
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nephrol., 21 March 2025
Sec. Pediatric Nephrology
Volume 5 - 2025 | https://doi.org/10.3389/fneph.2025.1539776
Introduction: This study aims to describe the outcome of levamisole (LEVA) treatment in children with frequently relapsing nephrotic syndrome (FRNS).
Methods: This prospective cohort study was conducted at the Department of Pediatric Nephrology, Sindh Institute of Urology and Transplantation from 1 January 2019 to 31 December 2020. Children aged 1–18 years diagnosed with FRNS were included. LEVA was started with a dose of 2–2.5 mg/kg every other day for 2 years along with low-dose prednisolone in the first year.
Results: A total of 70 children with FRNS were enrolled in the study. The median age was 7.5 [interquartile range (IQR) 5.0–9.6 years] with a slight predominance of boys (42, 60%). The mean number of relapses and cumulative dose of steroids significantly decreased after 2 years of LEVA therapy and during the 1-year follow-up. LEVA non-response was observed in half of the studied participants (28, 46%). The responders and non-responders were comparable in terms of cumulative dose of steroids and number of relapses in the year prior to starting LEVA [5,242 ± 1,738 versus 4,910 ± 1,469 (p-value = 0.52) and 5.4 ± 2.4 versus 5.2 ± 2.1 (p-value = 0.85)].
Conclusion: LEVA therapy resulted in a substantial reduction in the frequency of relapses and cumulative dosage, indicating its potential as an alternative option for children with relapsing disease.
Idiopathic nephrotic syndrome is the most common glomerular disease in children, affecting 2.92/100,000 children per year (1). Fortunately, 80%–85% of children respond to corticosteroid therapy at the first presentation (2). However, nearly 50% keep relapsing with either a steroid-dependent or frequently relapsing pattern (3). This cohort of children is at risk of steroid toxicity and needs sparing therapies to avoid deleterious effects (4).
The choice of a second-line agent has been long debated. In 2020, the Cochrane systematic review concluded that the choice between levamisole (LEVA), mycophenolate mofetil, calcineurin inhibitors, and cyclophosphamide must be left to physician preference (5). The Kidney disease improving global outcomes (KDIGO) guidelines in 2021 suggested the use of LEVA and cyclophosphamide specifically in frequently relapsing nephrotic syndrome (FRNS) (6). The Indian Society of Pediatric Nephrology (ISPN) recommends LEVA when there is a relapse on steroids of less than 1mg/kg on alternate days, no complicated relapse, and development of steroid toxicity (7). The duration and frequency (daily versus alternate day) of therapy with LEVA are also debated (8).
LEVA is an anthelminthic drug that has been used in the treatment of nephrotic syndrome since the 1980s (9). Apart from the modulation of the immune system with its alteration of T and B cells, LEVA has shown a direct effect on podocytes to achieve remission (10). LEVA offers the added advantage of fewer adverse effects and lower cost (11). Kuzma-Mroczkowska et al. showed that LEVA leads to a reduction in the number of relapses in both steroid-dependent and frequently relapsing nephrotic syndromes (12). Kiruba et al. has shown better efficacy of LEVA in children with frequently relapsing nephrotic syndrome (13).
In general, our children receive a high dose of steroids because of multiple relapses, and using LEVA could also postpone the introduction of CNI, thereby reducing the risk of its potential nephrotoxicity. We present the results of a prospective cohort study documenting the outcomes of a 2-year alternate-day LEVA therapy in children with frequently relapsing nephrotic syndrome.
This prospective cohort study utilized non-probability convenience sampling and was conducted at the outpatient Department of Pediatric Nephrology, Sindh Institute of Urology and Transplantation, Karachi. The study received approval from the ethical review committee. All children diagnosed with frequently relapsing nephrotic syndrome between 1 January 2019 and 31 December 2020 were enrolled.
Children aged 1 to 18 years with FRNS who had no prior use of immunosuppression drugs and were in complete remission at the time LEVA was prescribed were included in the study. The exclusion criteria encompassed children with steroid-dependent nephrotic syndrome, primary or secondary resistant nephrotic syndrome, or infantile or congenital nephrotic syndrome.
Before enrolling participants in the study, the diagnosis of FRNS, treatment protocol, and monitoring during therapy were established and published as per the national consensus recommendations (14). FRNS was defined as two relapses within 6 months of initial response with steroids or four relapses in any 12-month period (12). The relapse was treated with prednisolone 2 mg/kg/day for 2 weeks and then 1.5 mg/kg/day for 4 weeks. Complete remission was achieved before initiating LEVA.
LEVA was started with a dose of 2-2.5mg/kg on alternate days for 2 years. Steroids were tapered by 0.5 mg/kg every 2 weeks and a minimal dose of 0.25 mg/kg was continued for the first year. The children were monitored with complete blood count and liver function tests. Relapses during the study period were treated with the standard duration of steroid therapy, after which the original study protocol was resumed. Children who experienced two relapses within any 6-month period of the study were classified as LEVA non-responders, and an alternative immunosuppressant drug was considered.
A structured proforma was used to document the baseline demographics, duration since diagnosis of nephrotic syndrome, and pattern of FRNS (two relapses in 6 months or four in 12 months). Data on cumulative steroid exposure were collected for the year preceding the FRNS diagnosis, during the 2-year study period, and for 1 year after completing therapy.
The total number of children with FRNS seen in our institute in a year is 70. Based on an estimate of the efficacy of the alternate-day LEVA therapy of 82% with a margin of error of 5% and a 95% confidence level, a total of 55 patients were required. However, assuming that 5% would be lost to follow-up, a total of 60 patients was needed for this study (13).
SPSS version 26 was used for the statistical analysis. Normally distributed continuous variables were expressed as means with standard deviations and the rest as medians with interquartile ranges (IQRs). The qualitative variables were reported as percentages or ranges. Appropriate tests of significance were applied. A p-value < 0.05 was considered significant.
We prospectively enrolled 70 children with FRNS in the study. Of these, 9 (13%) could not complete the treatment protocol due to the reasons mentioned in Figure 1.
The baseline characteristics of the study cohort were comparable and are described in Table 1.
The median age was 7.5 (IQR: 5–9.6 years) with a slight predominance of boys (42, 60%). The majority of the children (57, 81.4%) were diagnosed with FRNS with the pattern of four relapses in a 12-month period. The median duration of nephrotic syndrome prior to enrollment in the study was 20 (IQR: 12.7–40.2 months) and the prescribed dose of LEVA was 2.3 (IQR: 2–2.5 mg/Kg) alternate day.
In the study cohort, 61 children completed 24 months of LEVA therapy and a 12-month follow-up period. The number of relapses significantly decreased in the period from 1 year before starting LEVA to during treatment either with LEVA and steroids or LEVA without steroids, with means of 3.6 ± 0.78, 0.87 ± 0.86, and 0.52 ± 0.73, respectively (p-value = 0.00). Similarly, the cumulative dose of steroids in the preceding year before starting LEVA was 5,067 ± 1,396 mg/m2. This decreased to 3,785 ± 1,636 mg/m2 during the 2 years of therapy, and further decreased to 1,856 ± 1,627 mg/m2 in the year following completion of LEVA (p-value = 0.00). This has been graphically shown in Figure 2 and the analysis excluded children with no response to LEVA.
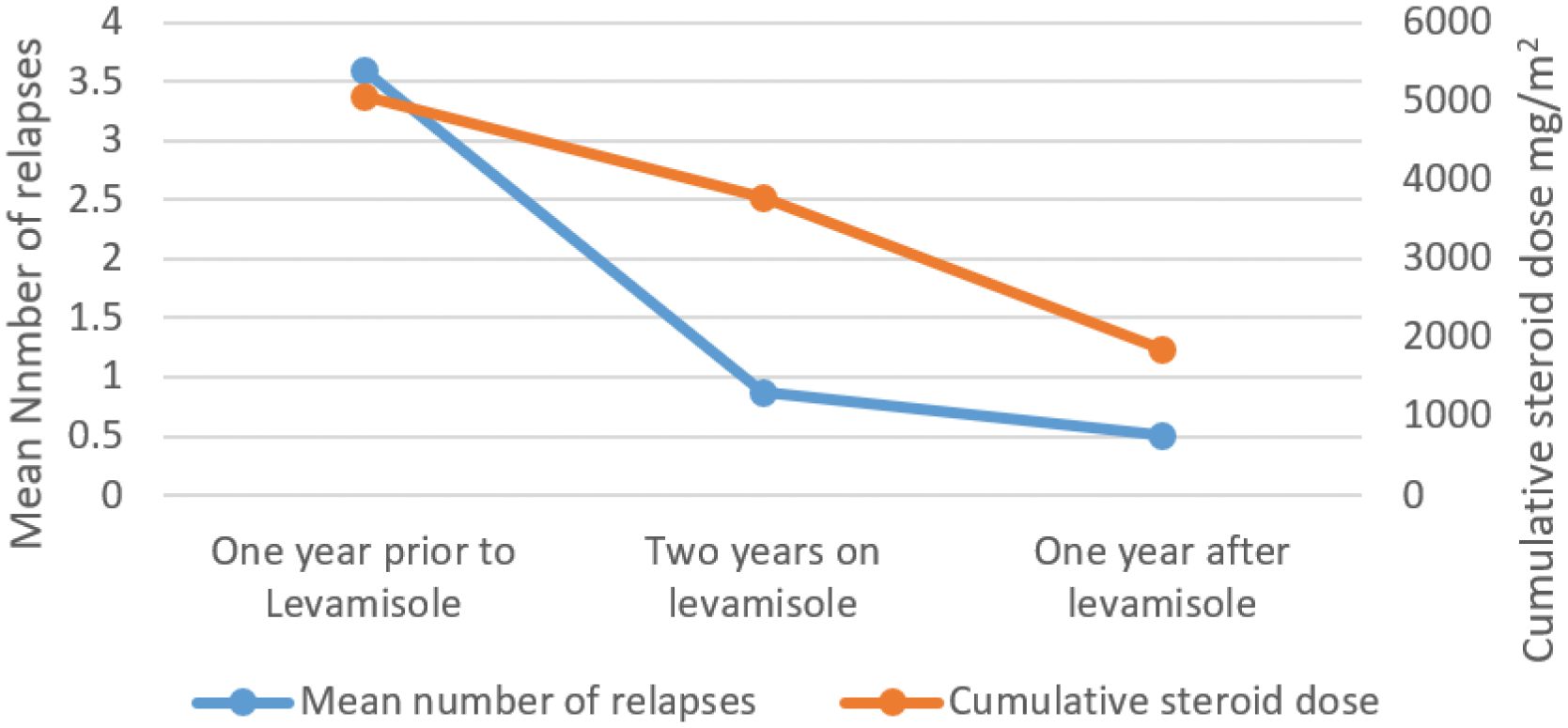
Figure 2. Effect of Levamisole on cumulative dose of steroids and mean number of relapses in the study cohort.
Non-response to therapy showed no significant association with gender (18 boys versus 10 girls, p = 0.30), age under 7 years (16 versus 12, p = 0.13), or a duration of more than 24 months from nephrotic syndrome diagnosis to the development of FRNS (16 versus 12, p = 0.42).
The majority of LEVA non-responders (23, 82%) required oral cyclophosphamide as an additional drug to achieve remission. Four children (14%) developed secondary steroid resistance and required a kidney biopsy which showed minimal change disease; cyclosporine was prescribed for this. Although one child (4%) was categorized as a LEVA non-responder, he attained sustained remission prior to the initiation of further immunosuppression. Despite administration of cyclophosphamide, 12 (52%) continued to relapse, with infrequent relapse patterns in 7 (58%) and persistent FRNS in 5 (42%), who subsequently required renal biopsies and treatment with calcineurin inhibitors.
LEVA showed a relatively better response in 33 (54%) children at the end of the therapy. In the 12-month follow-up period, 17 (52%) showed sustained completed remission, 9 (27%) had an infrequently relapsing course, and 6 (18%) demonstrated FRNS for which oral cyclophosphamide was administered. One child (3%) presented with secondary SRNS, a kidney biopsy showed FSGS, and cyclosporine was started.
Nine children (13%) could not complete the study protocol and follow-up period. Three (34%) were lost to follow-up and one (11%) showed non-adherence, so cyclophosphamide was prescribed considering the shorter duration of therapy. Complicated relapse of NS with septic shock was seen in one patient (11%). Reversible derangement of liver function tests (negative hepatitis A and E profiles) and leucopenia were documented in two (22%) and one (11%) children respectively. A 4-year-old boy (11%) presented at 18 months of therapy with malaise, generalized bodyache, and non-specific joint pain for a few days. He had normal renal function, his urine was negative for protein and RBCs, and ANA and rheumatoid factor were negative. A further workup revealed ANCA MPO positivity. LEVA was discontinued and analgesics were advised. During subsequent follow-ups, his symptoms resolved within 4 weeks and ANCA MPO titers gradually declined to negative in 12 months; he remained in sustained remission at 36 months.
The steroid-sparing effect of LEVA has been utilized for a long time. Our study selected a homogenous population of children with FRNS and prescribed a uniform protocol for 2 years along with 1-year follow-up after completion of the therapy. The median age of the study participants was 7.5 years (5 – 9.6) with a slight predominance of boys (42, 60%). The age is comparable to the regional data of Sinha et al. However, they had a higher proportion of boys (85%) (14). The median duration of nephrotic syndrome prior to starting LEVA was 20 months (12.7–40.2 months), which is a notably longer period than the multicenter randomized trial conducted by Gruppen et al., where they observed for 12 months (15). This correlates with the majority of our cohort being categorized as FRNS on the basis of four relapses in 12 months (57, 81%).
We prescribed LEVA for a total duration of 24 months and a similar duration was studied by Kiruba et al. and Ekambaram et al. (13, 16). Nonetheless, the duration of LEVA is variable in various other studies (15, 17). Even the recent guidelines on steroid-sensitive nephrotic syndrome lack uniformity on the duration of LEVA (6, 7, 18, 19). However, the ISPN advocates LEVA a dose of 2–2.5 mg/kg every other day (EOD) for 2–3 years (7). The most commonly studied dose of LEVA is 2–2.5 mg/kg EOD and we prescribed a median dose of 2.2 mg/Kg EOD (IQR: 2–2.5). Recently, there has been an inclination towards a daily dose of LEVA, especially in steroid-dependent FRNS and non-responders to the EOD schedule (17, 20). However, none of the international guidelines have recognized it so far. The concomitant administration of steroids with LEVA is very inconsistent and we continued low-dose steroids in the first year only. The cumulative dose of steroids prescribed in our study is comparable to other studies, as shown in Table 2.
We observed a significant reduction in exposure to steroids with LEVA treatment. Alsaran et al. demonstrated a proportionately greater reduction from 4,100 mg/m2 to 900 mg/m2. Similarly, the mean number of relapses prior to the LEVA in our study was 3.6 ± 0.78 and this reduced to 0.52 ± 0.73 (p-value 0.00) in the year after completion of the therapy. Our cohort exhibited a relatively better frequency of relapses compared to Alsaran et al. and Kiruba et al., as they reported 1.6 and 1.1 relapses during therapy, respectively (13, 21). This may be due to prolonging steroid therapy by a year in our protocol.
Of the children who completed the study, LEVA therapy resulted in responses in 33 (54%), and the rest (28, 46%) were categorized as non-responders. Moorani et al. reported a sustained remission rate of 76%, while Grupen et al. documented a 26% rate at 1 year, and Sinha et al. reported a rate of 34% (14, 15, 17). The wide discrepancy in the outcome may be due to the selection of patients (FRNS versus SDNS), concomitant administration of steroids, and duration of LEVA therapy. The response and non-response groups of children in our cohort to LEVA were comparable in terms of age, dose of LEVA, and cumulative doses of steroids.
Out of the nine (13%) who failed to complete the study protocol, three (33%) experienced drug effects. One child developed a transient rise in transaminases, while another experienced a rise in leucopenia. Although these children had reversible effects, as per our study protocol, we decided to switch them to another steroid-sparing agent. Abygunawardena et al. reported three children with deranged liver functions and one with neutropenia in a cohort of 72 children (20). One of our children with MPO-positive ANCA was identified through non-specific symptoms such as arthralgia and malaise. He developed symptoms after 12 months of therapy, highlighting that, although rare, long-term use can lead to ANCA positivity (22, 23). The same pattern was highlighted in the trial conducted by Grupen et al. (15).
The IPNA consensus guidelines now recommend 6-monthly monitoring of ANCA profile when on LEVA therapy (19).
Our study has certain limitations, such as its single-center, non-randomized design and a 13% attrition rate, which raise questions about its internal validity. Additionally, no distinction was made between relapses occurring spontaneously and those triggered by infections. However, the study’s strength lies in selecting a naive cohort of children with FRNS who had never been exposed to other steroid-sparing drugs. They were treated with a uniform protocol and prospectively followed-up.
In conclusion, our study demonstrated a positive response to LEVA with a significant reduction in steroid exposure and fewer relapses. This underscores the potential of LEVA as a steroid-sparing agent for frequently relapsing nephrotic syndrome. Further research with refined patient selection criteria is needed to optimize outcomes and clarify LEVA’s therapeutic role in this patient population.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the ethical review committee (SIUT-ERC-2019/A-157). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
SK: Conceptualization, Data curation, Formal Analysis, Writing – original draft, Writing – review & editing. IB: Data curation, Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. AZ: Data curation, Methodology, Writing – review & editing. AL: Data curation, Project administration, Supervision, Writing – review & editing. SH: Conceptualization, Project administration, Supervision, Validation, Writing – original draft.
The author(s) declare that no financial support was received for the research and/or publication of this article.
Iqbal Mujtaba.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Veltkamp F, Rensma LR, Bouts AHM, LEARNS consortium. Incidence and relapse of idiopathic nephrotic syndrome: meta-analysis. Pediatrics. (2021) 148:e2020029249. doi: 10.1542/peds.2020-029249
2. Trautmann A, Schnaidt S, Lipska-Ziętkiewicz BS, Bodria M, Ozaltin F, Emma F, et al. Long-term outcome of steroid-resistant nephrotic syndrome in children. J Am Soc Nephrol. (2017) 28:3055–65.
3. Robinson CH, Parekh RS. Treating frequently relapsing and steroid-dependent nephrotic syndrome: to obi or not to obi, that is the question. Clin J Am Soc Nephrol. (2023) 18:1527–9.
4. Croitoru A, Balgradean M. Treatment-associated side effects in patients with steroid-dependent nephrotic syndrome. Maedica (Bucur). (2022) 17:285–90.
5. Hahn D, Samuel SM, Willis NS, Craig JC, Hodson EM. Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev. (2024) 8:CD001533. doi: 10.1002/14651858.CD001533.pub2
6. Rovin BH, Adler SG, Barratt J, Bridoux F, Burdge KA, Chan TM, et al. Executive summary of the KDIGO 2021 guideline for the management of glomerular diseases. Kidney Int. (2021) 100:753–79. doi: 10.1016/j.kint.2021.05.015
7. Sinha A, Bagga A, Banerjee S, Mishra K, Mehta A, Agarwal I, et al. Steroid sensitive nephrotic syndrome: revised guidelines. Indian Pediatr. (2021) 58:461–81. doi: 10.1007/s13312-021-2217-3
8. Banerjee S, Sengupta J, Sinha R, Chatterjee S, Sarkar S, Akhtar S, et al. Daily compared with alternate-day levamisole in pediatric nephrotic syndrome: an open-label randomized controlled study. Pediatr Nephrol. (2024) 39:2969–77. doi: 10.1007/s00467-024-06402-9
9. Davin JC, Merkus MP. Levamisole in steroid-sensitive nephrotic syndrome of childhood: the lost paradise? Pediatr Nephrol. (2005) 20:10–4.
10. Veissi ST, van den Berge T, van Wijk JAE, van der Velden T, Classens R, Lunsonga L, et al. Levamisole modulation of podocytes’ Actin cytoskeleton in nephrotic syndrome. Biomedicines. (2023) 11:3039. doi: 10.3390/biomedicines11113039
11. Bhatt GC, Patel B, Das RR, Malik S, Bitzan M, Mishra NR. Efficacy and safety of levamisole in childhood nephrotic syndrome: A meta-analysis. Indian J Pharmacol. (2023) 55:43–52. doi: 10.4103/ijp.ijp_673_21
12. Kuźma-Mroczkowska E, Skrzypczyk P, Pańczyk-Tomaszewska M. Levamisole therapy in children with frequently relapsing and steroid-dependent nephrotic syndrome: a single-center experience. Cent Eur J Immunol. (2016) 41:243–7. doi: 10.5114/ceji.2016.63122
13. Kiruba Samuel EM, Krishnamurthy S, Bhanudeep S, Muske S. Levamisole in frequently-relapsing and steroid-dependent nephrotic syndrome. Indian Pediatr. (2017) 54:831–4. doi: 10.1007/s13312-017-1144-9
14. Bajeer IA, Lanewala AA, Khatri S, Hashmi S, Moorani K, et al. Consensus guidelines for the treatment of Nephrotic Syndrome in Children of Pakistan Endorsed by Pakistan Pediatric Association- Nephrology Group. Pakistan J Kidney Dis. (2019) 3(8). doi: 10.53778/pjkd38101
15. Sinha A, Puraswani M, Kalaivani M, Goyal P, Hari P, Bagga A. Efficacy and safety of mycophenolate mofetil versus levamisole in frequently relapsing nephrotic syndrome: an open-label randomized controlled trial. Kidney Int. (2019) 95:210–8. doi: 10.1016/j.kint.2018.08.039
16. Gruppen MP, Bouts AH, Jansen-van der Weide MC, Merkus MP, Zurowska A, Maternik M, et al. A randomized clinical trial indicates that levamisole increases the time to relapse in children with steroid-sensitive idiopathic nephrotic syndrome. Kidney Int. (2018) 93:510–8. doi: 10.1016/j.kint.2017.08.011
17. Ekambaram S, Mahalingam V, Nageswaran P, Udani A, Geminiganesan S, Priyadarshini S. Efficacy of levamisole in children with frequently relapsing and steroid-dependent nephrotic syndrome. Indian Pediatr. (2014) 51:371–3. doi: 10.1007/s13312-014-0419-7
18. Moorani KN, Zubair AM, Veerwani NR, Hotchandani HJ. Efficacy of Levamisole in children with Frequent Relapsing and Steroid Dependent Nephrotic Syndrome at Tertiary Care Center-Karachi. Pak J Med Sci. (2020) 36:1193–8. doi: 10.12669/pjms.36.6.2337
19. Esezobor C, Ademola AD, Adetunji AE, Anigilaje EA, Batte A, Jiya-Bello FN, et al. Management of idiopathic childhood nephrotic syndrome in sub-Saharan Africa: Ibadan consensus statement. Kidney Int. (2021) 99:59–67. doi: 10.1016/j.kint.2020.07.045
20. Trautmann A, Boyer O, Hodson E, Bagga A, Gipson DS, Samuel S, et al. IPNA clinical practice recommendations for the diagnosis and management of children with steroid-sensitive nephrotic syndrome. Pediatr Nephrol. (2023) 38:877–919.
21. Abeyagunawardena AS, Karunadasa U, Jayaweera H, Thalgahagoda S, Tennakoon S, Abeyagunawardena S. Efficacy of higher-dose levamisole in maintaining remission in steroid-dependant nephrotic syndrome. Pediatr Nephrol. (2017) 32:1363–7.
22. Alsaran K, Mirza K, Al-Talhi A, Al-Kanani E. Experience with second line drugs in frequently relapsing and steroid dependent childhood nephrotic syndrome in a large Saudi center. Int J Pediatr Adolesc Med. (2017) 4:66–70. doi: 10.1016/j.ijpam.2017.03.002
23. Bernardi S, Innocenti S, Charbit M, Boyer O. Late onset of ANCA vasculitis as a side effect of levamisole treatment in nephrotic syndrome. Medicina (Kaunas). (2022) 58:650. doi: 10.3390/medicina58050650
24. Elmas AT, Tabel Y, Elmas ÖN. Short- and long-term efficacy of levamisole in children with steroid-sensitive nephrotic syndrome. Int Urol Nephrol. (2013) 45:1047–55. doi: 10.1007/s11255-012-0241-x
Keywords: frequently relapsing nephrotic syndrome, levamisole, childhood, outcome, prospective
Citation: Khatri S, Bajeer IA, Zubair A, Lanewala AAA and Hashmi S (2025) Short-term outcome of levamisole in frequently relapsing nephrotic syndrome: a single-center prospective cohort study. Front. Nephrol. 5:1539776. doi: 10.3389/fneph.2025.1539776
Received: 04 December 2024; Accepted: 12 February 2025;
Published: 21 March 2025.
Edited by:
Mara Medeiros, Federico Gómez Children’s Hospital, MexicoReviewed by:
Ramona Stroescu, Victor Babes University of Medicine and Pharmacy, RomaniaCopyright © 2025 Khatri, Bajeer, Zubair, Lanewala and Hashmi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sabeeta Khatri, c2FiZWV0YWtoYXRyaUBob3RtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.