- 1Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 2Computed Tomgraphy Department of the Fifth Affiliated Hospital of Dali University, Baoshan, China
- 3Department of Medical Imaging, Wuhan Pulmonary Hospital, Wuhan, China
Atrial myxoma is a rare benign tumor that can cause a variety of complications, including cerebral infarction. We present a case of a 52-year-old female patient who developed cerebral infarction caused by an atrial myxoma. The patient underwent successful surgical resection of the tumor, and the infarction was managed accordingly. However, 15-months post-surgery, the patient developed new neurological symptoms. Imaging studies revealed multiple cerebral metastases, consistent with the possibility of seeding of tumor cells. This rare complication emphasizes the importance of long-term monitoring after the resection of atrial myxomas. The occurrence of metastasis in the brain, though rare, should be considered in follow-up care, particularly in patients who have had embolic events related to atrial myxomas. Our case highlights the potential for cerebral myxoma metastasis even after initial successful surgical intervention, underscoring the need for comprehensive follow-up and vigilant monitoring of such patients.
Introduction
Atrial myxoma is a rare benign primary cardiac tumor (Jaravaza et al., 2021), most commonly arising from the endocardial surface of the atria (Reynen, 1995). While it is generally considered non-malignant, a small subset of cases has shown potential for recurrence and even metastatic spread. Tumor fragmentation poses a significant risk, as embolization of detached fragments can result in systemic embolic events, and, in rare instances, lead to tumor metastasis (Hau et al., 2020; Alrohimi et al., 2019; Waliszewska-Prosół et al., 2018).
We present a case involving a 52-year-old female patient who was initially admitted with chest pain, subsequently developing an ischemic stroke that resulted in left-sided hemiparesis. Imaging studies revealed the presence of an atrial myxoma, which was complicated by the acute ischemic event. The patient underwent thoracotomy for the resection of the tumor. However, 1-year post-surgery, multiple brain metastases were detected. Herein, we present a rare case of tumor metastasis after the resection of atrial myxoma. And we recommend closely monitoring MRI follow-up after cerebral infarction caused by atrial myxoma, based on a comprehensive literature review and our experience with this case of multiple cerebral myxoma metastases.
Case presentation
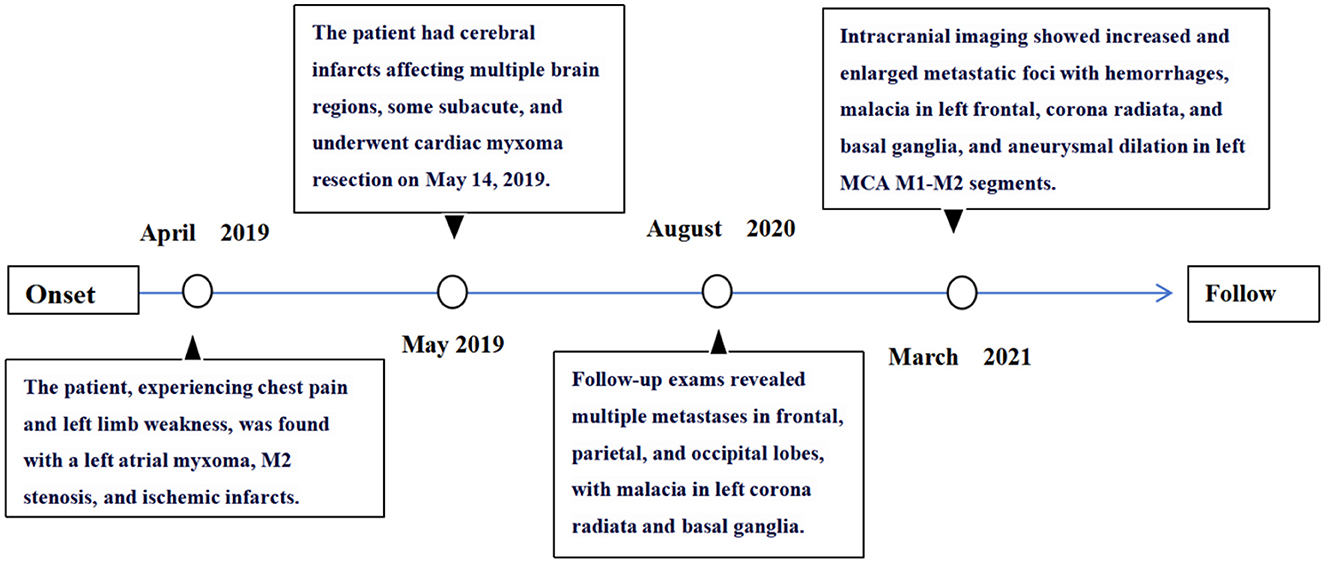
A 52-year-old female patient was admitted with symptoms of palpitations, chest pain, and weakness in her left lower limb with no prior medical history of conditions such as hypertension, diabetes, atrial fibrillation, smoking, or any other relevant factors. Emergency echocardiography revealed an abnormal echogenic mass in the left atrium (Figure 1A), suspected to be a thrombus or of other possible etiologies, and left atrial enlargement. Cardiac MRI identified an irregular mass within the left atrium, with a maximum cross-sectional diameter of ~3.9 × 2.6 cm (Figures 1B, C). This mass was attached to the interatrial septum and demonstrated good mobility.
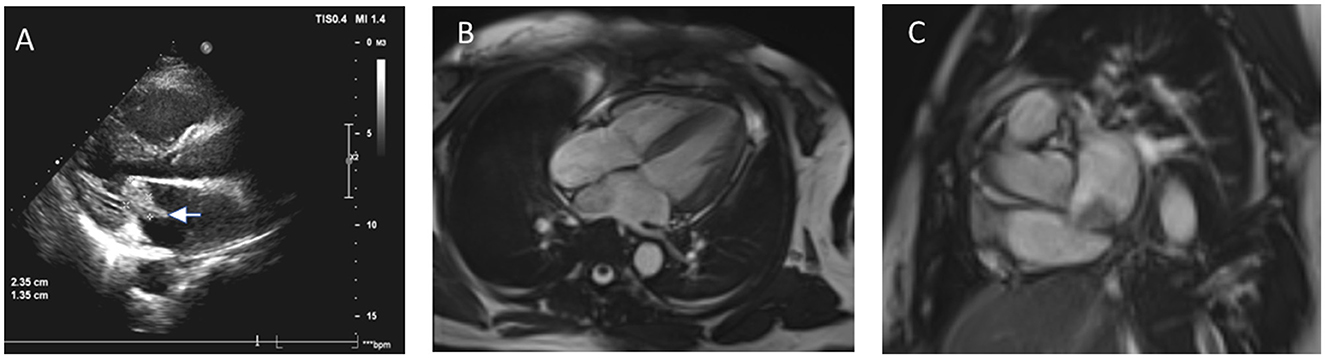
Figure 1. (A) Echocardiogram shows a 2.3 × 1.3 cm hyperechoic mass in the left atrium, attached to the interatrial septum. (B, C) MRI images reveal an irregular mass in the left atrium (~3.9 × 2.6 cm) with iso-intense signal on T1-weighted and hyperintense signal on T2-weighted images, attached to the interatrial septum with visible mobility.
Concurrently, the patient exhibited left-sided limb weakness. CT scans detected hypodense lesions in the left frontal lobe, basal ganglia, and insula, indicating potential cerebral infarction (Figures 2A, B). CTA showed localized stenosis in the M1 segment of the left middle cerebral artery (Figures 2C, D). Brain MRI revealed abnormal signals in multiple brain regions, suggesting infarction foci (Figures 2E–H).
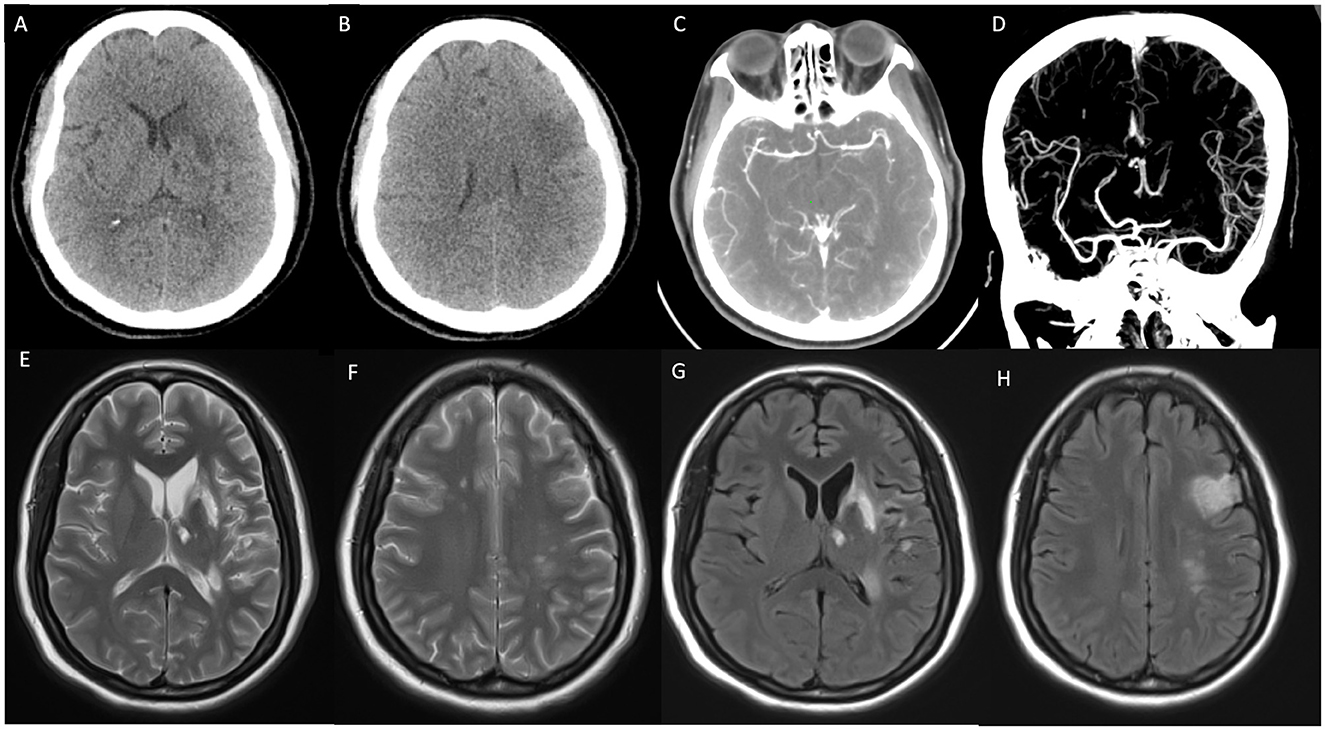
Figure 2. (A, B) Non-enhanced CT (NECT) indicates ischemic infarction in the deep region of the left temporal lobe. (C, D) CT angiography (CTA) shows localized stenosis in the M2 segment of the left middle cerebral artery. (E–H) T2-weighted imaging (T2WI) and T2 FLAIR demonstrate patchy hyperintense signals in the bilateral frontal lobes, left basal ganglia, thalamus, parietal-temporal lobes, and hippocampus.
The initial diagnoses included acute coronary syndrome with non-ST-elevation myocardial infarction, left atrial myxoma, and cerebral infarction. Once the patient's cerebral infarction symptoms stabilized, she underwent left atrial myxoma resection under general anesthesia and cardiopulmonary bypass. The tumor, which was gelatinous and partially ruptured with bleeding, measured 4 × 4 cm and was completely excised along its pedicle.
Histopathological analysis confirmed the diagnosis of left atrial myxoma (Figure 3), revealing tumor cells surrounded by abundant mucinous stroma. Postoperatively, the patient received no additional treatment after discharge.
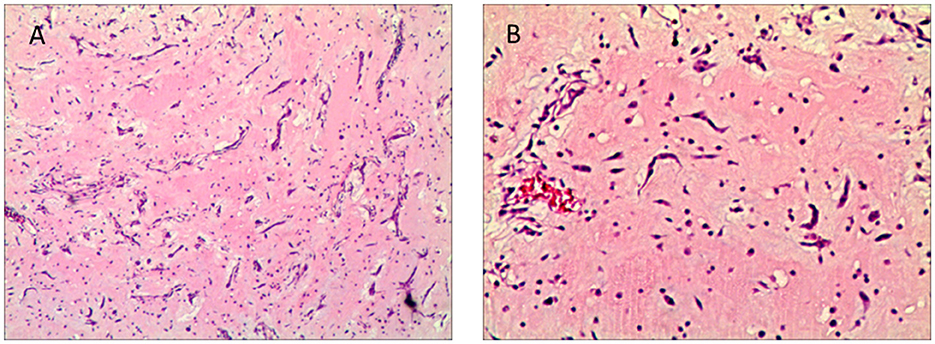
Figure 3. (A, B) Histopathological image of cardiac myxoma (H&E stain, 40 ×, 100×). The image shows cardiac myxoma tissue with round or polygonal tumor cells surrounded by abundant mucinous stroma under hematoxylin and eosin staining at 40×, 100× magnification.
Fifteen months later, the patient presented with new neurological symptoms, including headaches, nausea, and vomiting. Follow-up MRI revealed multiple metastatic lesions in multiple brain regions and signs of cerebral malacia in the left corona radiata and basal ganglia (Figure 4, MRI+C). By the 23 months post-surgery, head CT showed an increase in hyperdense lesions across multiple brain regions, indicative of progressive metastatic disease (Figures 5A, B). Abnormal signals in the left basal ganglia and occipital lobe on T1- and T2-weighted imaging, with partial diffusion restriction in the left temporo-occipital lobe on DWI/ADC (Figures 5C–F), and aneurysmal dilation was observed in segments of the left middle cerebral artery (Figures 5G, H), suggesting potential hemorrhagic metastasis from the myxoma.
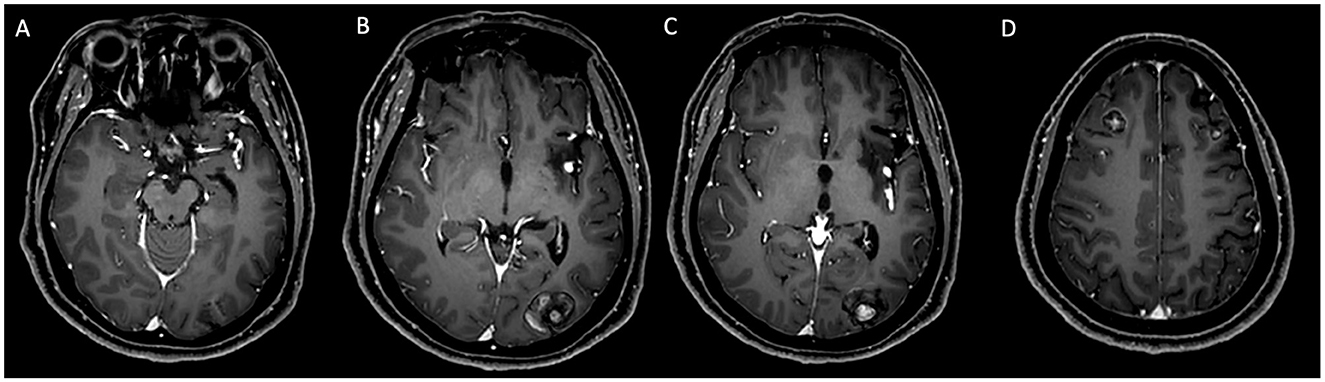
Figure 4. (A–D) MRI with contrast enhancement: follow-up examination 15 months post-surgery. Nodular enhancements were observed in the bilateral frontal lobes, right parietal lobe, and left occipital lobe, with the largest lesion measuring 25 × 20 mm in the left occipital lobe. Additionally, non-enhancing areas were noted in the left corona radiata and basal ganglia.

Figure 5. Follow-up examination 23 months post-surgery. [(A, B); CT] Hyperdense masses with hemorrhagic components observed in the left temporal and occipital lobes. [(C–F); MRI] Abnormal signals in the left basal ganglia and occipital lobe on T1- and T2-weighted imaging, with partial diffusion restriction in the left temporo-occipital lobe on DWI/ADC. [(G, H); T1WI + C] Multiple enhancing nodules observed, with aneurysmal dilation in the M1 and M2 segments of the left middle cerebral artery.
The increase in lesion number and size supported a diagnosis of recurrent cardiac myxoma with multiple intracranial metastatic sites.
The timeline (Figure 6) summarizes the progression from initial presentation through diagnosis, surgical intervention, and subsequent complications, illustrating the disease course and highlighting the need for long-term surveillance in cases of atrial myxoma.
Discussion
Primary cardiac tumors are rare (Ma et al., 2022), with half being myxomas mostly in the left atrium (Aggarwal et al., 2007). Most atrial myxomas are sporadic, but some show familial autosomal dominant inheritance like Carney syndrome, involving multiple tumors and endocrine issues (Reynen, 1995). Here, a patient with a left atrial myxoma had an acute stroke, often misdiagnosed, causing delays. After surgery, inadequate monitoring led to rare metastatic tumors in previously infarcted brain tissue.
Current understanding of this condition is limited, with neither comprehensive intracranial evaluations nor long-term follow-up performed. Atrial myxoma complicated by cerebral embolism often presents as an initial symptom, with embolus detachment leading to narrowing of blood vessels at the infarction site, particularly affecting the middle cerebral artery. In this patient, while metastatic foci developed in the initial infarction area, the supplying arteries progressed from stenosis to aneurysmal dilation, accompanied by tumor hemorrhage. Myxomatous aneurysms are particularly rare, and the mechanisms underlying their formation remain unclear (Hau et al., 2020). Two prevailing theories explain their genesis: (1) the vascular injury theory and (2) the tumoral origin theory. The latter is supported by autopsy pathological evidence and corresponds with the later stages of the disease, where metastatic tumors also exhibit hemorrhagic changes.
The literature lacks adequate description of craniocerebral metastasis mechanisms after atrial myxoma resection (Castaño-Leon et al., 2016). This case report emphasizes the need to assess tumor dissemination risk in patients with atrial myxoma and concurrent acute stroke, challenging the typical surgery outcomes. Even after successful resection, cerebral metastasis risk persists. It highlights rare clinical features of atrial myxoma with neurological complications and postoperative metastasis. For patients with cardiac myxoma, especially those with intracranial lesions, comprehensive evaluations and long-term follow-up are crucial to prevent cerebral metastasis or cerebrovascular diseases. CNS symptoms in patients with a history of cardiac myxoma may indicate cerebral metastasis or aneurysm, requiring prompt and thorough assessment and management (Castaño-Leon et al., 2016; Wan et al., 2019).
Currently, there are no treatment guidelines for systemic metastasis caused by cardiac myxoma. According to the literature, the cumulative recurrence rate of cardiac myxoma is 13%, and recurrences occur in a younger population (42 vs. 57 years), with the risk of recurrence decreasing after 4 years (Elbardissi et al., 2008). Therefore, regular follow-up within 4 years after surgery is recommended, with examinations conducted every 6 months.
Conclusion
Cerebral metastases and aneurysms are rare post-surgical complications of cardiac myxoma, more common in middle-aged females. They often involve the middle cerebral artery and present with vascular events, headaches, and seizures, while hemorrhage and aneurysm rupture are uncommon. Long-term observation is recommended for myxomatous aneurysms. Post-surgery follow-up is vital for detecting potential cerebral complications. Patients with cardioembolic infarctions and coexisting myxoma should be vigilant.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
The studies involving humans were approved by Tongji Hospital, Tongji Medical College, HUST, Wuhan, China. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. The animal study was approved by Tongji Hospital, Tongji Medical College, HUST, Wuhan, China. The study was conducted in accordance with the local legislation and institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XA: Writing – original draft, Writing – review & editing. QS: Writing – original draft, Writing – review & editing, Data curation. XT: Supervision, Data curation, Writing – original draft, Writing – review & editing. YZ: Data curation, Conceptualization, Supervision, Writing – original draft, Writing – review & editing. TZ: Data curation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to express our sincere gratitude to Yu Zhou for his invaluable contribution to refining our manuscript and response letters.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aggarwal, S. K., Barik, R., Sarma, T. C. S. R., Iyer, V. R., Sai, V., Mishra, J., et al. (2007). Clinical presentation and investigation findings in cardiac myxomas: new insights from the developing world. Am. Heart J. 154, 1102–1107. doi: 10.1016/j.ahj.2007.07.032
Alrohimi, A., Putko, B. N., Jeffery, D., Van Dijk, R., Chow, M., and McCombe, J. A. (2019). Cerebral aneurysm in association with left atrial myxoma. Can. J. Neurol. Sci. 46, 637–639. doi: 10.1017/cjn.2019.59
Castaño-Leon, A. M., Hernandez-Lain, A., Maroñas, L., López, P., Ayuso, L. L., Ramos, A., et al. (2016). Pathology-confirmed cerebral arterial invasion and recurrent multiple brain metastasis from cardiac myxoma without evidence of disease after surgery and radiotherapy. Clin. Neuropathol. 35, 84–88. doi: 10.5414/NP300900
Elbardissi, A. W., Dearani, J. A., Daly, R. C., Mullany, C. J., Orszulak, T. A., Puga, F. J., et al. (2008). Survival after resection of primary cardiac tumors: a 48-year experience. Circulation 118, S7–S15. doi: 10.1161/CIRCULATIONAHA.107.783126
Hau, M., Poon, T. L., and Cheung, F. C. (2020). Neurological manifestations of atrial myxoma and stereotactic radiosurgery for metastatic aneurysms. J. Radiosurg. SBRT 6, 329–331.
Jaravaza, D. R., Lalla, U., Zaharie, S. D., and de Jager, L. J. (2021). Unusual presentation of atrial myxoma: a case report and review of the literature. Am. J. Case Rep. 22:e931437. doi: 10.12659/AJCR.931437
Ma, K., Zhao, D., Li, X., Duan, H., Yan, C., Wang, S., et al. (2022). Case report: multiple brain metastases of atrial myxoma: clinical experience and literature review. Front. Neurol. 13:1046441. doi: 10.3389/fneur.2022.1046441
Reynen, K. (1995). Cardiac myxomas. N. Engl. J. Med. 333, 1610–1617. doi: 10.1056/NEJM199512143332407
Waliszewska-Prosół, M., Zimny, A., Chojdak-Łukasiewicz, J., Zagrajek, M., and Pardowski, B. (2018). Multiple fusiform cerebral aneurysms detected after atrial myxoma resection: a report of two cases. Kardiol. Pol. 76:1571. doi: 10.5603/KP.2018.0220
Keywords: left atrial myxoma, tumor resection, ischemic stroke, brain metastasis, aneurysm, radiological imaging
Citation: Ai X, Shao Q, Tian X, Zhou Y and Zhou T (2024) Neurological complications of left atrial myxoma: a case report on stroke with left atrial myxoma and postoperative brain metastasis and cerebral aneurysm. Front. Neuroimaging 3:1524901. doi: 10.3389/fnimg.2024.1524901
Received: 08 November 2024; Accepted: 30 November 2024;
Published: 19 December 2024.
Edited by:
Jiazheng Wang, Philips Research, NetherlandsReviewed by:
Yanlong Jia, Second Affiliated Hospital of Shantou University Medical College, ChinaDing Zhang, Rochester Regional Health, United States
Copyright © 2024 Ai, Shao, Tian, Zhou and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tiantian Zhou, MTAxNzU3MDU3NUBxcS5jb20=
 Xudong Ai
Xudong Ai Qingqing Shao
Qingqing Shao Xueyan Tian2
Xueyan Tian2