
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Neurol., 23 July 2019
Sec. Headache and Neurogenic Pain
Volume 10 - 2019 | https://doi.org/10.3389/fneur.2019.00785
This article is part of the Research TopicClinical and Pathophysiological Peculiarities of Headache in Children and AdolescentsView all 12 articles
 Pasquale Parisi1*
Pasquale Parisi1* Maria Chiara Paolino1
Maria Chiara Paolino1 Umberto Raucci2
Umberto Raucci2 Nicoletta Della Vecchia3
Nicoletta Della Vecchia3 Vincenzo Belcastro4
Vincenzo Belcastro4 Maria Pia Villa1
Maria Pia Villa1 Pasquale Striano5,6
Pasquale Striano5,6The relationship between headache and epilepsy is complex and despite the nature of this association is not yet clear. In the last few years, it has been progressively introduced the concept of the “ictal epileptic headache” that was included in the recently revised International Classification of Headaches Disorders 3rd edition (ICHD-3-revised). The diagnostic criteria for ictal epileptic headache (IEH) suggested in 2012 were quite restrictive thus leading to the underestimation of this phenomenon. However, these criteria have not yet been included into the ICHD-3 revision published in 2018, thus creating confusion among both, physicians and experts in this field. Here, we highlight the importance to strictly apply the original IEH criteria explaining the reasons through the analysis of the clinical, historical, epidemiological and pathophysiological characteristics of the IEH itself. In addition, we discuss the issues related to the neurophysiopathological link between headache and epilepsy as well as to the classification of these epileptic events as “autonomic seizure.”
Headache and epilepsy are characterized by transient attacks of altered brain function. The links between headache and epilepsy are complex and in the last century there have been several attempts to improve the classification, the clinical characterization, and the physiopathology of this association (1, 2).
In the 20th century, Sir W. R. Gowers, first suggested that “migraine is in the borderland of epilepsy” (2), sharing some pathophysiological mechanisms, presenting themselves as dysfunctions of neurotransmitters and ion channels. Indeed, these two conditions are common, often co-morbid, with headache attacks in epilepsy, temporally related as pre-ictal, ictal, post-ictal, or inter-ictal events. In addition, they can present with either visual, cognitive, sensorial and motor signs/symptoms (1, 2). Furthermore, the concept of “headache” as “an epileptic headache” that “… may even be the only clinical manifestation of idiopathic epilepsy” dates back from a long time ago. Already in the pre-EEG era, Gowers stated that “…in extremely rare instances one affection may develop while the other goes on,” (2). Nowadays, the availability of digital EEG recordings allow us to state that chronic headache itself may occasionally represent an epilepsy condition and that often headache can represent the only ictal epileptic phenomenon (i.e., ictal epileptic headache, IEH) (3–6).
The first description of IEH dates to the 1950s (7–10) but the term migralepsy was coined 10 years later by Lennox and Lennox (11) and become strongly rooted in the epileptological culture, hindering the verification and awareness among experts of the possible complete overlap of an epileptic seizure and a cephalalgic event. In fact, following the introduction of the migralepsy concept, an increasing number of ictal headaches have been described (12–15) and it has been hypothesized that the migralepsy sequence may not exist at all and that the initial part of the “migralepsy” may merely be an “ictal headache” followed by other ictal autonomic, sensory, motor or psychic signs/symptoms, being thus classified in fact as “hemicrania epileptica” (16).
Although the revised International Classification of Headaches Disorders 3rd edition (ICHD-3) now includes the term “ictal epileptic headache” (17), it does not take into account the original clinical criteria (3). Indeed, since the first demonstration (13) of the immediate remission of EEG abnormalities and of the headache after the administration of intravenous anti-epileptic drug, over than 30 cases of IEH have been reported (3–6, 12–16, 18–34). These papers suggest that a diagnosis of IEH is possible when all the following criteria occur (3): (a) headache lasting minutes, hours, or days, headache that is ipsilateral or contralateral (if the headache is not generalized) with epileptiform EEG discharges (if the anomalies are localized); (b) variable EEG abnormalities may be observed without a specific EEG or clinical headache pattern required; (c) headache and EEG abnormalities immediately resolved after antiepileptic drugs intravenous administration (Table 1).
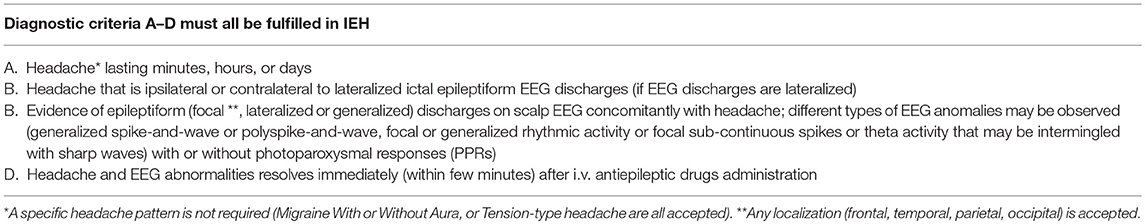
Table 1. Proposed original criteria for Ictal Epileptic Headache (IEH) [reproduce from Parisi et al. (3), with permission].
However, these criteria have not been fully taken into account into the recent revised ICHD-3 (17), thus creating confusion. However, we feel that even if the concomitant appearance of the EEG epileptiform discharges with headache is the mainstay criteria for the diagnosis of IEH, the prompt response to antiepileptic treatment is still crucial to confirm the clinical suspicion (34).
Coci and Riedel recently described two patients, with chronic headache unresponsive to analgesics therapy and disappeared after oral antiepileptic therapy (24). An ictal EEG recording in these adolescents during a headache attack revealed diffuse spike-wave and poly-spikes, and spontaneous drug withdrawal resulted in a recurrence of the headache, which resolved again on anticonvulsant therapy. These authors classified these cases as “probable IEH” due to the lack of clinical-EEG demonstration of the resolution of both the headache and EEG anomalies, after the administration of intravenous anticonvulsant therapy. Therefore, although an EEG recording may not be routinely recommended in children with headache, it should be performed promptly in patients with prolonged headache that do not respond to anti-migraine therapy (35–39), particularly in children with epilepsy that also express other types of seizures (34). Nevertheless, the use of clear-cut IEH criteria (3) will facilitate communication among clinicians and researchers, avoiding misdiagnoses, incorrect therapies, and eventually reducing health costs (40–52).
Several data support the view that increased neocortical excitability is the leading mechanism underlying headache and epilepsy (53). Taking into account that in migraine, during the “spreading depression,” hypo- and hyper-excitation occur, both (sequentially), as rebound phenomena, it could be suggested the term “dys-excitability” to better describe these physiopathologic events, rather than generically “hyperexcitability” (5, 6, 50, 54–57). Cortical Spreading Depression (CSD), that many Authors believe to be the most likely pathophysiological link between headache and epilepsy (5, 6, 36, 39, 40, 58, 59), is a slowly propagating wave of strong neuronal depolarization which induces fleeting (but intense) spike activity, followed by a neural suppression, lasting for minutes. The depolarization proceeds simultaneously with an increased regional cerebral blood flow, while the phase of reduced neural activity is associated with a decrease in brain perfusion. CSD starts the trigeminovascular system, provoking the release of many inflammatory molecules and neurotransmitters, responsible for the pain characterizing the headache phase (50, 60). Both, basic and clinical neurosciences findings, are in favor of “CSD” and “epileptic focus” as phenomenons able to facilitate reciprocally each other, although with different effectiveness and efficiency. The achievement of a minimum threshold necessary to start depolarization is the key to both phenomenas, but, the required threshold is presumed to be lower for CSD than for an epileptic discharge, the onset of both facilitating each other, anyway. This may explain why it is far more likely to observe an epileptic subject who also presents a peri-ictal headache than a cephalalgic patient who presents epilepsy (36, 40, 43, 50, 53, 57, 60). The two phenomena (CSD and epileptic seizure) possibly being triggered by more than one pathway converging upon the same destination: depolarization/dysexcitability (36, 40, 48, 50, 61).
The etiology could be environmental or individual (due genetic causes or not), originating a flow of ions that provokes CSD through neuronal and glial cytoplasmic bridges, rather than through interstitial ways as conversely occurs in the spreading of epileptic seizures (5, 50, 55, 56, 62).
Both migraine and epilepsy have an important genetic component, with strong evidence pointing to a shared genetic basis between headache and epilepsy emerging from clinical/EEG and genetic studies on Familial Hemiplegic Migraine (FHM) (63–69). Recent data suggest shared genetic substrates and phenotypic-genotypic correlations with mutations in some ion transporter genes, including CACNA1A, ATP1A2, and SCN1A (69–73). Other genetic findings pointing to a link between migraine and epilepsy have been published (74, 75). In addition, glutamate metabolism (76), serotonin metabolism (77), dopamine metabolism (78), and ion channel (sodium, potassium, and chloride) function might be impaired in both epilepsy and migraine (69, 79).
To clarify why headache could be the sole ictal epileptic manifestation, we (3, 5, 6, 34) previously hypothesized that an autonomic seizure remains purely autonomic if ictal neuronal activation of non-autonomic cortical areas does not achieve the symptomatogenic threshold (80). Accordingly, we suggested that IEH should be considered an autonomic form of epilepsy, like Panayiotopoulos syndrome, and, thus, people with long-lasting IEH attacks may even fulfill the criteria for autonomic status epilepticus (81). Although it is difficult to explain the reasons for which IEH remains an isolated manifestation lasting up to several hours or even days (13), one can speculate that the threshold for ictal autonomic manifestations could be lower from that required for motor-sensory areas, as observed for autonomic seizures in pediatric age (e.g., Panayiotopoulos syndrome).
In addition, while the presence of epileptiform abnormalities usually confirm the diagnosis of epilepsy, in IEH patients the lack of clear epileptic spike-and-wave activity does not rule out the diagnosis of epilepsy. The same diagnostic difficulties arise for patients with a deep epileptic focus arising, for example, from the orbito-mesial frontal zone (82). In such cases, ictal epileptic EEG activity may be recorded exclusively by means of deep stereo-EEG recording, even, sometimes, purely by chance (83).
Another crucial point is the lack of a clear, repetitive EEG headache-associated pattern, owing to the fact that the ictal EEG recording is usually not associated with specific EEG picture. Indeed, different EEG patterns have been recorded during headache-like complaints in both symptomatic and idiopathic IEH cases (18, 20, 28–34).
Moreover, when EEG abnormalities are recorded, no specific cortical correlations emerge (e.g., focal frontal, parietal, temporal, occipital and primary or secondary generalized), as reported (confirming, thus, our hypothesis) for autonomic manifestations in Panayiotopoulos syndrome.
Accordingly, we may interpret a headache as the sole expression of an epileptic seizure, supporting thus the autonomic nature of the IEH, at least in the most of the cases.
To understand the complexity of the pathways and networks involved in the onset and transmission of “primary headache” from the periphery (intracranial vessels) within the central nervous system until all potentially involved brain areas, you have to sum up the main stages of such nociceptive structures, fibers, pathways and such neuro-vascular structures. This careful examination can make evident why is so difficult, at moment, to classify the “Ictal Epileptic Headache” as “sensory” or “autonomic” seizure to propose a precise classification in the new Epilepsy classifications (84).
The cephalalgic attack originates as consequence of the activation of nociceptors innervating pial, arachnoid, and dural blood vessels, as well as large cortical arteries and sinuses. These structures are activated by mechanical, electrical or chemical stimulation (pro-inflammatory molecules, blood or infection), causing a painful perception similar to migraine and its most commonly associated symptoms/signs (nausea, throbbing pain, photophobia, and phonophobia).
The intracranial vessels and the meninges are innervated by unmyelinated fibers (C fibers) or thin little myelinated fibers (Ad fiber), which convey nociceptive sensitivity; these axonal terminations contain vasoactive neuropeptides such as substance P (SP) and the peptide related to the calcitonin gene (CGRP). They, originating from the trigeminal ganglion, reach the dura through the ophthalmic branch of the trigeminal nerve (V1) and, to a lesser extent, through the maxillary (V2) and mandibular branches (V3).
The dura is also innervated by neurons located in the ganglia of the upper cervical dorsal root. For decades, a possible vascular origin of headache pain has been debated. At present, the results of the various studies are conflicting and inconclusive, suggesting that vascular changes would not have a primary role, or at least, may not have a unique and predominant role in the pathophysiology of headache (85–87).
The mechanisms that explain the efficacy of the Vagus Nerve Stimulation (VNS) in the treatment of migraine and cluster headaches are not yet clear; probably, it is realized through a modulation of the intracranial trigeminal-vascular nociceptive transmission. Most of the fibers of the vagus nerve includes sensory afferents that terminate bilaterally in the nucleus tractus solitarius (NTS), before projecting into other nuclei, including the locus coeruleus (LC), the nucleus of the dorsal raphe (DRN), parabrachial nucleus, and PVN. It has been shown for the first time that VNS inhibits nociceptive activation of trigeminal-cervical neurons in preclinical models of acute dural-intracranial (migraine-like) and trigeminal-autonomic (cluster) pain (87).
The insula and other part of so-called Limbic System (part of frontal, temporal, and parietal regions which receive projections from autonomic networks), have a role in various processes including goal-directed cognition, conscious awareness, autonomic regulation, enteroception, and somatosensation. There are complex behaviors in migraine (conscious awareness and error detection), which are less investigated of other well-known, such as autonomic and somatosensory alterations during the clinical attacks. The insula processes and relays afferent inputs from brain areas involved in these functions, to areas involved in higher cortical function, such as frontal, temporal, and parietal regions. Insula role could be to decode the signals of altered internal milieu in migraine (along with other chronic pain conditions), taking into account the insula role in translating and integrating of multiple informations into complex behaviors (88).
It is also important to remember that, the activation of lateral and ventrolateral periacqueduttal gray (PAG) neurons by direct ascending lamina I e II projections (where make connection the afferent fibers C amyelinic which comes from cerebral vessels, as proposed for trigemino-vascular theory to explain physiopathology of migraine), produces non-selective, non-specific headache pain relief, cardiovascular reactions (decrease in blood pressure), homeostatic reactions (temperature changes), and defensive reactions (immobility, arousal, avoidance behavior, and vocalization), as well as a more general emotional state of fear and anxiety (89). Since the PAG undoubtedly projects a more dense fiber connections to the rostral ventromedial medulla (RVM), but minimally to the spinal and medullary dorsal horn, RVM neurons constitute a direct link for descending modulation through bilateral projections to all levels of spinal and medullary dorsal horns. These functional and anatomical studies are consistent with a broader modulatory role of the PAG–RVM circuit and suggest an “absence of specificity” for headache.
IEH does not have a specific clinical picture of headache/migraine (migraine without aura or tension-type headache or aspecific headache patterns, have all been reported), and it can last from seconds to days, with evidence of synchronous ictal epileptiform EEG anomalies; different EEG patterns may be observed, with or without a photoparoxysmal response (see Table 1). In fact, in particular, the ictal EEG recording in most patients does not yield a particular EEG pattern or specific cortical topographic correlations (focal frontal, parietal, temporal, occipital, and focal with primary or secondary generalization, have all been reported). EEG recording is not recommended routinely in children with headache but should be considered promptly in case of prolonged migraine/headache not responsive to antimigraine drugs. If the main IEH criterion (EEG-clinical response to antiepileptic intravenous administration) is not satisfied, we can just pose a “probable IEH” diagnosis. The concept of migralepsy is potentially confusing and should not be used to describe the sequence of visual aura-seizure and an ictal EEG recording is mandatory in these patients to exclude an “hemicrania epileptica” (16).
PP, MP, and PS formulated original idea and the design of the review and wrote the first draft of the manuscript. ND, UR, VB, and MV approved the design and final version of the manuscript. All authors reviewed, approved, and agreed to be accountable for all aspects of the work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Rajapakse T, Buchhalter J. The borderland of migraine and epilepsy in children. Headache. (2016) 56:1071–80. doi: 10.1111/head.12827
2. Gowers WR. The border-land of epilepsy. In: Arts & Boeve Nijmegen, Chapter V. Philadelphia, PA: P. Blakistons' Son & Co. (1995). p. 76–102.
3. Parisi P, Striano P, Kasteleijn-Nolst Trenite DGA, Verrotti A, Martelletti P, Villa MP, et al. Ictal epileptic headache”: recent concepts for new classifications criteria. Cephalalgia. (2012) 32:723–4. doi: 10.1177/0333102412447536
4. Verrotti A, Coppola G, Spalice A, Di FonzoA, Bruschi R, Tozzi E, et al. Peri-ictal and inter-ictal headache in children and adolescents with idiopathic epilepsy: a multicenter cross-sectional study. Childs Nerv Syst. (2011) 27:1419–23. doi: 10.1007/s00381-011-1428-7
5. Parisi P, Striano P, Negro A, Martelletti P, Belcastro V. Ictal epileptic headache: an old story with courses and appeals. J Headache Pain. (2012) 13:607–13. doi: 10.1007/s10194-012-0485-y
6. Parisi P, Striano P, Verrotti A, Villa MP, Belcastro V. What have we learned about ictal epileptic headache? A review of well-documented cases. Seizure. (2013) 22:253–8. doi: 10.1016/j.seizure.2013.01.013
7. Heyck H, Hess R. Vasomotoric headaches as symptom of masked epilepsy. Schweiz Med Wochenschr. (1955) 85:573–5.
8. Nymgard K. Epileptic headache. Acta Psych Neurol Scand Suppl. (1956) 108:291–300. doi: 10.1111/j.1600-0447.1956.tb01693.x
9. Lugaresi E. EEG investigations in monosymptomatic headache in infants. Riv Neurol. (1955) 25:582–8.
10. Morocutti C, Vizioli R. Episodes of paroxysmal headache as the only clinical manifestation of idiopathic epilepsy. Riv Neurol. (1957) 27:427–30.
12. Parisi P, Kasteleijn-Nolst Trenite DGA. “Migralepsy”: a call for revision of the definition. Epilepsia. (2010) 51:932–3. doi: 10.1111/j.1528-1167.2009.02407.x
13. Parisi P, Kasteleijn-Nolst Trenité DGA, Piccioli M, Pelliccia A, Luchetti A, Buttinelli C, et al. A case with atypical childhood occipital epilepsy “Gastaut type”: an ictal migraine manifestation with a good response to intravenous diazepam. Epilepsia. (2007) 48:2181–6. doi: 10.1111/j.1528-1167.2007.01265.x
14. Belcastro V, Striano P, Kasteleijn-NolstTrenite DGA, Villa MP, Parisi P. Migralepsy, hemicraniaepileptica, post-ictal headache and “ictal epileptic headache”: a proposal for terminology and classification revision. J Headache Pain. (2011) 12:289–94. doi: 10.1007/s10194-011-0318-4
15. Parisi P, Piccioli M, de Sneeuw S, de Kovel C, van Nieuwenhuizen O, Buttinelli C, et al. Redefining headache diagnostic criteria as epileptic manifestation? Cephalalgia. (2008) 28:408–9. doi: 10.1111/j.1468-2982.2008.01529_1.x
16. Parisi P, Belcastro V, Verrotti A, Striano P, Kasteleijn-Nolst Trenitè DGA. “Ictal epileptic headache” and the revised International Headache Classification (ICHD-3) published in Cephalalgia 2018, vol. 38, 1–211: Not just a matter of definition! Epilepsy Behav. (2018) 87:243–5. doi: 10.1016/j.yebeh.2018.07.018
17. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. (2018) 38:1–211.
18. Grossman RM, Abramovich I, Lefebvre AB. Epileptic headache: report of a case with EEG recorded during the crisis. Arq Neuropsiquiatr. (1971) 29:198–206. doi: 10.1590/S0004-282X1971000200008
19. Piccioli M, Parisi P, Tisei P, Villa MP, Buttinelli C, Kasteleijn-Nolst Trenité DGA. Ictal headache and visual sensitivity. Cephalalgia. (2009) 29:194–203. doi: 10.1111/j.1468-2982.2008.01707.x
20. Fanella M, Fattouch J, Casciato S, Lapenta L, Morano A, Egeo G, et al. Ictal epileptic headache as “subtle” symptom in generalized idiopathic epilepsy. Epilepsia. (2012) 53:e67–70. doi: 10.1111/j.1528-1167.2011.03387.x
21. Saitowitz Z, Flamini R, Berenson F. Ictal epileptic headache: a review of current literature and differentiation from migralepsy and other epilepsies. Headache. (2014) 54:1534–40. doi: 10.1111/head.12432
22. Fanella M, Morano A, Fattouch J, Albini M, Casciato S, Manfredi M, et al. Ictal epileptic headache revealing non convulsive status epilepticus in a case of eyelid myoclonia with absences. J Headache Pain. (2015) 16:105. doi: 10.1186/s10194-015-0587-4
23. Fanella M, Morano A, Fattouch J, Albini M, Manfredi M, Giallonardo AT, et al. Ictal epileptic headache in adult life: electroclinical patterns and spectrum of related syndromes. Epilepsy Behav. (2015) 53:161–5. doi: 10.1016/j.yebeh.2015.10.018
24. Coci EG, Riedel J. Exploring two novel cases of suspected ictal epileptic headache, a rare form of paediatric epilepsy. Acta Paediatr. (2017) 106:786–90. doi: 10.1111/apa.13713
25. Fanella M, Morano A, Fattouch J, Albini M, Basili LM, Casciato S, et al. Ictal epileptic headache in occipital symptomatic epilepsy: not only a matter of cortex. Headache. (2017) 57:956–61. doi: 10.1111/head.13014
26. Bae SY, Lee BI, Kim SE, Shin KJ, Ha SY, Park J, et al. Ictal epileptic headache in an elderly patient with a hippocampal tumor. J Clin Neurol. (2018) 14:120–2. doi: 10.3988/jcn.2018.14.1.120
27. Striano P, Belcastro V, Parisi P. Perucca P, Terzaghi M, Manni R. Status epilepticus migrainosus: clinical, electrophysiologic, and imaging characteristics. Neurology. (2011) 76:761. doi: 10.1212/WNL.0b013e3182068e56
28. Belcastro V, Striano P, Pierguidi L, Calabresi P, Tambasco N. Ictal epileptic headache mimicking status migrainosus: EEG and DWI-MRI findings. Headache. (2011) 51:160–2. doi: 10.1111/j.1526-4610.2010.01709.x
29. Cianchetti C, Pruna D, Porcu L, Peltz MT, Ledda MG. Pure epileptic headache and related manifestations: a video-EEG report and discussion of terminology. Epileptic Disord. (2013) 15:84–92.
30. Ghofrani M, Mahvelati F, Tonekaboni H. Headache as a sole manifestation in nonconvulsive status epilepticus. J Child Neurol. (2006) 21:981–3. doi: 10.1177/08830738060210111801
31. Fusco L, Specchio N, Ciofetta G, Longo D, Trivisano M, Vigevano F. Migraine triggered by epileptic discharges in a Rasmussen's encephalitis patient after surgery. Brain Dev. (2011) 33:597–600. doi: 10.1016/j.braindev.2010.09.014
32. Isler H, Wieser HG, Egli M. Hemicrania epileptica: synchronous ipsilateral ictal headachewith migraine features. In: Andermann F, Lugaresi E, editors. Migraine and Epilepsy. Boston: Butterworth Publishers (1987). p. 249–63.
33. Italiano D, Grugno R, Calabro‘ RS, Bramanti P, Di Maria F, Ferlazzo E. Recurrent occipital seizures misdiagnosed as status migrainosus. Epileptic Disord. (2011) 13:197–201.
34. Parisi P, Verrotti A, Costa P, Striano P, Zanus C, Carrozzi M, et al. Diagnostic criteria currently proposed for “ictal epileptic headache”: perspectives on strengths, weaknesses and pitfalls. Seizure. (2015) 31:56–63. doi: 10.1016/j.seizure.2015.07.005
35. Parisi P. Who's still afraid of the link between headache and epilepsy? Some reactions to and reflections on the article by Marte Helene Bjørk and co-workers. J Headache Pain. (2009) 10:327–329. doi: 10.1007/s10194-009-0149-8
36. Parisi P. Why is migraine rarely, and not usually, the sole ictal epileptic manifestation? Seizure. (2009) 18:309–12. doi: 10.1016/j.seizure.2009.01.010
37. Belcastro V, Striano P, Parisi P. Seizure or migraine? The eternal dilemma. Comment on: “recurrent occipital seizures misdiagnosed as status migrainosus”. Epileptic Disord. (2011) 13:456.
38. Verrotti A, Striano P, Belcastro C, Matricardi S, Villa MP, Parisi P. Migralepsy and related conditions: advances in pathophysiology and classification. Seizure. (2011) 20:271–5. doi: 10.1016/j.seizure.2011.02.012
39. Parisi P, Striano P, Belcastro V. The crossover between headache and epilepsy. Expert Rev Neurother. (2013) 13:231–3. doi: 10.1586/ern.13.16
40. Parisi P, Piccioli M, Villa MP, Buttinelli C, Kasteleijn-NolstTrenéte DGA. Hypothesis on neurophysiopathological mechanisms linking epilepsy and headache. Med Hypotheses. (2008) 70:1150–4. doi: 10.1016/j.mehy.2007.11.013
41. Kasteleijn-Nolst Trenite DGA, Cantonetti L, Parisi P. Chapter 97: Visual stimuli, photosensitivity and photosensitive epilepsy. In: Shorvon SD, Andermann F, Guerrini F, editors. The Causes of Epilepsy. Common and Uncommon Causes in Adults and Children. New York, NY: Cambridge University Press; Cambridge Medicine (2011). p. 687–94.
42. Parisi P. Comments on the article by Fusco L. et al. entitled “Migraine triggered by epileptic discharges in a Rasmussen's encephalitis patient after surgery”. Brain Dev. (2011) 33:704–705. doi: 10.1016/j.braindev.2011.03.008
43. Verrotti A, Coppola G, Di Fonzo A, Tozzi E, Spalice A, Aloisi P, et al. Should “migralepsy” be considered an obsolete concept? A multicenter retrospective clinical/EEG study and review of the literature. Epilepsy Behav. (2011) 21:52–9. doi: 10.1016/j.yebeh.2011.03.004
44. Striano P, Belcastro V, Parisi P. From “migralepsy” to “ictal epileptic headache” concept. Epilepsy Behav. (2012) 23:392. doi: 10.1016/j.yebeh.2011.12.004
45. Belcastro V, Striano P, Parisi P. “Ictal epileptic headache”: beyond the epidemiological evidence. Epilepsy Behav. (2012) 25:9–10. doi: 10.1016/j.yebeh.2012.07.002
46. Papetti L, Nicita F, Parisi P, Spalice A, Villa MP, Kasteleijn-NolstTrenitè DGA. “Headache and epilepsy” how are they connected? Epilepsy Behav. (2013) 26:386–93. doi: 10.1016/j.yebeh.2012.09.025
47. Parisi P, Striano P, Belcastro V. New terminology for headache/migraine as the sole ictal epileptic manifestation: the downsides. Reply to Cianchetti et al. Seizure. (2013) 22:798–799. doi: 10.1016/j.seizure.2013.07.015
48. Belcastro V, Striano P, Parisi P. Migraine and epilepsy terminology and classification: opening Pandora's box. Epileptic Disord. (2013) 15:216–7.
49. Belcastro V, Striano P, Parisi P. From migralepsy to ictal epileptic headache: the story so far. Neurol Sci. (2013) 34:1805–7. doi: 10.1007/s10072-012-1012-2
50. Parisi P. The complex relationship between epilepsy and headache and the concept of ictal epileptic headache. In: Striano P, editor. Epilepsy Towards the Next Decade. Contemporary Clinical Neuroscience. Cham: Springer International Publication (2015). p. 139-62. doi: 10.1007/978-3-319-12283-0_8
51. Belcastro V, Striano P, Parisi P. Is it migralepsy? Still don't know. Headache. (2015) 55:1446–7. doi: 10.1111/head.12696
52. Parisi P, Striano P, Verrotti A, Belcastro V. “Ictal epileptic headache” is certainly a seizure which manifests itself only as headache. Seizure. (2016) 38:77. doi: 10.1016/j.seizure.2016.04.001
53. Berger M, Speckmann EJ, Pape HC, Gorji A. Spreading depression enhances human neocortical excitability in vitro. Cephalalgia. (2008) 28:558–562. doi: 10.1111/j.1468-2982.2008.01556.x
54. Somjen GG. Mechanisms of spreading depression and hypoxic spreading depression-like depolarization. Physiol Rev. (2001) 81:1065–96. doi: 10.1152/physrev.2001.81.3.1065
55. Tottene A, Conti R, Fabbro A, Vecchia D, Shapovalova M, Santello M, et al. Enhanced excitatory transmission at cortical synapses as the basis for facilitated spreading depression in Ca(v)2.1 knockin migraine mice. Neuron. (2009) 61:762–73. doi: 10.1016/j.neuron.2009.01.027
56. Tottene A, Urbani A, Pietrobon D. Role of different voltage-gated Ca2+ channels in cortical spreading depression. Channels. (2011) 5:110–4. doi: 10.4161/chan.5.2.14149
57. Fabricius M, Fuhr S, Willumsen L, Dreier JP, Bhatia R, Boutelle MG, et al. Association of seizures with cortical spreading depression and peri-infarct depolarisations in the acutely injured human brain. Clin Neurophysiol. (2008) 119:1973–84. doi: 10.1016/j.clinph.2008.05.025
58. Moskowitz MA, Nozaki K, Kraig RP. Neocortical spreading depression provokes the expression of C-fos proteinlike immunoreactivity within trigeminal nucleus caudalis via trigeminovascular mechanisms. J Neurosci. (1993) 13:1167–77. doi: 10.1523/JNEUROSCI.13-03-01167.1993
59. Bolay H, Reuter U, Dunn AK, Huang Z, Boas DA, Moskowitz MA. Intrinsic brain activity triggers trigeminal meningeal afferents in migraine model. Nat Med. (2002) 8:136–42. doi: 10.1038/nm0202-136
60. Zhang X, Levy D, Kainz V, Noseda R, Jakubowski M, Burstein R. Activation of central trigeminovascular neurons by cortical spreading depression. Ann Neurol. (2011) 69:855–65. doi: 10.1002/ana.22329
61. Ghadiri MK, Kozian M, Ghaffarian N, Stummer W, Kazemi H, Speckmann EJ, et al. Sequential changes in neuronal activity in single neocortical neuron after spreading depression. Cephalalgia. (2012) 32:116–24. doi: 10.1177/0333102411431308
62. Gigout S, Louvel J, Kawasaki H, D'Antuono M, Armand V, Kurcewicz I, et al. Effects of gap junction blockers on human neocortical synchronization. Neurobiol Dis. (2006) 22:496–508. doi: 10.1016/j.nbd.2005.12.011
63. Haglund MM, Schwartzkroin PA. Role of Na-K pump potassium regulation and IPSPs in seizures and spreading depression in immature rabbit hippocampal slices. J Neurophysiol. (1990) 63:225–39. doi: 10.1152/jn.1990.63.2.225
64. De Fusco M, Marconi R, Silvestri L, Atorino L, Rampoldi L, Morgante L, et al. Haploinsufficiency of ATP1A2 encoding the Na+/K+ pump a2 subunit associated with familial hemiplegic migraine type 2. Nat Genet. (2003) 33:192–6. doi: 10.1038/ng1081
65. De Vries B, Frants RR, Ferrari MD, van den MAM. Molecular genetics of migraine. Hum Genet. (2009) 126:115–32. doi: 10.1007/s00439-009-0684-z
66. Gambardella A, Marini C. Clinical spectrum of SCN1A mutations. Epilepsia. (2009) 50:20–3. doi: 10.1111/j.1528-1167.2009.02115.x
67. Kors EE, Melberg A, Vanmolkot KR, Kumlien E, Haan J, Raininko R, et al. Childhood epilepsy, familial hemiplegic migraine, cerebellar ataxia, and a new CACNA1A mutation. Neurology. (2004) 63:1136–7. doi: 10.1212/01.WNL.0000138571.48593.FC
68. Wendorff J, Juchniewicz B. Photosensitivity in children with idiopathic headaches. Neurol Neurochir (2005) 39(4 Suppl. 1):S9–16.
69. Pietrobon D. Biological science of headache channels. Handb Clin Neurol. (2010) 97:73–83. doi: 10.1016/S0072-9752(10)97005-X
70. Riant F, Ducros A, Ploton C, Banbance C, Depienne C, Tournie-Lasserve E. De novo mutations in ATP1A2 and CACNA1A are frequent in early-onset sporadic hemiplegic migraine. Neurology. (2010) 75:967–72. doi: 10.1212/WNL.0b013e3181f25e8f
71. Uchitel OD, Inchauspe CG, Urbano FJ, Di Guilmi MN. Ca(V)2.1 voltage activated calcium channels and synaptic transmission in familial hemiplegic migraine pathogenesis. J Physiol. (2012) 106:12–22. doi: 10.1016/j.jphysparis.2011.10.004
72. Van Den Maagdenberg AM, Terwindt GM, Haan J, Frants RR, Ferrari MD. Genetics of headaches. Handb Clin Neurol. (2010) 97:85–97. doi: 10.1016/S0072-9752(10)97006-1
73. Vanmolkot KR, Kors EE, Hottenga JJ, Terwindt GM, Haan JJ, Hoefnagels WA. Novel mutations in the Na+/K+-ATPase pump gene ATP1A2 associated with familial hemiplegic migraine and benign familial infantile convulsions. Ann Neurol. (2003) 54:360–6. doi: 10.1002/ana.10674
74. Lonnqvist T, Paeteau A, Valanne L, Pihko H. Recessive twinkle mutations cause severe epileptic encephalopathy. Brain. (2009) 132:1553–62. doi: 10.1093/brain/awp045
75. Tzoulis C, Engelsen BA, Telstad W, Aasly J, Zeviani M, Winterthun S, et al. The spectrum of clinical disease caused by the A467Tand W748S POLG mutations: a study of 26 causes. Brain. (2006) 129:1685–92. doi: 10.1093/brain/awl097
76. Jen JC, Wan J, Palos TP. Mutations in the glutamate transporter EAAT1 causes episodic ataxia, hemiplegia, and seizures. Neurology. (2005) 65:529–34. doi: 10.1212/01.WNL.0000172638.58172.5a
77. Johnson MP, Griffiths LR. A genetic analysis of serotonergic biosynthetic and metabolic enzymes in migraine using a DNA pooling approach. J Hum Genet. (2005) 50:607–10. doi: 10.1007/s10038-005-0301-5
78. Chen SC. Epilepsy and migraine: the dopamine hypotheses. Med Hypotheses. (2006) 66:466–72. doi: 10.1016/j.mehy.2005.09.045
79. Steinlein OK. Genetic mechanisms that underlie epilepsy. Nat Rev Neurosci. (2004) 5:400–8. doi: 10.1038/nrn1388
80. Koutroumanidis M. Panayiotopoulos syndrome: an important electroclinical example of benign childhood system epilepsy. Epilepsia. (2007) 48:1044–53. doi: 10.1111/j.1528-1167.2007.01096.x
81. Ferrie CD, Caraballo R, Covanis A, Demirbilek V, Dervent A, Fejerman N, et al. Autonomic status epilepticus in Panayiotopoulos syndrome and other childhood and adult epilepsies: a consensus view. Epilepsia. (2007) 48:1165–72. doi: 10.1111/j.1528-1167.2007.01087.x
82. Nobili L. Nocturnal frontal lobe epilepsy and non-rapid eye movement sleep parasomnias: differences and similarities. Sleep Med Rev. (2007) 11:251–4. doi: 10.1016/j.smrv.2007.03.009
83. Laplante P, Saint-Hilaire JM, Bouvier G. Headache as an epileptic manifestation. Neurology. (1983) 33:1493–5. doi: 10.1212/WNL.33.11.1493
84. Scheffer IE, Berkovic S, Capovilla G, Connolly MB, French J, Guilhoto L, et al. ILAE classification of the epilepsies: position paper of the ILAE Commission for Classification and Terminology. Epilepsia. (2017) 58:512–21. doi: 10.1111/epi.13709
85. Amin FM, Asghar MS, Hougaard A, Hansen AE, Larsen VA, de Koning PJ, et al. Magnetic resonance angiography of intracranial and extracranial arteries in patients with spontaneous migraine without aura: a cross-sectional study. Lancet Neurol. (2013) 12:454–61. doi: 10.1016/S1474-4422(13)70067-X
86. Asghar M, Hansen AE, Amin FM, van der Geest RJ, Koning Pv, Larsson HB, et al. Evidence for a vascular factor in migraine. Ann Neurol. (2011) 69:635–45. doi: 10.1002/ana.22292
87. Akerman S, Simon B, Romero-Reyes M. Vagus nerve stimulation suppresses acute noxious activation of trigeminocervical neurons in animal models of primary headache. Neurobiol Dis. (2017) 102:96–104. doi: 10.1016/j.nbd.2017.03.004
88. Borsook D, Veggeberg R, Erpelding N, Borra R, Linnman C, Burstein R, et al. The insula: a “hub of activity” in migraine. Neuroscientist. (2016) 22:632–52. doi: 10.1177/1073858415601369
Keywords: ictal epileptic headache, hemicrania epileptica, epilepsy, migraine, tension-type headache, EEG, autonomic seizures, panayiotopoulos syndrome
Citation: Parisi P, Paolino MC, Raucci U, Della Vecchia N, Belcastro V, Villa MP and Striano P (2019) Ictal Epileptic Headache: When Terminology Is Not a Moot Question. Front. Neurol. 10:785. doi: 10.3389/fneur.2019.00785
Received: 22 December 2018; Accepted: 08 July 2019;
Published: 23 July 2019.
Edited by:
Massimiliano Valeriani, Bambino Gesù Children Hospital (IRCCS), ItalyReviewed by:
Andrea Nistri, Scuola Internazionale Superiore di Studi Avanzati (SISSA), ItalyCopyright © 2019 Parisi, Paolino, Raucci, Della Vecchia, Belcastro, Villa and Striano. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pasquale Parisi, cGFzcXVhbGUucGFyaXNpQHVuaXJvbWExLml0; cGFycGFzQGlvbC5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.