- 1Department of Neurology, College of Medicine, Ewha Womans University Mokdong Hospital, Seoul, South Korea
- 2Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea
- 3Department of Digital Health, SAIHST, Sungkyunkwan University, Seoul, South Korea
- 4Department of Neurology, Eunpyeong St.Mary's Hospital, The Catholic University of Korea, Seoul, South Korea
- 5Department of Neurology, Kyung Hee University College of Medicine, Seoul, South Korea
- 6Department of Neurology, Korea University Ansan Hospital, Korea University College of Medicine, Seoul, South Korea
- 7Department of Neurology, Korea University Guro Hospital, Korea University College of Medicine, Seoul, South Korea
- 8Department of Neurology, Korea University Anam Hospital, Korea University College of Medicine, Seoul, South Korea
- 9Department of Neurology, Chung-Ang University College of Medicine, Seoul, South Korea
- 10Department of Neurology, MyongjiHospital, Hanyang University, College of Medicine, Goyang-si, South Korea
- 11Department of Neurology, Jeju National University, Jeju-si, South Korea
- 12Department of Neurology, Chonnam National University Medical School and Hospital, Gwangju, South Korea
- 13Department of Neurology, School of Medicine, Kyungpook National University, Daegu, South Korea
Background and aims: Atrial fibrillation (AF) is a major cause of ischemic stroke; however, detailed clinical data and prognostic factors for stroke patients with AF are lacking in Korea. We aimed to investigate clinical information and factors associated with functional outcomes of stroke patients with AF from the Korean nationwide ATrial fibrillaTion EvaluatioN regisTry in Ischemic strOke patieNts (K-ATTENTION) database.
Methods: From January 2013 to December 2015, consecutive clinical information from acute stroke patients with AF or history of AF was collected from 11 centers in Korea. Collected data included demographics, risk factors, pre-stroke medication, stroke severity, stroke subtypes, concomitant cerebral atherosclerosis, brain image findings, recanalization therapy, discharge medication, and functional outcome at 3 months after index stroke.
Results: A total of 3,213 stroke patients (mean age, 73.6 ± 9.8 years; female, 48.6%) were included. The mean CHA2DS2-VASc score was 4.9. Among the 1,849 (57.5%) patients who had brain image and functional outcome data, poor outcome (modified Rankin scale > 2) was noted in 53.1% (981/1,849) of patients. After adjusting for age, sex, and variables that had a p < 0.05 in univariate analysis or well-known factors for functional outcome, presence of asymptomatic extracranial cerebral atherosclerosis [odd ratio (OR): 1.96, 95% confidence interval (CI): 1.36–2.82, p = 0.001] and less frequent prior stroke statin intake (OR: 0.69, 95% CI: 0.49–0.98, p = 0.038) were associated with poor functional outcome.
Conclusion: Our results suggest that presence of non-relevant extracranial cerebral atherosclerosis may affect poor functional outcome and prior stroke statin therapy may be feasible in Korean stroke patients with AF.
Introduction
Atrial fibrillation (AF) is frequent cardiac arrhythmia and is associated with increased risk of systemic embolism, hospitalization, and death (1, 2). Particularly, AF is a well-known major risk factor for occurrence and recurrence of stroke and stroke-related mortality (3). With the current aging population and associated increased concomitant vascular risk factors and/or cardiovascular disease, the burden of AF is increasing in the Western and Asian populations, including South Korea, China, and Japan (4–7).
Meanwhile, most of the current data on AF patients with a previous history of stroke have focused on secondary prevention from recurrent ischemic stroke or other thromboembolic complications; in contrast, evidence regarding acute stroke patients with AF has been limited. The functional outcome of AF patients with acute stroke is a major determinant of mortality and long-term recurrence and the decision whether to use oral anticoagulants is dependent on the neurological status and findings obtained from neuroimaging rather than conventional risk stratification schemes such as CHA2DS2-VASc score. Therefore, comprehensive real-world data considering neurological status, acute treatment pattern such as reperfusion therapy, neuroimaging findings, and early outcome of acute stroke in patients with AF is needed. Furthermore, although characteristics or outcome of stroke may be different according to race in stroke patients with AF, researches regarding characteristics and factors for short-term functional outcome of AF-related stroke for in Asian stroke population have been limited.
We aimed to demonstrate demographics and outcome parameters and to investigate factors associated with early functional outcomes of stroke patients with AF from the Korean nationwide ATrial fibrillaTion EvaluatioN regisTry in Ischemic strOke patieNts (K-ATTENTION) database.
Materials and Methods
Study Design
The K-ATTENTION is a multicenter, nationwide, retrospective cohort study to evaluate the diagnosis, treatment, and prognosis of acute stroke subjects with AF in a real-world clinical setting in Korea from January 2013 to December 2015. Regional and local emergency medical centers (9 tertiary and 2 secondary hospitals) from 5 provinces participated in this registry. The list of participating hospitals and numbers of included subjects are shown in Supplementary Figure 1. Criteria for inclusion are presented in Supplementary Table 1. Approximately 80% of stroke subjects who were admitted to each hospital were from the city, county, or district where the patient lives. In our registry, no subjects were registered in duplicate. The comparison between K-ATTENTION and other previous researches regarding stroke subjects with AF is shown in Supplementary Table 2. The primary, secondary, and exploratory purpose of our study and plans of our research are described in Supplementary Table 3. The design of this study was approved by the Institutional Review Board from each participating site. Because of the retrospective and observational nature of the protocol, written informed consents were waived (Samsung Medical Center, 2016-07-011).
Subjects
As described in Supplementary Table 1, all of subjects over 20 years of age who were diagnosed with cerebral infarction accompanying AF during the study period (January 1, 2013 to December 31, 2015) or having past history of AF were consecutively included in the study from each participating center. Cerebral infarction was defined as ischemic lesions as identified through brain imaging (CT or MRI) accompanied by neurologic symptoms or signs. The presence of AF was defined as arrhythmia that lasted for more than 30 s with irregular R-R intervals, no clear repetitive P-waves, and cardiologist confirmation at each hospital. AF was diagnosed via electrocardiogram (ECG), 24 or 48-h electrocardiogram, or telemonitoring with recording and automated rhythm detection. Subjects who were not adequately screened for stroke and arrhythmia (for example, subjects that did not undergo brain CT and/or MRI, MRA, or ECG) or without evidence of cerebral infarction on brain images were excluded from the study (8–10).
Clinical Data and Outcome Collection
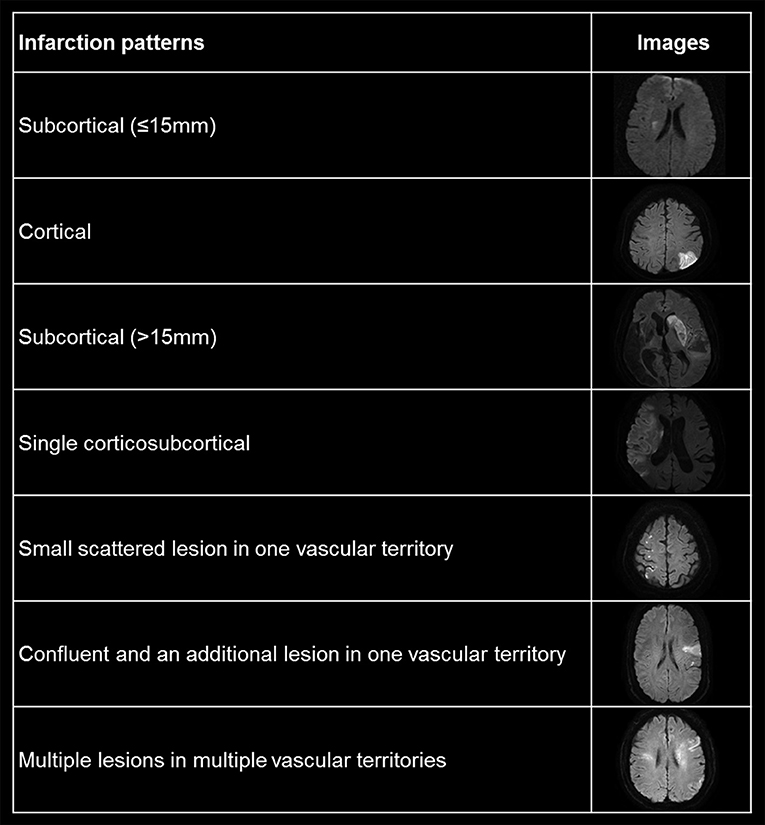
The following demographics, including vascular risk factors, previous medical history including stroke, underlying ≥50% intra- and/or extracranial atherosclerosis (ICAS, ECAS, respectively), whether recanalization therapy was performed, discharge medication (anti-thrombotics including anti-platelet, warfarin, or non-vitamin K dependent oral anti-coagulant), and modality of recanalization therapy were recorded (11, 12). Stroke severity was determined using the National Institutes of Health Stroke Scale (NIHSS) at admission (13). Stroke classification was determined based on the Trial of Org 10172 in the Acute Stroke Treatment (TOAST) classification system (14). For convenience, stroke subtypes were divided into AF only, AF + large artery atherosclerosis, AF + small vessel occlusion, and AF + stroke of other determined causes. The patterns of cerebral infarction were categorized into subcortical (≤15 mm), cortical, subcortical (>15 mm), single corticosubcortical, small scattered lesion in one vascular territory, confluent, and an additional lesion in one vascular territory and multiple lesions in multiple vascular territories (Figure 1). Presence and classification of hemorrhagic transformation, including symptomatic intracranial hemorrhage, was defined as based on the European Cooperative Acute Stroke Study criteria (15). The image findings of all included patients were validated by an expert group (WKS and BJK). Functional outcome was dichotomized to favorable outcome (mRS ≤ 2) or poor outcome (mRS > 2) at 3 months after index stroke (16). If the patient was found to have died within 3 months, the mRS at 3 months was defined as 6 points. The mRS was routinely checked by a well-trained research nurse or neurology specialist at each hospital.
Data Management and Quality Control
All data were collected and uploaded via a web-based electronic data capturing system. All investigators accessed this secure data base system and registered mandatory variables related to this study. The collected data were monitored and audited by a quality control team.
Statistical Analysis
Statistical analysis was performed using the SPSS 22.0 (IBM, Armonk, NY, USA) software program. The data obtained from this clinical study are expressed as the average value, standard deviation or median value and quartile range for continuous data, and frequency and corresponding percentage for categorical data. Independent Student's t-test was used for continuous data and the Chi-square test and Fisher's exact test for categorical data. If the parametric test was not satisfactory, we used the appropriate non-parametric test method. Univariate and multivariate binary logistic regression analyses were conducted using the poor outcome at 3 months after index stroke as the dependent variable. To control for over-fitting and small sample size, stroke subtype of AF + stroke for other determined causes was included using the stroke subtype of AF only. Age, sex, and variables with a p < 0.05 in univariate analyses and well-known factors related with functional outcome after stroke were entered into multivariate binary and ordinal logistic regression analyses. Because of multicollinearity between underlying risk factors and stratification risk scores, CHADS2 score, and CHA2DS2-VASc score were not entered in the multivariate analysis. A two-tailed p < 0.05 was considered significant.
Results
Demographics and Characteristics of the Registered Subjects
The baseline characteristics and profiles of vascular risk factors and possible etiologic classification of the subjects are described in Supplementary Table 4. A total of 3,213 stroke patients [mean age, 73.6 ± 9.8 years; men, 50.9% (1,246/3,213)] were included in the study. Etiologic stroke classification among patients who were classified into stroke subtypes was 76.2% (2,450/3,213), the AF only group comprised 83.8% (2,053/2,450), and was followed by two or more causes [atherosclerotic 12.2% (298/2,450), small vessel occlusion 3.0% (74/2,450), and other (1.0% (25/2,450)]. The median National Institute of Health Stroke Scale (NIHSS) score at presentation was 8. The CHADS2 score and CHA2DS2-VASc score were 3.4 ± 0.9 and 4.9 ± 1.3, respectively.
Factors Associated With Poor Functional Outcome at 3 Months
Among the 3,213 patients included, 959 patients without detailed brain image data [cerebral infarction patterns of diffusion weighed image (n = 807), presence of cerebral artery stenosis (n = 67), and information for presence of hemorrhagic transformation (n = 85)] were excluded. Then, 405 patients who did not have 3-month mRS information were also excluded. A total of 1,849 (57.5%) patients [favorable outcome of 46.9% (868/1,849), poor outcome of 53.1% (981/1,849)] that had prognosis data at 3 months were finally included in our study (Supplementary Figure 2). There were no differences regarding demographics and vascular risk factors among the included patients and non-included patients except frequency of dyslipidemia and persistent AF [more commonly noted in non-included patients; 31.1% vs. 18.6% for dyslipidemia (p = 0.001) and 57.4% vs. 45.1% for persistent AF (p = 0.001)] (Supplementary Table 5). Compared with non-included (without image data) patients, patients who included in our study had a higher frequency of previous ischemic stroke history (p < 0.001). Also, patients who included in our study had a lower frequency of hypercholesterolemia (p < 0.001) and stroke subtype of AF only (p < 0.001) than those of non-included patients. Considering initial NIHSS and mRS, included patients had higher NIHSS (p = 0.013) and mRS (p < 0.001) than those with non-included patients (Supplementary Table 6).
Among the 1,849 patients, reperfusion therapies including intravenous t-PA infusion and/or endovascular therapy at index event were performed for 31.5% (584/1,849) of patients. Regarding pre-stroke oral anticoagulant use undergoing reperfusion therapy, frequency of taking warfarin, and NOAC were 12.1%, 4.0% on t-PA, 25.0%, 3.1% for endovascular therapy, and 15.6%, 3.0% on combined therapy (Supplementary Figure 3).
Patients who prescribed antiplatelet at discharge had lower body mass index than that of patients who were not prescribed antiplatelet at discharge (22.7 ± 3.1 vs. 23.2 ± 3.2, p = 0.002). Moreover, patients who prescribed antiplatelet at discharge more frequently accompanied under-dosing NOAC at discharge (7.0% vs. 3.7% p = 0.008) and ICAS (33.8% vs. 28.3%, p = 0.031) than those of patients who were not prescribed antiplatelet at discharge (Supplementary Table 7).
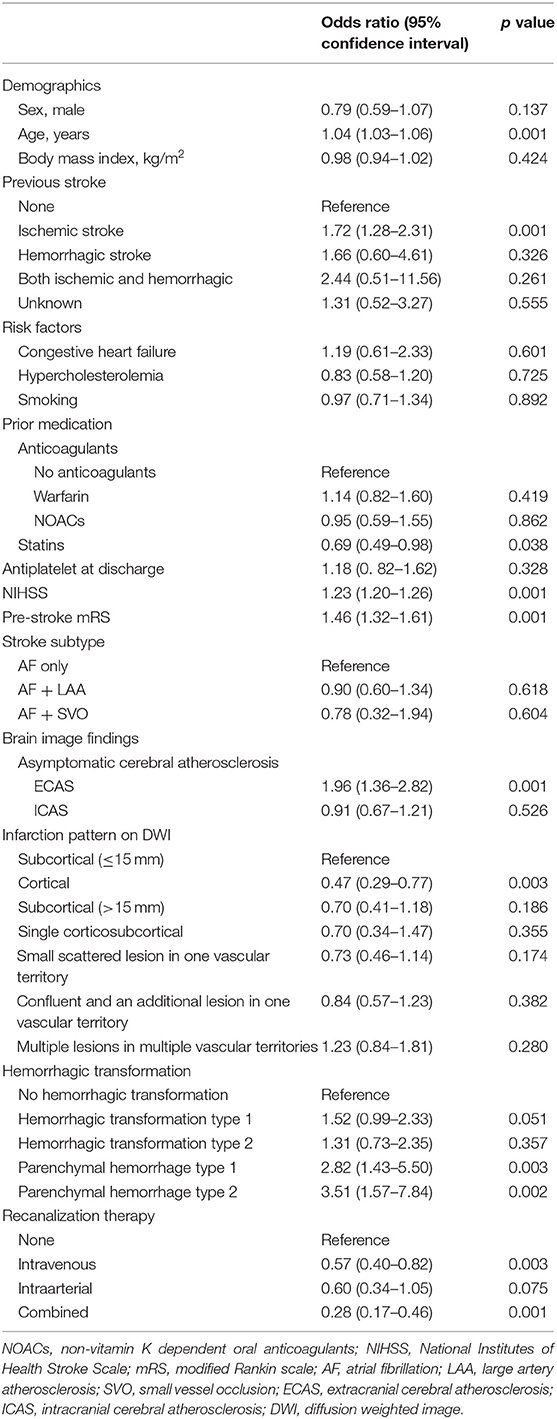
When comparing patients with poor outcome with good outcome, the poor outcome group less frequently included men, had higher NIHSS, pre-stroke mRS, and CHA2DS2-VASc score, were older and had lower body mass index than that of the good outcome group. Moreover, the poor outcome group more frequently had previous stroke history, congestive heart failure, prior stroke warfarin intake, AF only stroke subtype, asymptomatic ECAS, asymptomatic ICAS, specific infarction patterns (single corticosubcortical, confluent and an additional lesion in one vascular territory, or multiple lesions in multiple vascular territories), presence of hemorrhagic transformation, and thrombolytic therapy. In addition, the poor outcome group less frequently had hypercholesterolemia, current smoking, and prior stroke statin intake (Table 1). Distribution of mRS on 3 months (percent) according to infarction patterns and association of frequency of pre-stroke use of oral anticoagulants (percent) with mRS on 3 months were presented at Figures 2, 3.
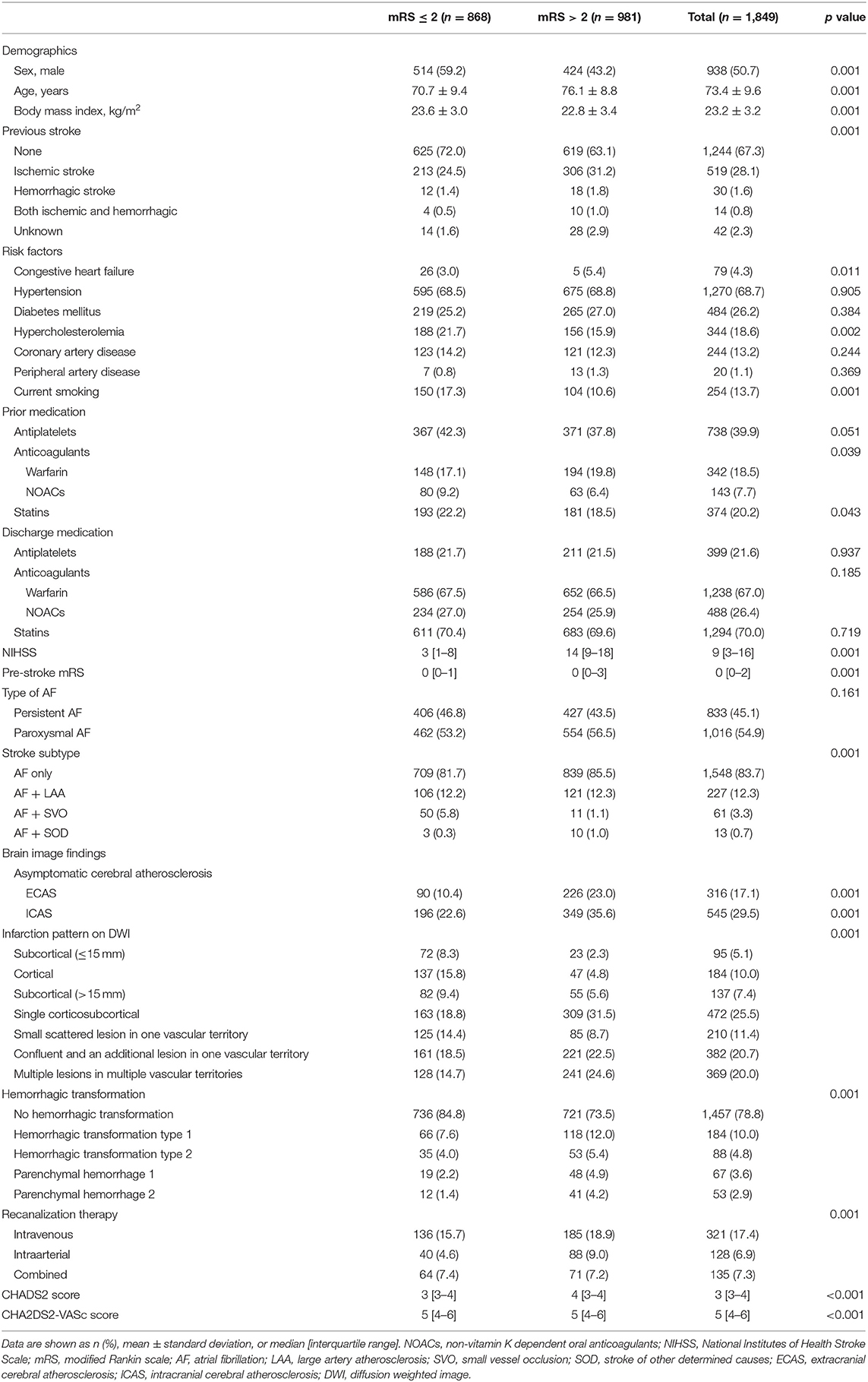
Table 1. Comparison of clinical and brain image findings according to functional outcome at 3 months after index stroke.
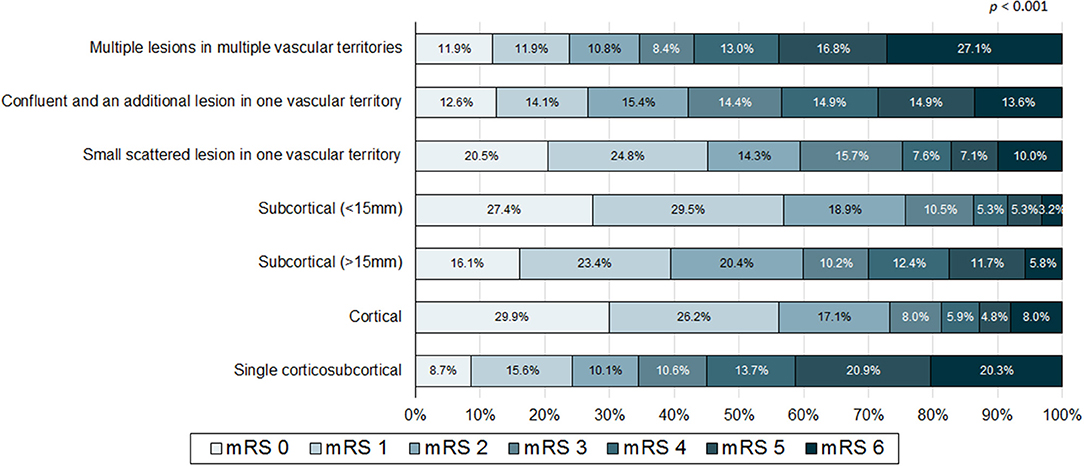
Figure 2. Distribution of modified Rankin score (mRS) on 3 months (percent) according to infarction patterns.
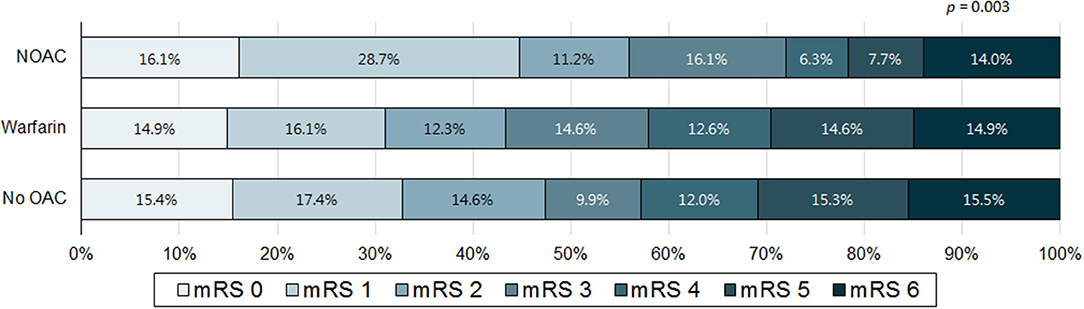
Figure 3. Association of frequency of pre-stroke use of oral anticoagulants (percent) with modified Rankin score (mRS) on 3 months. NOAC, non-vitamin K dependent oral anticoagulant; OAC, oral anticoagulant.
Independent Factors for Poor Functional Outcome at 3 Months
Multivariate analysis showed increased age [odds ratio (OR): 1.04, 95% confidence interval (CI): 1.03–1.06, p = 0.001], previous ischemic stroke history (OR: 1.72, 95% CI: 1.28–2.31, p = 0.001), NIHSS (OR: 1.23, 95% CI: 1.20–1.26, p = 0.001), pre-stroke mRS (OR: 1.46, 95% CI: 1.32–1.61, p = 0.001), presence of asymptomatic ECAS (OR: 1.96, 95% CI: 1.36–2.82, p = 0.001), parenchymal hemorrhage type 1 (OR: 2.82, 95% CI 1.43–5.50, p = 0.003), and parenchymal hemorrhage type 2 (OR: 3.51, 95% CI: 1.57–7.84, p = 0.002) were significantly associated with poor functional outcomes (Table 2). Prior stroke statin intake (OR: 0.69, 95% CI: 0.49–0.98, p = 0.038), cortex only located infarction (OR: 0.47, 95% CI: 0.29–0.77, p = 0.003), and thrombolytic therapy (intravenous (OR: 0.57, 95% CI: 0.40–0.82) or both (intravenous and intraarterial) (OR: 0.28, 95% CI: 0.17–0.46) were also negatively related to poor functional outcome (Table 2). These associations were consistently noted in ordinal logistic regression analysis including presence of asymptomatic ECAS (OR: 2.04, 95% CI: 1.61–2.58, p = 0.001), except prior stroke statin intake (OR: 0.94, 95% CI: 0.74–1.18, p = 0.606). Furthermore, in subgroup analysis, there were no statistical interaction between pre-stroke mRS and presence of asymptomatic ECAS (p = 0.205), prior stroke statin intake (p = 0.580) for poor functional outcome.
In subgroup analysis for patients with who were taking anti-thrombotics (antiplatelet, warfarin, and NOAC), multivariate analysis showed that previous ischemic stroke history (OR: 1.80, 95% CI: 1.16–2.80, p = 0.008), NIHSS (OR: 1.15, 95% CI: 1.10–1.20, p < 0.001), pre-stroke mRS (OR: 1.59, 95% CI: 1.38–1.84, p < 0.001), and presence of asymptomatic ICAS (OR: 1.75, 95% CI: 1.16–2.64, p = 0.007) were significantly associated with poor functional outcomes (Table 3). The cortex only located infarction (OR: 0.45, 95% CI: 0.20–0.98, p = 0.046) and combined intravenous and intraarterial reperfusion therapy (OR: 0.26, 95% CI: 0.11–0.58, p = 0.001) were also negatively related to poor functional outcome (Table 3).
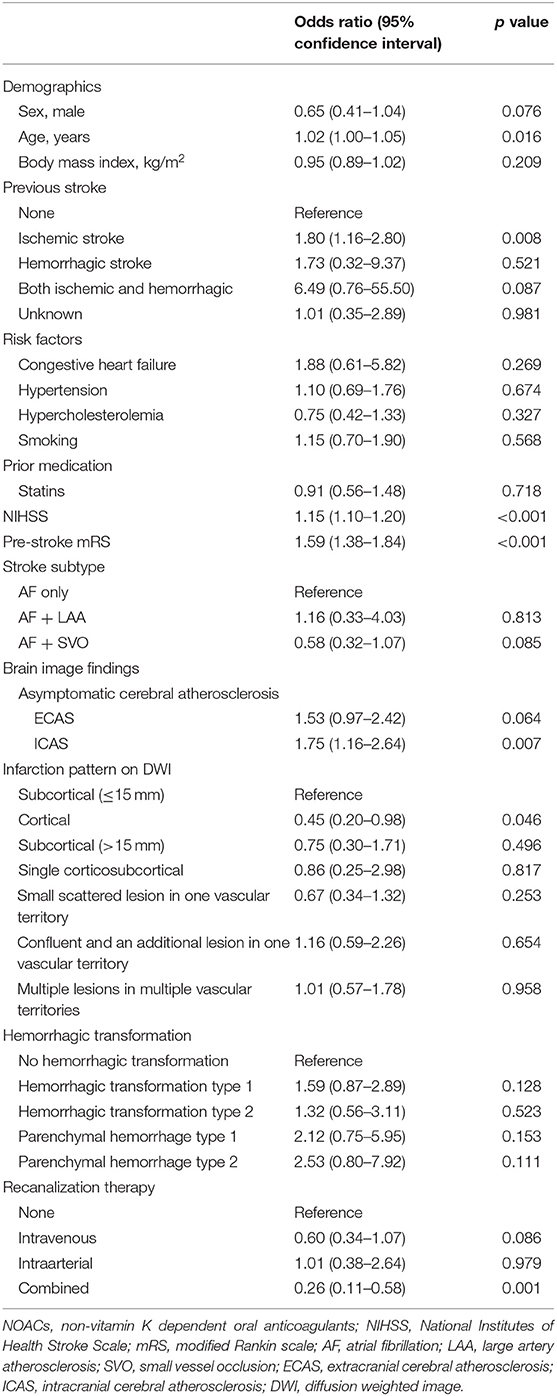
Table 3. Independent factors for poor functional outcome in patients who taking prior anti-thrombotics.
Discussion
The key findings of our study include the following: (1) to provide demographics and baseline characteristics for a Korean nationwide AF-stroke retrospective study (K-ATTENTION study) and (2) to investigate the independent factors for poor functional outcome at 3 months in this study sample.
Because stroke with AF is independent and different from stroke without AF, stroke subjects with AF should be treated prudently. There are cohort/registries of stroke subjects with AF in some countries other than Korea; however, several limitations exist in these cohort/registries such as small sample size (17), limited inclusion criteria (subjects who received intravenous thrombolytic agents) (18), were prescribed specific NOAC only (19), or warfarin only (20, 21) and lack of information regarding time in therapeutic range in warfarin users (22). In contrast, our K-ATTENTION study has the following significance and strength. First, our study was designed to supply important and timely insight into the management of acute cerebral infarction subjects with AF using a large multicenter, nationwide study. Second, apart from providing information for anticoagulant use and predictive factors for functional outcome, our study provides information on infarction pattern, recanalization therapy outcomes, and detailed anti-thrombotic therapy (particularly NOACs) information for Asian subjects. Third, anticoagulant therapy has important implications for acute stroke patients, including reperfusion therapy. The current guidelines recommend that intravenous tissue plasminogen activator inhibitors should not be administered as often as possible, especially if warfarin concentration is above the certain level or if NOACs are being administered. This means that intra-arterial thrombectomy should be considered immediately in situations requiring recanalization therapy (23, 24). Because our study mainly includes subjects who have been taking anticoagulants, the K-ATTENTION study may provide a current status of mechanical thrombectomy in stroke patients with AF, especially for patients on NOACs. K-ATTENTION study will provide researches with additional information on this part in subsequent studies.
In addition to the well-known factors associated with stroke outcome (age, previous stroke, NIHSS, pre-stroke mRS, infarction pattern, hemorrhagic transformation, and recanalization therapy), prior stroke statin intake was significantly associated with good functional outcomes in our study. A previous study showed that pre-stroke treatment with statins was an independent factor associated with good outcomes in patients with atherosclerotic stroke or lacunar stroke, but not with cardioembolic stroke (25). Additionally, the previous Fukuoka stroke registry-based study, which included cardioembolic stroke, revealed that prior stroke statin treatment in ischemic stroke patients was significantly related to mild neurological symptoms within 24 h of onset (26). Furthermore, a previous meta-analysis including 23,577 patients with AF showed that statin itself was beneficial for incidence or recurrence of AF (27). However, prior stroke statin treatment did not significantly influence the short-term functional outcome (26). In contrast, premorbid use of statins in AF patients is associated with excellent collateral flow in acute stroke patients (28). Our results are partially in line with these studies and any discrepancy may be caused by sample size differences, the inclusion of different patient characteristics or racial differences. Furthermore, we could not analyze the type and intensity of statin, and persistence of statin after admission; therefore, further study is needed.
Our study demonstrated that stenosis or occlusion of the non-relevant artery, especially asymptomatic extra-cranial atherosclerosis, was associated with poor functional outcomes. This may be due to a lack of collateral flow or a decrease in cerebral perfusion, or a recurrent stroke in the non-relevant artery itself. It has been reported that the burden of cerebral atherosclerosis increases with increasing CHADS2 score in stroke patients with AF (29). Moreover, another study demonstrated that the presence and increased burden of non-relevant artery stenosis were related to poor functional outcome in acute stroke patients (30). Thus, our data provides additional information that functional outcome may be poor if non-relevant artery stenosis is noted in stroke patients with AF.
In a previous study, severity of stroke at admission and functional outcome of cardioembolic stroke patients managed with NOACs and warfarin within therapeutic ranges were similar, and patient outcomes when taking NOACs were more favorable than those with warfarin below the therapeutic range or those without anticoagulants (31). Furthermore, a recent retrospective observational study of 94,474 patients with AF-stroke demonstrated that taking NOACs before admission was associated with lower odds of moderate to severe stroke and in-hospital mortality (32). Even though significance was only found in univariate analysis; our results demonstrated that taking NOACs before an index stroke might be more beneficial than taking warfarin for short-term functional outcomes. This may be due to the small sample size of subjects taking NOACs prior to an index stroke, or other clinical factors may have had stronger effects on poor functional outcome. Expecting that the prescription of NOACs would increase based on the national insurance coverage system in Korea, further studies regarding this issue are needed.
Our study has limitations. First, because it was performed retrospectively, even though subjects who were included in our study were prospectively collected from a stroke registry from each participating hospital, selection bias exists. Second, because K-ATTENTION was conducted only for subjects who visited regional or local emergency medical centers, it does not reflect the current overall managing status of subjects with AF in Korea. Third, in our dataset, the rate of patients who were lost to follow-up at 3 months is ~18%. This censoring could make selection bias in our study. Fourth, since our study period was not the time when antidote of NOAC was widely used, our study does not provide data on this. Fifth, as with other observational registries, any relationship between treatment and outcomes from K-ATTENTION are based on non-randomized comparisons and thus are potentially influenced by measured and unmeasured confounding factors.
Conclusions
The K-ATTENTION study provides a valuable opportunity for identifying the recent status of antithrombotic therapy for the secondary prevention of patients with AF-related stroke in Korea. Furthermore, our study suggests that prior stroke statin therapy may be feasible, and the presence of asymptomatic extra-cranial atherosclerosis may affect poor functional outcomes in stroke patient with AF.
Data Availability Statement
The datasets for this manuscript are not publicly available because: policy of ethical committee of each participating site. Request to access the datasets should be directed to W-KS (bWNhc3Rlbm9zaXNAZ21haWwuY29t).
Author Contributions
W-KS and T-JS drafted the paper with input and critical review from all authors. I-YB, HW, Y-JK, YC, BK, SH, J-MJ, KO, CK, SY, KP, J-MK, J-HP, JC, M-SP, J-TK, K-HC, Y-HH, J-WC, OB, and G-MK performed study selection, data extraction, and quality assessment.
Funding
W-KS provided financial support by a grant from Korean Neurological Association (KNA-17-MI-10) and National Research Foundation of Korea funded by the Ministry of Education (2019R1A2C2008788). T-JS provided financial support in the form of a grant from the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education (2018R1D1A1B07040959). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
W-KS received honoraria for lectures from Pfizer, Sanofi-Aventis, Otsuka Korea, Dong-A Pharmaceutical Co., Ltd., Beyer, Daewoong pharmaceutical Co., Ltd., Daiichi Sankyo Korea Co., Ltd., Boryung pharmaceutical, study grant from Daiichi Sankyo Korea Co., Ltd., consulting fee from OBELAB Inc., and stock option from JLK Inspection. J-MJ received honoraria for lectures from Pfizer, Sanofi-Aventis, Dong-A, Daewoong Pharmaceutical Co., Ltd., and Boryung Pharmaceutical Co., Ltd., a study grant from Il-dong Pharmaceutical Co., Ltd., and consulting fees from OBELAB Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the Korean Neurology Association.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2019.01101/full#supplementary-material
References
1. Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation: a global burden of disease 2010 study. Circulation. (2014) 129:837–47. doi: 10.1161/CIRCULATIONAHA.113.005119
2. Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the framingham heart study. Circulation. (1998) 98:946–52. doi: 10.1161/01.CIR.98.10.946
3. Lin HJ, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, et al. Stroke severity in atrial fibrillation. The framingham study. Stroke. (1996) 27:1760–4. doi: 10.1161/01.STR.27.10.1760
4. Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the anticoagulation and risk factors in atrial fibrillation (atria) study. JAMA. (2001) 285:2370–5. doi: 10.1001/jama.285.18.2370
5. Guo Y, Tian Y, Wang H, Si Q, Wang Y, Lip GY. Prevalence, incidence, and lifetime risk of atrial fibrillation in china: new insights into the global burden of atrial fibrillation. Chest. (2015) 147:109–19. doi: 10.1378/chest.14-0321
6. Inoue H, Fujiki A, Origasa H, Ogawa S, Okumura K, Kubota I, et al. Prevalence of atrial fibrillation in the general population of japan: an analysis based on periodic health examination. Int J Cardiol. (2009) 137:102–7. doi: 10.1016/j.ijcard.2008.06.029
7. Choi EJ, Lee IH, Je NK. Inadequate stroke prevention in korean atrial fibrillation patients in the post-warfarin era. Int J Cardiol. (2016) 220:647–52. doi: 10.1016/j.ijcard.2016.06.177
8. Lee BI, Nam HS, Heo JH, Kim DI, Yonsei Stroke T. Yonsei stroke registry. Analysis of 1,000 patients with acute cerebral infarctions. Cerebrovasc Dis. (2001) 12:145–51. doi: 10.1159/000047697
9. Choi HY, Seo JH, Yang JH, Kim YD, Jung YH, Cho HJ, et al. Beneficial effects of stroke-unit care in stroke patients with atrial fibrillation. Yonsei Med J. (2013) 54:301–5. doi: 10.3349/ymj.2013.54.2.301
10. Song TJ, Kim YD, Yoo J, Kim J, Chang HJ, Hong GR, et al. Association between aortic atheroma and cerebral small vessel disease in patients with ischemic stroke. J Stroke. (2016) 18:312–20. doi: 10.5853/jos.2016.00171
11. Song TJ, Cho HJ, Chang Y, Choi K, Jung AR, Youn M, et al. Low plasma proportion of omega 3-polyunsaturated fatty acids predicts poor outcome in acute non-cardiogenic ischemic stroke patients. J Stroke. (2015) 17:168–76. doi: 10.5853/jos.2015.17.2.168
12. Chang Y, Kim J, Kim MH, Kim YJ, Song TJ. Interarm blood pressure difference is associated with early neurological deterioration, poor short-term functional outcome, and mortality in noncardioembolic stroke patients. J Clin Neurol. (2018) 14:555–65. doi: 10.3988/jcn.2018.14.4.555
13. Oh MS, Yu KH, Lee JH, Jung S, Ko IS, Shin JH, et al. Validity and reliability of a korean version of the national institutes of health stroke scale. J Clin Neurol. (2012) 8:177–83. doi: 10.3988/jcn.2012.8.3.177
14. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. Toast. Trial of org 10172 in acute stroke treatment. Stroke. (1993) 24:35–41. doi: 10.1161/01.STR.24.1.35
15. Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ecass ii). Second european-australasian acute stroke study investigators. Lancet. (1998) 352:1245–51. doi: 10.1016/S0140-6736(98)08020-9
16. Song TJ, Chang Y, Chun MY, Lee CY, Kim AR, Kim Y, et al. High dietary glycemic load is associated with poor functional outcome in patients with acute cerebral infarction. J Clin Neurol. (2018) 14:165–73. doi: 10.3988/jcn.2018.14.2.165
17. Lopes RD, Shah BR, Olson DM, Zhao X, Pan W, Bushnell CD, et al. Antithrombotic therapy use at discharge and 1 year in patients with atrial fibrillation and acute stroke: results from the avail registry. Stroke. (2011) 42:3477–83. doi: 10.1161/STROKEAHA.111.625392
18. Saji N, Kimura K, Tateishi Y, Fujimoto S, Kaneko N, Urabe T, et al. Safety and efficacy of non-vitamin k oral anticoagulant treatment compared with warfarin in patients with non-valvular atrial fibrillation who develop acute ischemic stroke or transient ischemic attack: a multicenter prospective cohort study (davinci study). J Thromb Thrombolysis. (2016) 42:453–62. doi: 10.1007/s11239-016-1376-x
19. Yasaka M, Minematsu K, Toyoda K, Yamagami H, Yoshimura S, Nagao T, et al. Design and rationale of the relaxed (recurrent embolism lessened by rivaroxaban, an anti-xa agent, of early dosing for acute ischemic stroke and transient ischemic attack with atrial fibrillation) study. J Stroke Cerebrovasc Dis. (2016) 25:1342–8. doi: 10.1016/j.jstrokecerebrovasdis.2016.01.035
20. Palomaki A, Kiviniemi T, Mustonen P, Odei C, Hartikainen JEK, Nuotio I, et al. Mortality after stroke in patients with paroxysmal and chronic atrial fibrillation - the fibstroke study. Int J Cardiol. (2017) 227:869–74. doi: 10.1016/j.ijcard.2016.06.107
21. Pandey DK, Cursio JF, Investigators CS. Data feedback for quality improvement of stroke care: capture stroke experience. Am J Prev Med. (2006) 31:S224–9. doi: 10.1016/j.amepre.2006.08.006
22. Toyoda K, Arihiro S, Todo K, Yamagami H, Kimura K, Furui E, et al. Trends in oral anticoagulant choice for acute stroke patients with nonvalvular atrial fibrillation in Japan: the samurai-nvaf study. Int J Stroke. (2015) 10:836–42. doi: 10.1111/ijs.12452
23. Tsivgoulis G, Katsanos AH, Mavridis D, Magoufis G, Arthur A, Alexandrov AV. Mechanical thrombectomy improves functional outcomes independent of pretreatment with intravenous thrombolysis. Stroke. (2016) 47:1661–4. doi: 10.1161/STROKEAHA.116.013097
24. Demaerschalk BM, Kleindorfer DO, Adeoye OM, Demchuk AM, Fugate JE, Grotta JC, et al. Scientific rationale for the inclusion and exclusion criteria for intravenous alteplase in acute ischemic stroke: a statement for healthcare professionals from the american heart association/american stroke association. Stroke. (2016) 47:581–641. doi: 10.1161/STR.0000000000000086
25. Martinez-Sanchez P, Rivera-Ordonez C, Fuentes B, Ortega-Casarrubios MA, Idrovo L, Diez-Tejedor E. The beneficial effect of statins treatment by stroke subtype. Eur J Neurol. (2009) 16:127–33. doi: 10.1111/j.1468-1331.2008.02370.x
26. Ishikawa H, Wakisaka Y, Matsuo R, Makihara N, Hata J, Kuroda J, et al. Influence of statin pretreatment on initial neurological severity and short-term functional outcome in acute ischemic stroke patients: the fukuoka stroke registry. Cerebrovasc Dis. (2016) 42:395–403. doi: 10.1159/000447718
27. Fang WT, Li HJ, Zhang H, Jiang S. The role of statin therapy in the prevention of atrial fibrillation: a meta-analysis of randomized controlled trials. Br J Clin Pharmacol. (2012) 74:744–56. doi: 10.1111/j.1365-2125.2012.04258.x
28. Lee MJ, Bang OY, Kim SJ, Kim GM, Chung CS, Lee KH, et al. Role of statin in atrial fibrillation-related stroke: an angiographic study for collateral flow. Cerebrovasc Dis. (2014) 37:77–84. doi: 10.1159/000356114
29. Kim YD, Cha MJ, Kim J, Lee DH, Lee HS, Nam CM, et al. Increases in cerebral atherosclerosis according to chads2 scores in patients with stroke with nonvalvular atrial fibrillation. Stroke. (2011) 42:930–4. doi: 10.1161/STROKEAHA.110.602987
30. Kim J, Song TJ, Song D, Lee HS, Nam CM, Nam HS, et al. Nonrelevant cerebral atherosclerosis is a strong prognostic factor in acute cerebral infarction. Stroke. (2013) 44:2013–5. doi: 10.1161/STROKEAHA.113.001111
31. Tomita H, Hagii J, Metoki N, Saito S, Shiroto H, Hitomi H, et al. Severity and functional outcome of patients with cardioembolic stroke occurring during non-vitamin k antagonist oral anticoagulant treatment. J Stroke Cerebrovasc Dis. (2015) 24:1430–7. doi: 10.1016/j.jstrokecerebrovasdis.2015.03.004
Keywords: atrial fibrillation, stroke, Korea, nationwide cohort, outcome assessment
Citation: Song T-J, Baek I-Y, Woo HG, Kim Y-J, Chang Y, Kim BJ, Heo SH, Jung J-M, Oh K, Kim CK, Yu S, Park KY, Kim J-M, Park J-H, Choi JC, Park M-S, Kim J-T, Choi K-H, Hwang Y-H, Chung J-W, Bang OY, Kim G-M and Seo W-K (2019) Characteristics and Factors for Short-Term Functional Outcome in Stroke Patients With Atrial Fibrillation, Nationwide Retrospective Cohort Study. Front. Neurol. 10:1101. doi: 10.3389/fneur.2019.01101
Received: 12 April 2019; Accepted: 01 October 2019;
Published: 18 October 2019.
Edited by:
Thanh G. Phan, Monash Health, AustraliaReviewed by:
Jeongho Hong, Keimyung University Dongsan Medical Center, South KoreaWi-Sun Ryu, Dongguk University Ilsan Hospital, South Korea
Copyright © 2019 Song, Baek, Woo, Kim, Chang, Kim, Heo, Jung, Oh, Kim, Yu, Park, Kim, Park, Choi, Park, Kim, Choi, Hwang, Chung, Bang, Kim and Seo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tae-Jin Song, a25zdGFyQGV3aGEuYWMua3I=; Woo-Keun Seo, bWNhc3Rlbm9zaXNAZ21haWwuY29t
†These authors have contributed equally to this work
 Tae-Jin Song1*†
Tae-Jin Song1*† In-Young Baek
In-Young Baek Ho Geol Woo
Ho Geol Woo Yong-Jae Kim
Yong-Jae Kim Bum Joon Kim
Bum Joon Kim Sung Hyuk Heo
Sung Hyuk Heo Kyungmi Oh
Kyungmi Oh Jong-Ho Park
Jong-Ho Park Jay Chol Choi
Jay Chol Choi Jong-Won Chung
Jong-Won Chung Woo-Keun Seo
Woo-Keun Seo