- Department of Neurology, Wake Forest School of Medicine, Winston-Salem, NC, United States
There are five sites at which radial nerve entrapment at the elbow has been commonly reported. These include the level of the fibrous bands within the extensor carpi radialis brevis, the thickened fascial tissue at the radiocapitellar joint, the leash of Henry, the arcade of Frohse, and the distal border of the supinator muscle. This review describes the anatomy of the radial nerve at the elbow and the surrounding structures, and then provides an overview of the literature supporting the use of ultrasound to assist in the evaluation of suspected radial neuropathy at the elbow. This review concludes with a suggested ultrasonographic approach for the systematic evaluation of suspected radial neuropathy at the elbow.
Introduction
The radial nerve is one of the major nerves of the upper extremity and one of the main branches of the brachial plexus. It innervates a number of muscles responsible for extending the elbow, wrist, and fingers and transmits sensation from the posterior surface of the arm, forearm, and hand. There are several sites around the elbow at which the radial nerve can be compressed, and the site of compression determines the clinical syndrome. Some of these named syndromes are controversial and overlap with each other. We prefer the broader and encompassing term, “radial neuropathy at the elbow,” and will use this term throughout this article unless it is clear that compression is at a discrete site in a specific case (such as the arcade of Frohse).
The overall goal of this article is to define the anatomy of the radial nerve at the elbow, clarify the potential sites of radial nerve compression at the elbow, describe the studies involving ultrasound of the radial nerve at this site, and outline a clinical neuromuscular ultrasound approach for evaluation of radial neuropathy at the elbow.
Radial Nerve Anatomy
The radial nerve (which includes C5 to T1 nerve roots) is a terminal branch of the posterior cord of the brachial plexus, and it carries motor and sensory nerve fibers. The radial nerve arises in the axilla, posterior to the axillary artery. It enters the posterior compartment of the arm under the teres major muscle. Branches of the radial nerve innervate the long and lateral heads of the triceps brachii. The radial nerve travels over the shallow groove of the humerus (spiral groove) with the deep brachial artery. It wraps around the humerus laterally and branches off to supply the medial head of triceps brachii. The radial nerve travels between the brachialis and brachioradialis muscles anterior to the lateral epicondyle to innervate the brachioradialis and extensor carpi radialis longus muscles.
The radial nerve then travels distally into the forearm through the cubital fossa, a triangular region defined by the epicondyles superiorly, the pronator teres medially, and the brachioradialis laterally. It divides into two terminal branches, the superficial sensory branch and the deep motor branch.
The deep motor branch travels into the radial tunnel, a space spanning from the radiocapitellar joint to the distal edge of the superficial supinator muscle (1).
The tunnel is defined laterally by the mobile wad of Henry [brachioradialis, extensor carpi radialis longus, and extensor carpi radialis brevis (ECRB) muscles] and medially by the biceps tendons and brachialis. The tunnel is superficially bound by the radial recurrent vessels (leash of Henry), the superficial head of the supinator muscle, and the brachioradialis muscle. The capsule of the radiocapitellar joint and the deep head of the supinator muscle form the floor of the radial tunnel. The deep motor branch enters the radial tunnel underneath the fibrous bands of the extensor muscles in the forearm at the level of the radial head. It crosses the leash of Henry at the radial neck and beneath the tendinous margin of the ECRB. The deep motor branch innervates the ECRB and supinator. Lastly, the nerve exits the radial tunnel beneath the aponeurotic margin between the superficial and deep layers of the supinator muscle as the posterior interosseous nerve (PIN). The PIN travels distally along the interosseous membrane between the radius and ulna, supplying all the extensor muscles on the dorsal surface of the forearm, except the anconeus, brachioradialis, and extensor carpi radialis longus (which are innervated by the radial nerve proper).
The superficial sensory branch of the radial nerve travels laterally with the radial artery and beneath the brachioradialis. Once it passes between the tendons of the brachioradialis and extensor carpi radialis longus, the superficial branch pierces the fascia and divides into two branches to supply sensory innervation to the posterior skin of the lateral three and a half digits.
Radial Neuropathies at the Elbow
There are two ways in which radial neuropathy at the elbow can be conceptualized. The first is based on the anatomic location of the lesion within the radial nerve, which is discussed below. The second is based on the clinical syndrome, which are presented in Table 1.

Table 1. This table includes the named clinical syndromes that arise from radial mononeuropathies at the elbow.
The first location of potential radial mononeuropathy at the elbow is the floor of the radial tunnel, which is the fascial tissue of the radiocapitellar joint. Thickening of this tissue can induce entrapment of the radial nerve (2). Compression can also occur due to osteoarthritis or synovitis of the radiocapitellar joint (1). The second location is within the radial tunnel caused by hypertrophic crossing branches of the leash of Henry (3). The third location is the proximal and medial edge of the ECRB. The proximal tendinous arch of the ECRB and the aponeurosis of the undersurface of the ECRB are both suspected to contribute to possible radial nerve compression at this site (4). The fourth location (and likely the most common entrapment location) is the aponeurotic margin between the superficial and deep layers of the supinator muscle, often referred to as the arcade of Frohse (5). The fifth described location of radial entrapment neuropathy at the elbow is at the distal border of the supinator muscles. Compression at this site is intermittent due to pressure from the distal edge of the radial head (1).
Ultrasound for Radial Neuropathies at the Elbow
Neuromuscular ultrasound has been used to localize and visualize lesion sites, classify severity, and detect potential causes of mononeuropathies (6, 7). Measurement of nerve cross-sectional area with ultrasound is an accurate parameter for the diagnosis of carpal tunnel syndrome (8) and has been shown to significantly increase diagnostic sensitivity in ulnar neuropathy at the elbow when combined with electrodiagnosis (9). For the less frequently studied radial neuropathies at the elbow, neuromuscular ultrasound has shown benefit in case reports and series.
Neuromuscular ultrasound was used to establish reference ranges of cross-sectional area of the radial nerve at the antecubital fossa, which range between 4.5 mm2 and 14.3 mm2 (10). While the cross-sectional area is the preferred method for measuring nerve size, early studies reported results in nerve diameter, with the deep branch of the radial nerve ranging between 1.30 mm and 2.13 mm (11). Based on reference ranges of the radial nerve, neuromuscular ultrasound case reports and series have consistently identified nerve enlargement in radial neuropathies at the elbow in comparison to the contralateral arm and healthy controls (11–17). Additional characteristic ultrasound findings of an injured nerve that may assist in localization include decreased echogenicity, enlarged nerve fascicles, and increased nerve vascularity (13, 18–20). Given the variability in reported reference values, side-to-side ultrasonographic comparison of nerve cross-sectional area is often helpful in suspected unilateral cases of radial neuropathy at the elbow.
The ability to distinguish nerve from surrounding tissues (21) and demonstrate nerve morphology and dimensions (22) allow ultrasound to provide insight when electrodiagnostic studies are not conclusive, and ultrasound can also assist in identifying the underlying etiology (19, 23, 24). Electrophysiologic studies can define the severity of an entrapment injury, but often cannot identify the underlying cause of the mononeuropathy because they do not typically assess the surrounding structures. Numerous cases have utilized ultrasonography to identify various radial neuropathies at the elbow. Further, visualization of the surrounding anatomy at the site of lesion allows for the identification of the underlying causes of radial neuropathies. These reported etiologies include ganglion cysts (25–27), masses/tumors (28–30), entrapment from surrounding tissues (31), vascular structures (3), and iatrogenic causes from interventions (32, 33).
Interestingly, neuralgic amyotrophy (also known as Parsonage-Turner syndrome), has been redefined over the past several years, with new knowledge coming from ultrasonographic studies of the radial nerve (34–36). Neuralgic amyotrophy used to be described as a brachial plexopathy, but ultrasound and other imaging studies have shown that the majority of pathologic changes actually occur outside the brachial plexus, with several studies showing radial nerve abnormalities. The most commonly described nerve imaging abnormalities in this condition include hourglass deformities of the nerve. Detailed imaging has shown fascicles rotating around each other, which suggests nerve torsion, and, surgical exploration has confirmed nerve torsion in those cases (34). Further investigation is needed, but imaging findings now suggest that neuralgic amyotrophy is not a brachial plexopathy, but rather a process that involves motor-predominant peripheral nerves, and sometimes results in torsion of these nerves.
Clinical Recommendations
Given the challenges with electrodiagnostic studies in suspected radial mononeuropathies (37), neuromuscular ultrasound provides a convenient and complementary tool to potentially diagnose the specific etiology causing the radial neuropathy at the elbow. In addition, numerous studies and case reports already mentioned have integrated ultrasound findings with the clinical and electrical diagnosis of radial neuropathies at the elbow. Based on the literature review and clinical experiences, ultrasound findings detected in radial mononeuropathies include focal nerve enlargement, nerve hypoechogenicity, enlarged nerve fascicles, and increased nerve vascularity (20). Using these parameters, we outline a systematic approach to identify the site and potentially the etiology of radial neuropathies at the elbow with ultrasound. Other detailed resources are available to assist readers in further understanding approaches to imaging the radial nerve at the elbow and identifying key surrounding structures (38, 39).
The radial nerve bifurcates into the superficial radial sensory nerve and the deep motor nerve at the antecubital fossa. When the transducer is placed at the antecubital fossa to obtain a cross-sectional view (Figure 1), both the sensory and motor branches of the radial nerve are visualized between the brachialis and brachioradialis muscles. At this site (or within 1 cm proximally and distally), the ultrasonographer can assess for fibrous bands anterior to the radiocapitellar joint, the recurrent radial vessels of the leash of Henry, and the proximal edge of the ECRB. Moving the transducer proximally (Figure 2), the radial nerve can be identified adjacent to the humerus, coursing through the spiral groove between the long head of the triceps and the humerus. Near the spiral groove, the deep brachial artery can be identified adjacent to the radial nerve. If necessary, the radial nerve can be traced all the way proximally to the terminal branch of brachial plexus.
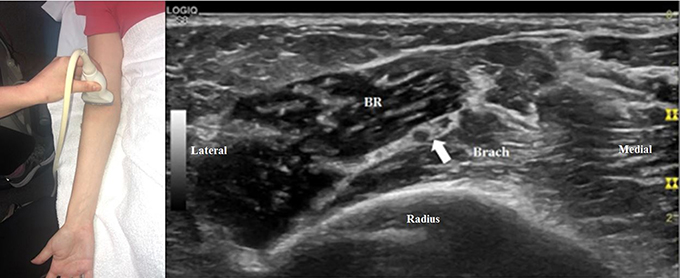
Figure 1. The transducer is placed just proximal to the right antecubital fossa to obtain a cross-sectional view. The radial nerve can be seen (arrow), with two large fascicles that will become the motor and sensory branches. In this image, the lateral fascicle will become the deep branch of the radial nerve and the medial fascicle will become the superficial branch. All images in this article were obtained from a volunteer specifically for illustrative purposes related to this article. Consent was provided. Brach, brachialis, BR, brachioradialis.
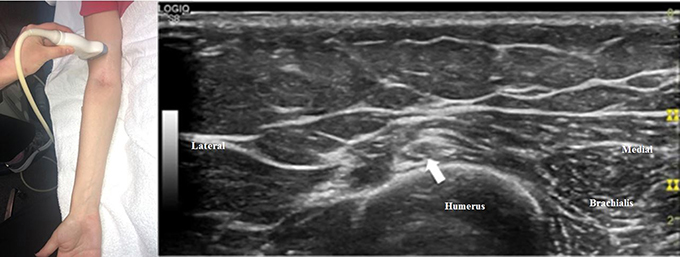
Figure 2. The transducer has been moved proximally compared to Figure 1, and the radial nerve (arrow) can now be seen adjacent to the humerus (the convex, hyperechoic structure just deep to the nerve) in the spiral groove.
To search for a more distal nerve injury, start at the initial antecubital location from Figure 1. As one moves distally, the deep motor branch dives into the arcade of Frohse between the two layers of the supinator muscle (Figure 3). Moving the transducer further distally, the deep motor branch of the radial nerve exits the tunnel as the PIN. Figure 4 shows the PIN coursing obliquely to the posterior forearm around the lateral aspect of the radius between the layers of the supinator muscle. It courses on the interosseous membrane and in front of the extensor pollicis longus until it divides to innervate the individual muscles of the radial and dorsal surface of the forearm.
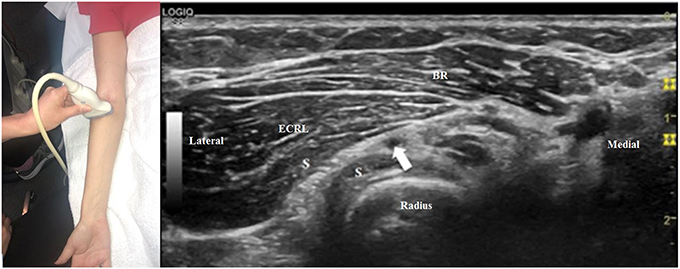
Figure 3. The transducer is now just distal to its position in Figure 1. The motor branch of the radial nerve (arrow) is just beginning to enter the arcade of Frohse, between the two layers of the supinator muscle (S). BR, brachioradialis; ECRL, extensor carpi radialis longus.
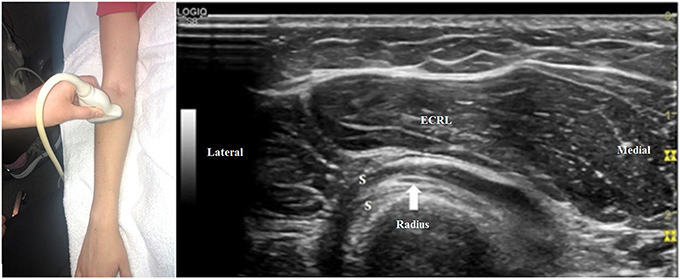
Figure 4. The transducer is just distal to its position in Figure 3. The motor branch of the radial nerve has now become the posterior interosseous nerve (arrow) and is imaged in a slightly oblique view between the two layers of the supinator (S). ECRL, extensor carpi radialis longus.
To track the superficial sensory branch of the radial nerve, start again in the antecubital fossa and move the transducer distally (Figure 5). The superficial radial sensory nerve travels lateral to the radial artery beneath the brachioradialis muscle and tendon (Figure 6). The nerve travels between the brachioradialis and extensor carpi radialis longus tendons. Eventually, the superficial radial nerve pierces the overlying forearm fascia and divides into lateral and medial divisions and further divides into dorsal digital nerves (40).
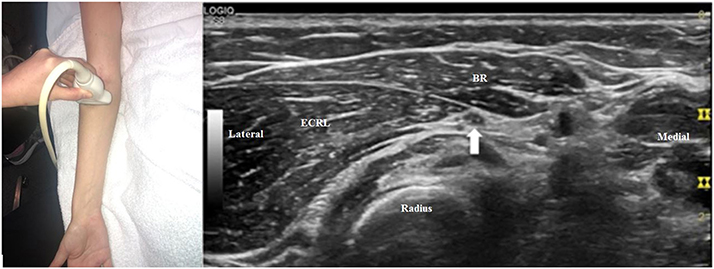
Figure 5. The transducer is just distal to the antecubital fossa and the superficial radial sensory branch of the radial nerve can be seen (arrow). BR, brachioradialis; ECRL, extensor carpi radialis longus.
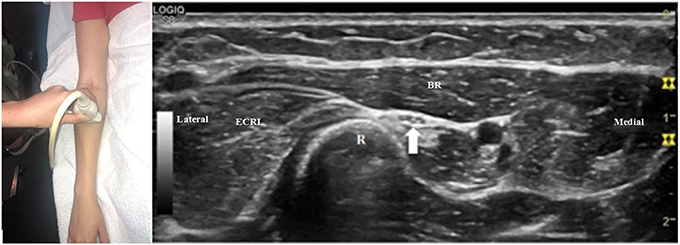
Figure 6. The transducer is now more distal than in Figure 5, and the superficial radial sensory nerve (arrow) is seen next to the convex, hyperechoic radius (R). BR, brachioradialis, ECRL, extensor carpi radialis longus.
As the radial nerve, deep motor branch, PIN, and/or superficial radial branch are scanned, it is important to note the cross-sectional area, overall echogenicity, echotexture, and fascicle size and distribution. At areas of focal nerve enlargement, the cross-sectional area of the nerve should be measured using the trace function of the ultrasound device and tracing along the inner border of the hyperechoic epineurium. This can then be compared to the contralateral side in individuals with unilateral symptoms. In addition, the nerve at the site of interest should be examined using Doppler to determine if there is increased blood flow within the nerve (41). Finally, it is important to view the site of interest in at least two orthogonal planes, and sometimes even more imaging planes are needed. Images from the site of interest should be saved for clinical care and documentation purposes.
Very high-frequency ultrasound (VevoMD with a 48 MHz transducer, FujiFilm, Bothell, WA, USA), if available, can demonstrate the highly detailed anatomy of the radial nerve (Figure 7), which may assist in diagnosis. While this technology is not currently universally available, it is becoming more commonplace and in our opinion may be part of the imaging standard in the near future.
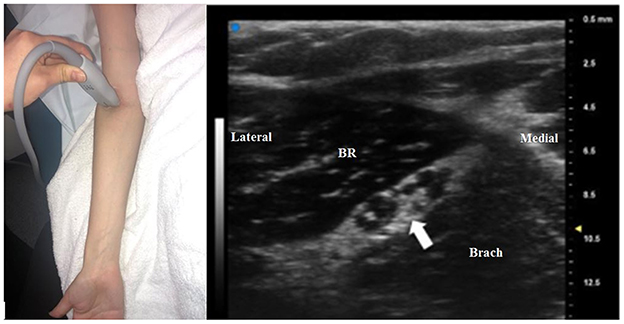
Figure 7. An ultra-high frequency 48 MHz transducer is used to image the radial nerve (arrow) just proximal to the antecubital fossa. Two prominent groups fascicles can be seen within the radial nerve, and the lateral group of fascicles will become the deep branch of the radial nerve and the medial fascicles will be become the superficial branch. This matches with the site of Figure 1, but the fascicular structure of the nerve can be seen in more detail. BR, brachioradialis; Brach, brachialis.
Conclusions
Radial neuropathy at the elbow involves a heterogeneous group of conditions in which the radial nerve proper or branches of the radial nerve (including the superficial sensory, deep motor, and PIN) may be involved. There are 5 sites at which entrapment can occur, and the underlying causes of radial mononeuropathies include cysts, vessels, trauma, or iatrogenic injuries that can be identified with ultrasound. A systematic approach to scanning the radial nerve with ultrasound can assist in the diagnosis and identification of these conditions. Future studies may involve evaluation of poorly understood conditions such as neuralgic amyotrophy and the use of ultra-high frequency ultrasound.
Ethics Statement
We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Author Contributions
MC contributed to the original idea, manuscript writing, editing, and proofreading. TX contributed to the literature search, manuscript writing, editing, and proofreading.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Moradi A, Ebrahimzadeh MH, Jupiter JB. Radial tunnel syndrome, diagnostic and treatment dilemma. Arch Bone J Surg. (2015) 3:156–62. doi: 10.22038/abjs.2015.4110
2. Thatte MR, Mansukhani KA. Compressive neuropathy in the upper limb. Indian J Plast Surg. (2011) 44:283–97. doi: 10.4103/0970-0358.85350
3. Loizides A, Peer S, Ostermann S, Henninger B, Stampfer-Kountchev M, Gruber H. Unusual functional compression of the deep branch of the radial nerve by a vascular branch (leash of Henry): ultrasonographic appearance. Rofo. (2011) 183:163–6. doi: 10.1055/s-0029-1245738
4. Vergara-Amador E, Ramirez A. Anatomic study of the extensor carpi radialis brevis in its relation with the motor branch of the radial nerve. Orthop Traumatol Surg Res. (2015) 101:909–12. doi: 10.1016/j.otsr.2015.09.030
5. Clavert P, Lutz JC, Adam P, Wolfram-Gabel R, Liverneaux P, Kahn JL. Frohse's arcade is not the exclusive compression site of the radial nerve in its tunnel. Orthop Traumatol Surg Res. (2009) 95:114–8. doi: 10.1016/j.otsr.2008.11.001
6. Suk JI, Walker FO, Cartwright MS. Ultrasonography of peripheral nerves. Curr Neurol Neurosci Rep. (2013) 13:328. doi: 10.1007/s11910-012-0328-x
7. Hobson-Webb LD, Padua L. Ultrasound of Focal Neuropathies. J Clin Neurophysiol. (2016) 33:94–102. doi: 10.1097/WNP.0000000000000233
8. Cartwright MS, Hobson-Webb LD, Boon AJ, Alter KE, Hunt CH, Flores VH, et al. Evidence-based guideline: neuromuscular ultrasound for the diagnosis of carpal tunnel syndrome. Muscle Nerve. (2012) 46:287–93. doi: 10.1002/mus.23389
9. Beekman R, Van Der Plas JP, Uitdehaag BM, Schellens RL, Visser LH. Clinical, electrodiagnostic, and sonographic studies in ulnar neuropathy at the elbow. Muscle Nerve. (2004) 30:202–8. doi: 10.1002/mus.20093
10. Cartwright MS, Passmore LV, Yoon JS, Brown ME, Caress JB, Walker FO. Cross-sectional area reference values for nerve ultrasonography. Muscle Nerve. (2008) 37:566–71. doi: 10.1002/mus.21009
11. Bodner G, Harpf C, Meirer R, Gardetto A, Kovacs P, Gruber H. Ultrasonographic appearance of supinator syndrome. J Ultrasound Med. (2002) 21:1289–93. doi: 10.7863/jum.2002.21.11.1289
12. Ozcakar L, Malas FU, Kara G, Kaymak B, Hascelik Z. Musculoskeletal sonography use in physiatry: a single-center one-year analysis. Am J Phys Med Rehabil. (2010) 89:385–9. doi: 10.1097/PHM.0b013e3181d89e63
13. Debek A, Nowicki P, Czyrny Z. Ultrasonographic diagnostics of pain in the lateral cubital compartment and proximal forearm. J Ultrason. (2012) 12:188–201. doi: 10.15557/JoU.2012.0006
14. Djurdjevic T, Loizides A, Loscher W, Gruber H, Plaikner M, Peer S. High resolution ultrasound in posterior interosseous nerve syndrome. Muscle Nerve. (2014) 49:35–9. doi: 10.1002/mus.23867
15. Nwawka OK. Update in musculoskeletal ultrasound research. Sports Health. (2016) 8:429–37. doi: 10.1177/1941738116664326
16. Kim Y, Ha DH, Lee SM. Ultrasonographic findings of posterior interosseous nerve syndrome. Ultrasonography. (2017) 36:363–9. doi: 10.14366/usg.17007
17. Babaei-Ghazani A, Roomizadeh P, Forogh B, Moeini-Taba SM, Abedini A, Kadkhodaie M, et al. Ultrasound-guided versus landmark-guided local corticosteroid injection for carpal tunnel syndrome: a systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil. (2018) 99:766–75. doi: 10.1016/j.apmr.2017.08.484
18. Koenig RW, Pedro MT, Heinen CP, Schmidt T, Richter HP, Antoniadis G, et al. High-resolution ultrasonography in evaluating peripheral nerve entrapment and trauma. Neurosurg Focus. (2009) 26:E13. doi: 10.3171/FOC.2009.26.2.E13
19. Dietz AR, Bucelli RC, Pestronk A, Zaidman CM. Nerve ultrasound identifies abnormalities in the posterior interosseous nerve in patients with proximal radial neuropathies. Muscle Nerve. (2016) 53:379–83. doi: 10.1002/mus.24778
20. Hommel AL, Cartwright MS, Walker FO. The use of ultrasound in neuromuscular diagnoses. Neurol Clin Pract. (2017) 7:266–73. doi: 10.1212/CPJ.0000000000000368
21. Yoon JS, Walker FO, Cartwright MS. Ulnar neuropathy with normal electrodiagnosis and abnormal nerve ultrasound. Arch Phys Med Rehabil. (2010) 91:318–20. doi: 10.1016/j.apmr.2009.10.010
22. Karabay N, Toros T, Ademoglu Y, Ada S. Ultrasonographic evaluation of the iatrogenic peripheral nerve injuries in upper extremity. Eur J Radiol. (2010) 73:234–40. doi: 10.1016/j.ejrad.2008.10.038
23. Wininger YD, Buckalew NA, Kaufmann RA, Munin MC. Ultrasound combined with electrodiagnosis improves lesion localization and outcome in posterior interosseous neuropathy. Muscle Nerve. (2015) 52:1117–21. doi: 10.1002/mus.24782
24. Erra C, De Franco P, Granata G, Coraci D, Briani C, Paolasso I, et al. Secondary posterior interosseous nerve lesions associated with humeral fractures. Muscle Nerve. (2016) 53:375–8. doi: 10.1002/mus.24752
25. Kara M, Tiftik T, Yetisgin A, Ural G, Ozcakar L. Ultrasound in the diagnosis and treatment of posterior interosseous nerve entrapment: a case report. Muscle Nerve. (2012) 45:299–300. doi: 10.1002/mus.22163
26. Erol B, Cakir T, Kose O, Ozyurek S. Radial nerve entrapment caused by a ganglion cyst at the elbow: treatment with ultrasound-guided aspiration. Am J Phys Med Rehabil. (2014) 93:e6–7. doi: 10.1097/PHM.0000000000000153
27. Seki Y. Posterior interosseous nerve palsy caused by a ganglion: conservative treatment with ultrasound-guided needle aspiration. J Ultrason. (2017) 17:73–5. doi: 10.15557/JoU.2017.0010
28. Fujioka H, Futani H, Fukunaga S, Okuno H, Kano M, Tsukamoto Y, et al. Posterior interosseous nerve palsy caused by synovial chondromatosis arising in the annular periradial recesses of the elbow. Mod Rheumatol. (2011) 21:192–6. doi: 10.3109/s10165-010-0358-7
29. Ali R, Yang LJ, Henning PT. Posterior interosseus nerve palsy resulting from inflammatory myofibroblastic pseudotumor: case presentation. PM R. (2014) 6:659–61. doi: 10.1016/j.pmrj.2013.12.016
30. Narayan S, Ahluwalia VV, Saharan PS, Gupta AK. Intraosseous lipoma of the proximal radius with extra osseous extension leading to posterior interosseous nerve compression: HRUS diagnosis. J Orthop Case Rep. (2016) 6:56–8.
31. Loizides A, Baur EM, Plaikner M, Gruber H. Triple hourglass-like fascicular constriction of the posterior interosseous nerve: a rare cause of PIN syndrome. Arch Orthop Trauma Surg. (2015) 135:635–7. doi: 10.1007/s00402-015-2177-y
32. Soh D, Cappelen-Smith C, Korber J, Heath T, Cordato D. The utility of ultrasound in showing a unique cause of posterior interosseous nerve syndrome. eNeurologicalSci. (2017) 8:34–5. doi: 10.1016/j.ensci.2017.07.002
33. Iskender O, Ozkan O, Leblebicioglu G, Ozcakar L. Ultrasound imaging for complete injury of the posterior interosseous nerve after forearm surgery. Am J Phys Med Rehabil. (2018). doi: 10.1097/PHM.0000000000001056. [Epub ahead of print].
34. Aranyi Z, Csillik A, Devay K, Rosero M, Barsi P, Bohm J, et al. Ultrasonographic identification of nerve pathology in neuralgic amyotrophy: enlargement, constriction, fascicular entwinement, and torsion. Muscle Nerve. (2015) 52:503–11. doi: 10.1002/mus.24615
35. Shi M, Qi H, Ding H, Chen F, Xin Z, Zhao Q, et al. Electrophysiological examination and high frequency ultrasonography for diagnosis of radial nerve torsion and compression. Medicine. (2018) 97:e9587. doi: 10.1097/MD.0000000000009587
36. Van Rosmalen M, Lieba-Samal D, Pillen S, Van Alfen N. Ultrasound of peripheral nerves in neuralgic amyotrophy. Muscle Nerve. (2018) 59:55–9. doi: 10.1002/mus.26322
38. Wu CH, Chang KV, Ozcakar L, Hsiao MY, Hung CY, Shyu SG, et al. Sonographic tracking of the upper limb peripheral nerves: a pictorial essay and video demonstration. Am J Phys Med Rehabil. (2015) 94:740–7. doi: 10.1097/PHM.0000000000000463
39. Chang KV, Mezian K, Nanka O, Wu WT, Lou YM, Wang JC, et al. Ultrasound imaging for the cutaneous nerves of the extremities and relevant entrapment syndromes: from anatomy to clinical implications. J Clin Med. (2018) 7:E457. doi: 10.3390/jcm7110457
40. Kim KH, Byun EJ, Oh EH. Ultrasonographic findings of superficial radial nerve and cephalic vein. Ann Rehabil Med. (2014) 38:52–6. doi: 10.5535/arm.2014.38.1.52
Keywords: ultrasound, radial nerve, entrapment, radial tunnel, clinical recommendation
Citation: Xiao TG and Cartwright MS (2019) Ultrasound in the Evaluation of Radial Neuropathies at the Elbow. Front. Neurol. 10:216. doi: 10.3389/fneur.2019.00216
Received: 16 November 2018; Accepted: 19 February 2019;
Published: 12 March 2019.
Edited by:
Ke-Vin Chang, National Taiwan University Hospital, TaiwanReviewed by:
Sang Beom Kim, Kyung Hee University, South KoreaChen-Yu Hung, National Taiwan University Hospital Bei-Hu Branch, Taiwan
Stefan Meng, Medical University of Vienna, Austria
Copyright © 2019 Xiao and Cartwright. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael S. Cartwright, bWNhcnR3cmlAd2FrZWhlYWx0aC5lZHU=
 Ted G. Xiao
Ted G. Xiao Michael S. Cartwright
Michael S. Cartwright