
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Med., 07 February 2025
Sec. Intensive Care Medicine and Anesthesiology
Volume 12 - 2025 | https://doi.org/10.3389/fmed.2025.1533841
This article is part of the Research TopicUnraveling the Health Impacts of Toxic ExposuresView all 5 articles
We studied the case of a 22-year-old Pregnant woman who self-administered about 200 ml of diquat solution (200 g/L) during a suicide attempt. She developed vomiting, and was admitted to the emergency department of our hospital 5 h later. Based on symptoms, and elevated levels of myoglobin and creatine kinase, the patient was diagnosed with rhabdomyolysis, acute renal failure and toxic encephalopathy caused by diquat poisoning. Undergoing hemoperfusion and hemofiltration were administered immediately. Rhabdomyolysis, toxic encephalopathy, and abortion occurred successively in the pregnant woman. The patient was discharged from the hospital after 37 days of treatment with a Glasgow–Pittsburgh Cerebral Classification (CPC) score of grade 2.this was a case of diquat poisoning complicated with renal failure, rhabdomyolysis, and toxic encephalopathy in a pregnant, which would enrich the experience of diquat poisoning treatment.
Diquat is a bipyridine-inactivating herbicide with strong toxic effects (1). It can be absorbed through the digestive tract, respiratory tract, eyes, or cutaneous mucosa, and is excreted mainly by the kidneys. Patients may experience oliguria, anuria, and other AKI manifestations during the early stages of poisoning. Multiple organ damage may also occur with disease progression, leading to fatal outcomes (2). At present, no specific antidote exists for diquat poisoning, and the main treatment methods include removing the unabsorbed poison and accelerating its excretion of the absorbed poison. Rhabdomyolysis, toxic encephalopathy, and abortion occurred successively in the pregnant woman. This article presents the case of a pregnant woman who was treated for diquat poisoning.
A 22-year-old woman was admitted to the emergency department due to intentional ingestion of diquat in September 2023 for “self-administration of diquat for over 5 h.” The patient had orally ingested approximately 200 mL of Diquat five or more hours before admission. Subsequently, the patient developed nausea and vomiting. She was sent to a local hospital for gastric lavage1 h prior and was then transferred to our department. Multiple suicide attempts had been made previously. The patient was 20 weeks pregnant at the time of admission. Physical examination revealed the following findings: T: 36.6°C, P: 92 bpm, R: 16 bpm, BP: 100/63 mmHg. The patient was conscious, and no abnormal signs were observed during the examination of the heart, lungs, and abdomen. Bilateral lower limbs showed no edema. At the time of admission, laboratory examinations showed the following: blood gas analysis: pH 7.40, partial pressure of oxygen (PaO2) 115 mmHg, partial pressure of carbon dioxide (PaCO2) 27 mmHg, oxygen saturation 99.2%; blood routine: leukocytes 20.17 × 109/L, neutrophil percentage 95.8%, erythrocytes 3.89 × 1012/L, hemoglobin 122 g/L, platelets 177 × 10/L, liver and kidney function: ALT 20 U/L, AST 58 U/L, total bilirubin 8.5 μmol/L, creatinine 66.6 μmol/L. She was diagnosed with diquat poisoning based on her medical history after admission, and activated charcoal with mannitol was administered orally. Anti-inflammatory, acid-suppressing, and antioxidant treatments were administered immediately.
The patient developed thoracodynia on the day of admission. Examination of abdominal distension: The uterine floor was located at the level of the naval plane. Palpable contractions occurred at intervals of 1–3 min with a duration of 20–30 s. Vaginal bleeding suggested threatened abortion. Bedside ultrasonography revealed a single live fetus in the uterus. Subsequently, the vaginal bleeding gradually increased, and on the fourth day of admission, a stillborn fetus was delivered. Bedside ultrasonography revealed no obvious tissue residue in the uterine cavity after miscarriage. The patient's vaginal bleeding gradually decreased, and the uterine fundus was located between the umbilicus. On the second day after the miscarriage, the patient had little dark-red vaginal blood without active bleeding. On the seventh day after the miscarriage, the patient had little bloody vaginal secretion with no obvious odor. On the 21st day after the abortion, the patient's uterus essentially recovered, and there was little intermittent light red vaginal discharge with no discernible odor. The vagina had no discernible secretions at the time of hospital discharge.
On admission, the blood concentration of diquat was measured using ultra-high-performance liquid chromatography tandem mass spectrometry (Figure 1 and Table 1). The patient experienced pain and swelling in both lower extremities. Her plasma creatine kinase level was 22,154 U/L (Figure 2), and her 24 h urine output was 330 mL on the first day of admission, which gradually decreased. The patient eventually developed anuria, and her creatinine levels progressively increased. Based on the patient's clinical manifestations and the results mentioned above, she was diagnosed with rhabdomyolysis and acute renal failure. On admission, the patient underwent bedside blood purification. On the 10th day of admission, the patient began to urinate (24 h urine output, 30 mL). On the 13th day, the patient's creatinine levels gradually decreased. The patient was discharged 37 days after admission. At the time of discharge, the patient's creatinine level was 132 μmol/L, and the 24 h urine volume was 2,300 mL (Figures 1, 3).
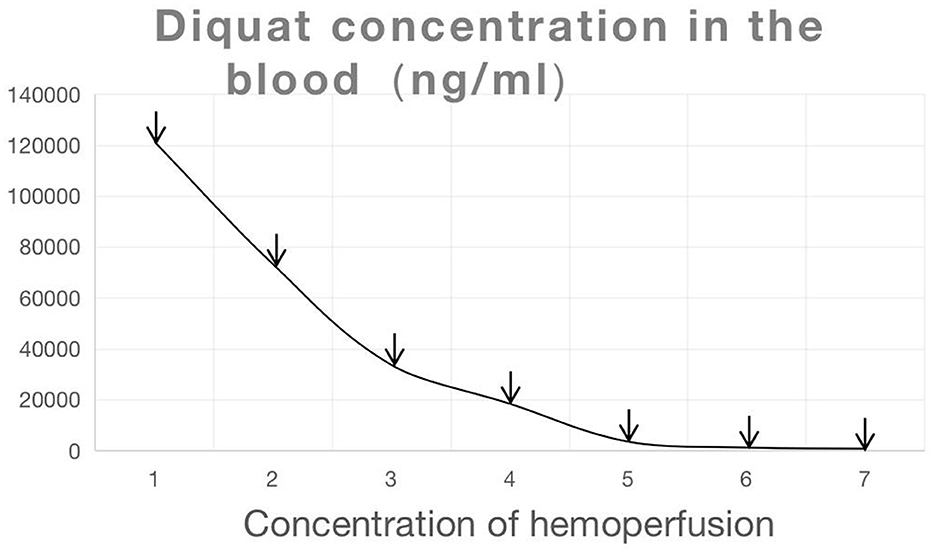
Figure 1. Changes in diquat concentration (The arrows represented that the patient underwent blood purification on that day).
The patient was conscious on the day of admission and had a Glasgow Coma Scale (GCS) score of 15 and a Glasgow–Pittsburgh Cerebral Classification (CPC) score of 1. On the second day of admission, the patient was semicomatose, with a GCS score of 7, a CPC score of 4, and progressive worsening of consciousness. On the 5th day of admission, the patient was extubated and placed on mechanical ventilation because of respiratory failure. Dyspnea reappeared on the 15th day of admission, leading to the initiation of mechanical ventilation support following tracheotomy. On the 27th day of admission, the patient's consciousness started to improve. The tracheal tube was closed on the 30th day after admission. The patient was discharged on the 37th day of admission. She was unresponsive, with a GCS score of 12 and a CPC score of 3. The patient was followed up 1 month after discharge, and the patient's consciousness was better than before, with a satisfactory response, the ability to independently finish daily activities, and a CPC score of grade 2 (Figure 4).
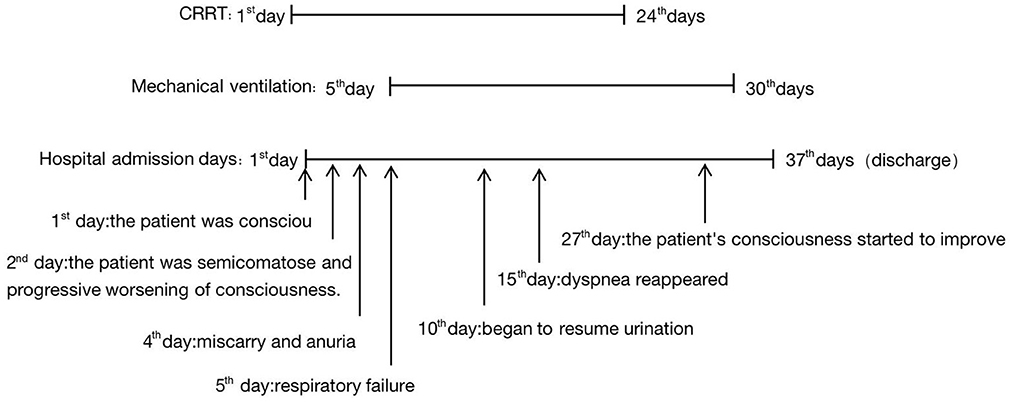
Figure 4. Patient's duration of treatment and significant change during the patients's hospitalization.
Diquat is a non-selective and fast-acting herbicide that is orally absorbed through the gastrointestinal tract. Diquat is excreted mainly through the digestive tract and kidneys. The toxic mechanism is primarily related to the oxidation-reduction process, leading to oxidative stress and cell death, ultimately resulting in multi-organ failure (3).
In severe cases of diquat poisoning, multiple organ damage occurs shortly after ingestion, affecting the liver, kidney, digestive, respiratory, and nervous system. Clinical manifestations and prognosis are related to the dose. In this case, a pregnant woman (15 weeks of gestation) rapidly developed acute renal failure, rhabdomyolysis, toxic encephalopathy, and miscarriage after self-administration of 200 mL of diquat. In a search for documented cases of diquat poisoning (4–9), complications that occurred simultaneously were not documented in previous reports.
In a previous case of diquat poisoning in a pregnant woman (15 weeks of gestation) (7), she miscarried 23 h after ingestion and died 44 h later. The concentration of diquat in the patient's blood 23 h after ingestion was 1.2 lg/mL. The diquat concentrations in the placental blood, umbilical cord blood, and amniotic fluid were 0.8 lg/mL, 0.7 lg/mL, and 0.4 lg/mL, respectively, which showed that diquat could cross the placenta and could be lethal to the fetus. However, information on the toxic effects of diquat on the female reproductive system is limited. Long-term exposure to diquat can impair oocyte function by improving the expression of apoptotic genes and enhancing ROS levels and can also affect fetal development and litter sizes (10). Diquat also causes embryonic malformations in humans (11). In this case, the pregnant woman experienced a miscarriage on the 4th day of admission, which may be attributed to the ability of diquat to cross the placenta and induce oxidative stress and cytotoxicity, ultimately leading to fetal demise. Fortunately, it has been reported that she is the only pregnant woman to have survived the poisoning.
Currently, no specific antidote exists for diquat poisoning. For patients who ingest diquat orally, treatment focuses on decreasing absorption and enhancing elimination. Gastric lavage, medicinal charcoal adsorption, oral mannitol, and other treatments can facilitate diquat excretion. Gastric lavage performed as early as possible in patients with oral intoxication, especially within 1 h, has the best effect on removing the poison, whereas gastric lavage can still be considered within 6 h for those with gastroparesis or considerable intake (2). In this case, the patient presented to a local hospital and underwent gastric lavage 1 h after ingesting diquat. Owing to the significant oral intake, the patient underwent gastric lavage again at our hospital. Blood purification is an effective choice to relieve the poisoning of diquaty. In this case, 13 blood purification treatments were performed, including 6 hemoperfusions and 13 renal replacement therapies. These treatments can maintain the stability of the internal environment and fluid balance during the recovery period of renal function. Animal experiments have indicated that diquats cause renal tubular degeneration and necrosis (12). Diquat is primarily metabolized by the kidneys and can easily cause acute kidney injury. In this case, in addition to acute kidney injury caused by diquat, rhabdomyolysis also exacerbated the condition. Diquat can also damage the central nervous system cells (13). Severe brain damage may be associated with higher mortality rates in patients with diquat poisoning (14). Although the mechanism of toxicity is not fully understood, research indicates that reduction-oxidation (redox) cycling may play a significant role (15, 16). The use of antioxidant drugs, such as glutathione, may alleviate the neurotoxic effects of diquat (17). In this instance, the patient developed disturbances in consciousness on the second day of drug administration. Subsequent head computed tomography revealed brainstem edema. She gradually regained consciousness with further treatment; however, she exhibited neurological sequelae.
The prognosis of patients is significantly correlated with the amount of poison administered, the timing of the first gastric lavage, blood purification, adsorption, and diarrhea. Decontamination of the digestive tract and blood purification should be performed immediately. Monitoring the concentration of toxins in the blood is recommended.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
ML: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. BQ: Conceptualization, Data curation, Writing – original draft. YCh: Conceptualization, Data curation, Writing – review & editing. YCu: Conceptualization, Data curation, Writing – review & editing. YH: Funding acquisition, Writing – review & editing. ZJ: Conceptualization, Data curation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Science and Technology Planning Project of Sichuan Province (2019JDPT0003).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Long J, Chen L, Lu Z. Important clinical advances in acute herbicide poisoning. Chin J Pract Intern Med. (2021) 41:194–97. doi: 10.19538/j.nk2021030105
2. Expert Consensus Group on the Diagnosis and Treatment of Acute Diquat Poisoning. Expert consensus on the diagnosis and treatment of acute diquat poisoning. Chin J Emerg Med. (2020) 128:2–19. doi: 10.3760cma/j.issn.1671-0282.2020.10.002
3. Magalhaes N, Carvalho F, Dinis-Oliveira RJ. Human and experimental toxicology of diquat poisoning: toxicokinetics, mechanisms of toxicity, clinical features, and treatment. Hum Exp Toxicol. (2018) 37:1131–60. doi: 10.1177/0960327118765330
4. Yang M, Xiong W, Zhang N, Tan X, Chen S, Wang J, et al. Effect of diagnosis and treatment on a case of rhabdomyolysis caused by diclofenac poisoning. Contemp Med. (2020) 18:148–50. doi: 10.3969/j.issn.2095-7629.2020.19.105
5. Yu G, Wang J, Jian T, Shi L, Zhao L, Li Y, et al. Case series: Diquat poisoning with acute kidney failure, myocardial damage, and rhabdomyolysis. Front Public Health. (2022) 10:991587. doi: 10.3389/fpubh.2022.991587
6. Yu G, Jian T, Cui S, Shi L, Kan B, Jian X. Acute diquat poisoning resulting in toxic encephalopathy: a report of three cases. Clin Toxicol. (2022) 60:647–50. doi: 10.1080/15563650.2021.2013495
7. Yu G, Cui S, Jian T, Kan B, Jian X. Diquat poisoning in a pregnant woman resulting in a miscarriage and maternal death. Clin Toxicol. (2021) 59:1275–7. doi: 10.1080/15563650.2021.1905164
8. Wang J, Tong S, Zhang T, Liu M, Zhao L, Yang Y, et al. Seven cases of diquat-associated toxic encephalopathy. Chin J Emerg Med. (2022) 1648–53. doi: 10.3760/cma.j.issn.1671-0282.2022.12.014
9. Meng N, Sun Y, Liu L, Yao D, Gao H, Ma Y, et al. Clinical analysis of 86 cases of acute diquat poisoning. Chin Emerg Med Crit Illn. (2022) 301–5. doi: 10.3760/cma.j.cn121430-20220128-00105
10. Zhang JQ, Gao BW, Wang J, Wang XW, Ren QL, Chen JF, et al. Chronic exposure to diquat causes reproductive toxicity in female mice. PLoS ONE. (2016) 11:e147075. doi: 10.1371/journal.pone.0147075
11. Sewalk CJ, Brewer G L, Hoffman DJ. Effects of diquat, an aquatic herbicide, on the development of mallard embryos. J Toxicol Environ Health A. (2001) 62:33–45. doi: 10.1080/00984100050201659
12. Wu Y, Cui S, Wang W, Jian T, Kan B, Jian X. Kidney and lung injury in rats following acute diquat exposure. Exp Ther Med. (2022) 23:275. doi: 10.3892/etm.2022.11201
13. Xing J, Chu Z, Han D, Jiang X, Zang X, Liu Y, et al. Lethal diquat poisoning manifesting as central pontine myelinolysis and acute kidney injury: a case report and literature review. J Int Med Res. (2020) 48: 300060520943824. doi: 10.1177/0300060520943824
14. Zhou JN, Lu YQ. Lethal diquat poisoning manifests as acute central nervous system injury and circulatory failure: a retrospective cohort study of 50 cases. EClinicalMedicine. (2022) 52:101609. doi: 10.1016/j.eclinm.2022.101609
15. Jones GM, Vale JA. Mechanisms of toxicity, clinical features, and management of diquat poisoning: a review. J Toxicol Clin Toxicol. (2000) 38:123–8. doi: 10.1081/CLT-100100926
16. Fussell KC, Udasin RG, Gray JP, Mishin V, Smith PJ, Heck DE, et al. Redox cycling and increased oxygen utilization contribute to diquat-induced oxidative stress and cytotoxicity in Chinese hamster ovary cells overexpressing NADPH-cytochrome P450 reductase. Free Radic Biol Med. (2011) 50:874–82. doi: 10.1016/j.freeradbiomed.2010.12.035
Keywords: diquat, diquat poison, rhabdomyolysis, toxic encephalopathy, abortion, acute kidney injury
Citation: Li M, Qin B, Chen Y, Cui Y, Hu YC and Jiang Z (2025) Case report: A case of acute renal failure, rhabdomyolysis, and toxic encephalopathy associated with diquat poisoning in a pregnant woman. Front. Med. 12:1533841. doi: 10.3389/fmed.2025.1533841
Received: 25 November 2024; Accepted: 20 January 2025;
Published: 07 February 2025.
Edited by:
Rahul Kashyap, WellSpan Health, United StatesReviewed by:
Ishita Mehra, Saint Michael Medical Center, United StatesCopyright © 2025 Li, Qin, Chen, Cui, Hu and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mengqin Li, bGltZW5ncWluZmVpZmVpQDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.