
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 15 November 2019
Sec. Movement Disorders
Volume 10 - 2019 | https://doi.org/10.3389/fneur.2019.01194
 Hongyan Huang1†
Hongyan Huang1† Xinglong Yang2†
Xinglong Yang2† Quanzhen Zhao1
Quanzhen Zhao1 Yalan Chen1
Yalan Chen1 Pingping Ning1
Pingping Ning1 Qiuyan Shen1
Qiuyan Shen1 Hui Wang1
Hui Wang1 Ran An1
Ran An1 Yanming Xu1*
Yanming Xu1*Background: Essential tremor (ET) is one of the most common movement disorders, and it has been associated with anxiety and depression, but risk factors for these mental symptoms are unclear. This study aimed to evaluate the prevalence and potential risk factors of depression and anxiety in ET patients in China.
Methods: This cross-sectional study involved 245 Han Chinese patients with ET. Depression was assessed using the Hamilton Depression Rating Scale-24 Items, and anxiety was assessed using the Hamilton Anxiety Rating Scale. Clinico-demographic characteristics were compared between patients with or without depression or anxiety.
Results: We revealed that 63.3% of patients had at least mild anxiety and 54.3% had at least mild depression. Severity of anxiety or depression was correlated with lower Mini-Mental State Exam score (P = 0.028 and P = 0.002, respectively), higher self-report functional disability score (P = 0.027 and P = 0.003, respectively), as well as the presence of tremor in the neck (both P < 0.001), face (P = 0.025 and P < 0.001, respectively), or voice (both P < 0.001). Binary logistic regression identified female sex, presence with cranial tremor, and greater functional disability score as risk factors of anxiety; the last two factors were also the determinants of depression. Neither anxiety nor depression correlated with physician-assessed severity of arm or leg tremor.
Conclusion: Chinese ET patients show high prevalence of depression and anxiety. ET patients should be screened for these mental symptoms, especially women and those with cranial tremor and self-reported functional disability.
Essential tremor (ET) is one of the most common movement disorders, with a prevalence of 4–39 cases per 1,000 worldwide (1). ET is characterized by tremor in upper limbs (including postural, simple kinetic, and intention tremor), and it can involve cranial tremor (including tremor in the neck, face, or voice tremor), as well as non-motor symptoms such as cognitive and mental impairment (2).
ET has been linked to anxiety and depression, with prevalence of these symptoms higher among ET patients than controls (2). In fact, the prevalence of moderate to severe depressive or anxiety symptoms among ET patients can range, respectively, from 5.4 to 48.4% and from 14 to 71.1% (2–6). Depression and anxiety can reduce quality of life (6–8) and self-reported medication compliance of ET patients (8). Depression may even contribute to ET or other important outcomes like embarrassment, rather than simply be a secondary response to tremor symptom (5, 9).
Despite the high prevalence of depression and anxiety in ET and their potential contribution to the disorder, few studies have examined risk factors for these conditions among ET patients. The few available studies have come to conflicting conclusions: some have found an association between tremor severity and depression and/or anxiety in ET, while others have not (2). These discrepancies may reflect the relatively small study populations, as well as differences in how tremor severity and mental symptoms were assessed (3–6, 10–15). ET is not a homogeneous condition: the disease may manifest with different non-motor symptoms and involve different pathological processes depending on the age at onset as well as the type and locations of tremor (16, 17). Studies aiming to clarify potential associations of mental symptoms with ET need to take these issues into account.
As a step in this direction, we undertook the present study with a relatively large sample of Chinese ET patients in order to understand the frequency of depression and anxiety symptoms, their co-occurrence, and the current state of treatment. We also aimed to identify clinico-demographic characteristics that may correlate with depression and anxiety symptoms.
In this cross-sectional study, a consecutive series of non-demented ET patients was recruited from the Department of Neurology at West China Hospital of Sichuan University (Chengdu, China) between August 2016 and April 2019. None of the patients had ever been diagnosed or treated for ET. The protocol of this study was approved by the Ethics Committee of West China Hospital of Sichuan University. Informed consent was obtained from all participants.
Patients were included if they fulfilled the criteria for probable or definite ET in the consensus statement of the Movement Disorder Society on Tremor (18) based on independent examinations by two neurologists specializing in movement disorders. Patients were excluded if they had the disease <3 years or if they had only isolated neck, face, or voice tremor. Patients were also excluded if they had (a) a medical history of severe head trauma or head surgery; (b) tremor related to other central nervous system disease, such as Parkinson's disease, multiple system atrophy, Wilson disease, or dystonia; (c) tremor related to enhanced physiological tremor, psychogenic tremor, task-specific tremor, orthostatic tremor, drug intake, or alcohol withdrawal; or (d) neuroimaging-based lesions such as infarcts or tumors. These patients were identified based on history and clinical examination.
All patients were interviewed to obtain demographic data and medical history. Demographic details included sex, age at presentation, age at tremor onset, years of education, employment, marital status, current smoking/drinking, disease duration, family history, treatment, medication history, and comorbidities.
Severity of rest, postural, and simple kinetic limb tremor was evaluated using the Fahn–Talosa–Marin Tremor Rating Scale (FTM-TRS), a well-validated tremor scoring system (19). The patient-assessed tremor score was obtained using part C of the FTM-TRS, which represents functional disability (19).
Action arm tremor included postural and simple kinetic arm tremor. The score was calculated using items 5–6 in part A of the FTM-TRS (postural and simple kinetic tremor score) as well as part B of the FTM-TRS (19). Action leg tremor including postural and simple kinetic leg tremor was evaluated using items 8–9 on part A of the FTM-TRS (postural and simple kinetic tremor score). If either leg scored at least 1 point, the patient was classified as having action leg tremor.
Rest limb tremor was assessed using items 5–6 and 8–9 on part A of the FTM-TRS (rest tremor score) (19). Rest tremor was considered presence if the score is at least 1 point in either limb.
Intention tremor was defined as tremor amplitude that increased during movement close to the target (20). Intention tremor was assessed by the finger–nose–finger test, which involved 10 repetitions per arm (20). Patients were scored as showing no intention tremor (0 point), probable intention tremor (0.5 points), definite intention tremor (1 point), and incapacitating intention tremor (2 points). Patients were classified as having intention tremor if they scored more than 0.5 points in at least one arm or 0.5 points in both arms (20).
Cranial tremor included neck, voice, and/or face tremor and the score was evaluated using the FTM-TRS (19). Tremor in each location was present if the individual scored at least 1 point at that location. Patients were classified overall as showing no cranial tremor (0), cranial tremor at one position (1), or cranial tremor at multiple positions (2).
We screened cognition impairment by using the Chinese version of Folstein Mini-Mental State Exam (MMSE) (21). The presence of depression was assessed using the Chinese version of Hamilton Depression Rating scale-24 Items (HDRS-24) (22). Scores <8 indicated no depression; 8–20, mild depression; and >20, moderate to severe depression (22, 23). Presence of anxiety was assessed using the Chinese version of Hamilton Anxiety Rating Scale (HARS) (24). Scores <7 indicated no anxiety; 7–14, mild anxiety; and >14, moderate to severe anxiety (23, 24).
Continuous data were presented as mean ± SD and median, while categorical or rank data were reported as numbers and percentages. Inter-group differences in categorical variables were assessed for significance using the chi-squared test. Inter-group differences in continuous variables or rank variables were assessed using the Kruskal–Wallis H test because the data were skewed. Post hoc comparisons were Bonferroni-corrected (P = 0.017).
Correlations between continuous variables were explored using Spearman's rho correlation coefficient. The correlation coefficient (r) value ≤0.19 was defined as a negligible correlation according to the previous report (25). Dependent variables were the absence of depression (HDRS score ≤20) or its presence (HDRS score >20), or the absence of anxiety (HARS score ≤14) or its presence (HARS score >14). We used stepwise binary logistic regression (forward likelihood ratio) to explore risk factors of depression and anxiety in ET. Considering the independent variables had co-linearity and interaction, we included sex, age at presentation, years of education, MMSE score, disease duration, cranial tremor (presence/absence), and self-reported functional disability score (on part C of the FTM-TRS) as independent variables. Correlations were represented as odds ratios (ORs) and 95% confidence intervals (CIs). Statistical analyses were performed in SPSS 23.0 (IBM, Chicago, IL, USA). All tests were two-sided, and significance was accepted at the 5% level (α = 0.05).
This study involved 245 patients (125 women, 51.0%) with a mean age at presentation of 53.31 ± 16.44 years and mean disease duration of 9.87 ± 9.74 years. All patients had postural or simple kinetic tremor, while 26 (10.6%) had rest tremor and 78 (31.8%) had intention tremor. All patients had arm tremor; 100 (40.8%), leg tremor; 85 (34.7%), neck tremor; 20 (8.2%), face tremor; and 65 (26.5%), voice tremor. Nearly half the patients (121, 49.4%) had cranial tremor, of whom 79 (32.2%) had cranial tremor at one position, 36 (14.7%) at two positions, and 6 (2.4%) at three positions (Table 1). Treatment of ET is based on the severity of tremor, tremor-related disability, and largely up to the patient's perception of the tremor impact on quality of life. Eventually, 39 (15.4%) patients were treated with β-blockers and 5 (2%) patients were treated with anticonvulsants.
A total of 93 patients (38.0%) had symptoms consistent with mild anxiety, while 62 (25.3%) had symptoms consistent with moderate to severe anxiety (Tables 2, 3). A total of 98 patients (40.0%) had symptoms consistent with mild depression, and 35 (14.3%) reported symptoms consistent with moderate to severe depression.
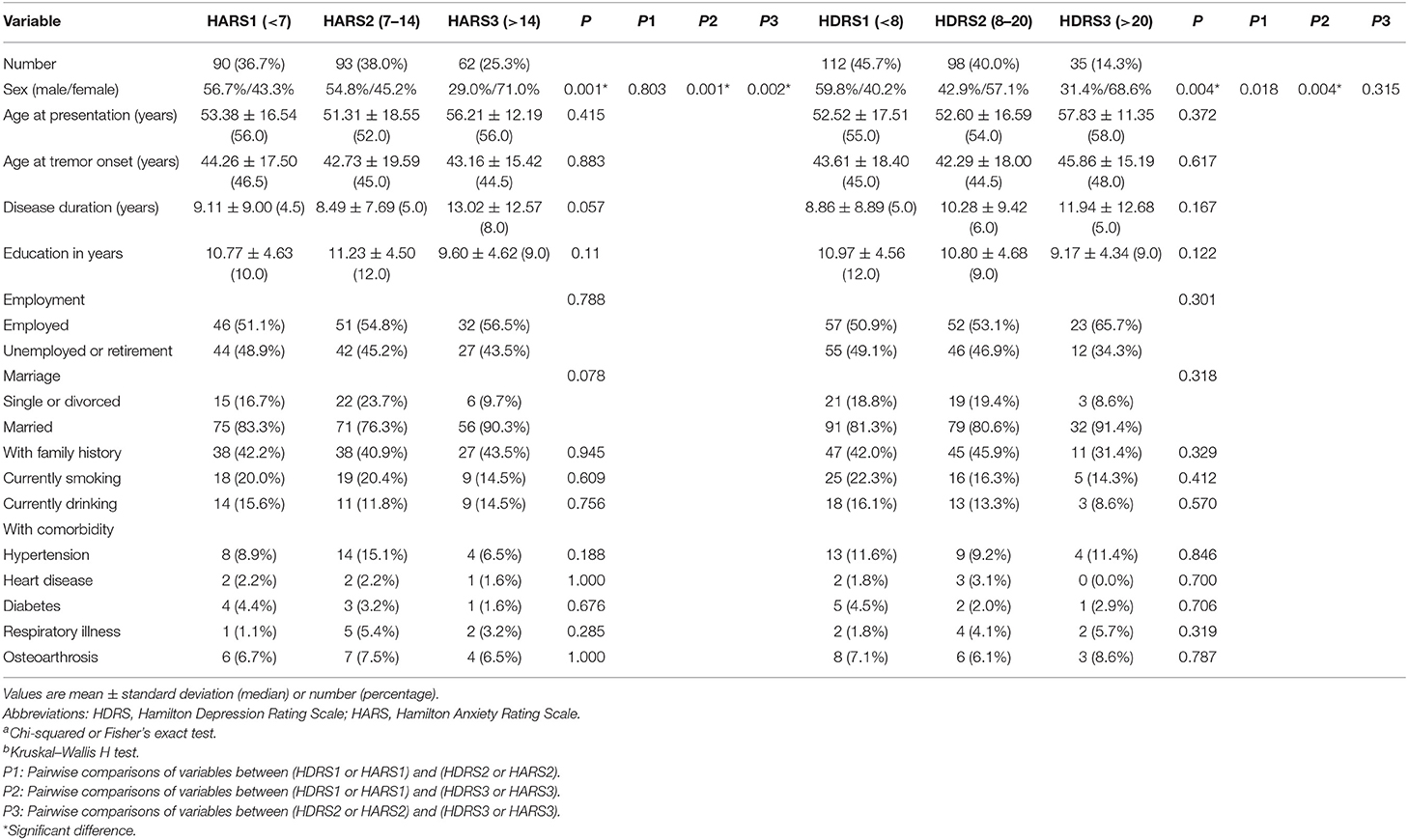
Table 2. Relationship between demographic characteristics and severity of anxiety or depression in 245 patients with essential tremor.
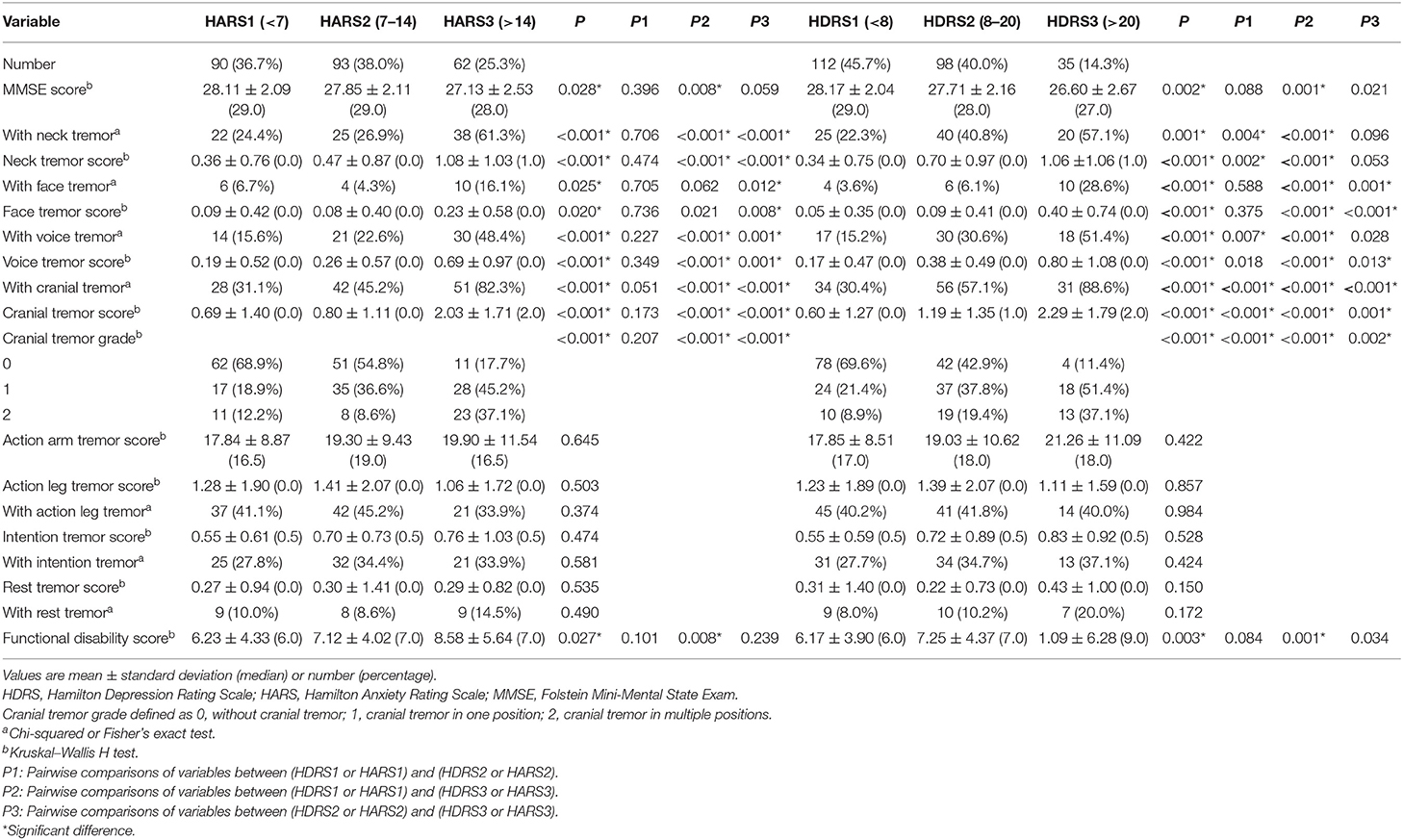
Table 3. Relationship between clinical characteristics and severity of anxiety or depression in 245 patients with essential tremor.
Univariate analysis showed that severity of anxiety and depression was significantly higher in women as well as in patients with neck, face, voice, or cranial tremor. Higher severity of anxiety and depression was associated with lower MMSE score, higher self-reported functional disability score, and neck, face, voice, or cranial tremor score (Tables 2, 3).
Correlation analysis identified the following scores as associated with HARS score: MMSE (r = −0.222, P < 0.001), self-reported functional disability (r = 0.206, P = 0.001), neck tremor (r = 0.296, P < 0.001), voice tremor (r = 0.277, P < 0.001), and cranial tremor (r = 0.390, P < 0.001). The factors were associated with HDRS score: MMSE (r = −0.272, P < 0.001), self-reported functional disability (r = 0.235, P < 0.001), neck tremor (r = 0.328, P < 0.001), face tremor (r = 0.204, P = 0.001), voice tremor (r = 0.269, P < 0.001), and cranial tremor (r = 0.415, P < 0.001). The correlation coefficient between HARS score and HDRS score was 0.855, P < 0.001. Scores for neck, face, voice, or cranial tremor did not correlate with arm or leg tremor score.
Binary logistic regression identified female sex, presence of cranial tremor, and higher self-reported functional disability score as risk factors for anxiety in ET patients (Table 4). The latter two factors were also risk factors for depression. Consistent with overlap in risk factors, we identified 30 patients who had concurrent anxiety (HARS score >14) and depression (HDRS score >20), meaning that 48.4% (30 in 62) of the patients with anxiety also had depression and 85.7% (30 in 35) of the patients with depression also had anxiety. Unfortunately, our data did not allow us to determine whether anxiety or depression symptoms occurred first and the sequence in which anxiety and depression occur with tremor.
Only five patients in our sample had a history of anti-anxiety or anti-depression therapy: one patient was taking benzodiazepines; two patients, a combination of selective serotonin reuptake inhibitors and benzodiazepines; one patient, serotonin and noradrenaline reuptake inhibitor; and one patient, tricyclic antidepressants. For patients with moderate to severe depression and/or anxiety symptoms in our initial evaluation, we recommended them to go to psychiatric outpatient clinics for further assessment, treatment, and to regular follow-up in our department and psychiatric department.
To our knowledge, this is the first large study focused on depression and anxiety in Chinese ET patients. We found that female sex, cranial tremor, and higher self-reported functional disability score may be risk factors of anxiety among these patients, while the latter two parameters may be risk factors of depression. In contrast, physical-evaluated tremor severity in limbs was not a risk factor for either depression or anxiety in these patients.
We assessed anxiety and depression in ET patients by applying the widely used and recognized scales and found that 63.3% of our ET patients had mild to severe anxiety, while 54.3% had mild to severe depression. These prevalences are within the ranges reported in studies from worldwide (2–6). These prevalence ranges are quite broad, which likely reflects differences in the studies, such as whether the sample was patient- or population-based, how large the sample was, and whether mental symptoms were assessed using DSM-IV, or screening scales. These broad ranges may also reflect clinical heterogeneity of ET syndrome and associated comorbidities. In any event, the high frequency of these disorders in ET suggests that they should be considered in ET management strategies. Fortunately, relatively few ET patients seem to suffer moderate or severe depression or anxiety in our sample and in previous studies in China (12).
Despite the high incidence of mental symptoms in ET patients, we found that very few of our patients had been diagnosed or treated for them. Untreated mental disorders correlate with lower quality of life, increased psychiatric disability, and greater use of health care resources (26). Health care workers should consider ET patients to be at elevated risk of depression and anxiety and should screen for these conditions appropriately. In particular, clinicians should be aware of the risk that both depression and anxiety are present, and treatment regimens should be rationally designed.
Cranial tremor and higher self-reported functional disability score emerged as determinants of anxiety and depression among our ET patients. The fact that we assessed all major tremor types and locations as well as the self-reported functional disability score may make our results particularly reliable. This may help clarify controversial results in the literature about associations between tremor severity and depression and/or anxiety in ET. For example, some studies found that depression or anxiety increased with action arm tremor (10, 11), while yet another study did not find that correlation (5). Some studies revealed that depression increased with total FTM-TRS score (including overall tremor and self-reported functional disability score) (12, 13). Another study found that depression, but not anxiety, correlated with FTM-TRS score without the self-reported functional disability component (4, 14).
Our study affirms the value of the self-reported functional disability score for assessing anxiety and depression in ET patients. Consistently, a small retrospective study found that functional disability score on its own was better than physician-reported tremor severity on its own at predicting anxiety and depression in ET patients following deep-brain stimulation (15). The patient-assessed tremor score may capture interaction between functional disability and emotional burden: greater self-perceived functional disability may increase risk of anxiety and depression symptoms, and at the same time, these mental symptoms may amplify subjective feelings of functional disability in daily life. Our results suggest the usefulness of screening ET patients based on functional disability score.
We found that ET patients with cranial tremor were more likely to suffer from depression and anxiety than those without such tremor, regardless of physician-assessed tremor severity at other positions. ET with cranial tremor is known to involve different motor symptom and/or pathology processes than ET without such tremor, such as manifest tandem gait disorder or vermis atrophy (16, 17). In addition to differences in motor symptoms, our study showed that ET patients with cranial tremor also showed differences in non-motor symptoms. At least three considerations support the idea that cranial tremor can increase risk of depression or anxiety in ET. One is that cranial tremor is associated with lesions in the vermis of the cerebellum (17), whereas limb tremor is associated with defects in the cerebellar hemispheres. The lobules VI–VII within the vermis are named the limbic cerebellum and participate in emotion processing, which may partly belong to the salience network and may also be connected with the amygdala and hippocampus; dysregulation in these areas can result in anxiety and depression (27). A second consideration is that balance and gait of ET patients are more severely affected in the presence of cranial tremor, which may exacerbate anxiety and fear (16, 28). A third consideration is that cranial tremor like voice tremor causes communication difficulties that reduce daily living abilities, which may contribute to anxiety and depression. Prospective studies or neuroimaging studies may be needed to further analyze the causes of the co-occurrence of these conditions in the subsequent studies.
Anxiety and depression are risk factors for dementia (29, 30), and our univariate analyses showed that lower MMSE scores were associated with more severe anxiety or depression in our patients. However, no such correlations were detected in multivariate models. These negative results may be considered preliminary because our patients were relatively young and the study did not include patients with dementia.
We found that incidence of anxiety was higher among women than men with ET. This result may reflect gender differences in genetics, psychosocial reactivity, psychosocial gender roles, and emotional expression (31). Clinicians should bear in mind the additional vulnerability of women with ET when performing psychological screening and designing treatment.
While our ET sample was relatively large and we comprehensively assessed potential risk factors of anxiety and depression, our study does have several limitations. The sensitivity of the MMSE scale is relatively lower than that of the MoCA scale, especially in the screening of mild cognitive impairment. Although Hamilton scales have good reliability and validity and are widely used in China, the ability to make a differential diagnosis between anxiety and depression is slightly inadequate. Screening instruments, rather than the DSM-5, were used to assess anxiety and depression, and the cross-sectional design prevents us from concluding any causal relationships. The number of ET cases with moderate to severe depression or anxiety symptom was relatively small and the patients came from one outpatient clinic. Despite this, our sample had adequate power to detect a sizable number of significant associations. Further prospective, longitudinal studies are required to confirm and extend our results.
Our results illustrate that depression and anxiety symptoms are common in ET. Neurologists should pay more attention to the possibility of these disorders in ET, especially among women and those with cranial tremor and greater self-report functional disability. ET is a heterogeneous syndrome. Our results re-emphasize that patients with cranial tremor may be a subtype of ET.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
This study was carried out in accordance with the recommendations of the Ethics Committee of West China Hospital of Sichuan University. The protocol was approved by the Ethics Committee of West China Hospital of Sichuan University. All subjects gave written informed consent in accordance with the Declaration of Helsinki.
(1) Research project: (A) YX, HH, and XY: conception. (B) HH, XY, QZ, YC, PN, QS, HW, and RA: execution. (2) Statistical analysis: (A) HH, XY, QZ, YC, PN, QS, HW, and RA: design and execution. (B) YX and XY: review and critique. (3) Manuscript: (A) HH: writing of the first draft. (B) YX and XY: review and critique.
This work was supported by the Basic Conditions Platform Construction Project of Sichuan Science and Technology Department (2019JDPT0015), the Major Clinical Disease Research Program from the Health and Family Planning Commission of Sichuan Province (17ZD011), the Yunnan Province Medical Health Research Institute Project (2018NS0102), and the first Affiliated Hospital of Kunming Medical University Doctoral Research Fund Project (2017BS005).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Louis ED, Ottman R, Hauser WA. How common is the most common adult movement disorder? Estimates of the prevalence of essential tremor throughout the world. Mov Disord. (1998) 13:5–10. doi: 10.1002/mds.870130105
2. Louis ED. Non-motor symptoms in essential tremor: a review of the current data and state of the field. Parkinsonism Relat Disord. (2016) 22:115–8. doi: 10.1016/j.parkreldis.2015.08.034
3. Louis ED, Barnes L, Albert SM, Cote L, Schneier FR, Pullman SL, et al. Correlates of functional disability in essential tremor. Mov Disord. (2001) 16:914–20. doi: 10.1002/mds.1184
4. Chandran V, Pal PK, Reddy JYC, Thennarasu K, Yadav R, Shivashankar N. Non-motor features in essential tremor. Acta Neurol Scand. (2012) 125:332–7. doi: 10.1111/j.1600-0404.2011.01573.x
5. Louis ED, Cosentino S, Huey ED. Depressive symptoms can amplify embarrassment in essential tremor. J Clin Mov Disord. (2016) 3:11–6. doi: 10.1186/s40734-016-0039-6
6. Sengul Y, Sengul HS, Yucekaya SK, Yucel S, Bakim B, Pazarc NK, et al. Cognitive functions, fatigue, depression, anxiety, and sleep disturbances: assessment of nonmotor features in young patients with essential tremor. Acta Neurol Belg. (2015) 115:281–7. doi: 10.1007/s13760-014-0396-6
7. Lorenz D, Poremba C, Papengut F, Schreiber S, Deuschl G. The psychosocial burden of essential tremor in an outpatient- and a community-based cohort. Eur J Neurol. (2011) 18:972–9. doi: 10.1111/j.1468-1331.2010.03295.x
8. Louis ED, Huey ED, Gerbin M, Viner AS. Depressive traits in essential tremor: impact on disability, quality of life, and medication adherence. Eur J Neurol. (2012) 19:1349–54. doi: 10.1111/j.1468-1331.2012.03774.x
9. Louis ED, León JB, Pareja FB. Self-reported depression and anti-depressant medication use in essential tremor: cross-sectional and prospective analyses in a population-based study. Eur J Neurol. (2007) 14:1138–46. doi: 10.1111/j.1468-1331.2007.01923.x
10. Tan EK, Chong SF, Lum SY, Gabriel C, Koh KK, Prakasha KM, et al. Non-motor manifestations in essential tremor: use of a validated instrument to evaluate a wide spectrum of symptoms. Parkinsonism Relat Disord. (2005) 11:375–80. doi: 10.1016/j.parkreldis.2005.04.007
11. Dogu O, Louis ED, Sevim S, Kaleagasi H, Aral M. Clinical characteristics of essential tremor in Mersin, Turkey. J Neuro. (2005) 252:570–4. doi: 10.1007/s00415-005-0700-8
12. Mao CJ, Chen JP, Hu WD, Liu CF. Depression associated with movement disorders. Zhonghua Yi Xue Za Zhi. (2013) 93:26–9.
13. Li ZW, Xie MJ, Tian DS, Li JJ, Zhang JP, Jiao L, et al. Characteristics of depressive symptoms in essential tremor. J Clin Neurosci. (2011) 18:52–6. doi: 10.1016/j.jocn.2010.05.021
14. Miller KM, Okun MS, Fernandez HF, Jacobson CE, Rodriguez RL, Bowers D. Depression symptoms in movement disorders: comparing Parkinson's disease, dystonia, and essential tremor. Mov Disord. (2007) 22:666–72. doi: 10.1002/mds.21376
15. Achey RL, Yamamoto E, Sexton D, Hammer C, Lee BS, Butler RS, et al. Prediction of depression and anxiety via patient-assessed tremor severity, not physician-reported motor symptom severity, in patients with Parkinson's disease or essential tremor who have undergone deep brain stimulation. J Neurosurg. (2018) 129:1–10. doi: 10.3171/2017.8.JNS1733
16. Louis ED, Eileen BS, Ashwini KR. Tandem gait performance in essential tremor: clinical correlates and association with midline. Tremors Mov Disord. (2010) 25:1633–8. doi: 10.1002/mds.23144
17. Cerasa A, Quattrone A. Linking essential tremor to the cerebellum-neuroimaging evidence. Cerebellum. (2016) 15:263–75. doi: 10.1007/s12311-015-0739-8
18. Deuschl G, Bain P, Brin M. Consensus statement of the movement disorder society on tremor, Ad. Hoc Sci Committ Mov Disord. (1998) 13:2–23. doi: 10.1002/mds.870131303
19. Fahn S, Tolosa E, Marin C. Clinical rating scale for tremor. In: Jankovic J, Tolosa E, editors. Parkinson's Disease and Movement Disorders. Baltimore; Munich: Urban and Schwarzenberg (1988). p. 225–34.
20. Louis ED, Frucht SJ, Rios E. Intention tremor in essential tremor: prevalence and association with disease duration. Mov Disord. (2009) 24:626–7. doi: 10.1002/mds.22370
21. Katzman R, Zhang MY, Qu OY, Wang ZY, Liu WT, Yu E, et al. A Chinese version of the mini-mental state examination; impact of illiteracy in a shanghai dementia survey. J Clin Epidemiol. (1988) 41:971–8. doi: 10.1016/0895-4356(88)90034-0
22. Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. (1967) 6:278–96. doi: 10.1111/j.2044-8260.1967.tb00530.x
23. Wang XD, Wang XL, Ma H. Rating Scales for mental health Chinese. Peking: Mental Health Journal Press (1999).
24. Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. (1959) 32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x
25. Tdv S. Correlation and regression. In: Statistics at Square One. London: BMJ Publishing Group (1997).
26. Ghio L, Gotelli S, Cervetti A, Respino M, Natta W, Marcenaro M, et al. Duration of untreated depression influences clinical outcomes and disability. J Affect Disorders. (2015) 175:224–8. doi: 10.1016/j.jad.2015.01.014
27. Adamaszek M, Agata FD, Ferrucci R, Habas C, Keulen S, Kirkby KC, et al. Consensus paper: cerebellum and emotion. Cerebellum. (2017) 16:552–76. doi: 10.1007/s12311-016-0815-8
28. Šumec R, Filip P, Sheardová K, Bareš M. Psychological benefits of nonpharmacological methods aimed for improving balance in parkinson's disease: a systematic review. Behav Neurol. (2015) 2015:1–16. doi: 10.1155/2015/620674
29. Cherbuin N, Kim S, Anstey KJ. Dementia risk estimates associated with measures of depression: a systematic review and meta-analysis. BMJ Open. (2015) 5:e008853. doi: 10.1136/bmjopen-2015-008853
30. Santabárbara J, Villagrasa B, López-Antón R, Olaya B, Bueno-Notivol J, de la Cámara C, et al. Clinically significant anxiety as a risk factor for dementia in the elderly community. Acta Psychiatr Scand. (2018) 139:6–14. doi: 10.1111/acps.12966
Keywords: essential tremor, depression, anxiety, female sex, cranial tremor, functional disability
Citation: Huang H, Yang X, Zhao Q, Chen Y, Ning P, Shen Q, Wang H, An R and Xu Y (2019) Prevalence and Risk Factors of Depression and Anxiety in Essential Tremor Patients: A Cross-Sectional Study in Southwest China. Front. Neurol. 10:1194. doi: 10.3389/fneur.2019.01194
Received: 15 August 2019; Accepted: 28 October 2019;
Published: 15 November 2019.
Edited by:
Steven Frucht, Mount Sinai Hospital, United StatesReviewed by:
Santiago Perez-Lloret, National Council for Scientific and Technical Research (CONICET), ArgentinaCopyright © 2019 Huang, Yang, Zhao, Chen, Ning, Shen, Wang, An and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanming Xu, bmV1cm94eW05OTlAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.