus stenosis persisted after CSF withdrawal, as previously reported (18). This contrast with recent evidence of the reversibility of stenosis after intracranial pressure normalization (19, 20). We may not exclude that the difference in outcome can be related to different timing of MRV after withdrawal and to the hypothesis that transverse sinus stenosis is only one of the contributing factors involved in intracranial hypertension (9, 12). A recent retrospective study supported this hypothesis, reporting that no individual radiological feature of intracranial hypertension (transverse sinus stenosis, empty sella, optic nerve sheath diameter, and flattening of the posterior sclerae) had sufficient specificity to be diagnostic for raised opening pressure. On the contrary, a combination of any three of these four MRI features was found to be nearly 100% specific and 64% sensitive for intracranial hypertension (21). Consequently, as a corollary, our findings confirm the need to combine opening pressure and neuroradiological criteria to make the diagnosis of IIHWOP.
The strength of this study is that all patients were consecutively evaluated using a 3T MR system with optimal structural details of intracranial venous system. The main limitations of the study include the relatively small sample, the lack of a control group, and the absence of CSF opening pressure measurement at follow-up. Moreover, due to feasibility reasons, patients underwent MRV only once during follow-up, set at 1 month after withdrawal as the first follow-up visit. Future epidemiological or multicenter studies with a larger number of refractory chronic migraine and chronic tension-type headache patients are needed to confirm these results.
Conclusion
Transverse sinus stenosis is a frequent radiological finding in chronic headache patients, mainly in refractory chronic migraine. Its prevalence in chronic headache sufferers is slightly higher than in the general population. However, isolated unilateral or bilateral transverse sinus stenosis finding is not suggestive of intracranial hypertension. Whether transverse sinus stenosis may be a possible risk factor for chronic headache or a comorbidity needs to be evaluated in larger epidemiological studies.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Local Ethics Committee of the local health service of Bologna, Italy (no. 12017/CE). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
VF, GP, LC, FT, CL, and SC designed the study. VF, GP, LC, FT, CL, MM, RA, and SC acquired the data. SA-R analyzed the data. All authors interpreted the data, contributed to manuscript revision, and read and approved the submitted version. VF and SC drafted the manuscript. PC revised it critically for important intellectual content.
Conflict of Interest
GP has served on advisory boards for Allergan plc and has received honoraria for speaking engagements or consulting activities with Teva and Allergan plc. CL has received speaker honoraria and travel reimbursement for meetings from Santhera Pharmaceuticals. PC has received honoraria for speaking engagements or consulting activities with Allergan Italia, AbbVie srl, Chiesi Farmaceutici, Teva, UCB Pharma S.p.A., Zambon. SC has received honoraria for speaking engagements or consulting activities with Teva, Novartis.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Miss Cecilia Baroncini who provided language assistance. The data of the present study had been presented at 17th Biennial Migraine Trust International Symposium, London, 6–9 September 2018 (22).
References
1. Bono F, Messina D, Giliberto C, Cristiano D, Broussard G, D'Asero S, et al. Bilateral transverse sinus stenosis and idiopathic intracranial hypertension without papilledema in chronic tension-type headache. J Neurol. (2008) 255:807–12. doi: 10.1007/s00415-008-0676-2
2. Bono F, Salvino D, Tallarico T, Cristiano D, Condino F, Fera F, et al. Abnormal pressure waves in headache sufferers with bilateral transverse sinus stenosis. Cephalalgia. (2010) 30:1419–25. doi: 10.1177/0333102410370877
3. De Simone R, Ranieri A, Montella S, Cappabianca P, Quarantelli M, Esposito F, et al. Intracranial pressure in unresponsive chronic migraine. J Neurol. (2014) 261:1365–73. doi: 10.1007/s00415-014-7355-2
4. Fofi L, Giugni E, Vadalà R, Vanacore N, Aurilia C, Egeo G, et al. Cerebral transverse sinus morphology as detected by MR venography in patients with chronic migraine. Headache. (2012) 52:1254–61. doi: 10.1111/j.1526-4610.2012.02154.x
5. Mathew NT, Ravishankar K, Sanin LC. Coexistence of migraine and idiopathic intracranial hypertension without papilledema. Neurology. (1996) 46:1226–30. doi: 10.1212/WNL.46.5.1226
6. Wang SJ, Silberstein SD, Patterson S, Young WB. Idiopathic intracranial hypertension without papilledema: a case-control study in a headache center. Neurology. (1998) 51:245–9. doi: 10.1212/WNL.51.1.245
7. Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. (2013) 81:1159–65. doi: 10.1212/WNL.0b013e3182a55f17
8. Kwee RM, Kwee TC. Systematic review and meta-analysis of MRI signs for diagnosis of idiopathic intracranial hypertension. Eur J Radiol. (2019) 116:106–15. doi: 10.1016/j.ejrad.2019.04.023
9. Bono F, Messina D, Giliberto C, Cristiano D, Broussard G, Fera F, et al. Bilateral transverse sinus stenosis predicts IIH without papilledema in patients with migraine. Neurology. (2006) 67:419–23. doi: 10.1212/01.wnl.0000227892.67354.85
10. Ayanzen RH, Bird CR, Keller PJ, McCully FJ, Theobald MR, Heiserman JE. Cerebral MR venography: normal anatomy and potential diagnostic pitfalls. AJNR Am J Neuroradiol. (2000) 21:74–8.
11. Durst CR, Ornan DA, Reardon MA, Mehndiratta P, Mukherjee S, Starke RM, et al. Prevalence of dural venous sinus stenosis and hypoplasia in a generalized population. J Neurointerv Surg. (2016) 8:1173–7. doi: 10.1136/neurintsurg-2015-012147
12. Favoni V, Pierangeli G, Toni F, Cirillo L, La Morgia C, Abu-Rumeileh S, et al. Idiopathic intracranial hypertension without papilledema (IIHWOP) in chronic refractory headache. Front Neurol. (2018) 9:503. doi: 10.3389/fneur.2018.00503
13. Headache Classification Committee of the International Headache Society. The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. (2013) 33:629–808. doi: 10.1177/0333102413485658
14. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. (2018) 38:1–211 doi: 10.1177/0333102417738202
15. Tfelt-Hansen PC. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. (2013) 80:869–70. doi: 10.1212/01.wnl.0000427909.23467.39
16. Martelletti P, Katsarava Z, Lampl C, Magis D, Bendtsen L, Negro A, et al. Refractory chronic migraine: a consensus statement on clinical definition from the European Headache Federation. J Headache Pain. (2014) 15:47. doi: 10.1186/1129-2377-15-47
17. Farb RI, Vanek I, Scott JN, Mikulis DJ, Willinsky RA, Tomlinson G, et al. Idiopathic intracranial hypertension: the prevalence and morphology of sinovenous stenosis. Neurology. (2003) 60:1418–24. doi: 10.1212/01.WNL.0000066683.34093.E2
18. Bono F, Giliberto C, Mastrandrea C, Cristiano D, Lavano A, Fera F, et al. Transverse sinus stenoses persist after normalization of the CSF pressure in IIH. Neurology. (2005) 65:1090–3. doi: 10.1212/01.wnl.0000178889.63571.e5
19. Rohr AC, Riedel C, Fruehauf M-C, van Baalen A, Bartsch T, Hedderich J, et al. MR imaging findings in patients with secondary intracranial hypertension. AJNR Am J Neuroradiol. (2011) 32:1021–9. doi: 10.3174/ajnr.A2463
20. Horev A, Hallevy H, Plakht Y, Shorer Z, Wirguin I, Shelef I. Changes in cerebral venous sinuses diameter after lumbar puncture in idiopathic intracranial hypertension: a prospective MRI study. J Neuroimaging. (2013) 23:375–8. doi: 10.1111/j.1552-6569.2012.00732.x
Keywords: chronic headache, refractory headache, MRI, sinus stenosis, idiopathic intracranial hypertension
Citation: Favoni V, Pierangeli G, Cirillo L, Toni F, Abu-Rumeileh S, La Morgia C, Messia M, Agati R, Cortelli P and Cevoli S (2019) Transverse Sinus Stenosis in Refractory Chronic Headache Patients: An Observational Study. Front. Neurol. 10:1287. doi: 10.3389/fneur.2019.01287
Received: 02 September 2019; Accepted: 20 November 2019;
Published: 12 December 2019.
Edited by:
Massimiliano Valeriani, Bambino Gesù Children Hospital (IRCCS), ItalyReviewed by:
Christian Lampl, Ordensklinikum Linz, AustriaFilippo Brighina, University of Palermo, Italy
Copyright © 2019 Favoni, Pierangeli, Cirillo, Toni, Abu-Rumeileh, La Morgia, Messia, Agati, Cortelli and Cevoli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Valentina Favoni, dmFsZW50aW5hLmZhdm9uaTJAdW5pYm8uaXQ=
 Valentina Favoni
Valentina Favoni Giulia Pierangeli1,2
Giulia Pierangeli1,2 Francesco Toni
Francesco Toni Samir Abu-Rumeileh
Samir Abu-Rumeileh Chiara La Morgia
Chiara La Morgia Pietro Cortelli
Pietro Cortelli Sabina Cevoli
Sabina Cevoli