
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Med. , 19 February 2025
Sec. Hepatobiliary Diseases
Volume 12 - 2025 | https://doi.org/10.3389/fmed.2025.1525442
This article is part of the Research Topic Case Reports in Hepatobiliary Diseases View all 16 articles
Biliary complications pose substantial challenges in liver transplantation (LT), particularly with regard to non-anastomotic strictures (NASs). Among these ischemic-type biliary complications, bile cast syndrome (BCS) is a particularly severe condition. Currently, there are limited data on the formation of complete hepatic casts in BCS. In this case report, we present a unique instance of a second LT involving the formation of a complete hepatic bile cast and discuss its diagnostic and therapeutic process. This case aims to enhance the understanding of the anatomical and pathological features of BCS.
Liver transplantation (LT) is widely recognized as the optimal therapeutic approach for end-stage liver disease (1). Biliary complications, which are frequently observed post-transplantation, remain a significant source of morbidity in LT recipients. Biliary complications can be categorized into anastomotic stricture (AS) complications and non-anastomotic stricture (NAS) complications based on therapeutic aspects (2). The management of biliary complications poses considerable challenges, especially for NASs, often necessitating repeated interventions or even secondary LT (3). Bile cast syndrome (BCS) represents a rare occurrence of NASs, which manifests as blackened hardened material conforming to the shape of bile ducts (4). Although some studies have reported on the morphological aspects of BCS, comprehensive images that fully depict complete hepatic bile cast formation are still limited (5). In this study, we present a unique case involving complete hepatic bile cast formation and its diagnostic and therapeutic process with the aim of enhancing understanding of NASs and BCS from both anatomical and pathophysiological perspectives.
A 32-year-old man was admitted to the liver transplantation (LT) department with a 2-day history of jaundice and abdominal pain. 7 months prior, he had undergone ABO-incompatible LT for hepatitis B virus (HBV)-related cirrhosis and acute-on-chronic liver failure, with maintenance immunosuppressive therapy consisting of tacrolimus and mycophenolic acid. The donor was donated after brain death and was HCV-positive. Prior to LT, the recipient underwent plasma exchange twice and received two doses of 300 mg rituximab, resulting in an ABO antibody titer below 1:64. On admission, the patient presented without fever and exhibited stable vital signs. Additionally, the patient had a medical history of hip arthroplasty due to femoral head necrosis, received entecavir treatment for HBV prophylaxis, and achieved HCV eradication.
Physical examination revealed jaundiced skin and sclera, along with mild tenderness in the upper right abdomen. Laboratory findings included white blood cells 2.85 × 109/L (reference 3.5–9.5 × 109/L) with hemoglobin 119 g/L (reference 130–175 g/L), platelets 85 × 109/L (reference 125–350 × 109/L), C-reactive protein 4.62 mg/L (reference 0–6 mg/L), and procalcitonin 5.29 ng/mL (reference <0.1 ng/mL). Liver function tests revealed total bilirubin 262.8 μmol/L (reference 0–26 μmol/L), with albumin 34.8 g/L (reference 40–55 g/L), and aspartate aminotransferase 141 U/L (reference 0–45 U/L). Tacrolimus concentration was 22.2 ng/mL (reference 5–15 ng/mL). Hepatitis B serologic test revealed HBsAg 0.20 IU/mL (reference 0–0.05 IU/mL) with HBcAb 7.85 (reference <1). Kidney function revealed creatinine 134 μmol/L (reference 57–97) with urea 9.73 mmol/L (reference 3.1–8 mmol/L). Clotting function, thyroid function, gastrointestinal tumor markers, Epstein–Barr virus, cytomegalovirus, and coronavirus were all within normal limits.
Multiple imaging tests, including abdominal contrast-enhanced computed tomography (CT) (Figure 1A) and magnetic resonance cholangiopancreatography (MRCP), demonstrated intrahepatic biliary ductal dilatation and stricture (Figure 1B). Abdominal CT angiography with three-dimensional reconstruction of the hepatic artery (Figure 1C) and portal vein (Figure 1D) revealed no evidence of anastomotic stenosis.

Figure 1. Imaging examinations and ERC procedures of the patient. (A) Abdominal contrast-enhanced computed tomography; (B) abdominal magnetic resonance cholangiopancreatography; (C) three-dimensional reconstruction of the hepatic artery; (D) three-dimensional reconstruction of the portal vein; (E) placement of biliary stents using ERC procedure; and (F) nasobiliary drainage using ERC procedure.
We conducted multiple endoscopic retrograde cholangiography (ERC) procedures, including balloon dilation, placement of biliary stents (Figure 1E), and nasobiliary drainage (Figure 1F) for the management of this patient. However, despite these interventions, the patient’s cholangitis and biliary obstruction continued to worsen. Ultimately, a second modified piggyback LT with bilioenteric anastomosis was conducted. During the dissection of the explanted liver, complete casts within the entire biliary tract were removed (Figure 2). Pathological examination revealed extensive cholestasis and infectious cholangitis with necrosis throughout the entire bile duct system (Figure 3). By post-transplantation day 20, the patient’s serum total bilirubin and transaminase levels had returned to normal values (Figure 4).
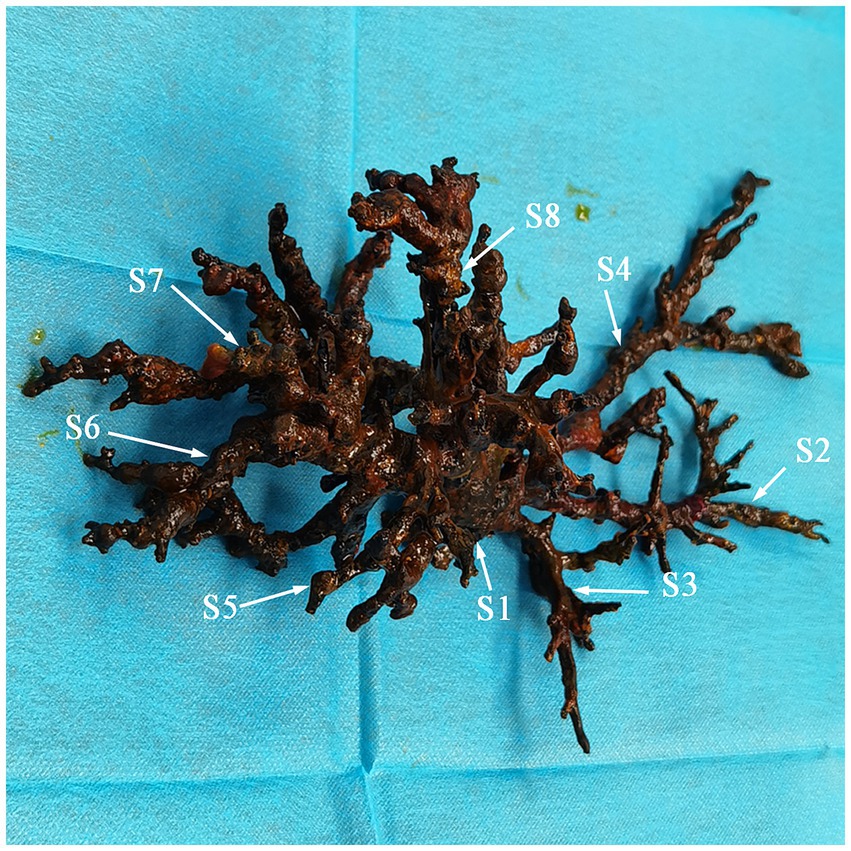
Figure 2. Complete casts within the entire biliary tract removed from the explanted liver (S, segment).
The incidence of NASs varies between 5 and 25% across different studies (2, 3). The occurrence of graft loss in NASs is frequently observed, with reported rates as high as 46% (6). BCS is a rare NAS post-liver transplant complication first described in 1975 (7). The incidence of BCS in LT patients ranges from approximately 2.1 to 3.6%, often necessitating re-transplantation (4). However, there is limited imaging evidence available regarding BCS, particularly complete hepatic cast formation, which plays a crucial role in comprehending the anatomy of the biliary tract and underlying pathological mechanisms.
This is a serious biliary complication that occurs following LT and is characterized by jaundice, increased cholestatic enzymes, and recurrent cholangitis. Imaging findings suggestive of a stricture at the biliary anastomotic site may lead to misdiagnosis as a biliary complication caused by AS. For AS, endoscopic interventions with ERC are recommended as first-line treatment (2, 8). Studies have consistently shown that complications associated with AS typically manifest during the early postoperative period, particularly within 3–6 months rather than later (9, 10). We concluded that this patient’s initial biliary obstruction and cholangitis symptoms were likely due to an NAS complication.
Etiologic mechanisms contributing to NASs include hepatic artery thrombosis or stenosis, ABO incompatibility, presence of T-tubes or bile leaks, ampullary dysfunction, chronic rejection, primary sclerosing cholangitis, circulatory instability, prolonged cold or warm ischemia, and marginal donor factors (2, 11, 12). This NAS case was due to ABO incompatibility. All bile ducts underwent immunological pathogenesis, resulting in complete cast formation, which is known as BCS. Buis CI et al. reported that NASs can lead to biliary destruction in four anatomical regions: hilar bifurcation, ducts between the first- and second-order branches, between second and third-order branches, and in the periphery of the liver (12). Involvement of ducts between second and third-order branches or in the periphery of the liver presents greater therapeutic challenges with a poorer prognosis, often necessitating re-transplantation for these patients (2, 13). Consequently, a second LT combined with bilioenteric anastomosis emerged as the sole viable treatment option for this patient.
This case report presents the most detailed replicas of the entire intrahepatic biliary tree documented to date, thereby enhancing our understanding of both the anatomical and pathological features of BCS.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of Shenzhen Third People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
PW: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. LZ: Data curation, Formal analysis, Funding acquisition, Investigation, Visualization, Writing – review & editing. DZ: Conceptualization, Methodology, Resources, Validation, Visualization, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported, in part, by grants from the Shenzhen High-level Hospital Construction Fund (XKJS-PWK-001) and the Shenzhen Science and Technology Research and Development Fund (JCYJ20220530163011026).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AS, anastomotic stenosis; BCS, bile cast syndrome; CT, computed tomography; ERC, endoscopic retrograde cholangiography; HBV, hepatitis B virus; HCV, hepatitis C virus; LT, liver transplantation; MRCP, magnetic resonance cholangiopancreatography; NAS, non-anastomotic strictures.
1. Lucey, MR, Furuya, KN, and Foley, DP. Liver transplantation. N Engl J Med. (2023) 389:1888–900. doi: 10.1056/NEJMra2200923
2. Seehofer, D, Eurich, D, Veltzke-Schlieker, W, and Neuhaus, P. Biliary complications after liver transplantation: old problems and new challenges. Am J Transplant. (2013) 13:253–65. doi: 10.1111/ajt.12034
3. Fasullo, M, Ghazaleh, S, Sayeh, W, Vachhani, R, Chkhikvadze, T, Gonda, T, et al. Prognostic factors for non-anastomotic biliary strictures following adult liver transplantation: a systematic review and Meta-analysis. Dig Dis Sci. (2023) 68:2683–94. doi: 10.1007/s10620-023-07861-0
4. Voigtländer, T, Negm, AA, Strassburg, CP, Lehner, F, and Manns, MPLankisch TO. Biliary cast syndrome post-liver transplantation: risk factors and outcome. Liver Int. (2013) 33:1287–92. doi: 10.1111/liv.12181
5. Wang, K, and Wu, S. Biliary cast syndrome. N Engl J Med. (2020) 382:e13. doi: 10.1056/NEJMicm1909877
6. Guichelaar, MM, Benson, JT, Malinchoc, M, Krom, RA, Wiesner, RH, and Charlton, MR. Risk factors for and clinical course of non-anastomotic biliary strictures after liver transplantation. Am J Transplant. (2003) 3:885–90. doi: 10.1034/j.1600-6143.2003.00165.x
7. Waldram, R, Williams, R, and Calne, RY. Bile composition and bile cast formation after transplantation of the liver in man. Transplantation. (1975) 19:382–7. doi: 10.1097/00007890-197505000-00004
8. Manay, P, Seth, A, Jackson, K, Lentine, KL, Schnitzler, MA, Xiao, H, et al. Biliary complications after liver transplantation in the United States: changing trends and economic implications. Transplantation. (2023) 107:e127–38. doi: 10.1097/TP.0000000000004528
9. Mahajani, RV, Cotler, SJ, and Uzer, MF. Efficacy of endoscopic management of anastomotic biliary strictures after hepatic transplantation. Endoscopy. (2000) 32:943–9. doi: 10.1055/s-2000-9619
10. Thuluvath, PJ, Pfau, PR, Kimmey, MB, and Ginsberg, GG. Biliary complications after liver transplantation: the role of endoscopy. Endoscopy. (2005) 37:857–63. doi: 10.1055/s-2005-870192
11. Lin, YC, Lin, TS, Lin, CC, Liu, YW, Wang, SH, Wu, YJ, et al. Can microscopic biliary reconstruction reduce biliary complication rate in ABO-incompatible adult living donor liver transplantation? Ann Transplant. (2021) 26:e931963. doi: 10.12659/AOT.931963
12. Jiménez-Romero, C, Manrique, A, García-Conde, M, Nutu, A, Calvo, J, Caso, Ó, et al. Biliary complications after liver transplantation from uncontrolled donors after circulatory death: incidence, management, and outcome. Liver Transpl. (2020) 26:80–91. doi: 10.1002/lt.25646
Keywords: liver transplantation, biliary complication, non-anastomotic stricture, bile cast syndrome, biliary tree
Citation: Wang P, Zhong L and Zhao D (2025) Case report: Complete cast formation of the entire intrahepatic biliary tree. Front. Med. 12:1525442. doi: 10.3389/fmed.2025.1525442
Received: 09 November 2024; Accepted: 27 January 2025;
Published: 19 February 2025.
Edited by:
Hiroyuki Nojima, Teikyo University Chiba Medical Center, JapanReviewed by:
Farzad Kakaee, Tabriz University of Medical Sciences, IranCopyright © 2025 Wang, Zhong and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dong Zhao, emRvbmcxMjMzQDEyNi5jb20=
†ORCID: Pusen Wang, orcid.org/0009-0008-2947-7992
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.