
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Med. , 19 March 2025
Sec. Obstetrics and Gynecology
Volume 12 - 2025 | https://doi.org/10.3389/fmed.2025.1537930
This article is part of the Research Topic Advancing HIV Treatment and Prevention for Cisgender Women: Approaches to Optimize Health Outcomes View all 5 articles
HIV disproportionately impacts women, particularly in sub-Saharan Africa and other low-and middle-income countries, where conflict and displacement heighten their vulnerability to HIV. Refugee women face compounded challenges, including trauma before and during migration and healthcare inequities in host countries. This perspective paper aims to assess existing evidence on HIV treatment and prevention for refugee women resettling in the U.S., using intersectional stigma and the status-neutral service delivery model as theoretical frameworks, to propose an implementation strategy. Trauma-informed care (TIC) offers a promising approach to address these challenges, emphasizing culturally responsive, safe, and empowering healthcare. Integrating TIC with the status-neutral model, which centers on HIV testing and pathways for prevention or treatment, can improve care access and outcomes. Moreover, including refugee women and stakeholders in designing tailored interventions that address individual and systemic-level barriers is critical to fostering health equity.
HIV remains a significant global public health challenge, with approximately 39.9 million people living with HIV (PWH) by the end of 2023, 53% of whom are women and girls (1). Sub-Saharan Africa bears the highest burden, accounting for two-thirds of PWH globally, with women and girls representing 63% of new HIV infections (2). Globalization and increasing cross-border movements have reshaped HIV distribution patterns, often reflecting migration routes (3). With over 117 million forcibly displaced people globally as of 2023, Refugees—Persons fleeing to a place of safety to escape danger, persecution, or economic distress in their own country—represent a population at heightened risk for HIV infection (4). Forced migration, driven by factors such as oppression, economic hardship, sociopolitical marginalization, and armed conflict, exposes individuals – particularly refugee women—to severe trauma and heightened vulnerability to HIV (5, 6). This risk is compounded by conditions in countries of origin with high HIV prevalence, limited healthcare access during migration, and increased exposure to violence (7–9). Gender inequities, socioeconomic disadvantages, and the breakdown of protective social networks further exacerbate their susceptibility, leading to sexual and gender-based violence and exploitation such as transactional sex, which significantly amplifies their HIV risk (8). In 2023, the U.S. admitted 60,060 refugees, with 41% from Africa, 34% from Near East/South Asia, and 11% from Latin America/Caribbean; and 41.6% were women. This paper examines HIV prevention and care for refugee women in the U.S. and proposes a framework to improve services (4).
Host countries often lack the capacity or commitment to deliver adequate, culturally-sensitive care to refugee women, who must navigate unfamiliar healthcare systems during resettlement with limited support (5, 7). Many arrive with histories of trauma, including violence and displacement, which profoundly impact their physical and mental health (5). The United States, historically a leading refugee resettlement destination, has limited and fragmented research on the intersection of HIV and refugee women’s health, leaving critical gaps in understanding. Addressing these gaps requires tailored trauma-informed care (TIC) programs that integrate refugees’ unique vulnerabilities and social determinants of health, particularly in HIV prevention and care (5, 8). Such programs must address language barriers, limited educational opportunities in refugee camps, and the challenges of securing employment and housing in host countries. Culturally sensitive care respects and incorporates patients’ cultural beliefs, values, and experiences, ensuring services are adapted to diverse populations (10). Cultural considerations are often inconsistently applied and measured, as a 2011–2021 review found only 12% of HIV interventions were culturally sensitive (11) Understanding these overlapping challenges is essential to dismantling the systemic and structural obstacles to HIV equity for this population.
Intersectional stigma provides a powerful framework for analyzing and addressing the barriers encountered by refugee women. This theory highlights that stigmatization does not occur in isolation but rather as a complex web of intersecting societal oppressions (12). For example, a refugee woman living with HIV may simultaneously face HIV-related stigma, characterized by fear of ostracism within her community; gender stigma, which limits her autonomy in healthcare decision-making; racial stigma, manifesting as discrimination within healthcare systems; and migrant stigma, driven by fears of being perceived as a burden or outsider in the host country, as some are often accused of importing HIV in the host countries (13). The literature shows that African immigrants and refugees have HIV infection rates six times higher than any other minority group in the U.S. (14). Migrant stigma related to HIV is particularly pronounced in refugee populations, as they are often scapegoated for bringing the virus into host communities (3, 9). This discriminatory perception can further leads refugees to neglecting their health needs, while survival priorities—such as securing food, safety, and shelter—frequently take precedence over seeking healthcare, delaying HIV testing and treatment (3, 5, 15). Moreover, language barriers and cultural stigma further exacerbate these issues, leading to delayed care initiation and poor treatment retention (5, 7, 16). These overlapping stigmas compound to erode trust in healthcare providers, delay testing, and reduce engagement in care (15–17). Furthermore, historical exclusionary policies related to HIV have deepened these fears, leaving a legacy of mistrust that persists even after policy changes (3). Additionally, refugees often reside in crowded living conditions where inadvertent disclosure of HIV status can lead to social exclusion or discrimination (18). This fear is particularly acute for women, who may experience compounded stigma. These cultural dynamics intersect with additional structural and systemic barriers, making healthcare access even more challenging. Intersectional stigma theory helps to explain how these overlapping stigmas magnify the challenges of accessing HIV testing and care as women navigate a healthcare system that often lacks culturally sensitive approaches.
The status-neutral model offers a novel framework for the HIV continuum of care integrating both PWH and those at risk of HIV (19). Beginning with an HIV test, the model divides into two pathways: “HIV Primary Prevention Engagement” for those testing negative and “HIV Treatment Engagement” for those testing positive. Both pathways share a common goal: sustained engagement in clinical care to minimize HIV transmission or acquisition risk. The model emphasizes that preventive and quality care services require continuous collaboration between patients and providers to sustain engagement in care or treatment.
Applying the status-neutral model to refugee women, requires addressing the intricate interplay of factors across multiple levels (Figure 1):
a. Individual level: studies have shown inconsistencies between knowledge of HIV acquisition and behaviors relating to HIV positive individuals among US based refugee women from Africa, which may indicate limited understanding of HIV transmission and prevention often shaped by cultural beliefs or lack of education (20, 21)
b. Interpersonal level: norms from the country of origin around HIV prevention and care, gender-based power imbalances, fear of partner violence, and stigma within families can hinder testing and treatment engagement (21).
c. Community Level: Discrimination against refugees and individuals living with HIV, as well as cultural taboos surrounding discussions of sexual health limit awareness and access to services (8, 19, 21).
d. Organizational level: language barriers remain a major challenge. While Spanish translation is common in U.S. healthcare, many refugee languages, like Burmese and African dialects, are underrepresented (16). Additionally, providers often lack trauma-informed training, as TIC is still emerging in refugee healthcare, limiting awareness and capacity (22). Social support, culturally safe providers, and patient navigators can improve comfort, knowledge, participation, and trust in host country health system (5, 17, 23).
e. Policy level: refugee women face healthcare access barriers due to complex eligibility tied to immigration status. While the Refugee Medical Assistance (RMA) program offers short-term coverage, gaps emerge if they do not qualify for Medicaid or state programs. The Ryan White HIV/AIDS Program covers PWH regardless of status but is limited to HIV care, excluding preventive services like PrEP. Expanding access to public and private insurance is crucial for improving preventive healthcare.
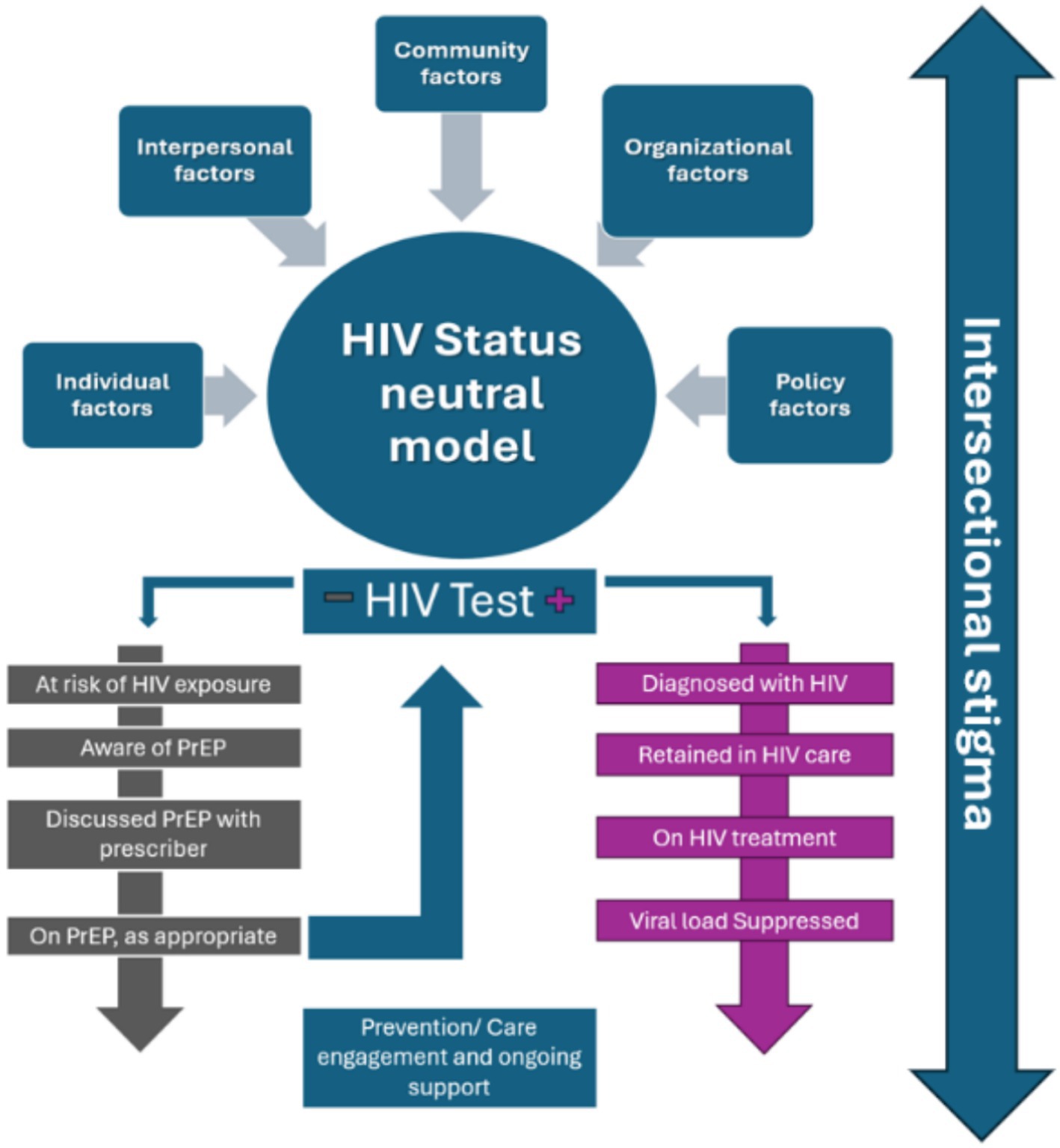
Figure 1. Status-neutral HIV care and prevention model. This figure illustrates the interplay of various factors that impact refugee women throughout the continuum.
Acknowledging and addressing these interconnected factors is critical to improving outcomes and ensuring the success of this initiative (Figure 1).
Historically, public health responses to the needs of refugee women have been scarce. Existing TIC efforts in the US primarily focused on addressing issues such as intimate partner violence (IPV), domestic abuse, and child abuse, with a limited number of interventions or research reflecting HIV and TIC among refugee women highlighting the need for tailored interventions for that vulnerable group (17, 24). Moreover, existing, efforts are often hampered by logistical challenges, under-resourced health systems, and a lack of targeted interventions that consider the specific needs of displaced women (3, 7).
HIV testing is a critical entry point for the implementation of the status-neutral HIV service delivery model. The Center for Diseases Prevention and Control (CDC) recommends routine opt-out HIV screening for refugees and immigrants as part of post-arrival healthcare (3). However, data on adherence to these guidelines and implementation outcomes remain limited. For testing to occur, women must be aware of their HIV risk, have access to primary care, sexually transmitted infection (STI) clinics, or other healthcare settings, and consult with culturally sensitive health providers. Studies looking at refugee women’s Knowledge, Attitudes, and Practices (KAP) reveal that many women have low knowledge and perception of their own HIV risk due to cultural or contextual factors, further reducing testing rates (19, 21, 25). Structural barriers such as lack of insurance, transportation challenges, and fragmented healthcare systems significantly limit access to care and contribute to the low rates of HIV testing and counseling among refugee and immigrant women (23). Additionally, intersectional stigma—stemming from the interplay of race, ethnicity, gender, HIV status, forced displacement, and refugee identity—creates fear and hesitancy around seeking testing (mistrust in how asylum host countries may use this information and difficulty in maintaining confidentiality in refugee settings) (3, 18).
Prenatal care presents another critical opportunity, as HIV testing is mandated during pregnancy. However, studies have identified missed opportunities, as refugee status has been associated with the late presentation of HIV (26). While women testing positive during prenatal care can be linked to care with good outcomes, those testing negative often receive minimal counseling on HIV prevention. Language barriers exacerbate these issues, as limited English proficiency hinders effective communication with healthcare providers. Compounding these challenges is the frequent lack of trauma-informed and culturally responsive care, as many healthcare providers are not trained to address the unique needs and lived experiences of refugee populations. Strategies that increase the ease of accessing HIV testing will likely result in decreased morbidity, mortality, and transmission of disease among this population. Paramount to that, gaps in KAP should be addressed, as studies showed inadequate knowledge of HIV transmission and inconsistencies between knowledge of HIV acquisition and behaviors relating to HIV-positive individuals, which may indicate HIV-associated stigma among refugee women (19, 25).
Despite these challenges, several strategies have shown promise in improving HIV testing and reducing the stigma around it. Studies on social support and its impact on HIV testing and adherence among refugee populations showed that informational support encouraged refugees to test for HIV (27).
Prevention strategies for HIV among refugee women must be culturally sensitive and context-specific, recognizing the unique challenges faced by this population. A review of various HIV prevention interventions highlights the importance of integrating cultural beliefs and experiences into program designs to improve their effectiveness (28). This is particularly crucial for refugee women who may have different social norms and barriers to health care access. Educational interventions hold great promise as a study by Cianelli et al. showed that increased HIV knowledge positively correlates with self-efficacy in HIV prevention, meaning women with more knowledge are more confident in their ability to adopt HIV prevention measures (29).
Culturally tailored programs that engage community members as peer leaders have proven effective in promoting HIV prevention strategies. Such participatory approaches not only enhance knowledge but also build social capital, which is critical for facilitating access to health services among refugee populations (9, 11, 16). Programs must provide information about available health services within refugee settlements, ensuring that women are aware of their options for prevention and treatment (5).
Furthermore, it is essential to incorporate strong social and psychological support systems from families, communities, and healthcare providers to improve adherence to HIV care within these settings (5). Promoting awareness and education among men and boys regarding sexual and reproductive health and gender equity is another critical component of HIV prevention strategies (3). By fostering gender equity, interventions can reduce stigma and discrimination, thereby facilitating more effective HIV prevention efforts for refugee women.
Research on the HIV continuum of care for refugee women in the U.S. remains limited, but studies from other countries provide valuable insights into the challenges these women face in engaging with HIV care. Pregnancy often serves as a pivotal entry point and represent the first sustained interaction with formal healthcare services, as it necessitates medical attention for maternal and child health needs (26, 30, 31). However, recent studies suggest that the prevalence of HIV among refugee women is typically higher than that of pregnant women in host countries, underscoring the urgency of targeted interventions (30). Furthermore, research indicated that refugee women who access antenatal visits face an increased risk of delayed HIV diagnosis due to their migrant background, which can jeopardize the health of both the mother and the unborn baby (26). High HIV prevalence in this population is further associated with severe maternal morbidity, emphasizing the importance of early and consistent HIV testing as a life-saving measure (31).
Studies exploring ART use among pregnant refugee women with HIV highlight significant factors influencing non-adherence. Late initiation of prevention of mother to child transmission (PMTCT) services in the third trimester reduces the time available for viral suppression, psychological adjustment, and treatment adherence. Additionally, women not requiring partner or family permission for PMTCT services exhibited lower adherence, likely reflecting insufficient social support (13). Negative attitudes from healthcare providers further diminished adherence, emphasizing the need for better training and support for service providers to foster trust and engagement.
The intersection of pregnancy, HIV and the cultural and systemic challenges of resettlement compounds the vulnerability of refugee women, who often conceal their HIV diagnosis due to stigma (32). Social support plays a crucial role in mitigating these challenges. For example, a study by Rouhani et al. in Southwestern Uganda demonstrated the dual importance of emotional support, which helps individuals cope with HIV diagnoses, and instrumental support, which facilitates ART adherence (27). Refugee women living with HIV also acted as agents of change by educating their social networks promoting testing, and accompanying others to testing sites. These findings underscore the importance of involving refugee women living with HIV in the design and implementation of programs to improve testing and treatment access for their social network.
Trauma-informed care for refugee women addresses the profound effects of trauma stemming from experiences during displacement, conflict, or resettlement. Refugee women face unique challenges, including high rates of sexual and intimate partner violence during migration, leading to mental health issues such as post-traumatic stress disorder (PTSD) (5, 33, 34). Women with lifetime trauma are more likely to report PTSD, depression, anxiety, and substance use, which negatively impact their quality of life and adherence to antiretrovirals (35). This care model emphasizes creating a safe, trusting healthcare environment that focuses on cultural sensitivity and patient empowerment (36). Such models should aim to avoid re-traumatization and facilitate healing through comprehensive, interdisciplinary approaches. TIC is particularly relevant for HIV care, as trauma is prevalent among people with or at risk for HIV and contributes to HIV acquisition, morbidity, and mortality. NASTAD’s Trauma-Informed Approaches Toolkit is a valuable resource that offers guidelines for healthcare providers on implementing TIC within HIV care systems. The toolkit emphasizes the importance of healing-centered care, recognizing that achieving viral suppression is just one aspect of comprehensive HIV treatment (36).
Few studies have examined the impact of TIC interventions on HIV care outcomes among this population. However, recent findings suggest that a trauma-informed approach to developing interventions may help to improve treatment outcomes, such as engagement in care and adherence to antiretrovirals (37). Research shows that social support is essential in reducing feelings of isolation and improving healthcare access for refugee women (5). Interventions like the “Tree of Life” for women with HIV have shown potential in helping refugee women identify personal strengths and qualities that enabled them to cope and build their resilience by empowering them to re-author their life narratives (38).
Despite its significance, the implementation of TIC faces considerable challenges, including systemic barriers such as limited access to mental health services, cultural stigma surrounding mental health, and language barriers that can complicate communication between providers and refugee women (33, 39, 40). Additionally, inadequate training among healthcare professionals in trauma-specific practices can hinder effective care delivery, underscoring the necessity for ongoing education and policy advocacy to support this population (22, 41).
We propose applying the Consolidated Framework for Implementation Research (CFIR) to guide the systematic implementation of TIC for refugee women living with or at risk of HIV (42). The CFIR framework allows for a structured approach to identifying and addressing individual, organizational, and policy-level determinants influencing the implementation process (Table 1). The CFIR was chosen for its multi-level approach, considering individual, organizational, and policy factors in implementing TIC (43). Unlike frameworks focused solely on behavior change or readiness, CFIR systematically assesses barriers and facilitators, making it ideal for complex interventions like trauma-informed, status-neutral HIV care for refugee women. However, its main limitation is the lack of guidance on adapting interventions based on identified factors.
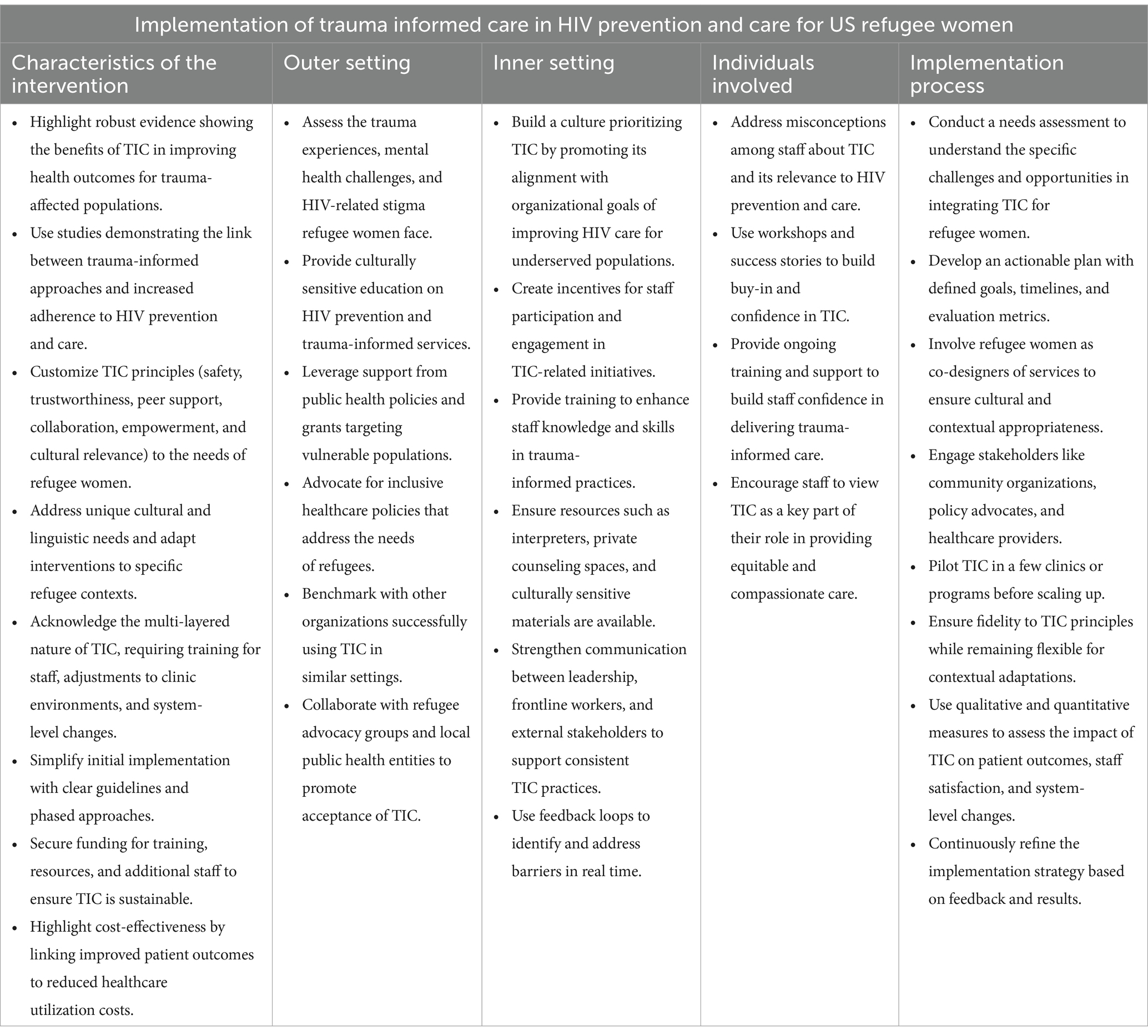
Table 1. Using the consolidated framework for implementation research (CFIR) to guide the systematic implementation of trauma-informed care for refugee women living with or at risk of HIV.
The co-design of a tailored action plan, informed by the needs assessment, should actively engage refugee women and key stakeholders to ensure cultural relevance and stakeholder buy-in. Developing implementation outcomes, such as engagement in prevention and care programs, is crucial for evaluating success. Continuous quality improvement can enhance fidelity and sustainability by enabling ongoing adaptation to systemic, organizational, and policy environments. This evidence-based approach ensures that TIC implementation is robust, scalable, and effective in meeting the needs of refugee women.
Efforts to address HIV prevention and care for refugee women must account for their unique challenges, including heightened vulnerability due to migration-related trauma, limited healthcare access, and stigmas. Trauma-informed care (TIC) plays a pivotal role in addressing both immediate mental health needs and the broader emotional well-being of refugee women and their families. Combining the HIV status-neutral service delivery model with TIC can significantly enhance access to testing, prevention, and treatment services, offering culturally sensitive, tailored interventions. To implement such approaches effectively, the CFIR framework can guide efforts to address systemic and individual-level barriers essential for ensuring equitable healthcare access and improving outcomes for refugee women, bringing us closer to ending the HIV epidemic.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
EN: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. NF: Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. UNAIDS. Global HIV statistics. (2024). Available at: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf (Accessed November 22, 2024)
2. Thematic_fs_hiv_girls_women.pdf. (n.d.). Available at: https://thepath.unaids.org/wp-content/themes/unaids2023/assets/files/thematic_fs_hiv_girls_women.pdf (Accessed November 22, 2024)
3. CDC. (2024). HIV infection. Immigrant and Refugee Health. Available online at: https://www.cdc.gov/immigrant-refugee-health/hcp/domestic-guidance/hiv-infection.html
4. Schofield, Noah, and Yap, Amanda. 2024_1108_ohss_refugee_annual_flow_report_2023.pdf. (n.d.). Retrieved February 14, 2025. Available online at: https://ohss.dhs.gov/sites/default/files/2024-11/2024_1108_ohss_refugee_annual_flow_report_2023.pdf
5. Hawkins, MM, Schmitt, ME, Adebayo, CT, Weitzel, J, Olukotun, O, Christensen, AM, et al. Promoting the health of refugee women: a scoping literature review incorporating the social ecological model. Int J Equity Health. (2021) 20:45. doi: 10.1186/s12939-021-01387-5
6. Palattiyil, G, Sidhva, D, Seraphia Derr, A, and Macgowan, M. Global trends in forced migration: policy, practice and research imperatives for social work. Int Soc Work. (2022) 65:1111–29. doi: 10.1177/00208728211022791
7. Davidson, N, Hammarberg, K, Romero, L, and Fisher, J. Access to preventive sexual and reproductive health care for women from refugee-like backgrounds: a systematic review. BMC Public Health. (2022) 22:403. doi: 10.1186/s12889-022-12576-4
8. Stirling-Cameron, E, Almukhaini, S, Dol, J, DuPlessis, BJ, Stone, K, Aston, M, et al. Access and use of sexual and reproductive health services among asylum-seeking and refugee women in high-income countries: a scoping review. PLoS One. (2024) 19:e0312746. doi: 10.1371/journal.pone.0312746
9. Zhang, X, Rhoads, N, Rangel, MG, Hovell, MF, Magis-Rodriguez, C, Sipan, CL, et al. Understanding the impact of migration on HIV risk: an analysis of Mexican migrants’ sexual practices, partners, and contexts by migration phase. AIDS Behav. (2017) 21:935–48. doi: 10.1007/s10461-016-1622-4
10. Claeys, A, Berdai-Chaouni, S, Tricas-Sauras, S, and De Donder, L. Culturally sensitive care: definitions, perceptions, and practices of health care professionals. J. Trans. Nurs. (2021) 32:484–92. doi: 10.1177/1043659620970625
11. Vitsupakorn, S, Pierce, N, and Ritchwood, TD. Cultural interventions addressing disparities in the HIV prevention and treatment cascade among black/African Americans: a scoping review. BMC Public Health. (2023) 23:1748. doi: 10.1186/s12889-023-16658-9
12. Thompson, VE. Intersectionality (Key concepts 2nd edition). In: Ethnic and racial studies vol. 44. (2020) p. 1472–1474.
13. Tusabe, J, Nangendo, J, Muhoozi, M, and Muyinda, H. Use and non-adherence to antiretroviral therapy among refugee HIV positive pregnant mothers aged 18–49 years in Kyangwali refugee camp, Western Uganda. AIDS Res Ther. (2024) 21:54. doi: 10.1186/s12981-024-00645-0
14. Moore, S, Zajicek-Farber, ML, and Donaldson, LP. A snapshot of HIV/AIDS knowledge, behaviors, and attitudes of Ethiopian immigrants in the District of Columbia. J Ethn Cult Divers Soc Work. (2024) 33:110–20. doi: 10.1080/15313204.2022.2154879
15. Darebo, TD, Spigt, M, Teklewold, B, Badacho, AS, Mayer, N, and Teklewold, M. The sexual and reproductive healthcare challenges when dealing with female migrants and refugees in low and middle-income countries (a qualitative evidence synthesis). BMC Public Health. (2024) 24:520. doi: 10.1186/s12889-024-17916-0
16. Vu, M, Besera, G, Ta, D, Escoffery, C, Kandula, NR, Srivanjarean, Y, et al. System-level factors influencing refugee women’s access and utilization of sexual and reproductive health services: a qualitative study of providers’ perspectives. Front. Glob. Women Health. (2022) 3:1048700. doi: 10.3389/fgwh.2022.1048700
17. Mathis, CM, Steiner, JJ, Kappas Mazzio, A, Bagwell-Gray, M, Wachter, K, Johnson-Agbakwu, C, et al. Sexual and reproductive healthcare needs of refugee women exposed to gender-based violence: the case for trauma-informed Care in Resettlement Contexts. Int J Environ Res Public Health. (2024) 21:1046. doi: 10.3390/ijerph21081046
18. Correa-Salazar, C, Amon, JJ, Page, K, Groves, AK, Bilal, U, Vera, A, et al. Barriers and facilitators to HIV prevention and care for Venezuelan migrant/refugee women and girls in Colombia. Jo. Migr. Health. (2023) 8:100206. doi: 10.1016/j.jmh.2023.100206
19. Myers, JE, Braunstein, SL, Xia, Q, Scanlin, K, Edelstein, Z, Harriman, G, et al. Redefining prevention and care: a status-neutral approach to HIV. Open Forum Infect Dis. (2018) 5:ofy097. doi: 10.1093/ofid/ofy097
20. Agbemenu, K, Aidoo-Frimpong, G, Auerbach, S, and Jafri, A. HIV attitudes and beliefs in U.S.-based African refugee women. Ethn Health. (2022) 27:499–508. doi: 10.1080/13557858.2020.1740175
21. Feresu, S, and Smith, L. Knowledge, attitudes, and beliefs about HIV/AIDS of Sudanese and bantu Somali immigrant women living in Omaha, Nebraska. Open J Prev Med. (2013) 3:84–98. doi: 10.4236/ojpm.2013.31011
22. Im, H, and Swan, LET. Working towards culturally responsive trauma-informed Care in the Refugee Resettlement Process: qualitative inquiry with refugee-serving professionals in the United States. Behav. Sci. (2021) 11:9. doi: 10.3390/bs11110155
23. Li, K, Thaweesee, N, Kimmel, A, Dorward, E, and Dam, A. Barriers and facilitators to utilizing HIV prevention and treatment services among migrant youth globally: a scoping review. PLOS Glob. Public Health. (2024) 4:e0002851. doi: 10.1371/journal.pgph.0002851
24. Sales, JM, Swartzendruber, A, and Phillips, AL. Trauma-informed HIV prevention and treatment. Curr HIV/AIDS Rep. (2016) 13:374–82. doi: 10.1007/s11904-016-0337-5
25. Khan, MN, Rahman, MM, Rahman, MM, and Islam, MM. HIV transmission knowledge among Rohingya refugee women in Bangladesh: a cross-sectional survey. BMJ Open. (2021) 11:e047516. doi: 10.1136/bmjopen-2020-047516
26. Singer, K, Schulze-Sturm, U, Alba-Alejandre, I, Hollwitz, B, Nguyen, TTT, Sollinger, F, et al. Impact of refugee influx on the epidemiology of late-presenting HIV-infected pregnant women and mother-to-child transmission: comparing a southern and northern medical Centre in Germany. Infection. (2019) 47:847–52. doi: 10.1007/s15010-019-01332-3
27. Rouhani, SA, O’Laughlin, KN, Faustin, ZM, Tsai, AC, Kasozi, J, and Ware, NC. The role of social support on HIV testing and treatment adherence: a qualitative study of HIV-infected refugees in southwestern Uganda. Glob Public Health. (2017) 12:1051–64. Scopus. Doi:10.1080/17441692.2015.1132472. doi: 10.1080/17441692.2015.1132472
28. Wyatt, GE, Williams, JK, Gupta, A, and Malebranche, D. Are cultural values and beliefs included in U.S. based HIV interventions? Prev Med. (2012) 55:362–70. doi: 10.1016/j.ypmed.2011.08.021
29. Cianelli, R, Villegas, N, McCabe, BE, de Tantillo, L, and Peragallo, N. Self-efficacy for HIV prevention among refugee Hispanic women in South Florida. J Immigr Minor Health. (2017) 19:905–12. doi: 10.1007/s10903-016-0462-7
30. Goosen, S, Hoebe, CJPA, Waldhober, Q, and Kunst, AE. High HIV prevalence among asylum seekers who gave birth in the Netherlands: a Nationwide study based on antenatal HIV tests. PLoS One. (2015) 10:e0134724. doi: 10.1371/journal.pone.0134724
31. Wanigaratne, S, Cole, DC, Bassil, K, Hyman, I, Moineddin, R, and Urquia, ML. Contribution of HIV to maternal morbidity among refugee women in Canada. Am J Public Health. (2015) 105:2449–56. doi: 10.2105/AJPH.2015.302886
32. Chulach, T, Gagnon, M, and Holmes, D. The lived experience of pregnancy among HIV-positive refugee women: a qualitative study. ANS Adv Nurs Sci. (2016) 39:130–49. doi: 10.1097/ANS.0000000000000117
33. DeSa, S, Gebremeskel, AT, Omonaiye, O, and Yaya, S. Barriers and facilitators to access mental health services among refugee women in high-income countries: a systematic review. Syst Rev. (2022) 11:62. doi: 10.1186/s13643-022-01936-1
34. Wylie, L, Van Meyel, R, Harder, H, Sukhera, J, Luc, C, Ganjavi, H, et al. Assessing trauma in a transcultural context: challenges in mental health care with immigrants and refugees. Public Health Rev. (2018) 39:22. doi: 10.1186/s40985-018-0102-y
35. Cuca, YP, Shumway, M, Machtinger, EL, Davis, K, Khanna, N, Cocohoba, J, et al. The association of trauma with the physical, behavioral, and social health of women living with HIV: pathways to guide trauma-informed health care interventions. Women’s Health Issues: Official Publication of the Jacobs Institute of Women’s Health. (2019) 29:376–384. doi: 10.1016/j.whi.2019.06.001
36. Using Trauma-Informed Approaches to End the HIV Epidemic | NASTAD. (2023). Available online at: https://nastad.org/blog/using-trauma-informed-approaches-end-hiv-epidemic
37. Brown, MJ, and Adeagbo, O. Trauma-informed HIV care interventions: towards a holistic approach. Curr HIV/AIDS Rep. (2022) 19:177–83. doi: 10.1007/s11904-022-00603-3
38. Vitale, A, Khawaja, NG, and Ryde, J. Exploring the effectiveness of the tree of life in promoting the therapeutic growth or refugee women living with HIV. Arts Psychother. (2019) 66:101602. doi: 10.1016/j.aip.2019.101602
39. Bailey, T. (2017). Enhancing evidence-based interventions for refugees. Trauma Psychology News. Available online at: https://traumapsychnews.com/2017/07/enhancing-evidence-based-interventions-for-refugees/
40. Moezzi, SMI, Etemadi, M, Lankarani, KB, Behzadifar, M, Katebzada, H, and Shahabi, S. Barriers and facilitators to primary healthcare utilization among immigrants and refugees of low and middle-income countries: a scoping review. Glob Health. (2024) 20:75. doi: 10.1186/s12992-024-01079-z
41. Policy Guide: Improving Access to Mental Healthcare for Refugees and Other Displaced People in the United States. (n.d.). The Refugee Advocacy Lab. Retrieved November 26, 2024. Available online at: https://www.refugeeadvocacylab.org/resources/mental-health-policy-guide
42. Damschroder, LJ, Aron, DC, Keith, RE, Kirsh, SR, Alexander, JA, and Lowery, JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. (2009) 4:50. doi: 10.1186/1748-5908-4-50
Keywords: HIV prevention and care, women, refugee, trauma informed care, implementation framework
Citation: Nkodo ENE and Fadul N (2025) A trauma-informed care model for HIV prevention and care for refugee women in the United States: perspectives and implementation framework. Front. Med. 12:1537930. doi: 10.3389/fmed.2025.1537930
Received: 02 December 2024; Accepted: 24 February 2025;
Published: 19 March 2025.
Edited by:
Maria L. Alcaide, University of Miami, United StatesReviewed by:
Emily M. Cherenack, University of Miami, United StatesCopyright © 2025 Nkodo and Fadul. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nada Fadul, bmFkYS5mYWR1bEB1bm1jLmVkdQ==
†ORCID: Emmanuel Nazaire Essam Nkodo, orcid.org/0009-0006-4388-8398
Nada Fadul, orcid.org/0000-0001-5022-9063
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.