- 1Sussex Eye Hospital, University Hospitals Sussex NHS Foundation Trust, Brighton, United Kingdom
- 2Department of Ophthalmology, Rabin Medical Center, Petach Tikva, Israel
- 3Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
- 4Brighton and Sussex Medical School, University of Sussex, Brighton, United Kingdom
Purpose: Mini-monovision is a vision correction technique that allows for a broader spectrum of spectacle independence while minimizing anisometropia. This systemic review aims to evaluate the clinical outcomes of pseudophakic mini-monovision with three types of intraocular lenses (IOLs): monofocal, enhanced monofocal, and extended depth of focus (EDOF).
Methods: A comprehensive literature search was conducted using PubMed and MEDLINE to identify studies reporting mini-monovision outcomes within the three categories of IOLs up to July 2024. Inclusion criteria were studies with more than 20 patients, target refraction to achieve mini-monovision difference in the fellow eye, and minimum follow-up of 3 months. The primary outcome measure was uncorrected binocular intermediate visual acuity (UCIVA). The secondary outcomes were binocular uncorrected distance visual acuity (UCDVA), binocular uncorrected near visual acuity (UCNVA), patient-reported outcomes measures (PROMs), spectacle independence, contrast sensitivity, photic phenomenon, enhancement surgeries and IOL exchange.
Results: A total of 113 studies were screened, of which 19, with a total of 1,530 patients, were eligible for inclusion in this review. Mean logMAR binocular UCIVA was 0.16 ± 0.01, 0.11 ± 0.06, 0.08 ± 0.07 (p = 0.41), and mean logMAR UCDVA was 0.08 ± 0.05, 0.04 ± 07, 0.04 ± 0.04 (p = 0.36), in the monofocal, enhanced monofocal, and EDOF groups, respectively. The mean spectacle independence rate was 51% ± 22.1, 55% ± 35.4 and 63.4% ± 24.6 (p = 0.05), respectively, in the monofocal, enhanced monofocal and EDOF groups. A comparable low incidence of halos and glare was observed when enhanced monofocal lenses were evaluated against traditional monofocal lenses. EDOF lenses have, however, demonstrated mixed results. The complications, IOL exchange, and excimer laser enhancement rates were low across all groups.
Conclusion: While enhanced monofocal and EDOF IOLs may provide slightly better binocular intermediate visual outcomes and higher spectacle independence compared to monofocal lenses with regards to mini-monovision and intermediate vision performance, the differences are not statistically significant. All three IOL types exhibit high patient satisfaction rates when choosing a mini-monovision approach with decreased dependence on spectacles.
Introduction
In the ever-evolving landscape of cataract surgery, the scales have now tilted more toward providing refractive correction rather than its original purpose of visual rehabilitation. Advances and innovations in technology have significantly improved the surgical management of presbyopia (1). Given the change in visual needs over time, patients’ expectations for excellent visual performance and spectacle independence not only for distant vision but also for intermediate and near, mainly due to daily tasks that require this range of vision (tablet and smartphone reading, working on computers, driving), have substantially increased (2). Current armamentarium of pseudophakic presbyopia corrections for cataract surgeons primarily include (1) implantation of multifocal intraocular lenses (IOLs), (2) implantation of extended-depth of focus (EDOF) IOLs (3), (3) implantation of accommodative IOLs, and (4) pseudophakic monovision with monofocal IOLs (4).
Multifocal IOLs usually provide high rates of spectacle independence; however, they could be associated with visually significant photic phenomena due to light distribution into multiple foci, especially if patient selection is inappropriate (5–7). Traditional monovision with monofocal IOLs, wherein the dominant eye is targeted for distance emmetropia and the non-dominant is targeted for a near emmetropia leaving a residual myopic error, has been used to overcome the photic phenomena of multifocal IOLs. More recently, mini-monovision with monofocal IOLs, wherein the non-dominant eye is targeted for a relatively smaller residual myopia of −0.75 D to −1.50 D, has been employed and has achieved similar results. This technique also helps in reducing to a greater extent the rate of positive dysphotopsias, being harmless for stereopsis compared to traditional monovision (8). When the non-dominant eye is chosen for distance vision, the technique is crossed monovision. The prevalence of monovision or mini-monovision after cataract surgery is rarely reported in the literature and varies according to clinical practices and the studied population, ranging from 22 to 34% (9). The prevalence can depend on factors such as patient preference, surgeon recommendation, and pre-surgical considerations like the patient’s tolerance to anisometropia (9).
In the hybrid monovision technique, a diffractive multifocal IOL is implanted in the non-dominant eye, whereas a monofocal IOL is implanted in the dominant eye (2). The most widely used approach is the implantation of monofocal IOL in both eyes because of the relatively low-cost of monofocal lenses and satisfying performances for far vision restoration (8, 10).
Extended depth of focus IOLs create an elongated focal point to extend the range of vision and decrease photic phenomena by eliminating overlapping far and near images, thereby accepting some compromise for near-vision (3, 11, 12). The mini-monovision approach has also been successfully adopted with EDOF IOLs (13–20). Another strategy is to employ so-called enhanced monofocal IOLs. These IOLs possess a high-order aspheric anterior surface with a continuous change in power from the periphery toward the lens center (21). This characteristic creates a modified anterior surface with a small central zone designed to extend the depth of focus and consequently improve intermediate vision while maintaining good performance at a distance (22–24) and higher patient satisfaction than classic monofocal IOL (25–28). This maintains a profile similar to photic phenomena in aspheric monofocal IOLs (28). Mini-monovision with these enhanced monofocal IOLs also improves patient satisfaction with low dysphotopsia (21, 29, 30).
The primary objective of this study was to review published literature regarding the efficacy of pseudophakic mini-monovision using monofocal, enhanced monofocal and EDOF IOLs in the correction of presbyopia after cataract extraction in comparison to each other, based on objective parameters, including visual acuity (VA) at near, intermediate and distance and possible complications postoperatively and subjective parameters like patient satisfaction and spectacle independence.
Materials and methods
A comprehensive literature search was conducted to identify studies reporting mini-monovision outcomes after cataract surgery. We included studies that specify mini-monovision refraction targeting in their abstract. We compared three different intra-ocular lens types: monofocal, enhanced monofocal and EDOF IOLs. Inclusion criteria were retrospective or prospective studies published until August 2024 with a minimum of 20 patients and a minimum follow-up of 3 months published in peer-reviewed journals. Studies not published in the English language were excluded.
A systematic literature search for related studies was carried out on PubMed and MEDLINE using the Medical Subject Headings (MeSH) terms “mini-monovision,” “monovision,” “monofocal,” “pseudophakic mini-monovision,” “enhanced monofocal,” “EDOF” and “extended depth of focus.” The Boolean operators “AND” and “OR” combined these MeSH terms and search studies on mini monovision with either of the three IOLs. The initial search was performed without any filters or language restrictions. Data published in any other language but English was excluded from the study. The titles and abstracts resulting from the searches were reviewed. A full-text copy of all potentially relevant studies was reviewed for eligibility, and only those studying mini monovision using monofocal, enhanced monofocal or EDOF IOLs were included in the study.
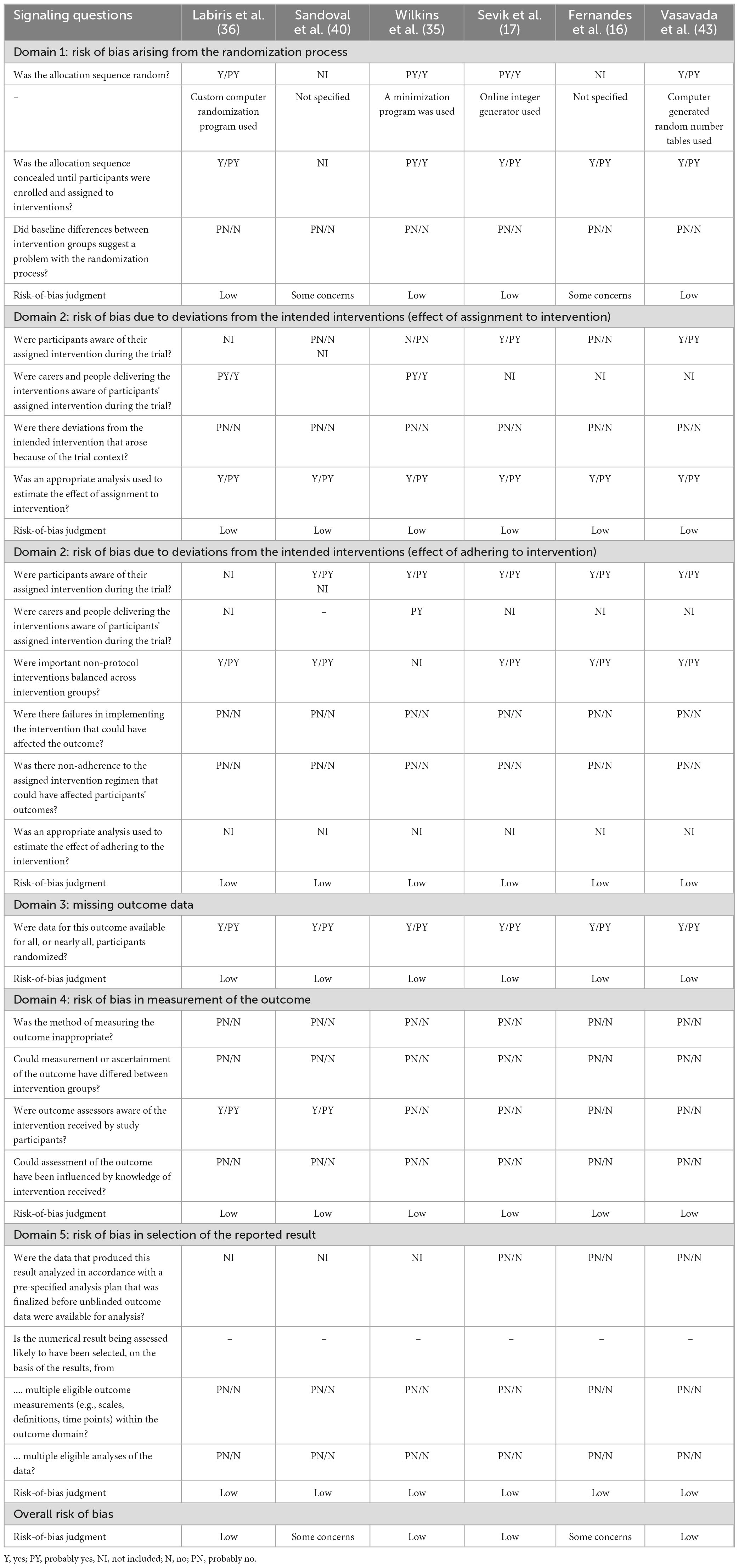
The risk of bias in the articles was assessed using the RoB version 2 tool which considered the following factors: Random sequence generation and allocation concealment (selection bias), blinding of participants (performance bias), blinding of outcome assessment (detection bias), missing outcome data (attrition bias) and selective reporting (reporting bias).
Data collection was performed on an Excel 365 spreadsheet (Microsoft, Redmond, WA, United States) outlining all the relevant parameters. The primary outcome measure was uncorrected binocular intermediate visual acuity (UCIVA). The secondary outcomes were binocular uncorrected distance visual acuity (UCDVA), binocular uncorrected near visual acuity (UCNVA), patient-reported outcomes measures (PROMs), spectacle independence, contrast sensitivity, photic phenomenon, enhancement surgeries and IOL exchange. One review author inputted the data into the spreadsheets; another author re-checked and validated it. Any disagreements regarding the inclusion or exclusion of the studies were resolved through discussion among the authors. We used the data from the latest follow-up visit. The Kolmogorov–Smirnov test was performed to assess the normality of the data distribution, and it was found to have a normal distribution. Then, statistical analysis was performed using Single-factor ANOVA to assess the differences across groups. The level of statistical significance is set at P < 0.05. All visual acuity data were standardized by converting them to logMAR format when originally presented in Snellen or decimal formats. This conversion allowed for uniformity in the measurement scale, enabling more precise statistical interpretation and comparison across datasets. Of all the studies in the three different categories, only Sevik et al. (16) and Lee (20) from the EDOF group reported statistical powers of 0.8 and 0.9, respectively.
Results
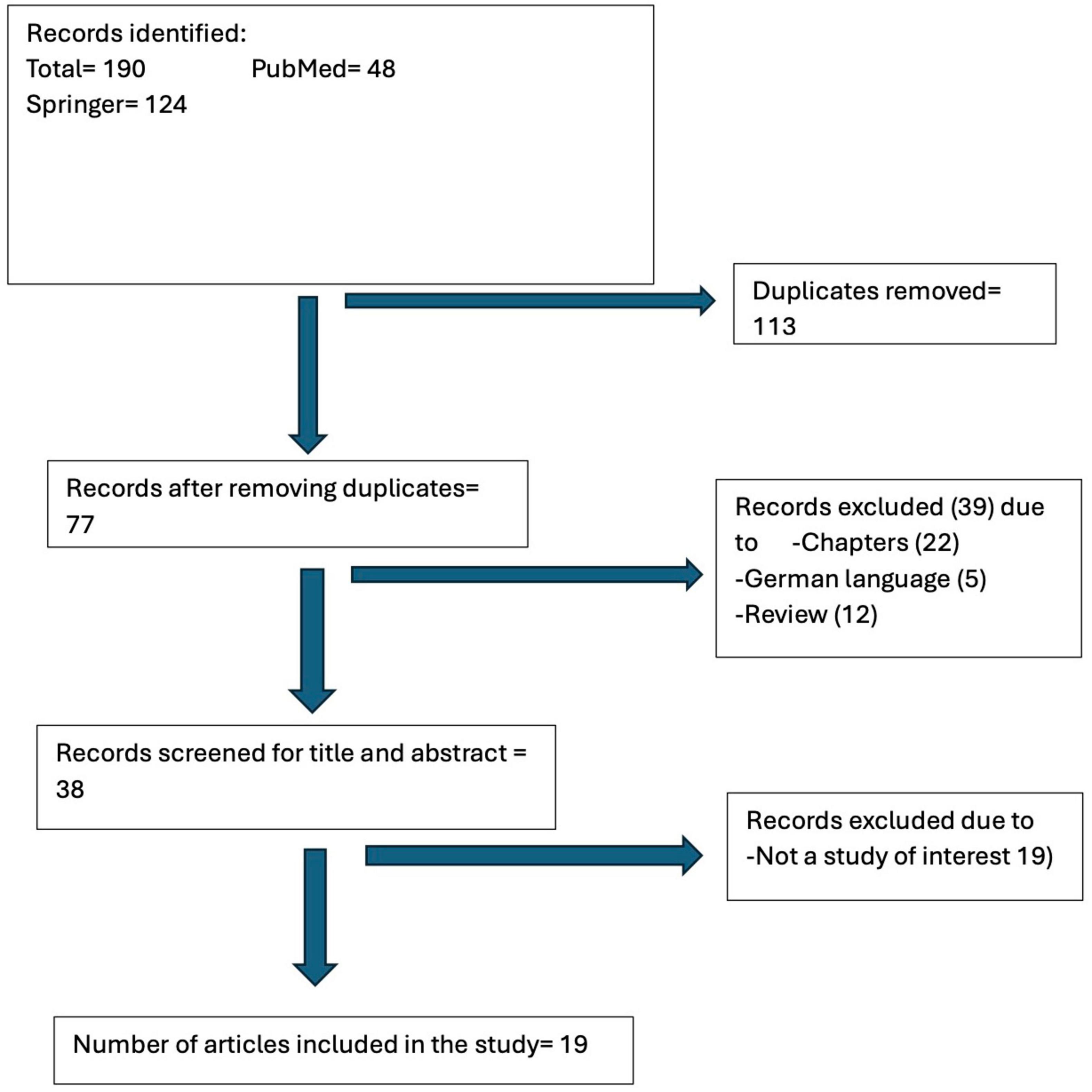
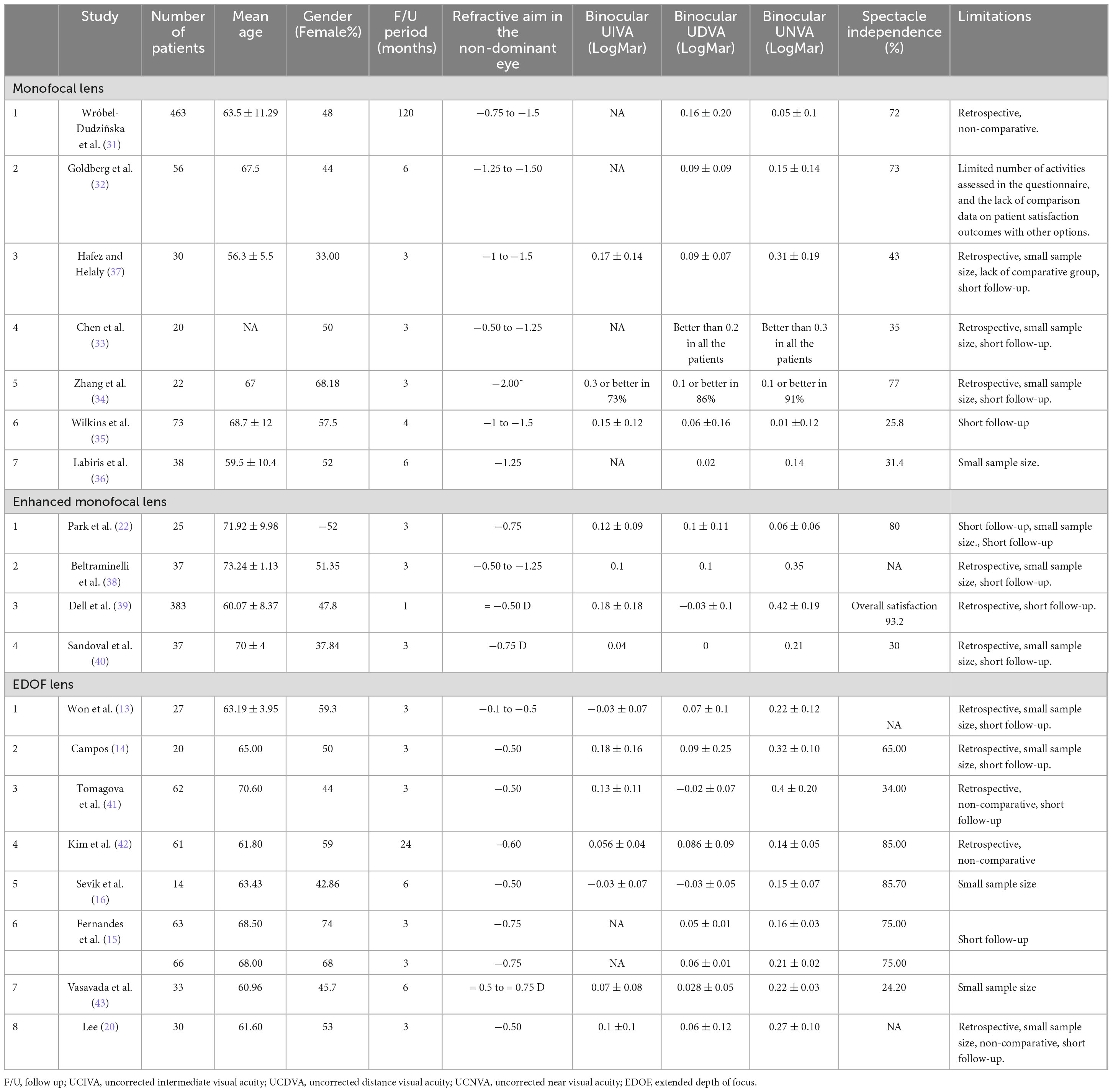
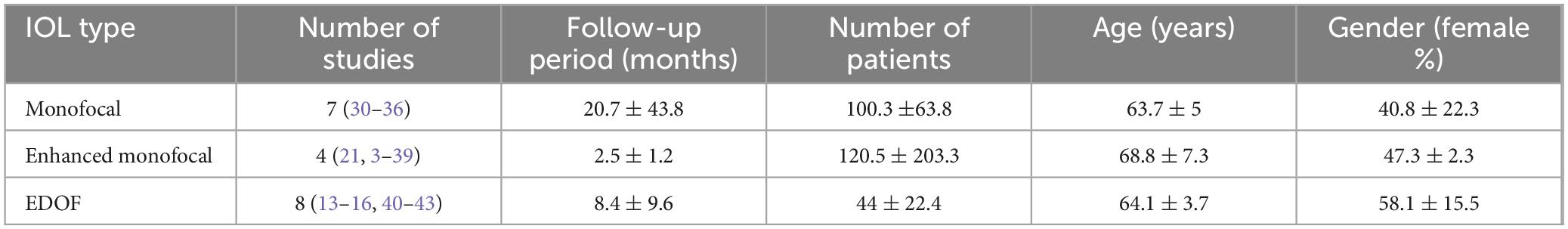
This review included a total of 19 studies published over 17 years involving 1,530 patients (Figure 1). A total of one German article, four German Conference abstracts, 22 chapters and 12 Review articles were excluded (Supplementary Table 1). There were seven studies within the monofocal group (31–37) four in the enhanced monofocal group (22, 38–40), and eight in the EDOF group (13–16, 20, 41–43). The included studies are summarized in Table 1 and the overall demographics in Table 2.
Primary outcome
In the monofocal group the binocular UCIVA was reported only in three of these studies (33, 35, 36). Two studies found a mean of 0.16 ± 0.01 logMAR (criteria of monovision as target postoperative refraction between −0.75 D and −1 D) (35, 37) and one (34) described 0.3 logMAR or better in 73% of the patients (criteria of mini-monovision as target postoperative refraction approximately −2 D) (Table 1). In the enhanced monofocal group the mean binocular UCIVA was 0.11 ± 0.06 logMAR (criteria of mini-monovision as target postoperative refraction between −0.50 D and −0.75 D) and in the EDOF group the mean binocular UCIVA was 0.08 ± 0.07 logMAR (criteria of mini-monovision as target postoperative refraction in all studies up to −0.75 D), respectively. No statistically significant difference was found between the different intraocular lens types (p = 0.41) (Table 1).
Secondary outcomes
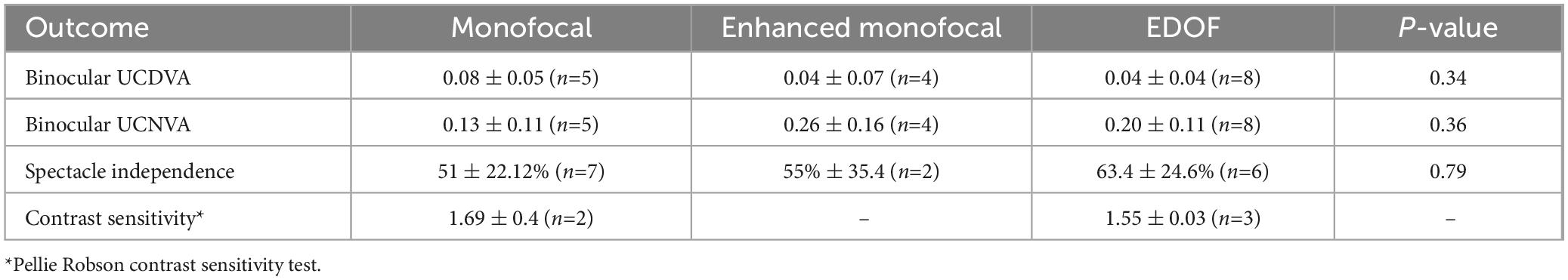
There was no statistically significant difference when comparing mean binocular UDCVA, UCNVA and spectacle independence rates between the different intraocular lens types. The main secondary outcomes are presented in Table 3.
Patient-reported outcomes measures
Spectacle independence
The mini-monovision technique demonstrated that the three types of IOL groups achieved an overall spectacle independence of 50% or more. Patients reported high satisfaction levels, with low rates of needing refractive correction for distance and intermediate vision. Additionally, no statistical differences were observed between the groups (p = 0.78). Within the monofocal group, patients reported a high satisfaction rate with high variability of nearly complete spectacle independence from 25 to 77% (31–37). In the enhanced monofocal group–all studies showed a high satisfaction rate ranging from 84 to 96%, (22, 40) with most patients reporting they would recommend the procedure to others (39). EDOF group– patients showed a high satisfaction rate and variable complete spectacle independent rate from 24 to 75% (13–16, 41–43).
Quality of vision
Studies comparing contrast sensitivity performance in enhanced monofocal lenses versus traditional monofocal lenses found good performance and no statistically significant difference under low and high luminance conditions for any spatial frequency (22, 38, 40, 44).
In the monofocal group, studies observed minimal to no occurrences of clinically significant photic phenomena. Although some studies reported an absence of halos and glare, it is important to note that these studies did not directly inquire about patients’ experiences (31, 32, 37). As expected, significantly fewer complaints of positive photopic phenomena were found compared to those reported with multifocal lenses (1–3, 34–36). A comparable low incidence of halos and glare was observed when enhanced monofocal lenses were evaluated against traditional monofocal lenses (22, 39, 40, 44). EDOF lenses have, however, demonstrated mixed results. Some studies found a similar rate of positive photopic phenomena as in traditional monofocal lenses (16, 20, 43) whilst others experienced frequent halos and glare (14, 41).
Rates of repeat surgical procedures
Intraocular lenses exchange can be offered in cases of patient dissatisfaction due to non-resolved, intolerable, positive dysphotopsias, residual refractive error, or refractive surprise. IOL exchange rate and secondary corneal enhancement therapy were reported only within the monofocal groups. Only two studies provided data on the incidence of secondary corneal enhancement procedures performed via laser vision correction. One study recorded an incidence of 1%, whereas the other reported an incidence of 9.7% (31, 35). Four studies (31, 32, 34, 35) provided data on intraocular lens exchange rate. Goldberg et al. (32) reported an exchange rate of 3.6%, corresponding to two patients, while three other studies indicated no cases of IOL exchange (2–4).
Risk of bias
Six randomized controlled trials [Labiris et al. (36), Sandoval et al. (40), Wilkins et al. (35), Sandoval et al. (17), Sevik et al. (16), Vasavada et al. (43)] were assessed for risk of bias using RoB tool version 2 under five domains (Table 4). Four trials employed the method of computerized randomization and were assessed as low risk. The methods of randomization and allocation concealment employed by Sandoval et al. (40) and Sevik et al. (16) have not been specified, and there could be some concerns pertaining to the risk of bias in these trials. Low risk of bias was seen in the rest of the domains for all trials. Assessment of risk of bias using RoB 2 tool could not be performed for the remaining thirteen studies, as they are observational studies.
Discussion
Our review of 19 studies, including 1,530 patients, found that the mini-monovision technique in cataract surgery, whether using traditional monofocal lenses or more advanced options like enhanced monofocal or EDOF lenses, can be an effective alternative for patients seeking glasses independence (Table 1). The definition of mini-monovision targeting low myopia varies in the literature from a residual refractive error of −0.75 D to −2.00 D in the non-dominant eye (Table 1).
Traditional cataract surgery, involving monofocal lens implantation, significantly improves visual acuity, predominantly for distance vision. However, these lenses offer a limited depth of focus, resulting in a considerable reliance on refractive correction for various daily activities in the intermediate and near vision ranges. The increasing working age and the increased use of computers, tablets, and smartphones as an integral part of almost every daily activity results in decreased functional vision and the need for a cost-effective solution (45). Today, we can offer several types of IOLs to help our patients gain functional vision at a broader range of distances (2), Patients have varying needs and personalities, and some may have ocular comorbidities that can impact their vision. Considering these factors, it’s essential to tailor the choice of intraocular lens to each individual. Multifocal IOLs can provide a wide range of vision; however, they may also lead to an increase in positive dysphotopsias, and a decrease in contrast sensitivity and overall visual quality. Therefore, these lenses are not suitable for everyone (5, 46, 47). As discussed earlier, enhanced monofocal and EDOF IOLs can improve depth-of-focus while providing better intermediate visual acuity and maintaining vision quality similar to monofocal IOLs (48).
We found no statistically significant differences in binocular UCIVA, UCDVA and UCNVA between the three lens types (Table 1). Enhanced monofocal and EDOF lenses, engineered to provide a broader range of vision, did not show significant clinical advantages in this review with regard to UCIVA with mini-monovision (Tables 1, 3). Current literature suggests enhanced monofocal lenses perform slightly better or are comparable to standard monofocal lenses in the distance and intermediate vision (20). In contrast, EDOF lenses are associated with improved intermediate and near visual acuity outcomes (25–30, 49–51).
Patient satisfaction was homogeneously high across all three groups, with most patients reporting positive experience and a decreased need for refractive correction. Spectacle independence rates were reported across all three groups, with rates above 50% in most studies. Enhanced monofocal and EDOF lenses showed slightly incremental improvement, but the difference was not statistically significant. This suggests that monofocal lenses still provide reasonable spectacle independence when using the mini-monovision technique. Although we did not find statistically significant difference in the primary outcomes of UCIVA between the groups, it has to be noted the mean UCIVA was best with EDOF, followed by enhanced monofocal and then monofocal lens (Table 1). Similarly although there was no statistically significant difference in mean percentage of patients achieving spectacle independence (Table 3), spectacle independence was highest in EDOF, followed by enhanced monofocal and then monofocal groups, respectively (Table 3). The lack of statistical significant despite of changes in mean UCIVA and spectacle independence may be attributable to low number included studies in each group, variable definition of mini-monovision used and variations in study designs.
Contrast sensitivity is essential for good functional vision, particularly in low-light settings. It significantly affects visual performance and the ability to distinguish objects and details in those challenging conditions. Contrast sensitivity performance showed no significant differences between traditional monofocal and enhanced monofocal lenses under low and high luminance conditions, confirming that both IOL types offer comparable outcomes. However, EDOF lenses showed some variability, with studies reporting similar or higher halos and glare rates than monofocal lenses (38, 52, 53).
Extended depth of focus lenses are categorized: diffractive, refractive, and hybrid. Halos and glare are particularly associated with diffractive lens designs. Diffractive EDOF IOLs use microstructures to split light into multiple focal points, extending the depth of focus. This can result in scattering, creating positive visual aberrations like halos, especially in low lights. Refractive EDOF IOLs are generally less prone to these effects but can still cause halos and glare if their refractive zones lead to variations in light entering the eye. Overall, these artefacts arise from the lens’s attempt to provide extended vision ranges, which can lead to imperfections in light processing (3, 12, 54). This suggests a need for caution when recommending EDOF lenses to patients sensitive to photic phenomena. Interestingly, enhanced monofocal lenses displayed a low incidence of halos and glare, supporting their value for patients desiring minimal photic disturbances (22, 39, 40, 44). Our review raises an important question–should we offer mini-monovision to all patients undergoing cataract surgery? Patients need to be assessed thoroughly before surgery to understand their needs and functional vision requirements. One way to provide this insight is to use the validated questionnaires in addition to open conversation (55). According to the patient’s ocular history and vision needs, the suitable type of IOL can be selected with the appropriate refractive target. The mini-monovision approach can be particularly beneficial for patients with a high priority on distance vision but requiring only functional intermediate vision. Mini-monovision may provide a reasonable solution by incorporating mild anisometropia. Such a tailored approach, including enhanced monofocal IOLs, should be considered standard practice in cases where full presbyopia correction is either not possible, or not deemed necessary or desired, thereby helping patients achieve greater satisfaction in both visual function and vision-related quality of life.
High levels of safety were found with all lens types using the mini-monovision technique. We describe low rates of IOL exchange and secondary corneal enhancement procedures. IOL exchange was rarely done, which on sight contrast to multifocal IOLs, which are associated with higher rates of IOL exchange due to dissatisfaction with visual quality or photic phenomena. Only two studies provided data on the incidence of secondary corneal enhancement procedures performed via laser vision correction. One study recorded an incidence of 1%, whereas the other reported an incidence of 9.7% (31, 35). Four studies (31, 32, 34, 35) provided data on intraocular lens exchange rate. Goldberg et al. (32) reported an exchange rate of 3.6%, corresponding to two patients, while three other studies indicated no cases of IOL exchange (2–4). There are different reasons for IOL exchange, Goemaere et al. (56) reported a 15 years studies regarding IOL exchange and found IOL opacification to be the primary reason (28%), with multifocal IOL being second with 15%. Dissatisfaction with multifocal IOL can be effectively addressed, not only by exchanging to monofocal IOL but also by selecting an alternative multifocal IOL design (57, 58). Laser vision correction as a secondary enhancement procedure was reported only in two studies (31, 35), with incidences ranging from 1 to 9.7%, suggesting that while secondary interventions are rare, but sometimes necessary to optimize visual outcomes in patients with residual refractive errors (59).
The definition of mini-monovision remains ambiguous, with no clear consensus on the precise refractive targets or optimal range of anisometropia. Traditionally, monovision involves correcting one eye for distance vision and the other for near (60, 61) but mini-monovision aims for a smaller interocular difference, providing a broader range of functional vision with minimal discomfort. In this review, most studies in the monofocal group targeted the myopic eye from −0.75 D up to −1.5 D and one even −2.00 D, (31–37) as opposed to the enhanced monofocal and EDOF lens, where the target was up to −0.75 D (13–16, 20, 41–43). This course can be explained by the broader range of focus these lenses provide. While the ideal target may vary between patients, this range offers a practical compromise for functional vision across distances.
The limitations included an unequal number of studies in each group and variations in study design; some studies had two arms and differing follow-up durations, which may have affected the outcomes. Additionally, not all parameters were reported consistently across the studies, and there is no standard definition of mini-monovision. Furthermore, the outcomes of the enhanced monofocal and EDOF IOLs may vary based on their refractive or diffractive optical designs too and this review does not differentiate the IOLs based on their refractive or diffractive designs. Pertaining to the risk of bias in the trails, two studies did not mention the method of randomization employed. This could raise some concerns regarding risk of bias in these trials. No robust studies comparing two groups of lenses directly for mini-monovision outcomes were identified. Moreover, not all included studies report the statistical power. Further studies are request comparing these three groups of IOLs with adequate statistical power to ensure statistical significance for UCIVA and spectacle independence with mini-monovision.
In summary, our review suggests that, whilst enhanced monofocal and EDOF IOLs may provide slightly better intermediate visual outcomes and higher spectacle independence compared to monofocal lenses with regards to mini-monovision and intermediate vision performance, the differences are not statistically significant. All three IOL types exhibit high patient satisfaction rates when choosing a mini-monovision approach with decreased dependence on spectacles. Monofocal and enhanced monofocal showed the lowest incidence of positive dysphotopsia and comparable contrast sensitivity performance. These findings support using all three lens types depending on patient preferences. Future studies should focus on long-term outcomes and employ standardized tools for evaluating visual performance and patient satisfaction.
Author contributions
IL: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review and editing. RS: Data curation, Formal analysis, Methodology, Project administration, Resources, Writing – original draft, Writing – review and editing. RM: Data curation, Formal analysis, Investigation, Methodology, Resources, Writing – original draft, Writing – review and editing. MN: Conceptualization, Formal analysis, Investigation, Methodology, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1522383/full#supplementary-material
References
1. Saraiva J, Neatrour K, Waring Iv GO. Emerging technology in refractive cataract surgery. J Ophthalmol. (2016) 2016:7309283.
2. Ribeiro F, Dick HB, Kohnen T, Findl O, Nuijts R, Cochener B, et al. Evidence-based functional classification of simultaneous vision intraocular lenses: Seeking a global consensus by the ESCRS Functional Vision Working Group. J Cataract Refract Surg. (2024) 50:794–8. doi: 10.1097/j.jcrs.0000000000001502
3. Nanavaty MA. Evolving generation of new Extended Depth of Focus intraocular lenses. Eye (Lond). (2024) 38:1–3.
4. Charman WN. Developments in the correction of presbyopia II: Surgical approaches. Ophthalmic Physiol Opt. (2014) 34:397–426.
5. De Vries NE, Webers CAB, Touwslager WRH, Bauer NJ, de Brabander J, Berendschot TT, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. (2011) 37:859–65. doi: 10.1016/j.jcrs.2010.11.032
6. Finkelman YM, Ng JQ, Barrett GD. Patient satisfaction and visual function after pseudophakic monovision. J Cataract Refract Surg. (2009) 35:998–1002.
7. Rodov L, Reitblat O, Levy A, Assia EI, Kleinmann G. Visual outcomes and patient satisfaction for trifocal, extended depth of focus and monofocal intraocular lenses. J Refract Surg. (2019) 35:434–40.
8. Mencucci R, Cennamo M, Venturi D, Vignapiano R, Favuzza E. Visual outcome, optical quality, and patient satisfaction with a new monofocal IOL, enhanced for intermediate vision: Preliminary results. J Cataract Refract Surg. (2020) 46:378–87.
9. Bafna S, Gu X, Fevrier H, Merchea M. IRIS§Registry (Intelligent Research In Sight) analysis of the incidence of monovision in cataract patients with bilateral monofocal intraocular lens implantation. Clin Ophthalmol. (2023) 17:3123–9. doi: 10.2147/OPTH.S424195
10. Mahrous A, Ciralsky JB, Lai EC. Revisiting monovision for presbyopia. Curr Opin Ophthalmol. (2018) 29:313–7.
11. Schmid R, Luedtke H, Borkenstein AF. Enhanced depth-of-focus intraocular lenses: Latest wavefront-shaped optics versus diffractive optics. Optom Vis Sci. (2022) 99:335–41.
12. Kanclerz P, Toto F, Grzybowski A, Alio JL. Extended depth-of-field intraocular lenses: An update. Asia Pac J Ophthalmol (Phila). (2020) 9:194–202.
13. Won YK, Choi SH, Chung TY, Lim DH. Clinical outcomes after bilateral implantation of a wavefront-shaping Extended Depth of Focus (EDOF) IOL with mini-monovision. J Clin Med. (2024) 13:3225. doi: 10.3390/jcm13113225
14. Campos N. Clinical outcomes and patient satisfaction of an enhanced depth of focus intraocular lens targeted for mini-monovision. Clin Ophthalmol. (2024) 18:1607–13. doi: 10.2147/OPTH.S459868
15. Fernandes MC, Nunomura CY, Messias A. Visual performance and photic disturbances with diffractive and nondiffractive EDOF intraocular lenses using mini-monovision: Randomized trial. J Cataract Refract Surg. (2024) 50:153–9. doi: 10.1097/j.jcrs.0000000000001330
16. Sevik MO, Akkaya Turhan S, Toker E. Clinical outcomes with a low add multifocal and an extended depth of focus intraocular lenses both implanted with mini-monovision. Eye (Basingstoke). (2022) 36:1168–77. doi: 10.1038/s41433-021-01600-3
17. Sandoval HP, Lane S, Slade SG, Donnenfeld ED, Potvin R, Solomon KD, et al. Defocus curve and patient satisfaction with a new extended depth of focus toric intraocular lens targeted for binocular emmetropia or slight myopia in the non-dominant eye. Clin Ophthalmol. (2020) 14:1791–8.
18. Schojai M, Schultz T, Jerke C, Böcker J, Dick HB. Visual performance comparison of 2 extended depth-of-focus intraocular lenses. J Cataract Refract Surg. (2020) 46:388–93.
19. Sandoval HP, Lane S, Slade S, Potvin R, Donnenfeld ED, Solomon KD, et al. Extended depth-of-focus toric intraocular lens targeted for binocular emmetropia or slight myopia in the nondominant eye: Visual and refractive clinical outcomes. J Cataract Refract Surg. (2019) 45:1398–403.
20. Lee MW. Visual outcomes following bilateral implantation of a non-diffractive extended depth of focus toric intraocular lens using a mini-monovision approach. Int Ophthalmol. (2024) 44:334. doi: 10.1007/s10792-024-03247-x
21. Nanavaty MA, Ashena Z, Gallagher S, Borkum S, Frattaroli P, Barbon E. Visual acuity, wavefront aberrations, and defocus curves with an enhanced monofocal and a monofocal intraocular lens: A prospective, randomized study. J Refract Surg. (2022) 38:10–20.
22. Park ESY, Ahn H, Han SU, Jun I, Seo KY, Kim EK, et al. Visual outcomes, spectacle independence, and patient satisfaction of pseudophakic mini-monovision using a new monofocal intraocular lens. Sci Rep. (2022) 12:21716. doi: 10.1038/s41598-022-26315-7
23. Gigon E, Bouthour W, Panos GD, Pajic B, Massa H. Real world outcomes of the new Tecnis Eyhance IOL. Eur J Ophthalmol. (2023) 33:1390–7.
24. Auffarth GU, Gerl M, Tsai L, Janakiraman DP, Jackson B, Alarcon A, et al. Clinical evaluation of a new monofocal IOL with enhanced intermediate function in patients with cataract. J Cataract Refract Surg. (2021) 47:184–91.
25. Choi WK, Han HJ, Son HS, Khoramnia R, Auffarth GU, Choi CY. Clinical outcomes of bilateral implantation of new generation monofocal IOL enhanced for intermediate distance and conventional monofocal IOL in a Korean population. BMC Ophthalmol. (2023) 23:157. doi: 10.1186/s12886-023-02897-2
26. Goslings O, Veraart H, van de Laar-Muskens J, Piñero DP. Clinical outcomes with an aspheric monofocal and a new enhanced monofocal intraocular lens with modified optical profile. Graefes Arch Clin Exp Ophthalmol. (2023) 261:2315–26. doi: 10.1007/s00417-023-06128-8
27. Giglio R, Vinciguerra AL, Presotto M, Jonak K, Rejdak R, Toro MD, et al. Visual outcomes and patient satisfaction after bilateral implantation of an enhanced monofocal intraocular lens: A single-masked prospective randomized study. Int Ophthalmol. (2024) 44:112. doi: 10.1007/s10792-024-02946-9
28. Micheletti JM, Duncan NB, Hall B. Head-to-head comparison of intermediate vision of two monofocal intraocular lenses. Clin Ophthalmol. (2023) 17:3983–90. doi: 10.2147/OPTH.S444696
29. Corbelli E, Iuliano L, Bandello F, Fasce F. Comparative analysis of visual outcome with 3 intraocular lenses: Monofocal, enhanced monofocal, and extended depth of focus. J Cataract Refract Surg. (2022) 48:67–74. doi: 10.1097/j.jcrs.0000000000000706
30. Corbett D, Black D, Roberts TV, Cronin B, Gunn D, Bala C, et al. Quality of vision clinical outcomes for a new fully-refractive extended depth of focus Intraocular Lens. Eye (Basingstoke). (2024) 38:9–14. doi: 10.1038/s41433-024-03039-8
31. Wróbel-Dudziñska D, Moura-Coelho N, Palma-Carvajal F, Zebdeh A, Manero F, Güell JL. Ten-year outcomes of pseudophakic mini-monovision correction of hyperopic presbyopia. J Cataract Refract Surg. (2023) 49:367–72. doi: 10.1097/j.jcrs.0000000000001116
32. Goldberg DG, Goldberg MH, Shah R, Meagher JN, Ailani H. Pseudophakic mini-monovision: High patient satisfaction, reduced spectacle dependence, and low cost. BMC Ophthalmol. (2018) 18:293. doi: 10.1186/s12886-018-0963-3
33. Chen M, Atebara NH, Chen TT. A comparison of a monofocal acrysoft IOL using the “blended monovision” formula with the multifocal array IOL for glasses independence after cataract surgery. Ann Ophthalmol. (2007) 39:237–40. doi: 10.1007/s12009-007-0035-4
34. Zhang F, Sugar A, Jacobsen G, Collins M. Visual function and patient satisfaction: Comparison between bilateral diffractive multifocal intraocular lenses and monovision pseudophakia. J Cataract Refract Surg. (2011) 37:446–53. doi: 10.1016/j.jcrs.2010.10.045
35. Wilkins MR, Allan BD, Rubin GS, Findl O, Hollick EJ, Bunce C, et al. Randomized trial of multifocal intraocular lenses versus monovision after bilateral cataract surgery. Ophthalmology. (2013) 120:2449–55.e1. doi: 10.1016/j.ophtha.2013.07.048
36. Labiris G, Giarmoukakis A, Patsiamanidi M, Papadopoulos Z, Kozobolis VP. Mini-monovision versus multifocal intraocular lens implantation. J Cataract Refract Surg. (2015) 41:53–7. doi: 10.1016/j.jcrs.2014.06.015
37. Abdelrazek Hafez T, Helaly HA. Spectacle independence and patient satisfaction with pseudophakic mini-monovision using aberration-free intraocular lens. Clin Ophthalmol. (2019) 13:2111–7. doi: 10.2147/OPTH.S215229
38. Beltraminelli T, Rizzato A, Toniolo K, Galli A, Menghini M. Comparison of visual performances of enhanced monofocal versus standard monofocal IOLs in a mini-monovision approach. BMC Ophthalmol. (2023) 23:170. doi: 10.1186/s12886-023-02920-6
39. Dell SJ, Hannan SJ, Venter JA, Teenan D, Hannan NC, Raju D, et al. Comparative analysis of clinical and patient-reported outcomes of a new enhanced monofocal IOL and a conventional monofocal IOL. Clin Ophthalmol. (2024) 18:1157–69. doi: 10.2147/OPTH.S456332
40. Sandoval HP, Potvin R, Solomon KD. Comparing visual performance and subjective outcomes with an enhanced monofocal intraocular lens when targeted for emmetropia or monovision. Clin Ophthalmol. (2023) 17:3693–702. doi: 10.2147/OPTH.S442752
41. Tomagova N, Elahi S, Vandekerckhove K. Clinical outcomes of a new non-diffractive extended depth-of-focus intraocular lens targeted for mini-monovision. Clin Ophthalmol. (2023) 17:981–90. doi: 10.2147/OPTH.S405267
42. Kim J, Kim T, Tchah H, Koh K. Long-term results after bilateral implantation of extended depth of focus intraocular lenses with mini-monovision. Korean J Ophthalmol. (2024) 38:129–36. doi: 10.3341/kjo.2023.0139
43. Vasavada V, Vasavada SA, Shastri L, Nath V, Vasavada AR, Srivastava S. Visual outcomes comparing emmetropia vs mini-monovision after bilateral implantation of a nondiffractive extended vision intraocular lens: Randomized trial. J Cataract Refract Surg. (2024) 50:799–804. doi: 10.1097/j.jcrs.0000000000001458
44. Mencucci R, Morelli A, Cennamo M, Roszkowska AM, Favuzza E. Enhanced monofocal intraocular lenses: A retrospective, comparative study between three different models. J Clin Med. (2023) 12:3588. doi: 10.3390/jcm12103588
45. Ribeiro F, Cochener B, Kohnen T, Mencucci R, Katz G, Lundstrom M, et al. Definition and clinical relevance of the concept of functional vision in cataract surgery ESCRS Position Statement on Intermediate Vision: ESCRS Functional Vision Working Group. J Cataract Refract Surg. (2020) 46 Suppl. 1:S1–3. doi: 10.1097/j.jcrs.0000000000000096
46. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochr Datab Syst Rev. (2016) 2016:CD003169. doi: 10.1002/14651858.CD003169.pub4
47. Cao K, Friedman DS, Jin S, Yusufu M, Zhang J, Wang J, et al. Multifocal versus monofocal intraocular lenses for age-related cataract patients: A system review and meta-analysis based on randomized controlled trials. Surv Ophthalmol. (2019) 64:647–58. doi: 10.1016/j.survophthal.2019.02.012
48. Ribeiro F, Piñero DP, Dick HB, Findl O, Cochener B, Kohnen T. Should enhanced monofocal intraocular lenses be the standard of care? An evidence-based appraisal by the ESCRS Functional Vision Working Group. J Cataract Refract Surg. (2024) 50:789–93. doi: 10.1097/j.jcrs.0000000000001479
49. Nowik KE, Nowik K, Kanclerz P, Szaflik JP. Clinical performance of Extended Depth of Focus (EDOF) intraocular lenses – A retrospective comparative study of mini well ready and symfony. Clin Ophthalmol. (2022) 16:1613–21. doi: 10.2147/OPTH.S341698
50. Chao CC, Lin HY, Lee CY, Mai EL, Lian IB, Chang CK. Difference in quality of vision outcome among extended depth of focus, bifocal, and monofocal intraocular lens implantation. Healthcare (Switzerland). (2022) 10:1000. doi: 10.3390/healthcare10061000
51. Chang DH, Janakiraman DP, Smith PJ, Buteyn A, Domingo J, Jones JJ, et al. Visual outcomes and safety of an extended depth-of-focus intraocular lens: Results of a pivotal clinical trial. J Cataract Refract Surg. (2022) 48:288–97. doi: 10.1097/j.jcrs.0000000000000747
52. Wang J, Che J, Yuan X, Zhang JB. Effects of different types of intraocular lens implantation on patient’s visual quality and function after phacoemulsification. Natl Med J China. (2024) 104:1391–6. doi: 10.3760/cma.j.cn112137-20231125-01198
53. Choi JY, Won YK, Lee SJ, Kang SW, Lim DH. Visual outcomes and patient satisfaction of enhanced monofocal intraocular lens in phacovitrectomy for idiopathic epiretinal membrane. Bioengineering. (2024) 11:939. doi: 10.3390/bioengineering11090939
54. Kohnen T, Berdahl JP, Hong X, Bala C. The novel optical design and clinical classification of a wavefront-shaping presbyopia-correcting intraocular lens. Clin Ophthalmol. (2023) 17:2449–57. doi: 10.2147/OPTH.S400083
55. Lundstrom M, Roos P, Jensen S, Fregell G. Catquest questionnaire for use in cataract surgery care: Description, validity, and reliability. J Cataract Refract Surg. (1997) 23:1226–36.
56. Goemaere J, Trigaux C, Denissen L, Dragnea D, Hua MT, Tassignon MJ, et al. Fifteen years of IOL exchange: Indications, outcomes, and complications. J Cataract Refract Surg. (2020) 46:1596–603. doi: 10.1097/j.jcrs.0000000000000349
57. Al-Shymali O, Cantó M, Alió del Barrio JL, McAlinden C, Yebana P, Alio JL. Managing dissatisfaction after multifocal intraocular lens implantation through lens exchange using monofocal or alternative multifocal IOLs. Acta Ophthalmol. (2024) 102:e1040–9. doi: 10.1111/aos.16720
58. Al-Shymali O, McAlinden C, Alio del Barrio JL, Canto-Cerdan M, Alio JL. Patients’ dissatisfaction with multifocal intraocular lenses managed by exchange with other multifocal lenses of different optical profiles. Eye Vision. (2022) 9:8.
59. Schallhorn SC, Venter JA, Teenan D, Schallhorn JM, Hettinger KA, Hannan SJ, et al. Outcomes of excimer laser enhancements in pseudophakic patients with multifocal intraocular lens. Clin Ophthalmol. (2016) 10:765–76. doi: 10.2147/OPTH.S106731
60. Labiris G, Toli A, Perente A, Ntonti P, Kozobolis VP. A systematic review of pseudophakic monovision for presbyopia correction. Int J Ophthalmol. (2017) 10:992–1000. doi: 10.18240/ijo.2017.06.24
Keywords: mini-monovision, enhanced monofocal intraocular lenses, extended depth of focus intraocular lens, monofocal intraocular lens, intermediate visual acuity
Citation: Levy I, Shah RP, Mukhija R and Nanavaty MA (2025) Outcomes of mini-monovision with monofocal, enhanced monofocal and extended depth-of-focus intraocular lenses. Front. Med. 12:1522383. doi: 10.3389/fmed.2025.1522383
Received: 04 November 2024; Accepted: 17 January 2025;
Published: 21 February 2025.
Edited by:
Ferdinando Cione, University of Salerno, ItalyReviewed by:
Hun Lee, University of Ulsan, Republic of KoreaMarco Gioia, University of Salerno, Italy
Wiktor Stopyra, MW-med Eye Center, Poland
Copyright © 2025 Levy, Shah, Mukhija and Nanavaty. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mayank A. Nanavaty, bWF5YW5rLm5hbmF2YXR5QG5ocy5uZXQ=
 Issac Levy
Issac Levy Rachana Prashant Shah
Rachana Prashant Shah Ritika Mukhija
Ritika Mukhija Mayank A. Nanavaty
Mayank A. Nanavaty