- 1Vijaya ENT Care Centre, Superspeciality Otology Centre, Bangalore, India
- 2Department of Otolaryngology-Head and Neck Surgery, University of Illinois Hospitals, Chicago, IL, United States
Background: Our tertiary otology center treats facial weakness and paralysis after motor vehicle crashes. We evaluate these patients with physical exam, audiogram, Schirmer's test, and CT scan. Our protocol for management of the facial weakness provides good results for our patients.
Methods: Our protocol begins with oral steroids, and serial evaluations. Indications for decompression and our unique transcanal approach to identify the sites for decompression are described. A retrospective review of the medical record presents our patients treated between 1998 and 2017.
Results: One hundred and forty one patients with grade 4 or more weakness underwent decompression. Mean pre-operative and post-operative House-Brackmann (HB) scores were HB5 and HB2, respectively. Fourteen of 104 patients (13%) presenting with HB5 and 6 still had HB5 or HB6 after decompression. Eighty-three of thee 104 patients (80%) achieved HB1 or HB2 at 6 months. Post-operative bone levels were unchanged. Post-operative air levels were improved in cases of perigeniculate fractures (84%).
Conclusion: This Bangalore protocol facilitates advantageous improvement in facial function and conductive hearing loss after traumatic facial nerve crush injuries. The surgical technique, albeit challenging, helps identify the fracture lines, facilitates reconstruction of disrupted ossicles, and avoids craniotomy.
Introduction
Facial nerve injury after temporal bone fracture usually involves the perigeniculate ganglion area (1, 2). Additional sites may be involved, leading some surgeons to suggest middle cranial fossa, transmastoid, or combined approaches to address those lesions (1–5). It has been noted, however, that the exact site(s) of injury can be difficult to delineate (1).
In Bangalore India, our Center commonly treats injuries after traffic collisions. Our evaluation protocol and surgical approach have served our patients well, in the absence of the access to electrodiagnostic testing. Our decision tree selects whom to explore, and our transcanal approach to the facial nerve exposes the labyrinthine portion of the nerve through the first genu and geniculate ganglion, tympanic segment, second genu, and mastoid segment. This approach enables the surgeon to follow the fracture course directly to the site of lesion, enables addressing the ossicles which are often disrupted in trauma, and avoids craniotomy.
Methods
IRB approval was obtained.
Patient Selection
Patients undergo physical examination, House-Brackmann (HB) grading (6), audiometry, CT scan and Schirmer's testing. No electrophysiologic testing is available at this time. Non-surgical treatment is initiated, and the patients' responses indicate who will likely benefit from surgery. In longitudinal fractures, the patients have hematorrhea, tympanic membrane rupture, or hemotympanum with conductive hearing loss. In transverse fractures, the patients have severe giddiness, vomiting, and sensorineural hearing loss. In the majority of cases, the lesion has been found to be around the perigeniculate ganglion area. We find that a positive Schirmer's test (lacrimation absent) in longitudinal fracture indicates probable involvement of the facial nerve proximal to the geniculate ganglion, involving the greater superficial petrosal nerve. If the patient presents with HB4, we proceed to decompression.
If the patient has less than grade 4 at the time of presentation, a trial of oral steroids in a tapering dosage along with physiotherapy is given. These patients are followed for 3 weeks and are then evaluated for improvement of facial function. Patients who achieve eye closure after 3 weeks will achieve complete or near-complete recovery of facial nerve function within 3 months, without surgical intervention. Patients with an initial HB3 who do not achieve eye closure at the end of 3 weeks of conservative management, will undergo surgical intervention. In our experience with this latter scenario, the earlier the intervention, the better will be the final outcome. Best results are achieved if intervention occurs between 3 weeks and 12 weeks. In palsies of 3–6 months', the procedure can be performed with guarded prognosis for improved facial nerve function.
Surgical Technique
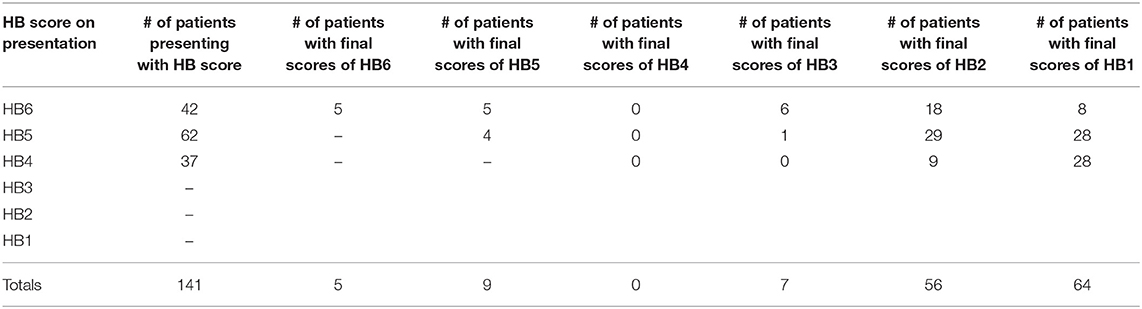
Patients are operated under local anesthesia with sedation or under general anesthesia in the pediatric age group. The mastoid cortex is exposed through a post-auricular incision. Through a transcanal approach, a 270° tympanomeatal flap is raised from 2 through 12 to 6 o'clock in the right ear, and from 10 through 12 to 6 o'clock in the left ear. A wide canalplasty, removing the posterior inferior canal wall, increases exposure while an atticotomy exposes the malleus head and incus body. The fracture lines usually extend from the squamous temporal bone along the posterior canal wall in stepwise fashion toward the middle ear. In most cases, this fracture line dislocates the incudo-malleolar joint and proceeds superior to the supralabyrinthine area—the site most commonly involved in longitudinal fractures. Occasionally, the fracture line can be seen extending over the incudo-stapedial joint, causing its dislocation. Tympanomeatal flap elevation and the boney removal from the canal and attic, allow identification of the destructive route of the fracture line (Figure 1).
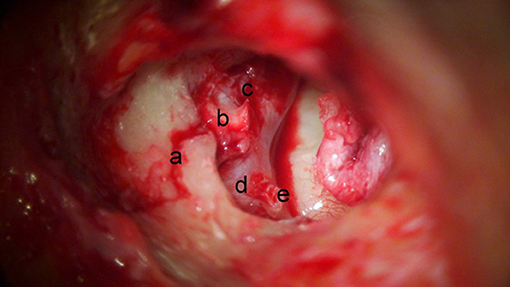
Figure 1. Destructive course of fracture line (right ear). The fracture (a) can be seen extending (b) over the geniculate ganglion, into the perigeniculate ganglion area (c). For orientation horizontal facial nerve (d) and stapes (e) are labeled.
The incudo-stapedial joint is disarticulated, and the incus is removed and preserved (As our results will later show, the majority of these fractures involve the peri-geniculate region which can be reached through the epitympanum, but not via a transmastoid approach. In addition, as our hearing outcomes will later show, the ossicles are already disrupted by the trauma in most of these peri-geniculate cases). The malleus head is amputated and the manubrium is retained with the tympanomeatal flap. The boney removal in the attic is further extended to expose the supralabyrinthine region. The cochleariform process is fractured to expose the geniculate ganglion beneath it (Figure 2). Fragments of the supralabyrinthine cells, which typically impinge into the perigeniculate ganglion area, are removed meticulously with the drill and variously sized curettes, to decompress the labyrinthine segment, first genu and greater superficial petrosal nerve (Figure 3). The route of the labyrinthine facial canal is slowly exposed using a small diamond burr, accessed either medial-anterior-superior or medial-anterior-inferior to the geniculate ganglion.
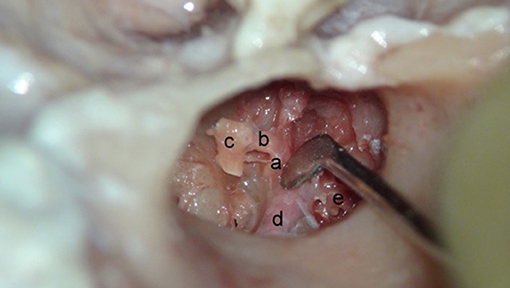
Figure 2. Visualization of the supralabyrinthine region with exposure of the geniculate ganglion (left ear—cadaver). Incus body and malleus head have been removed. The cochleariform process (a) is being down-fractured with the attached tensor tympani tendon (b) and manubrium (c). Horizontal facial nerve (d) and supralabyrinthine area (e) are seen.
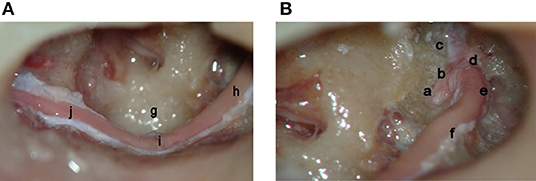
Figure 3. (A,B) Complete facial nerve decompression—labyrinthine meatus to stylomastoid foramen (left ear—cadaver). Seen are the meatal foramen (a), labyrinthine portion of the facial nerve (b), greater superficial petrosal nerve (c), the first genu (d), the geniculate ganglion (e), the horizontal segment of the facial nerve (superior image) (f), the sinus tympani (g), the horizontal facial nerve (inferior image) (h), the second genu (i), and the vertical segment out to the stylomastoid foramen (j).
In a majority of cases of temporal bone fractures, decompression of the labyrinthine segment, geniculate ganglion, greater superficial petrosal nerve, and horizontal facial nerve is sufficient to obtain good facial nerve recovery. In cases of multiple fracture lines or isolated fracture lines which involve other segments of the facial nerve, the nerve can be traced distally to the stylomastoid foramen using the same transcanal exposure (Figure 3). To obtain exposure of the vertical segment, the posterior canal wall is drilled under direct visualization by tracing the facial nerve from distal horizontal segment, downwards to stylomastoid foramen.
After the nerve is exposed and fracture fragments are removed, the epineurium is incised in all cases, using a tenotome. Primary ossicular reconstruction is performed in all cases. Pre- and post-operative air/bone conduction and HB scores (Figure 4) are documented.
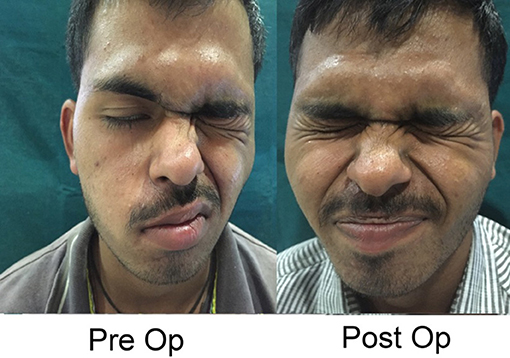
Figure 4. Typical post-decompression, 27 year old man. Pre-operative photograph is 30 days after longitudinal fracture. Post-operative photograph is 6 months after complete transcanal decompression. Permission for publication of these images for educational purposes given by patient and signed by patient and two witnesses, as well at the translator.
This surgical technique requires considerable otologic experience and very accurate anatomic knowledge of the location and course of the labyrinthine facial nerve medial to the geniculate ganglion.
Results
Table 1 tallies the raw HB scores of 141 patients with post-traumatic unilateral facial nerve weakness grade 4 or worse who underwent decompression from 1998 to 2017. Shown are the segment involved by fracture and their HB scores pre-operatively and 6 months post-operatively. Although bone fragments were removed from several the facial nerve sheathes, none of these 141 patients had a confirmed partial transection. We exclude the one patient from that time period who was found to have a completely transsected nerve.
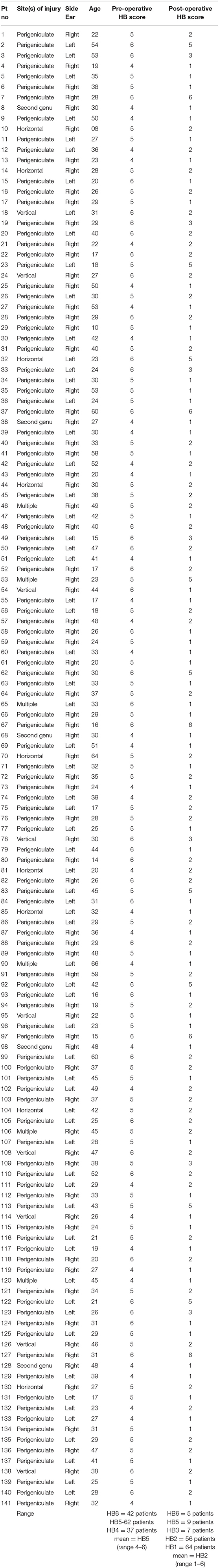
Table 1. One hundred forty-one patients with House-Brackmann (HB) grades HB6, HB5, and HB4 facial weakness after temporal bone fracture—sites of fracture and pre- vs. post- operative HB scores.
Sites of injury were: the perigeniculate area only (labyrinthine and greater superficial petrosal nerve and geniculate ganglion) = 112/141 (79%); the horizontal segment = 9/141 (6%); the vertical segment = 9/141 (6%); the second genu (5/141 = 4%), and multiple sites—a combination of perigeniculate area with either the second genu or vertical segment = 6/141 (4%). The perigeniculate area, therefore, was involved in 118/141 (84%) of fractures.
On Table 2 the mean (with SD) HB outcomes for patients whose facial function was HB6, HB5 and HB4 on presentation were HB2.79 (1.66), HB1.76 (1), and HB1.24 (0.44), respectively. Fourteen of the 141 (10%) patients showed HB6 or HB5 at 6 months. One hundred twenty of 141 (92%) showed HB2 or HB1 post-operative scores. Just considering the 104 patients with the worst presenting scores of HB6 and HB5: 14/104 (13%) had poor outcomes, and 83/104 (80%) had good outcomes.
The Analysis of Variance (ANOVA) test demonstrates that these post-operative HB scores differ between the patients whose facial function was HB6, HB5, and HB4 on presentation (f-statistic = 19.05 and p < 0.0001). The post-hoc Tukey Honestly Significant Difference (Tukey HSD) test, at α-level 0.05 distinguishes between these three presenting patient groups in detail: The outcomes for HB4 and HB5 are each better than the outcome for HB6 (p < 0.05), but do not differ from each other.
Table 3 reports average pre- and post-operative air and bone conduction levels parsed by site of injury/decompression. Post-operative bone levels were unchanged. The post-operative air levels were improved in cases of perigeniculate fractures and multiple fractures (perigeniculate plus another site), even after the ossicular disarticulation needed for the approach and the subsequent reconstruction.
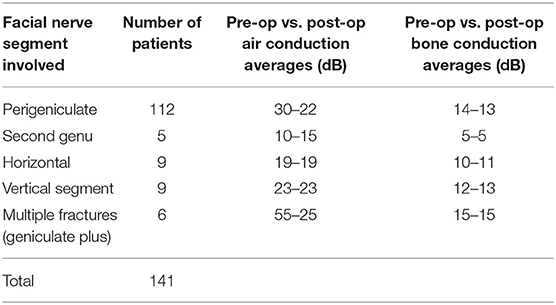
Table 3. Sites of injury vs. hearing improvement in 140 patients after facial nerve decompression with ossiculoplasty.
Discussion
Traffic collisions in Bangalore are a major cause of temporal bone fractures with facial nerve palsy. One hundred forty-one cases of traumatic facial nerve palsy with an intact nerve were decompressed at our center through transcanal approach from January 1998 to December 2017. We found our protocol as detailed in the Materials section to very useful both for evaluation and treatment. We do not use electrophysiologic testing, but we have found that the Schirmer's test helps identify injuries proximal to the greater superficial petrosal nerve. And we have found that failure to achieve eye closure at 3 weeks indicates that the patient's course will be better with surgical intervention.
The House-Brackman scale as modified in 1984 is the standard facial nerve instrument approved by the American Academy of Otolaryngology–Head and Neck Surgery, but presents limitations, nonetheless (7). Chief among these are inter-observer differences as well as the ambiguity of scoring secondary effects like synkinsis, contracture and spasm (7). Therefore, in summarizing the results of this series, to be as rigorous as possible, we count HB6 and HB5 outcomes together to find that 14/141 patients (10%) were left with substantial disfigurement after decompression. Considering only those patients with the worst prognoses: 14/104 patients (13%) presenting with HB6 or HB5 had poor outcomes. Similarly, combining HB2 and HB1 as good outcomes, we found that 120/141 patients (92%) had favorable post-operative outcomes. Or that 83/104 (80%) presenting with the worst prognoses—HB6 and HB5—had good outcomes. Statistical analysis found that patients presenting with HB6 had worse outcomes than those presenting with HB5 or HB4.
Comparison to summaries of the literature finds that these results seem slightly more encouraging than previously reported. Adgebite et al. (8) and Brodie and Thompson (9) disagree on the relative prognosis of immediate vs. delayed paralysis after temporal bone trauma. Outcomes as reported in the literature are further complicated by the tendency to combine HB2 and HB1 (9) as we have done here, or to combine HB2-HB5 together (10) as in a large meta-analysis of 35 patient series. With these confounding factors, along with the inter-observer problems with the HB scale, it seems that 0–50% of observation-only post-traumatic paralyzes (9, 10), 44% of steroid-treated paralysis (10), and 21% of decompressed (10) paralysis had HB1 outcomes; while 2, 0, and 10% of these three treatment options had HB6 outcomes (10). In our series 80% of the HB6 and HB5 patients ended with HB2 and HB1, while 13% of these most affected patients ended with HB6 or HB5. Unfortunately, we have no control group to compare the post-decompression results to. However, these results compare favorably to observation-only, the steroid, and the decompression reports in the literature above.
Our patient series shows that the perigeniculate area was involved in 84% of these 141 cases. This area can be reached via the middle cranial fossa. However, the transcanal technique, though technically challenging, gives access to the geniculate ganglion and the labyrinthine facial nerve without craniotomy. In addition, as the improvement in the air conduction scores demonstrates (Table 3), the disarticulation of the ossicles, with their subsequent reconstruction actually improves the post-operative hearing. Most cases have pre-existing disarticulation of the ossicles due to impact of trauma (As an aside, the middle cranial fossa approach affords no access to the ossicles which are often dislocated in temporal bone fracture). Another advantage of this technique is that the routes of the fracture line can be exactly delineated while the corresponding facial nerve pathology can be addressed. Therefore, the transcanal approach avoids a craniotomy, improves the hearing in more than 80% of the cases, and provides exact visualization.
The most frequent objection to this technique is the belief that the labyrinthine portion of the facial nerve cannot be accessed through this approach. Careful practice in the temporal bone laboratory using high magnification will demonstrate otherwise. One has to practice this technique by doing multiple temporal bone dissections before performing live surgeries.
Data Availability Statement
All datasets generated for this study are included in the manuscript/supplementary files.
Ethics Statement
The studies involving human participants were reviewed and approved by Vijaya ENT Care Center Ethics Board Committee. Written informed consent for participation was not provided by the participants' legal guardians/next of kin because: This is a review of medical records. As a review of medical records, it was reviewed and approved by the IRB committee. As far as the actual operations—parents and patients gave full informed consent for medical and surgical care. Also the sole facial photograph was obtained with explicit written consent for publication. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
VH assembled this post-traumatic facial nerve protocol from his decades of experience in Bangalore. VV assisted in patient management and together with NM assembled the data and prepared the tables. NM assembled the patient data, prepared the tables, and wrote the first draft of the introduction and materials and methods. MR wrote the final complete article, creating the presentation format commonly used for article submission.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to recognize the Indian Otology Society for its consistent efforts to promote scholarship on the Indian subcontinent.
References
1. Kong K, Sevy A. Temporal bone fracture requiring facial nerve decompression or repair. Oper Techniques Otolaryngol. (2017) 28:277–83. doi: 10.1016/j.otot.2017.08.014
2. Sun DQ, Andresen NS, Gantz BJ. Surgical management of acute facial palsy. Otolaryngol Clin North Am. (2018) 51:1077–92. doi: 10.1016/j.otc.2018.07.005
3. Cannon RB, Thomson RS, Shelton C, Gurgel RK. Long-term outcomes after middle fossa approach for traumatic facial nerve paralysis. Otol Neurotol. (2016) 6:799–804. doi: 10.1097/MAO.0000000000001033
4. Liu Y, Han J, Zhou X, Gao K, Luan D, Xie F, et al. Surgical management of facial paralysis resulting from temporal bone fractures. Acta Oto-Laryngol. (2014) 134:656–60. doi: 10.3109/00016489.2014.892214
5. Eby TL, Pollak A, Fisch U. Histopathology of the facial nerve after longitudinal temporal bone fracture. Laryngoscope. (1988) 98:717–20. doi: 10.1288/00005537-198807000-00005
6. House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. (1985) 93:146–7. doi: 10.1177/019459988509300202
7. Kang TS, Vrabec JT, Giddings N, Terris DJ. Facial nerve grading systems (1985–2002): beyond the House-Brackmann scale. Otol Neurotol. (2002) 23:767–71. doi: 10.1097/00129492-200209000-00026
8. Agdebite AB, Khan MI, Tan L. Predicting recovery of facial nerve function following injury from a basilar skull fracture. J Neurosurg. (1991) 75:759–62. doi: 10.3171/jns.1991.75.5.0759
9. Brodie HA, Thompson TC. Management of complications from 820 temporal bone fractures. Am J Otol. (1997) 18:188–97.
Keywords: facial nerve injury, facial nerve trauma, surgical decompression, facial paralysis, geniculate ganglion
Citation: Honnurappa V, Vijayendra VK, Mahajan N and Redleaf M (2019) Facial Nerve Decompression After Temporal Bone Fracture—The Bangalore Protocol. Front. Neurol. 10:1067. doi: 10.3389/fneur.2019.01067
Received: 18 July 2019; Accepted: 23 September 2019;
Published: 04 October 2019.
Edited by:
P. Ashley Wackym, Rutgers, The State University of New Jersey, United StatesReviewed by:
Ravi N. Samy, University of Cincinnati, United StatesAkira Ishiyama, University of California, Los Angeles, United States
Copyright © 2019 Honnurappa, Vijayendra, Mahajan and Redleaf. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Miriam Redleaf, bXJlZGxlYWYmI3gwMDA0MDt1aWMuZWR1
 Vijayendra Honnurappa1
Vijayendra Honnurappa1 Vinay Kumar Vijayendra
Vinay Kumar Vijayendra Miriam Redleaf
Miriam Redleaf