
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CORRECTION article
Front. Microbiol. , 18 March 2025
Sec. Antimicrobials, Resistance and Chemotherapy
Volume 16 - 2025 | https://doi.org/10.3389/fmicb.2025.1584655
This article is a correction to:
Understanding the burden of antibiotic resistance: a decade of carbapenem-resistant Gram-negative bacterial infections in Italian intensive care units
 Giovanni Scaglione1,2†
Giovanni Scaglione1,2† Matilde Perego3†
Matilde Perego3† Marta Colaneri1,4*
Marta Colaneri1,4* Camilla Genovese1,2
Camilla Genovese1,2 Fabio Brivio1,2
Fabio Brivio1,2 Alice Covizzi1
Alice Covizzi1 Bruno Viaggi5
Bruno Viaggi5 Alessandra Bandera6,7
Alessandra Bandera6,7 Andrea Gori1,2,4*
Andrea Gori1,2,4* Stefano Finazzi3‡
Stefano Finazzi3‡ Emanuele Palomba1‡
Emanuele Palomba1‡A corrigendum on
Understanding the burden of antibiotic resistance: a decade of carbapenem-resistant Gram-negative bacterial infections in Italian intensive care units
by Scaglione, G., Perego, M., Colaneri, M., Genovese, C., Brivio, F., Covizzi, A., Viaggi, B., Bandera, A., Gori, A., Finazzi, S., and Palomba, E. (2024). Front. Microbiol. 15:1405390. doi: 10.3389/fmicb.2024.1405390
In the published article, there was an error in Figure 3, page 6 as published.
In Panel B of Figure 3 the percentage of carbapenem-resistant strains was not correct.
The corrected Figure 3 and its caption appear below.
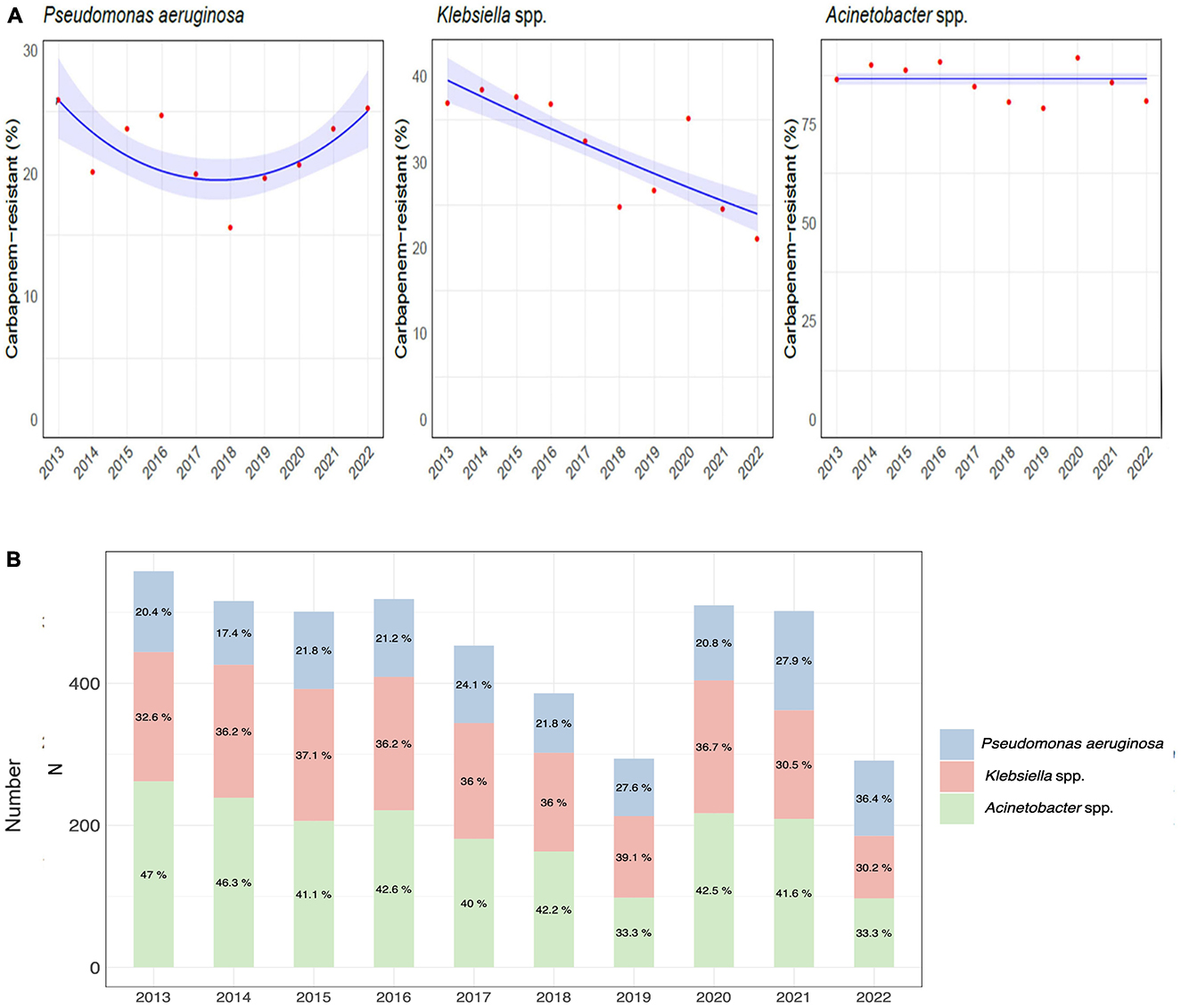
Figure 3. Etiology of hospital-acquired infections caused by carbapenem-resistant gram-negative bacteria over the course of the study. (A) Trend models of the carbapenem-resistance of Pseudomonas aeruginosa, Klebsiella spp., and Acinetobacter spp. (B) Distribution and percentage of hospital-acquired infections caused by carbapenem-resistant Pseudomonas aeruginosa, Klebsiella, and Acinetobacter species.
In the published article, there was an error in Figure 6, page 8 as published.
In Figure 6 the percentage of carbapenem-resistant strains was not correct.
The corrected Figure 6 and its caption appear below.
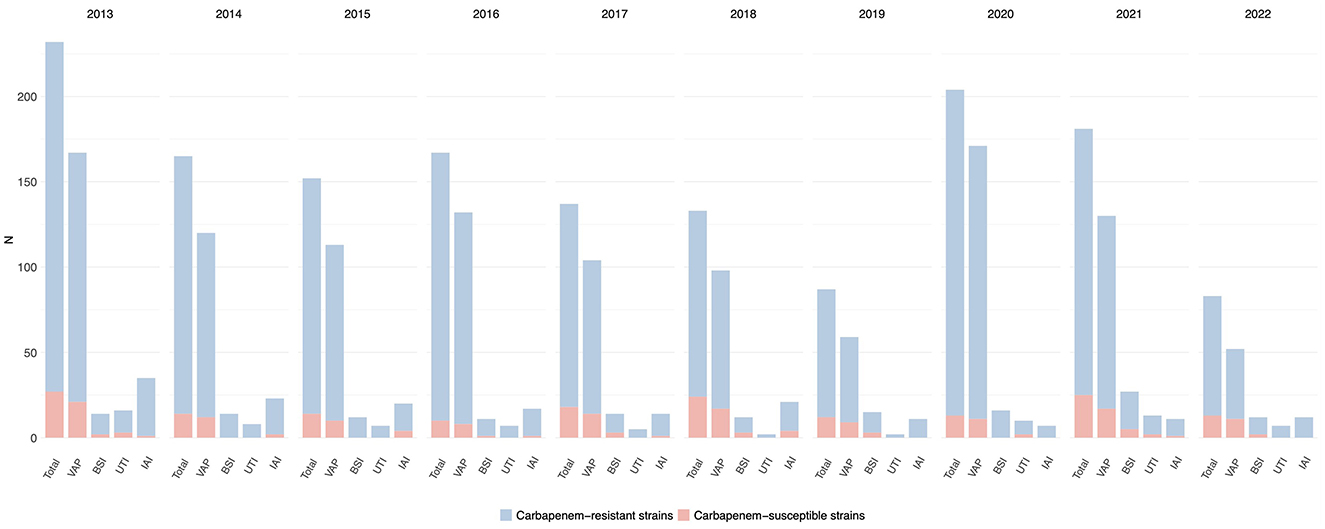
Figure 6. Distribution of infections caused by Acinetobacter spp. acquired in intensive care during the study period, overall and for infection site, with the relative prevalence of carbapenem-resistant strains.
In the published article, there was an error in Supplementary Table 2. The percentages of carbapenem-resistant Acinetobacter spp. strains were not correct. The corrected supplementary table has been published in the original article.
In the published article, there was an error in Supplementary Table 5. The percentages of carbapenem-resistant Acinetobacter spp. strains were not correct. The corrected supplementary table has been published in the original article.
In the published article, there was an error. The percentages of carbapenem-resistant Acinetobacter spp. strains were not correct.
A correction has been made to Results, 3.2.3 Acinetobacter spp. Infections, page 7.
This sentence previously stated:
“Acinetobacter spp. was the least frequently isolated GNB of the three in study (2183/25966, 8.4%) and displayed the overall lowest rates of resistance to carbapenems (290/2183, 13.3%). This pathogen was mainly responsible for VAP (1146/9260, 12.4%) and to a lesser extent for IAI (171/1921, 9.0%), BSI (147/2940, 5.0%), and UTI (77/1959, 3.9%). The carbapenem resistance proportion was the highest in BSI (19/147, 13.0%), followed by VAP (130/1146, 11.3%), UTI (7/77, 9.1%) and IAI (14/171, 8.2%). Carbapenem-resistant Acinetobacter spp. rates varied greatly from one year to the other and this pathogen was most prevalent in the years 2019 (21%) and 2022 (19.2%)”
The corrected sentence appears below:
“Acinetobacter spp. was the least frequently isolated GNB of the three in study (2,183/25,966, 8.4%) and displayed the overall highest rates of resistance to carbapenems (1,893/2,183, 86.7%). This pathogen was mainly responsible for VAP (1146/9260, 12.4%) and to a lesser extent for IAI (171/1,921, 9.0%), BSI (147/2,940, 5.0%), and UTI (77/1959, 3.9%). The carbapenem resistance proportion was the highest in IAI (157/171, 91.8%), followed by UTI (70/77, 90.1%), VAP (1,016/1146, 88.7%), and BSI (130/147, 88.4%). Carbapenem-resistant Acinetobacter spp. rates varied greatly from one year to the other, with a peak of 91.9% in 2020.”
A correction has been made to Discussion, page 7.
This sentence previously stated:
“The findings of our study shed light on the epidemiology of HAIs in Italian ICUs over a ten-year period. Our analysis reveals a substantial burden of HAIs, with an average of 1.5 infections per patient over the study period, with high prevalence of CR-GNB, particularly Pseudomonas aeruginosa, Klebsiella and Acinetobacter species. This trend was mainly driven by Klebsiella spp. and Pseudomonas aeruginosa, with 31.4% and 21.8% of isolate showing this susceptibility profile, respectively. In particular, CR-GNB accounted for a third of IAI and a quarter of each VAP, BSI and UTI caused by these pathogens. Finally, during the SARS-CoV-2 pandemic, ICU-HAIs showed a peak in both incidence and CR-GNB rates, in contrast to a previously declining trend.”
The corrected sentence appears below:
“The findings of our study shed light on the epidemiology of HAIs in Italian ICUs over a ten-year period. Our analysis reveals a substantial burden of HAIs, with an average of 1.5 infections per patient over the study period, with high prevalence of CR-GNB, particularly Pseudomonas aeruginosa, Klebsiella and Acinetobacter species. This trend was mainly driven by Klebsiella spp. and Pseudomonas aeruginosa, with 31.4% and 21.8% of isolate showing this susceptibility profile, respectively. In particular, CR-GNB accounted for a third of IAI and a quarter of each VAP, BSI and UTI caused by these pathogens. Notably, over the course of the decade, up to 90% of Acinetobacter spp. isolates retrieved showed carbapenem-resistant. Finally, during the SARS-CoV-2 pandemic, ICU-HAIs showed a peak in both incidence and CR-GNB rates, in contrast to a previously declining trend.”
A correction has been made to Discussion, page 8.
This sentence previously stated:
“In our cohort, Acinetobacter spp. caused less than one tenth of all ICU-acquired infections and showed the overall lowest rates of resistance to carbapenems (13.3%). This data is in contrast with European and national reports, where carbapenem-resistant strains account for up to one third of all isolates globally, with even higher percentages in Italy, where carbapenem-resistance in Acinetobacter baumannii reaches peaks of 88% (European Centre for Disease Prevention and Control, 2022). These differences may be explained by the higher prevalence of carbapenem-resistant strains in settings different than ICU, as other European studies have already observed (Said et al., 2021; Kinross et al., 2022). Furthermore, our analysis only included infections diagnosed by a physician and did not consider respiratory, intestinal and device colonisations, which are often characteristic of Acinetobacter species. Finally, we considered all Acinetobacter spp. strains, not focusing only on Acinetobacter baumannii, which may have partially lowered the overall prevalence of carbapenem-resistance. As confirmed by our findings, infections caused by Acinetobacter spp. typically exhibit a varied distribution, marked by sporadic outbreaks, thereby serving as an indicator for evaluating infection control and prevention strategies. The emergence of the SARS-CoV-2 pandemic has accentuated these distinctive patterns, highlighting avenues for enhancing management approaches (Mangioni et al., 2023b).”
The corrected sentence appears below:
“In our cohort, Acinetobacter spp. caused less than one tenth of all ICU-acquired infections and showed the overall highest rates of resistance to carbapenems (86.7%). This data is in line with European and national reports, where carbapenem-resistant strains account for up to one third of all isolates globally, with even higher percentages in Italy, where carbapenem-resistance in Acinetobacter baumannii reaches peaks of 88% (European Centre for Disease Prevention and Control, 2022). These findings confirm an alarmingly high prevalence of carbapenem-resistant strains in infections among critically ill patients, a trend previously observed in other European studies outside the ICU (Said et al., 2021; Kinross et al., 2022). As showed by our data, infections caused by Acinetobacter spp. typically exhibit a varied distribution, marked by sporadic outbreaks, thereby serving as an indicator for evaluating infection control and prevention strategies. The emergence of the SARS-CoV-2 pandemic has accentuated these distinctive patterns, highlighting avenues for enhancing management approaches (Mangioni et al., 2023b).”
The authors apologize for these errors and state that this does not change the scientific conclusions of the article in any way. The original article has been updated.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Keywords: epidemiology, multidrug-resistant, intensive care unit, gram-negative, carbapenem-resistant, hospital-acquired infections
Citation: Scaglione G, Perego M, Colaneri M, Genovese C, Brivio F, Covizzi A, Viaggi B, Bandera A, Gori A, Finazzi S and Palomba E (2025) Corrigendum: Understanding the burden of antibiotic resistance: a decade of carbapenem-resistant Gram-negative bacterial infections in Italian intensive care units. Front. Microbiol. 16:1584655. doi: 10.3389/fmicb.2025.1584655
Received: 27 February 2025; Accepted: 04 March 2025;
Published: 18 March 2025.
Edited and reviewed by: Maria Teresa Mascellino, Sapienza University of Rome, Italy
Copyright © 2025 Scaglione, Perego, Colaneri, Genovese, Brivio, Covizzi, Viaggi, Bandera, Gori, Finazzi and Palomba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marta Colaneri, bWFydGEuY29sYW5lcmlAZ21haWwuY29t; Andrea Gori, YW5kcmVhLmdvcmlAdW5pbWkuaXQ=
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.