
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Neurol. , 13 November 2019
Sec. Endovascular and Interventional Neurology
Volume 10 - 2019 | https://doi.org/10.3389/fneur.2019.01195
 Alicia C. Castonguay1†
Alicia C. Castonguay1† Mouhammad A. Jumaa1
Mouhammad A. Jumaa1 Osama O. Zaidat2
Osama O. Zaidat2 Diogo C. Haussen3
Diogo C. Haussen3 Ashutosh Jadhav4
Ashutosh Jadhav4 Hisham Salahuddin1
Hisham Salahuddin1 Syed F. Zaidi1*†
Syed F. Zaidi1*†Background and Purpose: The role of intra-arterial (IA) thrombolysis in modern endovascular therapy is not well-understood. Here, we surveyed neurointerventionalists to understand their current clinical practices and opinions of IA thrombolysis in the new era of mechanical thrombectomy (MT).
Method: A 24-question anonymous survey was distributed via email to the members of the Society of Vascular and Interventional Neurology.
Results: One hundred and four responses were included in the analysis. Most respondents were interventional neurologists (76.9%) and had ≥5-years in neuro-interventional practice (80.8%). IA thrombolytics are presently used by 60.6%. Aspiration plus stent-retriever was the most common MT approach used with IA-thrombolysis (66.0%). IA-thrombolysis was used in mainly three approaches: (1) treatment of primary distal occlusions, (2) as rescue after proximal occlusion thrombectomy, and (3) or as adjunct therapy to primary MT approach. The most frequent IA-rtPA dose was 3–10 mg, with 1 mg/min infusion rate (56.6%). 84.9% do not have a standardized protocol for administering IA-rtPA. About half (50.9%) believed there should be no time limit for administering IA lytic if there is a favorable imaging profile, while 30.2% indicated ≤6 h. Most respondents (76.5%) would consider using IA-tenecteplase in a trial setting. Only 12.9% felt there was no role for IA thrombolysis in modern endovascular practice. Respondents with ≥10-years' experience were less supportive of the future of IA lytic (98.0 vs. 76.4%, p = 0.006).
Conclusion: IA-thrombolysis is currently used in clinical practice; however, there is no clear consensus on best practices or criteria for administration. Further studies are needed to define the role of IA-thrombolysis in the context of MT.
Although mechanical thrombectomy (MT) has become the gold standard for the treatment of large vessels occlusions (LVOs), limited complete reperfusion rates by current generation stent-retrievers give way for adjunctive therapies to potentially augment their revascularization effectiveness. Complete or near-complete rates of reperfusion correlate with better functional outcomes in acute ischemic stroke patients (1).
Intra-arterial (IA) thrombolysis, once a first-line therapy for LVOs prior to the advent of MT, has reemerged with a potential new role in the modern endovascular era. Recent studies have demonstrated promising results of IA recombinant tissue plasminogen activator (rtPA) in the context of MT (2–4); however, the role of IA thrombolysis in contemporary endovascular therapy is not well-understood and limited data exists on its current use in real-world practice. Here, we surveyed the neuro-interventional field to evaluate the current clinical practices and opinions of IA thrombolysis in the context of MT and to better understand its future role in endovascular stroke therapy.
A 24-question survey was developed to understand current practices and opinions of physicians on the use of IA thrombolytics in endovascular stroke therapy. The survey was designed using SurveyMonkey (SurveyMonkey, Inc., San Mateo, CA, www.surveymonkey.com), an online survey development cloud-based software. This survey was classified as exempt human subject research by the University of Toledo institutional review board. As such, written informed consent was not required. The survey link was distributed to the Society of Vascular and Interventional Neurology members (SVIN) via email. All responses were anonymous, and the survey link allowed for only one completion per individual. Questions were presented in the following categories: (1) clinical and practice background, (2) IA thrombolytic use, (3) case examples, and (4) IA thrombolysis in modern endovascular practice (Table 1). Skip logic was incorporated to promote efficiency and ease of survey navigation. For analysis, all survey data were presented as frequencies of responses.
From February to May 2019, 106 responses were collected with an 80% completion rate. Of those, 104 respondents had completed at minimum questions 1 through 7 and were included in this analysis (Supplementary Table 1).
Of the 104 respondents, 80 (76.9%) were interventional neurologists, 16 (15.4%) interventional neuro-radiologists, and 8 (7.7%) were endovascular neurosurgeons (Supplementary Table 1). Most respondents had ≥5-years of neuro-interventional experience (80.8%). Almost half (49.0%) were in an academic practice, and 52.9% were in a Joint Commission certified comprehensive stroke center. On average, 42.3% performed more than 75 MTs per year. Only 23.1% had previous experience as a participating investigator in the Interventional Management of Stroke-III and/or the Prolyse in Acute Cerebral Thromboembolism II trial.
Most respondents (60.6%) used IA thrombolytics in their practice, of which 47.1% treated 1–5 cases/year with IA-rtPA (Table 1).
Of those that use IA lytics, 60.4% indicated that they used IA-rtPA in all three different approaches: (1) for treating primary distal occlusion, (2) as rescue therapy, and/or (3) adjunctive therapy (Supplementary Figure 1).
The average IA-rt-PA dosage was 3–5 mg among 35.9% and 6–10 mg among 32.1% of respondents (Table 1). 56.6% infuse IA-rtPA at a rate of 1 mg/min and 54.7% sometimes use microwire clot maceration with IA-rtPA.
In reference to where in relation to the clot should IA lytic be administered for distal M3/M4 occlusions, the majority of respondents (62.3%) would administer IA-rtPA proximal to the clot and 26.4% would administer within the clot itself (Table 1).
When questioned regarding types of MT that were used in conjunction with IA-rt-PA (irrespective of the approach), 70.0% chose a single response, of which 51.4% answered aspiration plus stent-retriever (Table 1, Supplementary Figure 2).
Most respondents (86.8%) chose a single response when asked which scenario they would not feel comfortable giving a patient IA-rtPA, with 56.5% indicating that they would feel comfortable in all scenarios (age >85 years, NIHSS >25, and IV rt-PA prior to MT) and 32.6% would not feel comfortable using IA-rtPA in patients treated with IV-rtPA (Supplementary Table 1, Supplementary Figure 3).
There was no consensus by respondents on an Alberta Stroke Program Early CT Score cut-off for use of IA-rtPA, with 20.8% answering 8–10, 17.0% 7–10, 35.9% 6–10, and 26.4% preferred no cut-off. The core infarct volume (on MR/CT perfusion) cut-off for not giving IA-rtPA varied; however, 60.4% answered either 51–70 ml (32.1%) or 71–100 ml (28.3%).
Approximately half of the respondents feel that there should be no time limit for IA lytic administration with favorable imaging, while 30.2% indicted ≤6 h.
Importantly, 84.9% did not have a standardized protocol for administering IA-rtPA.
Two case examples were provided to gauge respondents preferred treatment approaches for distal occlusions after MT (Supplementary Table 1).
For case example 1 (Figure 1), treatment preferences varied; however, the majority of respondents agreed that further treatment is necessary (78.9%).
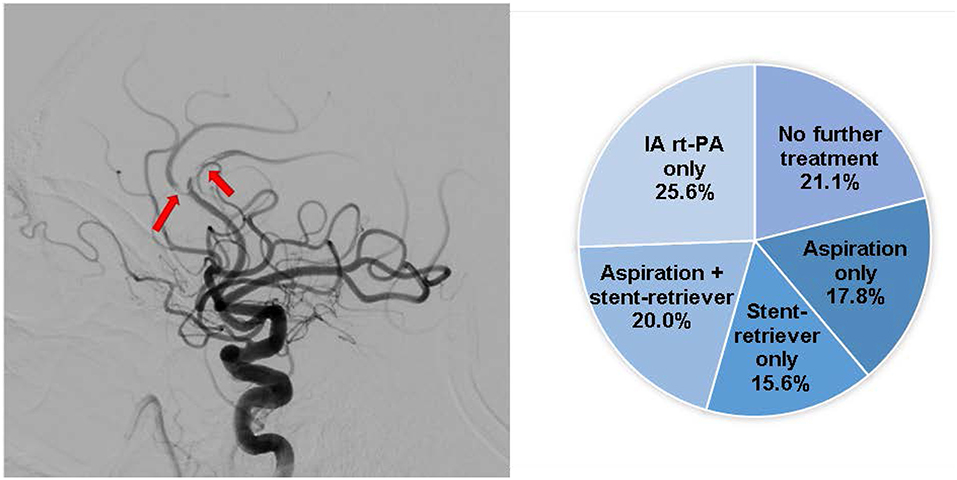
Figure 1. Case presentation #1. A 75-year-old with RICA T occlusions post-IV t-PA and MT with distal embolization into the right ACA A2. The MCA territory has completely recanalized; however, there is a subocclusive thrombus in the right pericallosal and callosmarginal divisions. Pie chart depicts the respondents' treatment preferences.
For case example 2 (Figure 2), about half of the respondents (47.1%) would recommend no further treatment and 41.4% would treat with IA-rtPA only.
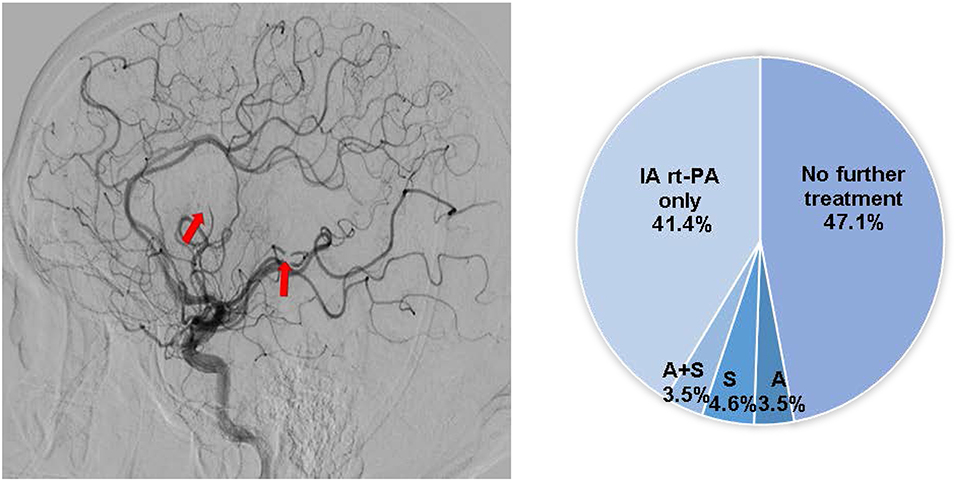
Figure 2. Case presentation #2. A 65-year-old with right sided weakness and aphasia, NIHSS 18, last known well 8 h prior to presentation, ASPECTS 9, with a left M1 occlusion on head CTA. Post left MCA MT, distal embolization occurred into multiple M3 branches. Pie chart depicts the respondents' treatment preferences. A, aspiration only; S, stent-retriever only; A+S, aspiration and stent-retriever.
When asked if respondents would consider using IA tenecteplase for treatment of distal occlusions in a trial setting, 76.5% answered yes (Supplementary Table 1).
Almost half (49.4%) of those surveyed believed that IA thrombolysis may have a role in modern endovascular practice, but more evidence is needed, while 37.6% agreed that IA thrombolysis has a role in current endovascular practice (Supplementary Table 1).
When stratifying the results by case volume or experience level, no difference was found in use of IA lytic; however, those with ≥10 years of experience were less enthusiastic about the future of IA lytic (p = 0.006) (Figure 3, Supplementary Tables 1, 2).
To date, little is known about the use of IA thrombolysis in the current era of endovascular stroke therapy. Recent studies after the landmark MT trials (5–10) have investigated IA-rtPA use in conjunction with MT (2–4); however, these studies were limited by their retrospective non-randomized nature, small sample size, and heterogeneous populations and techniques. Our study revealed that most respondents use IA thrombolysis in their current clinical practice; however, few implement standardized protocols for IA-rtPA administration.
Our survey highlights the variability of IA-rt-PA use, with most respondents using IA lytic for primary distal occlusions, or RT for distal embolization and embolization into new territory after MT, and in different settings of MT, including aspiration and stent-retrievers. When presented with two different cases of distal occlusions after MT, there was no consensus on the preferred treatment approach. As distal vessel occlusions (DVO) may cause significant deficits depending on the eloquence of the affected branch or branches (11, 12), endovascular therapies, such as IA rt-PA, may be viable treatment options for these occlusions. A recent retrospective single center case study of DVO demonstrated an acceptable safety and reperfusion profile with endovascular therapy (52% treated with IA-rtPA) (13). Although newer devices have made MT in distal vessels possible, in cases of extreme tortuosity, IA thrombolytics may be preferable.
Additionally, we also found a wide-range of IA-rtPA dosing for anterior circulation LVOs and distal occlusions; however, more than half of survey respondents administered in the range of 3–10 mg with varying infusion rates. Recent MT trials, MR CLEAN, and ESCAPE, allowed the use of IA-rtPA (9, 10). MR CLEAN allowed for a maximum of dose of 90 mg (if IV-rtPA was not administered) and 30 mg (if IV-rtPA was administered) administered via micro-catheter at the level of occlusion. The ESCAPE Trial protocol recommended a maximum dose of 10 mg rtPA via micro-catheter for use as adjunctive therapy. Two retrospective studies reported dosing of IA rt-PA of up to 15 mg and <5 mg (3, 4). As there are no standardized dosing guidelines, prospective studies are warranted to determine the dosing threshold for IA-rtPA.
Currently, there are no established criteria for IA thrombolysis administration in the context of MT and results of our survey highlight the lack of consensus among MT practitioners. Less than 50% of respondents would feel comfortable administering IA-rtPA to those >85 years, NIHSS>25, or received IV-rt-PA prior to endovascular therapy and no clear consensus was reached for a cut-off regarding Alberta Stroke Program Early CT Score or time window. The above results further demonstrate the need for clinical studies to define the criteria for use of IA thrombolysis in endovascular therapy, including the optimal patient population.
Respondents believed that IA thrombolysis may have a place in modern endovascular practice, but more evidence is required to define its role. This was supported by the respondents' enthusiasm for enrolling in future IA lytic trials, including IA tenecteplase.
Our study has several limitations, including the inherent limitations of survey research. As this survey was administered to SVIN members, results may not be inclusive of the practice patterns or opinions of other MT practitioners not affiliated with SVIN. For example, 76.9% of respondents were interventional neurologists and only 7.7% were endovascular neurosurgeons. As not all respondents answered all survey questions, it is possible that lack of response may have introduced selection bias into the survey results. Additionally, the small sample size may limit the interpretability and generalizability of this study.
Our survey demonstrates that IA thrombolysis is widely used in current practice. These results support the need for further studies on IA thrombolysis in the context of MT and may serve as a guide for the design of future IA thrombolysis clinical studies.
All datasets generated for this study are included in the article/Supplementary Material.
This survey was classified as exempt human subject research by the University of Toledo institutional review board. As such, written informed consent was not required.
AC, SZ, OZ, DH, MJ, and AJ participated in the design, analysis, drafting, and editing of the manuscript. HS participated in the analysis and critical review of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2019.01195/full#supplementary-material
1. Zaidat OO, Castonguay AC, Linfante I, Gupta R, Martin CO, Holloway WE, et al. First pass effect: a new measure for stroke thrombectomy devices. Stroke. (2018) 49:660–6. doi: 10.1161/STROKEAHA.117.020315
2. Zaidi SF, Castonguay AC, Jumaa MA, Malisch TW, Linfante I, Marden FA, et al. Intraarterial thrombolysis as rescue therapy for large vessel occlusions. Stroke. (2019) 50:1003–6. doi: 10.1161/STROKEAHA.118.024442
3. Yi TY, Chen WH, Wu YM, Zhang MF, Lin DL, Lin XH. Adjuvant intra-arterial rt-pa injection at the initially deployed solitaire stent enhances the efficacy of mechanical thrombectomy in acute ischemic stroke. J Neurol Sci. (2018) 386:69–73. doi: 10.1016/j.jns.2018.01.012
4. Heiferman DM, Li DD, Pecoraro NC, Smolenski AM, Tsimpas A, Ashley WW Jr. Intra-arterial alteplase thrombolysis during mechanical thrombectomy for acute ischemic stroke. J Stroke Cerebrovasc Dis. (2017) 26:3004–8. doi: 10.1016/j.jstrokecerebrovasdis.2017.07.031
5. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. (2016) 387:1723–1. doi: 10.1016/S0140-6736(16)00163-X
6. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-pa vs. T-pa alone in stroke. N Engl J Med. (2015) 372:2285–95. doi: 10.1056/NEJMoa1415061
7. Campbell BC, Mitchell PJ, Investigators E-I. Endovascular therapy for ischemic stroke. N Engl J Med. (2015) 372:2365–6. doi: 10.1056/NEJMoa1414792
8. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. (2015) 372:2296–306. doi: 10.1056/NEJMoa1503780
9. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. (2015) 372:1019–30. doi: 10.1056/NEJMoa1414905
10. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. (2015) 372:11–20. doi: 10.1056/NEJMoa1411587
11. Kurre W, Vorlaender K, Aguilar-Perez M, Schmid E, Bazner H, Henkes H. Frequency and relevance of anterior cerebral artery embolism caused by mechanical thrombectomy of middle cerebral artery occlusion. AJNR Am J Neuroradiol. (2013) 34:1606–11. doi: 10.3174/ajnr.A3462
12. King S, Khatri P, Carrozella J, Spilker J, Broderick J, Hill M, et al. Anterior cerebral artery emboli in combined intravenous and intra-arterial rtpa treatment of acute ischemic stroke in the IMS I and II trials. AJNR Am J Neuroradiol. (2007) 28:1890–4. doi: 10.3174/ajnr.A0702
Keywords: intra-arterial, thrombolysis, thrombectomy, stroke, occlusion
Citation: Castonguay AC, Jumaa MA, Zaidat OO, Haussen DC, Jadhav A, Salahuddin H and Zaidi SF (2019) Insights Into Intra-arterial Thrombolysis in the Modern Era of Mechanical Thrombectomy. Front. Neurol. 10:1195. doi: 10.3389/fneur.2019.01195
Received: 16 August 2019; Accepted: 28 October 2019;
Published: 13 November 2019.
Edited by:
Shakir Husain Hakim, University Hospital Zürich, SwitzerlandReviewed by:
Sombat Muengtaweepongsa, Thammasat University, ThailandCopyright © 2019 Castonguay, Jumaa, Zaidat, Haussen, Jadhav, Salahuddin and Zaidi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Syed F. Zaidi, c3llZC56YWlkaTJAdXRvbGVkby5lZHU=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.