- 1The Queen’s Medical Center, Honolulu, HI, United States
- 2Department of Medicine, John A. Burns School of Medicine, University of Hawaii, Honolulu, HI, United States
- 3Department of Native Hawaiian Health, John A. Burns School of Medicine, University of Hawaii, Honolulu, HI, United States
Background: Disparities in outcome after intracerebral hemorrhage (ICH) among Asians, Native Hawaiians, and other Pacific Islanders (NHOPI) have been inadequately studied. We sought to assess differences in functional outcome between Asians and NHOPI after ICH.
Methods: A multiracial prospective cohort study of ICH patients was conducted from 2011 to 2016 at a tertiary center in Honolulu, HI, USA to assess racial disparities in outcome after ICH. Favorable outcome was defined as 3-month modified Rankin Scale (mRS) score ≤2. Patients with no available 3-month functional outcome, race other than Asians and NHOPI, and baseline mRS > 0 were excluded. Multivariable analyses using logistic regression were performed to assess the impact of race on favorable outcome after adjusting for the ICH Score, early do-not-resuscitate (DNR) order and dementia/cognitive impairment.
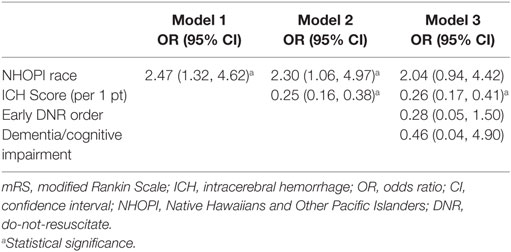
Results: A total of 220 patients (161 Asians, 59 NHOPI) were studied. Overall, 65 (29.5%) achieved favorable outcome at 3 months. NHOPI were younger than Asians (p < 0.0001) and had higher prevalence of diabetes (p = 0.007), obesity (p < 0.0001), and lower prevalence of dementia/cognitive impairment (p = 0.02), early DNR order (p = 0.0004), and advance directive presence (p = 0.0005). NHOPI race was a predictor of favorable outcome in the unadjusted model [odds ratio (OR) 2.47, 95% confidence interval (CI): 1.32–4.62] and after adjusting for the ICH Score (OR 2.30, 95% CI: 1.06–4.97) but not in the final model (OR 2.04, 95% CI: 0.94–4.42). In the final model, the ICH Score was the only independent negative predictor of outcome (OR 0.26, 95% CI: 0.17–0.41 per point).
Conclusion: NHOPI are more likely to achieve favorable functional outcome after ICH compared with Asians even after controlling for ICH severity. However, this association was attenuated by the DNR and dementia/cognitive impairment status.
Introduction
Intracerebral hemorrhage (ICH) has disproportionately high mortality and morbidity with only 21–31% of patients gaining functional independence at 3 months (1–3). Prior studies that assessed racial/ethnic disparities in ICH have shown that minority groups, particularly African Americans and Hispanics, have a higher incidence of ICH and younger age of presentation than whites (4, 5). Asians are also estimated to have a higher incidence of ICH compared with Caucasians (6). In Hawaii, Native Hawaiians and Other Pacific Islanders (NHOPI), have been shown to have younger age of ICH onset and higher burden of cardiovascular risk factors compared with whites (7, 8).
Although the overall incidence of stroke is greater among minorities, the reported impact of ethnicity on outcomes after stroke has been inconsistent and unclear. Prior studies showed greater initial physical impairments and greater residual disability in African American stroke patients compared with white stroke patients (9, 10). Another study showed that blacks had severer cases and higher prevalence of coma after ICH (11). However, more recent studies have shown comparable or better outcomes after ICH among blacks and Hispanics compared with whites (3, 12). A few studies that specifically assessed Asians showed lower risk-adjusted mortality after ICH and ischemic stroke compared with whites.
Overall, there is still a paucity of data on racial disparities in ICH outcome among Asians and NHOPI. Furthermore, NHOPI have been historically aggregated with Asians into a single racial category in many studies. Since Asians and NHOPI may have different underlying phenotype, lifestyle, socioeconomic status and different level of acculturation to the western civilization, aggregating them into a single racial group may have masked potentially important differences between the two groups (13). Therefore, we sought to compare the functional outcome after ICH between Asians and NHOPI. We hypothesized that Asians, a racial group that has higher life expectancy and lower cardiovascular risk factors than NHOPI, are more likely to have better functional outcome after ICH compared with NHOPI.
Patients and Methods
A multiracial prospective cohort study of ICH patients (Queen Emma Stroke Study) was conducted from July 2011 to June 2016 at The Queen’s Medical Center (QMC) to assess racial disparities in long-term functional outcome after ICH. Last patient enrollment occurred in June 2015, and last follow up assessment occurred in June 2016. QMC is a 505-bed medical center located in downtown Honolulu, the largest hospital in Hawaii and the tertiary referral center for the Pacific Basin. QMC is a Joint Commission-certified Comprehensive Stroke Center and has the only Neuroscience Intensive Care Unit in the state of Hawaii. Since ICH is a condition that is preferably treated in the Neuroscience Intensive Care Unit, QMC is the primary referral center for acute management of ICH patients from other major islands. This study was approved by the University of Hawaii Institutional Review Board, and written informed consent was obtained from the patient or legally authorized surrogate decision-maker.
Patients
All ICH patients hospitalized at QMC were prospectively screened for enrollment by the investigators and research staff. Inclusion criteria for the cohort study included: age ≥18 years; non-traumatic ICH with confirmation by computed tomography (CT); resident of Hawaii for greater than 3 months in a household with a telephone. Exclusion criteria were: ICH related to ruptured cerebral aneurysm; ICH related to brain tumor or hemorrhagic conversion of ischemic stroke, and the patients or surrogate decision-makers being non-English speaking. Management of ICH at QMC was in accordance with the most current guidelines (14) at the time of patient enrollment.
Study Procedures
This was an observational study and no intervention was provided. Patient demographic information (race, ethnicity, marital status, income level, insurance status, etc.) was obtained directly from the patients or their family if the patients were incapacitated. Since mixed racial background is relatively common in Hawaii, race was defined as the single racial/cultural background that the patient most closely associated with and was based on patient self-identification or family’s identification if the patient was incapacitated. Race was ultimately categorized as whites, Asians, NHOPI or other. Clinical diagnosis of preexisting dementia or cognitive impairment had to be made by their respective physicians before the hospitalization through formal clinical evaluation. Initial systolic blood pressure, diastolic blood pressure (DBP), and Glasgow Coma Scale (GCS) score were obtained from the medical record. Obesity was defined as body mass index >30 kg/m2 for all racial groups. Regular visit to a primary care physician was defined as a minimum of one routine visit per year over the past year. Prehospital baseline functional status was assessed using the modified Rankin Scale (mRS) and was obtained through direct patient/family interview. All initial head CT scans were reviewed by one of the physician investigators (Kazuma Nakagawa) using a standardized protocol. Hematoma volume was measured using the previously described ABC/2 method (15). Presence of intraventricular hemorrhage (IVH) was recorded, and ICH location was coded as deep (basal ganglia or thalamus), lobar, brainstem, cerebellum, or primary IVH. The ICH Score was calculated based on the age, initial head CT findings, and the initial GCS on arrival. Do-not-resuscitate (DNR) orders were defined as any plan to limit cardiopulmonary resuscitation or mechanical ventilation in the event of a cardiopulmonary arrest. Based on the date/time of the DNR order entry, DNR status was categorized to “early DNR” (within 24 h of presentation) or “any DNR” (DNR orders at any time). Presence of advance directive was confirmed by its physical presence in the paper chart and documentation of its content by the primary provider.
Outcome Measures
Outcome at 3 months was assessed by telephone or in-person interview using a standardized, simplified mRS questionnaire algorithm (16). Favorable outcome was defined as 3-month mRS score ≤2.
Statistical Analysis
Data were analyzed using SPSS version 23.0 (SPSS IBM Inc., Chicago, IL, USA). For this study, patients with no available 3-month functional outcome and patients with race other than Asians and NHOPI were excluded. Although we had initially planned to include whites as a reference racial group for the study, whites were ultimately excluded from the analysis since only 37 whites were enrolled in the study, and their inclusion would have weakened the statistical analyses and generalizability. Finally, patients with baseline mRS > 0 were excluded since preexisting disability would have confounded the results. Patient characteristics were summarized using descriptive statistics appropriate to variable type. NHOPI were compared with Asians (reference group) using the chi-square test for categorical data, two-tailed t-test for normally distributed, continuous variables, and Mann–Whitney U test for non-parametric data (i.e., age, blood pressure, GCS, and hematoma volume). To determine the impact of race on outcome, multivariable analyses using a logistic regression model were performed to assess whether NHOPI race, compared with Asian race, is an independent predictor of 3-month functional outcome. Due to the small sample size, which limited our ability to include numerous variables in the model, we had preselected three potential confounders in the model: ICH Score, early DNR order status and history of dementia/cognitive impairment, based on biological plausibility and prior studies showing association between these factors and functional outcome after ICH (1, 2, 17, 18). For secondary analyses, a similar process was repeated after excluding the in-hospital non-survivors to eliminate the impact of in-hospital mortality as the primary factor driving the potential racial differences in 3-month outcome. Odds ratio (OR) and 95% confidence interval (CI) were calculated from the beta coefficients and their SEs. Levels of p < 0.05 were considered statistically significant.
Results
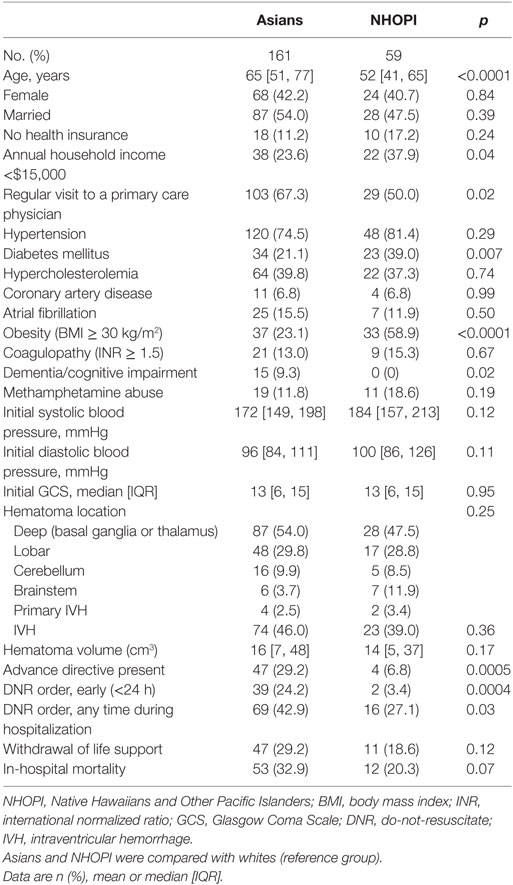
A total of 323 ICH patients were enrolled in the cohort study between July 2011 and June 2015. Among them, 32 patients who did not have 3-month outcome data were excluded from the analyses. Of the remaining 291 patients, 37 patients with white race and 9 with other race were excluded due to small population size. Furthermore, 25 patients with baseline mRS > 0 were excluded. Table 1 provides the demographic and clinical information of 220 patients [Asians 73.2% (n = 161), NHOPI 26.8% (n = 59)] who were included in the final analyses. Overall, NHOPI had younger age (12.1 years younger), lower socioeconomic status, lower rate of regular visit to their primary care physician, higher prevalence of diabetes and obesity, higher initial DBP and lower prevalence of dementia/cognitive impairment compared with Asians. NHOPI had lower rate of advance directive, early DNR order, and any DNR order compared with Asians. Sub-analyses comparing the hematoma size for each ICH location showed that hematoma size was larger among Asians than NHOPI for lobar hemorrhage (lobar: Asians: 41 [15, 90] cm3 vs. NHOPI: 15 [4, 51] cm3, p = 0.03). However, no differences in the hematoma size was observed in the other locations (deep: Asians: 14 [5, 36] cm3 vs. NHOPI: 14 [7, 32] cm3, p = 0.85; cerebellum: Asians: 11 [6, 19] cm3 vs. NHOPI: 24 [10, 39] cm3, p = 0.31; brainstem: Asians: 5 [2, 11] cm3 vs. NHOPI: 3 [2, 8] cm3, p = 0.84).
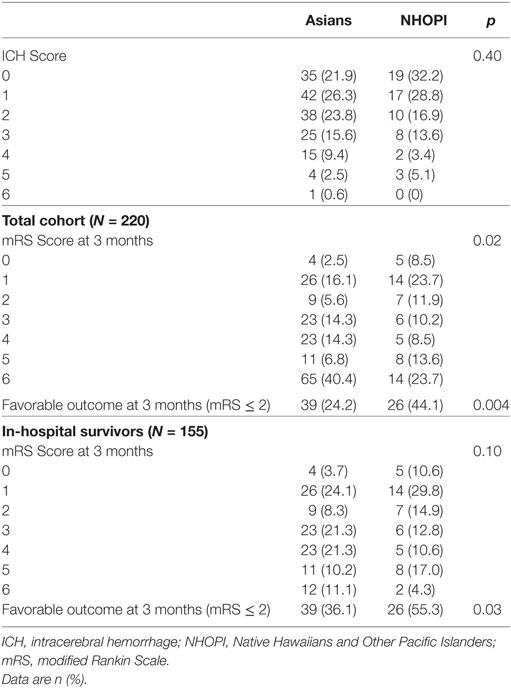
Overall, 65 (29.5%) achieved favorable outcome at 3 months. The comparison of mRS distribution between Asians and NHOPI is shown in Table 2 and demonstrates a significance difference between the two races. The prevalence of favorable 3-month outcome was higher among NHOPI compared with Asians (44.1 vs. 24.2%, respectively, p = 0.02) despite having similar ICH Score distribution. After excluding the in-hospital non-survivors, the difference in functional outcome between NHOPI and Asians persisted among the survivors of the initial hospitalization (55.3 vs. 36.1%, respectively, p = 0.03). Table 3 demonstrates the univariate and multivariable models. Compared with Asian race, NHOPI race was a predictor of favorable outcome in the unadjusted model (OR 2.47, 95% CI: 1.32–4.62) and after adjusting for the ICH Score (OR 2.30, 95% CI: 1.06–4.97) but not in the final model, which included ICH Score, early DNR order status and history of dementia/cognitive impairment (OR 2.04, 95% CI: 0.94–4.42). In this model, the ICH Score remained as the only independent negative predictor of outcome (OR 0.26, 95% CI: 0.17–0.41 per point).
Discussion
Our results showed that 29.5% of the ICH patients achieved favorable functional outcome at 3 months, which is consistent with the prior studies (1–3). Contrary to our hypothesis, NHOPI in our study were more likely to achieve favorable 3-month functional outcome compared with Asians after adjusting for the ICH Score. However, our observed impact of race on functional outcome after ICH was attenuated after adjusting for early DNR order and dementia/cognitive impairment, suggesting that the higher prevalence of these factors among Asians may have driven the observed racial differences in outcome. In the final model, the ICH Score remained as the only independent predictor of 3-month functional outcome as previously described (2). Despite a higher prevalence of cardiovascular risk factors and low socioeconomic status as shown in this study, functional outcome remained significantly better in NHOPI compared with Asians.
Our study emphasizes the importance of disaggregating racial and ethnic populations who may be historically grouped into a single racial/ethnic group but upon a more detailed analysis, suggests that other social or cultural factors (i.e., aggressiveness in clinical care) may underlie some of the observed differences in racial/ethnic outcomes (19, 20). Moreover, other unmeasured factors such as social support, spiritual, or cultural factors may have also influenced the differences in outcome and may be partly reflected in the aggressiveness of treatment after ICH.
Much of the differences in functional outcome could be explained by the racial differences in the aggressiveness of care that the patient’s families seek in the inpatient and post-discharge settings, as supported by the lower rate of early DNR, any DNR and advance directive presence among NHOPI compared with Asians. Also, there was a trend toward lower rate of withdrawal of life support among NHOPI compared with Asians. The lower rates of these measures often reflect the patients and families’ wishes to provide more aggressive and less palliative-oriented patient care. These decisions may be impacted by social, religious or cultural factors that may differ by race. It is possible that this outlook impacted the intensity and frequency of post-discharge rehabilitation processes for the NHOPI.
Although less aggressive care and higher prevalence of dementia/cognitive among the Asians may partially explain the observed racial differences in outcome, there may be other possible explanations. First, although we limited our studies to patients with baseline mRS of 0 (no symptoms), it is possible that older Asian group had lower baseline function than NHOPI, but were not captured by the prehospital mRS survey in this study. Second, there may be racial differences in the perception of disability after stroke and one group may score themselves higher on the disability rating despite having similar physical disabilities. Also, collective culture such as Asian culture strives for common social identify and may lead individuals with disabilities to perceive themselves as having greater burden to the society compared with those in more individualistic culture. Third, there may be fundamental biological differences between the two groups that impact functional outcome. For example, apolipoprotein E (APOE) 4 allele carriers have been associated with worse functional outcome after ICH compared with the non-carriers (21, 22), and therefore it is possible to have racial differences in the prevalence of APOE four allele carriers between Asians and NHOPI.
The strength of our study is that this is the largest prospective cohort study to characterize functional outcome after ICH among a diverse group of Asians and NHOPI. Prior ICH studies that assessed Asians and NHOPI in Hawaii were retrospective single-center studies that only assessed in-hospital mortality as an outcome measure (7). This study recruited a relatively large number of NHOPI population, which has been historically underrepresented in prior prospective stroke studies. The limitation of this study is the relatively low sample size, which led to the elimination of whites from the analyses. Also, since this is a single-center study, generalizability of our results to other populations may be limited. Specifically, because our institution is a tertiary referral center, there may have been a referral bias toward more severe ICH patients since those with small hematomas and minor neurological symptoms may not have been transferred to our facility. Also, it is possible that some of the older ICH patients with preexisting DNR orders or those with terminal illness may not have transferred to our facility, creating a possible selection bias toward younger ICH patients. We also did not completely account for the age factor in the model since dichotomized age factor (<80 vs. ≥80 years) used in the ICH Score may not necessarily distinguish the disparate number of very young population. Finally, we cannot exclude the possibility that this cohort study enrolled ICH patients with different severity mix compared with other published studies. However, 65 of 220 patients (29.5%) achieved mRS score ≤2 at 3 months, which is comparable to other observational studies (1–3). This study showed that after ICH, NHOPI are more likely to achieve favorable functional outcome compared with Asians even after adjusting for the severity of ICH. However, this difference was attenuated after adjusting for the DNR and baseline cognitive status. This study further supports efforts to disaggregate Asians and NHOPI from the traditionally combined “Asian American Pacific Islander” classification, which may mask potentially different underlying mechanisms as well as cultural differences between Asians and NHOPI in patient and family responses to severely disabling conditions such as ICH.
Ethics Statement
This study was approved by the University of Hawaii Institutional Review Board, and written informed consent was obtained from the patient or legally authorized surrogate decision-maker.
Author Contributions
KN participated in the conception and design of the study, the acquisition of data, the analysis and interpretation of data, and was responsible for drafting and finalizing the manuscript. SK participated in the acquisition of data and helped to draft and finalize the manuscript. TS participated in the study supervision, analysis and interpretation of data, and was responsible for drafting and finalizing the manuscript. MM participated in the study supervision, analysis and interpretation of data, and was responsible for drafting and finalizing the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was presented as a poster abstract presentation at the Neurocritical Care Society Meeting on October 11, 2017.
Funding
This study was supported in part by the National Institute on Minority Health and Health Disparities of the NIH (P20MD000173; U54MD007584) and in part by the American Heart Association (11CRP7160019).
References
1. Rost NS, Smith EE, Chang Y, Snider RW, Chanderraj R, Schwab K, et al. Prediction of functional outcome in patients with primary intracerebral hemorrhage: the FUNC score. Stroke (2008) 39(8):2304–9. doi:10.1161/STROKEAHA.107.512202
2. Hemphill JC III, Farrant M, Neill TA Jr. Prospective validation of the ICH Score for 12-month functional outcome. Neurology (2009) 73(14):1088–94. doi:10.1212/WNL.0b013e3181b8b332
3. Koch S, Elkind MS, Testai FD, Brown WM, Martini S, Sheth KN, et al. Racial-ethnic disparities in acute blood pressure after intracerebral hemorrhage. Neurology (2016) 87(8):786–91. doi:10.1212/WNL.0000000000002962
4. Sacco RL, Boden-Albala B, Abel G, Lin IF, Elkind M, Hauser WA, et al. Race-ethnic disparities in the impact of stroke risk factors: the northern Manhattan stroke study. Stroke (2001) 32(8):1725–31. doi:10.1161/01.STR.32.8.1725
5. Stansbury JP, Jia H, Williams LS, Vogel WB, Duncan PW. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke (2005) 36(2):374–86. doi:10.1161/01.STR.0000153065.39325.fd
6. van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol (2010) 9(2):167–76. doi:10.1016/S1474-4422(09)70340-0
7. Nakagawa K, Koenig MA, Seto TB, Asai SM, Chang CW. Racial disparities among Native Hawaiians and Pacific Islanders with intracerebral hemorrhage. Neurology (2012) 79(7):675–80. doi:10.1212/WNL.0b013e3182608c6f
8. Nakagawa K, Vento MA, Ing MM, Seto TB. Racial disparities in methamphetamine-associated intracerebral hemorrhage. Neurology (2015) 84(10):995–1001. doi:10.1212/WNL.0000000000001339
9. Horner RD, Matchar DB, Divine GW, Feussner JR. Racial variations in ischemic stroke-related physical and functional impairments. Stroke (1991) 22(12):1497–501. doi:10.1161/01.STR.22.12.1497
10. Horner RD, Swanson JW, Bosworth HB, Matchar DB. Effects of race and poverty on the process and outcome of inpatient rehabilitation services among stroke patients. Stroke (2003) 34(4):1027–31. doi:10.1161/01.STR.0000060028.60365.5D
11. Kuhlemeier KV, Stiens SA. Racial disparities in severity of cerebrovascular events. Stroke (1994) 25(11):2126–31. doi:10.1161/01.STR.25.11.2126
12. Xian Y, Holloway RG, Smith EE, Schwamm LH, Reeves MJ, Bhatt DL, et al. Racial/ethnic differences in process of care and outcomes among patients hospitalized with intracerebral hemorrhage. Stroke (2014) 45(11):3243–50. doi:10.1161/STROKEAHA.114.005620
13. Park CB, Braun KL, Horiuchi BY, Tottori C, Onaka AT. Longevity disparities in multiethnic Hawaii: an analysis of 2000 life tables. Public Health Rep (2009) 124(4):579–84. doi:10.1177/003335490912400415
14. Hemphill JC III, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke (2015) 46(7):2032–60. doi:10.1161/STR.0000000000000069
15. Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke (1996) 27(8):1304–5. doi:10.1161/01.STR.27.8.1304
16. Bruno A, Shah N, Lin C, Close B, Hess DC, Davis K, et al. Improving modified Rankin Scale assessment with a simplified questionnaire. Stroke (2010) 41(5):1048–50. doi:10.1161/STROKEAHA.109.571562
17. Zahuranec DB, Morgenstern LB, Sanchez BN, Resnicow K, White DB, Hemphill JC III. Do-not-resuscitate orders and predictive models after intracerebral hemorrhage. Neurology (2010) 75(7):626–33. doi:10.1212/WNL.0b013e3181ed9cc9
18. Morgenstern LB, Zahuranec DB, Sanchez BN, Becker KJ, Geraghty M, Hughes R, et al. Full medical support for intracerebral hemorrhage. Neurology (2015) 84(17):1739–44. doi:10.1212/WNL.0000000000001525
19. Zahuranec DB, Brown DL, Lisabeth LD, Gonzales NR, Longwell PJ, Smith MA, et al. Ethnic differences in do-not-resuscitate orders after intracerebral hemorrhage. Crit Care Med (2009) 37(10):2807–11. doi:10.1097/CCM.0b013e3181a56755
20. Shaw KM, Gallek MJ, Sheppard KG, Ritter L, Vento MA, Asai SM, et al. Ethnic differences in withdrawal of life support after intracerebral hemorrhage. Hawaii J Med Public Health (2015) 74(6):203–9.
21. McCarron MO, Nicoll JA. High frequency of apolipoprotein E epsilon 2 allele is specific for patients with cerebral amyloid angiopathy-related haemorrhage. Neurosci Lett (1998) 247(1):45–8. doi:10.1016/S0304-3940(98)00286-9
Keywords: race, functional outcome, intracerebral hemorrhage
Citation: Nakagawa K, King SL, Seto TB and Mau MKLM (2018) Disparities in Functional Outcome After Intracerebral Hemorrhage Among Asians and Pacific Islanders. Front. Neurol. 9:186. doi: 10.3389/fneur.2018.00186
Received: 03 November 2017; Accepted: 09 March 2018;
Published: 27 March 2018
Edited by:
Souvik Sen, University of South Carolina, United StatesReviewed by:
Christoph Stretz, Yale University, United StatesAshfaq Shuaib, University of Alberta, Canada
Copyright: © 2018 Nakagawa, King, Seto and Mau. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kazuma Nakagawa, a2F6dW1hLm5ha2FnYXdhJiN4MDAwNDA7aGF3YWlpLmVkdQ==
 Kazuma Nakagawa
Kazuma Nakagawa Sage L. King1
Sage L. King1 Todd B. Seto
Todd B. Seto Marjorie K. L. M. Mau
Marjorie K. L. M. Mau