- 1Tongzhou Maternal and Child Health Hospital of Beijing, Beijing, China
- 2Beijing Tongren Eye Center, Beijing Tongren Hospital, Beijing Ophthalmology & Visual Sciences Key Laboratory, Capital Medical University, Beijing, China
- 3Tianjin Key Laboratory of Retinal Functions and Diseases, Tianjin Branch of National Clinical Research Center for Ocular Disease, Eye Institute and School of Optometry, Tianjin Medical University Eye Hospital, Tianjin, China
Background: The high myopia prevalence in young East Asian children necessitates early detection and prevention strategies. Axial length (AL), corneal radius of curvature (CR), and the AL to CR ratio (AL/CR) are potential myopia biomarkers. However, the influence of genetic, growth and development, and environmental factors on these metrics in Chinese preschool children remains unclear. Therefore, this study aimed to investigate the effects of these factors on the AL, CR, and AL/CR ratio in children aged 3–6 years in Beijing.
Methods: In this 3-month study, initiated in November 2021, children aged 3–6 years from nine kindergartens in Beijing were randomly selected for ocular biological parameter measurements. The height and weight of each child were measured, and their parents completed a questionnaire on parental myopia and environmental influences. The AL/CR ratio were calculated. One-way analysis of variance, univariate analysis, and multiple linear regression models (with age, sex, height, weight, parental myopia, continuous near-work time, electronic products use, and outdoor activity time as variables) were used to compare the effects of different variables on the AL, CR, and AL/CR ratio.
Results: Overall, 1,353 participants (708 boys; mean age, 4.37 ± 0.82 years) were included in this study. The multiple linear regression analysis revealed that parental myopia significantly increased the AL and AL/CR ratio (p = 0.002, p < 0.001). Male participants had a longer AL, larger CR, and greater AL/CR ratio than female participants (all p < 0.001). A longer AL and larger CR were associated with greater height (both p < 0.001). The AL/CR ratio increased with age (p < 0.001). The CR was positively associated with the amount of time spent outdoors (p = 0.004).
Conclusion: Ocular biological parameters are influenced by genetic, growth and development, and environmental factors. Among children aged 3–6 years in Beijing, monitoring growth and development, investigating parental myopia, and evaluating eye habits have certain guiding significance for delaying increases in the AL and AL/CR ratio. This study may provide some suggestions for the development of healthy eye habits.
1 Background
Myopia is considered a major public health problem worldwide (1). By 2050, the number of individuals with myopia and high myopia is expected to reach 4.758 billion (prevalence, 49.8%) and 938 million (prevalence, 9.8%), respectively (2). Myopia and high myopia not only cause visual problems but also lead to serious complications, including macular degeneration and retinal detachment, which cause considerable social and economic burdens (3). Early onset myopia can result in severe myopia and subsequent complications (4). By 2050, the prevalence of myopia among children and adolescents in China will reach approximately 84% (5). Therefore, the early detection and prevention of myopia have become the focus of global research.
As children develop, their biometric parameters show varying degrees of change (6). Ocular biometric parameters are potential biomarkers for assessing myopia in children and adolescents (7). The axial length (AL) is a major determinant of myopia (8); the longer the AL, the more severe the myopia (9). Additionally, the AL to corneal radius of curvature (CR) ratio (AL/CR) may be used to evaluate myopia risk (10). The AL/CR ratio is significantly more effective for detecting myopia in children than either naked-eye vision or the AL and could be a useful marker for the onset and development of myopia (11).
Factors affecting myopia development are heritable and influenced by the environment (12, 13). As an endophenotype of myopia with a distinct genetic component (9), the AL/CR ratio is also associated with genetic factors (14). A survey of myopia-related factors in Japanese preschool children indicated that the AL and AL/CR ratio were associated with genetic and environmental factors (15).
Therefore, we aimed to elucidate which factors affect the ocular biological parameters of Chinese children. We conducted a survey to understand the effects of genetic, growth and development, and environmental factors on the ocular biometric parameters of preschool children in Beijing, China.
2 Methods
2.1 Participants
This cross-sectional study, involving a school-based cohort, began in November 2021 across nine kindergartens in the Tongzhou District, Beijing. The detailed methodology has been discussed previously (16). Overall, 1,917 children from two public and seven private kindergartens in Tongzhou District were selected using stratified random cluster sampling. The ocular biological parameters, height, and weight of each child were measured, and parents completed an online questionnaire on parental myopia and environmental influences. The AL/CR ratio were calculated. Children with obvious eye conditions, including glaucoma, cataracts, fundus disease, and strabismus, were excluded from this study. Participants who had difficulty following up or failed to cooperate with the questionnaire and examination were also excluded. Ultimately, 1,353 participants were enrolled in the study.
The study protocol conformed to the tenets of the Declaration of Helsinki, and the Ethics Committee of Beijing Tongren Hospital, affiliated with Capital Medical University, approved this study (TRECKY2020-152). Through online parent meetings, we described the purpose, methods, significance, and precautions of the project to the guardians of the participants, from whom informed consent was obtained.
2.2 Eye measurements
Ophthalmologists and nurses were involved in the study and received professional training before the examination. An ophthalmologist conducted the anterior segment and strabismus examinations. Ocular biometrics were measured in each eye using Lenstar 900 (Haag–Streit, Koeniz, Switzerland). The average of three measurements, automatically documented using the instrument, was recorded as the final result. If a significant deviation was observed in the results, the test was repeated. All participants were tested using the same machine.
The guardians of the participants completed an online questionnaire regarding genetic and environmental factors. Parental myopia was defined as biological parental myopia, and the exact degree was determined. Environmental factors included electronic product use, average daily outdoor time, and average daily continuous near-work time.
2.3 Definitions
Outdoor activities included exercise and rest. Near-work was defined as tasks performed within 33 cm of the eyes. Electronic products included mobile phones, computers, tablet computers, and game consoles. The average daily hours spent outdoors and performing continuous near-work were calculated using the following formula: [(hours spent on weekdays) × 5 + (hours spent on weekends) × 2]/7. Incomplete questionnaires were excluded from the analysis. The CR was determined as the average of the flattest and steepest radius. The AL/CR ratio was calculated as the AL divided by the CR. The correlation of the parameters of the two eyes was analyzed.
2.4 Statistical analysis
Data analysis was performed using R4.2.1 software. Ocular biological parameters are presented as the mean ± standard deviation. Due to the non-normal distribution and lack of variance homogeneity across different classification conditions of ocular biological parameters, the Mann–Whitney U test was used for binary variables. The Kruskal–Wallis test was used for variables with multiple classifications in the univariate analysis to explore the relationships between each risk factor and the AL, CR, and AL/CR ratio. We set the condition from univariate to multivariate. A value of 0.1 was also set to enter multivariate analysis. Subsequently, to understand the influence of parental myopia, environmental factors, sex adjustment, age, and other factors on the AL, CR, and AL/CR ratio, a multiple linear regression model was used. Statistical significance was set at p < 0.05.
3 Results
Overall, 1,353 children participated in this study, including 708 (52.32%) boys and 645 (47.68%) girls. Their ages ranged from 3 to 6 years, with an average age of 4.37 ± 0.82 years. According to the questionnaire, 855 (63.19%) children had parents who had myopia, and 498 (36.81%) had parents who did not have myopia. Additionally, 1,101 (81.37%) children used electronic products. Regarding the daily time spent outdoors, 525 (38.80%), 529 (39.10%), and 299 (22.10%) children spent 0–45, 46–90, and >90 min outdoors, respectively. Concerning the daily time spent performing continuous near-work, 209 (15.45%), 627 (46.34%), 376 (27.79%), and 141 (10.42%) children spent 0–15, 16–30, 31–45, and >45 min, respectively. Furthermore, we found that the AL and CR of the left eyes were highly correlated with those of the right eyes (r = 0.953, p < 0.001; and r = 0.957, p < 0.001, respectively). We chose to analyze data from the right eyes. Data on the demographic characteristics of the participants, parental myopia prevalence, growth and development variables, and environmental factors are presented in Table 1. The distribution density of data is shown in Figure 1.
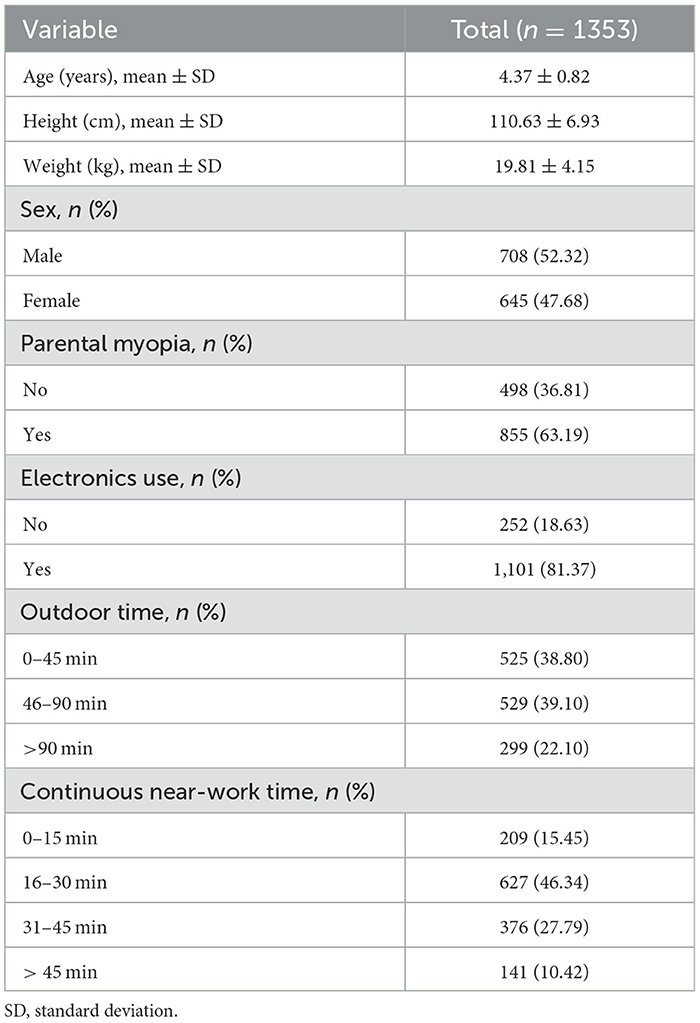
Table 1. Data on demographics, parental myopia, growth and development, and environmental factors in preschool children.
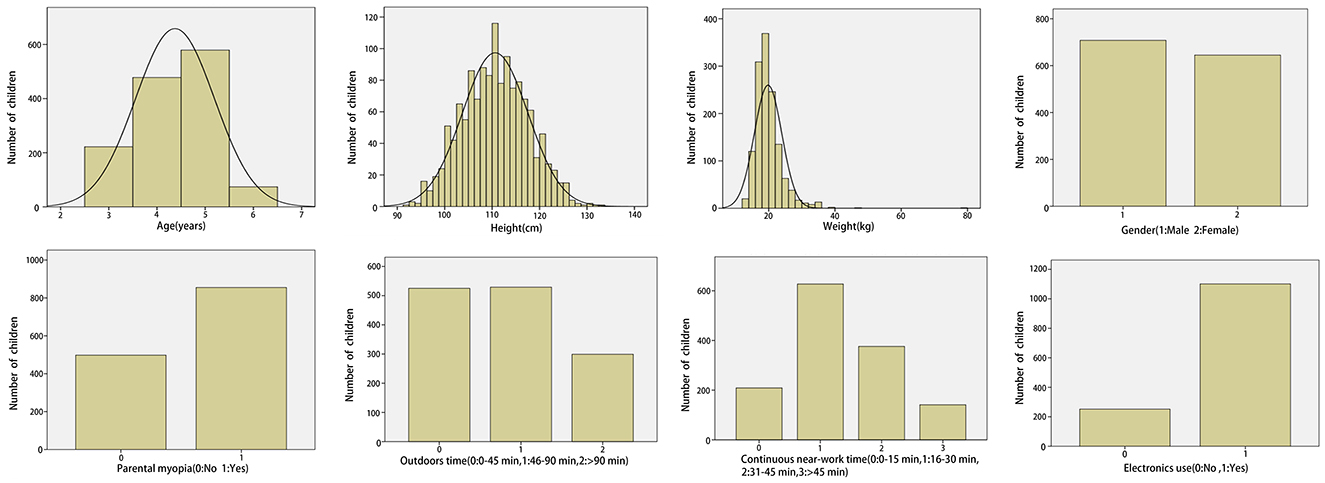
Figure 1. Data distribution density on demographics, parental myopia, growth and development, and environmental factors in preschool children.
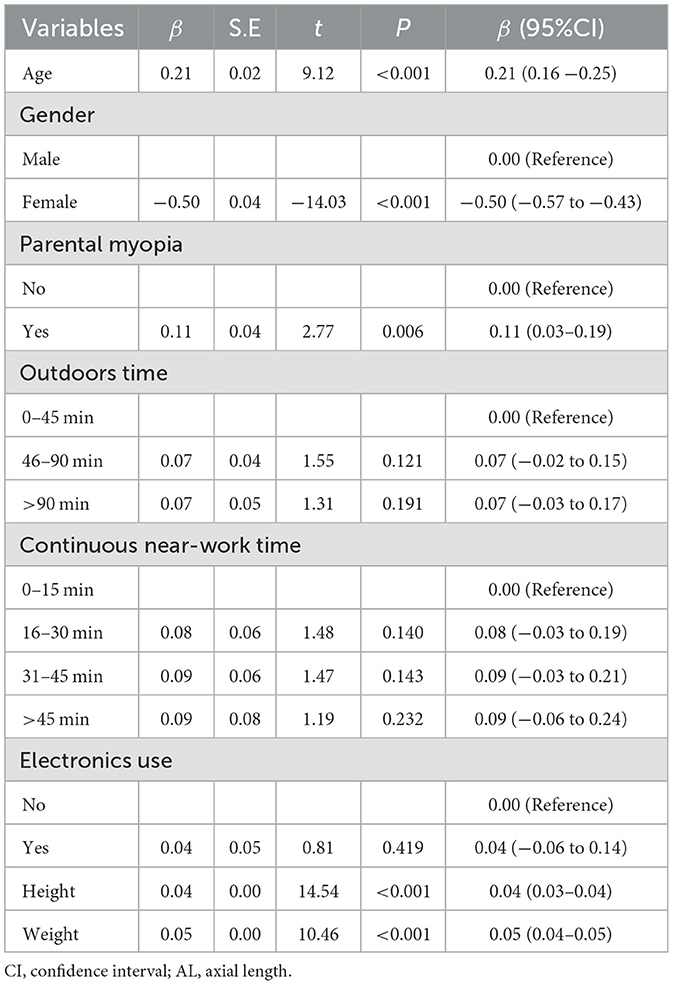
Univariate and multiple linear regression analyses of the impact of sex, age, parental myopia, and environmental factors on the AL are presented in Tables 2, 3. The univariate analysis revealed that longer ALs were significantly associated with older age (p < 0.001), male sex (p < 0.001), greater height (p < 0.001), higher weight (p < 0.001), and parental myopia (p = 0.006). The multiple linear regression model revealed that longer ALs were associated with male sex (p < 0.001), greater height (p < 0.001), and parental myopia (p = 0.002).
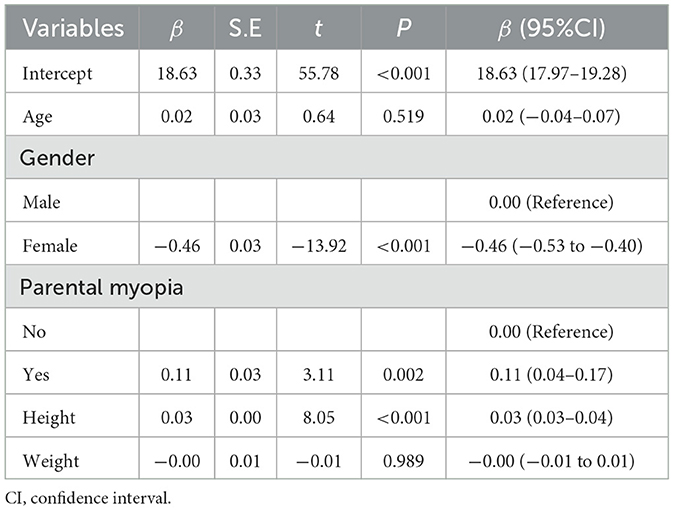
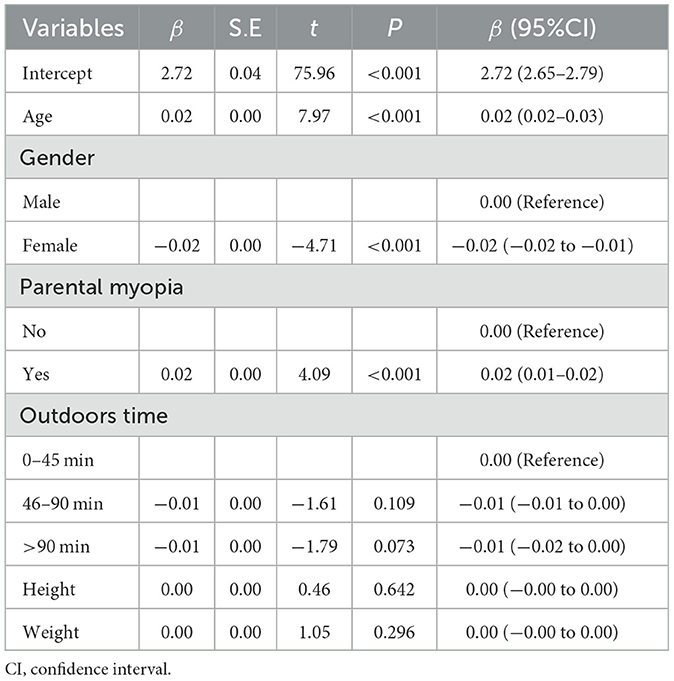
Univariate and multiple linear regression analyses of the impact of sex, age, parental myopia, and environmental factors on the CR are presented in Tables 4, 5. The univariate analysis revealed that larger CRs were associated with male sex (p < 0.001), greater height (p < 0.001), higher weight (p < 0.001). The CR was significantly larger when the time spent outdoors exceeded 45 min (p = 0.023) and even more pronounced when it exceeded 90 min (p = 0.006). The multiple linear regression model revealed that larger CRs were associated with male sex (p < 0.001), greater height (p < 0.001). The CR was significantly larger when the time spent outdoors exceeded 90 min (p = 0.004).
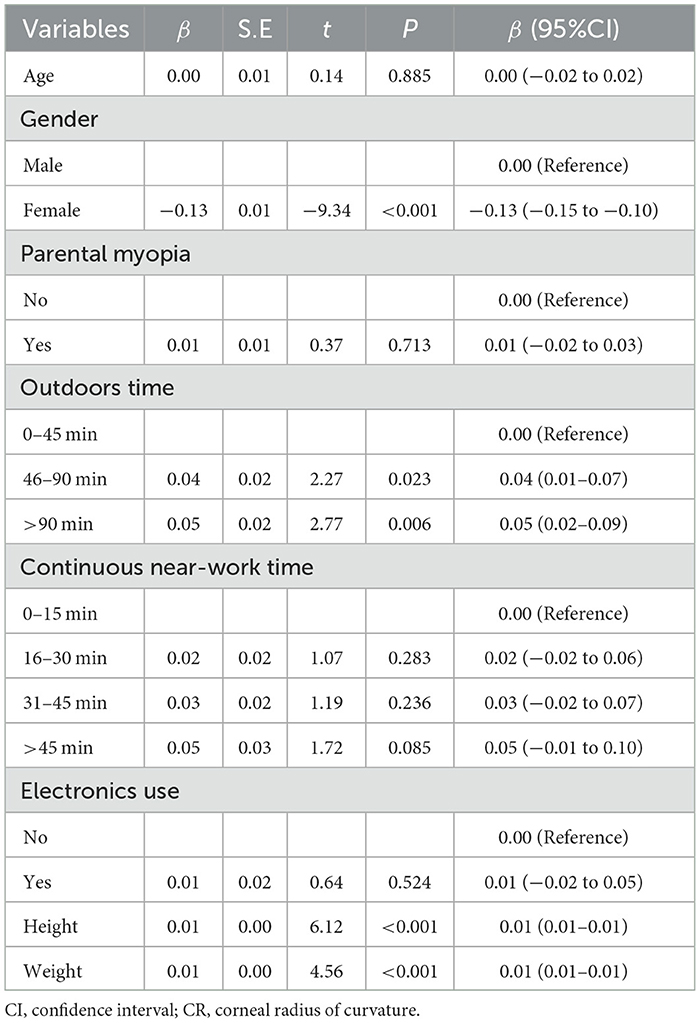
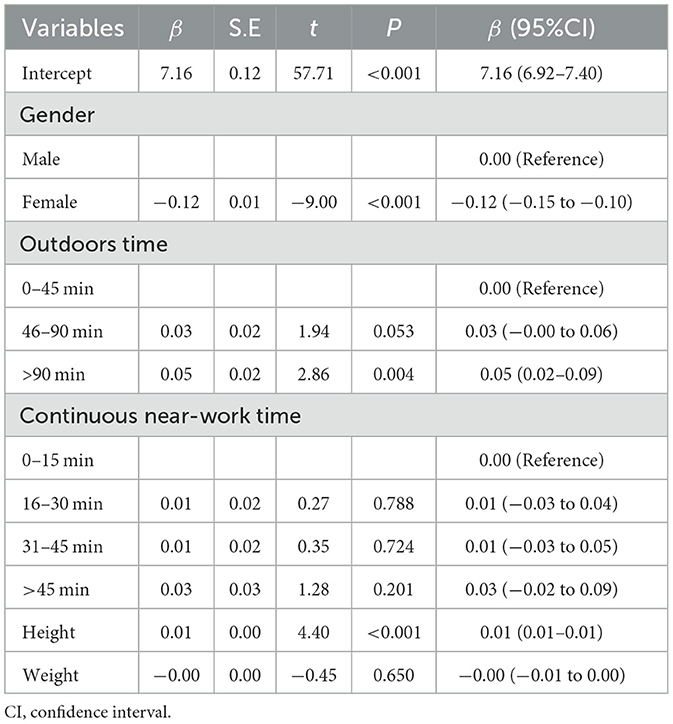
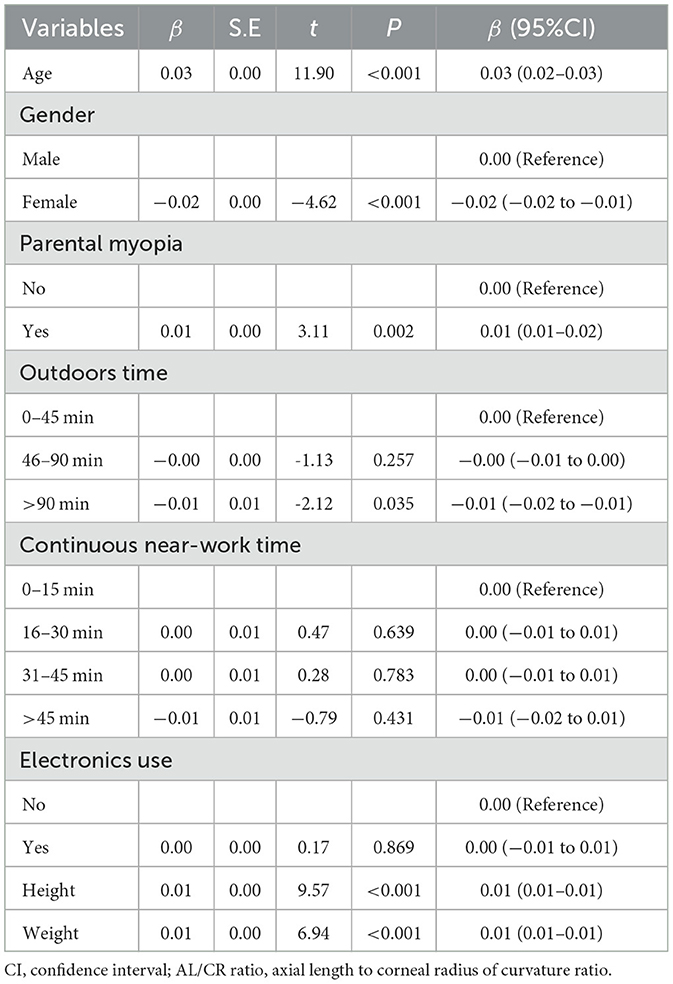
Univariate and multiple linear regression analyses of the impact of sex, age, parental myopia, and environmental factors on the AL/CR ratio are presented in Tables 6, 7. The univariate analysis revealed that higher AL/CR ratios were associated with older age (p < 0.001), male sex (p < 0.001), greater height (p < 0.001), higher weight (p < 0.001), and parental myopia (p = 0.002). When the time spent outdoors exceeded 90 min, the AL/CR ratio decreased (p = 0.035). The multiple linear regression model revealed that greater AL/CR ratios were significantly associated with older age, male sex, and parental myopia (all p < 0.001).
4 Discussion
This study of kindergarten children demonstrated that ocular biological parameters are influenced by genetic, growth and development, and environmental factors. Multivariate analysis revealed that the AL, CR, and AL/CR ratio were greater in boys than in girls. Furthermore, the AL and CR were positively associated with height, while the AL/CR ratio increased with age. Parental myopia was associated with a significantly increased AL and AL/CR ratio, and the CR significantly increased when the daily time spent outdoors exceeded 90 min.
In this study, male sex and greater height were both associated with longer ALs and larger CRs in preschool children, consistent with the findings of previous studies (17–20). These results may be due to the coordinated growth between the eyes and body (21, 22). Zhang et al. (23) reported a significant association between the AL and height. In a 5-year cohort study, the AL was positively correlated with height; therefore, during periods of rapid height growth, more attention should be paid to the AL (21). Previous studies also showed that deeper vitreous cavities, longer ALs, and flatter corneas were observed in taller children (24–26). The AL and height elongation may be mediated partially by common genes (23). Hormone levels also affect the AL, and hormones associated with increased height can accelerate AL growth (27, 28). Therefore, the AL increases concurrently with height. Because boys were taller than girls between the ages of 3 and 6 years (29), they had longer ALs and greater CRs.
Additionally, we found that the AL/CR ratio was higher in males than in females, consistent with previous findings (17). Since most cases of juvenile myopia include axial myopia, AL elongation is considered the most crucial determinant of myopia incidence (30). When the AL is elongated to a certain extent, the CR is compensated, and the lens becomes thinner, focusing parallel light in front of the retina and preventing myopia (31). However, corneal flattening and lens thinning are limited (32–35). As boys develop faster than girls at this age, we speculate that the AL increases more rapidly than the CR; consequently, the AL/CR ratio will also be larger.
In this study, older children had higher AL/CR ratios; however, no significant correlation was found between the CR and age, although the CR increased slightly with age. The Anyang Childhood Eye Study (36) similarly found that 7-year-old children had CRs comparable to those of 14-year-old children. This may be because the corneal power has been shown to remain stable during the preschool stage (37). However, AL increased with age (38). Therefore, these studies collectively demonstrate that the AL/CR ratio increases with age. Our univariate analysis revealed a positive correlation between the AL and age, whereas the multiple linear regression model did not reveal this relationship. Moreover, previous study had demonstrated that older children have shorter CRs (39). Thus, more longitudinal studies are required to further investigate changes in the AL and CR with age during the preschool and school stages.
In our study, the AL and AL/CR ratio were strongly associated with parental myopia. Preschool children with parental myopia had longer ALs and higher AL/CR ratios (15). Klein et al. (40) reported that the refractive index and AL were highly heritable, and another study (9) showed that genes mainly determined the AL. Demir et al. (41) reported that Swedish children with two parents who had myopia had greater myopia and ALs than those with one or no parents with myopia. Edwards et al. (42) proposed that children with parents without myopia had smaller ALs than those with parents with myopia. A 2.5-year longitudinal cohort study (43) showed that children with parents with myopia had a faster rate of AL elongation, particularly those with two parents with myopia. A cohort study of cycloplegic refraction data from 9,793 children aged 6–72 months demonstrated that parental myopia, particularly in both parents, was associated with a greater risk of myopia, less hyperopic refraction, and a higher AL/CR ratio before school age (44). A study reported that when the AL/CR ratio was >2.99, children were more likely to have myopia (45). Therefore, eye development in children with parental myopia should be monitored as early as possible to prevent myopia.
In a 4-year follow-up study of Chinese primary school children in Beijing, greater axial elongation and larger increases in the AL/CR ratio were associated with less time spent outdoors (46). Comparably, a school-based cluster randomized trial showed that more time spent outdoors corresponded to less myopic shift and axial elongation (47). A meta-analysis of clinical studies reported that more hours of outdoor activity was associated with a slower increase in the AL (48). Our study found no significant relationship between the AL, AL/CR ratio, and time spent outdoors. However, this was a cross-sectional study; longitudinal follow-up studies should be conducted to observe the rate of AL, AL/CR ratio changes and determine the relationship between the time spent outdoors and AL, AL/CR ratio growth in preschool children in Beijing. In contrast, we found that the CR increased as the amount of time spent outdoors increased. While a previous study showed that corneal curvature was not associated with time spent outdoors (18). Longitudinally, observations of how the CR of Chinese preschool children changes with an increase in outdoor activity are necessary.
Using multiple linear regression models, we found no significant effects of body weight, continuous close-work time, and electronic use on the biological parameters of the eye. Wong et al. (49) reported that obesity does not affect eye growth. The link between screen time and myopia remains controversial. In one study, increased screen time (screen time >2 h per day) was associated with more myopic SER and a longer AL, shorter CR, and higher AL/CR ratio, while no association was found between ocular biometric parameters and reading time (50). Matsumura et al. (15) reported that a longer AL was significantly associated with screen time (>1 h per day on smartphones, tablets, and computers), while no significant correlation was found between the AL/CR ratio and screen time.
This study had some limitations. First, data on environmental and genetic factors were provided by parents and collected using a self-administered questionnaire, which may introduce recall bias. Second, this was a cross-sectional study, and we could not longitudinally assess how genetic, growth and development, and environmental factors contribute to alterations in ocular biological parameters. Third, we did not compare the effect of myopia severity in parents and the number of parents with myopia on the ocular biological parameters of children. Fourth, the outdoor light intensity was not quantified in this study. Fifth, although we found that genetics, outdoor time, height and other factors have a certain impact on children's eye biological parameters, but the child's other lifestyle, including diet, sleep, screen time, and other factors may also have different degrees of impact on their eye parameters. Therefore, we should have a more comprehensive understanding of children's life and eye habits. In addition, the study was based on data from Beijing, so its generalizability to other regions or countries may be limited. In the future, we will conduct longitudinal, in-depth, comprehensive research on the risk factors for ocular biological parameters.
5 Conclusions
Ocular biological parameters are influenced by genetic, growth and development, and environmental factors. Among children aged 3–6 years in Beijing, monitoring growth and development, investigating parental myopia, and intervening in eye habits have certain guiding significance for delaying the growth of the AL and AL/CR ratio. Our findings are expected to provide new ideas and new methods for the development of healthy eye habits, so that school, family and society can better supervise and develop habits for preschool children.
Data availability statement
The data used and/or analyzed during the current study are available from the corresponding author upon reasonable request. Requests to access the datasets should be directed to Bidan Zhu, emJkMjAxN0BxcS5jb20=.
Ethics statement
The studies involving humans were approved by Ethics Committee of Beijing Tongren Hospital Affiliated with Capital Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
XQ: Data curation, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. YS: Conceptualization, Investigation, Software, Supervision, Validation, Writing – review & editing. SW: Data curation, Investigation, Supervision, Validation, Writing – review & editing. XX: Investigation, Software, Supervision, Validation, Writing – review & editing. LG: Investigation, Supervision, Validation, Writing – review & editing. HL: Investigation, Validation, Writing – review & editing. RW: Conceptualization, Writing – review & editing, Project administration, Supervision. JF: Conceptualization, Formal analysis, Methodology, Project administration, Resources, Supervision, Visualization, Writing – review & editing. BZ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This project was supported by the Tianjin Key Medical Discipline (Specialty) Construction Project [grant number TJYXZDXK-037A] and the Beijing Tongzhou District Outstanding Young Scientists and Technologists Project [grant number JCQN2024030].
Acknowledgments
We would like to acknowledge the contribution of the team of ophthalmologists and nurses, and the school managers and teachers. We also would like to thank Tongzhou Maternal and Child Health Hospital, Beijing Tongren Hospital, and Tianjin Medical University Eye Hospital for data collection, data analysis, and financial support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AL, axial length; CR, corneal radius of curvature; AL/CR ratio, axial length to corneal radius of curvature ratio; CI, confidence interval.
References
1. World Health Organization. The Impact of Myopia and High Myopia. Geneva, Switzerland: World Health Organization (2018).
2. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. (2016) 123:1036–42. doi: 10.1016/j.ophtha.2016.01.006
3. Haarman AEG, Enthoven CA, Tideman JWL, Tedja MS, Verhoeven VJM, Klaver CCW. The complications of myopia: a review and meta-analysis. Invest Ophthalmol Vis Sci. (2020) 61:49. doi: 10.1167/iovs.61.4.49
4. Chua SYL, Sabanayagam C, Cheung YB, Chia A, Valenzuela RK, Tan D, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt. (2016) 36:388–94. doi: 10.1111/opo.12305
5. Dong L, Kang YK, Li Y, Wei WB, Jonas JB. Prevalence and time trends of myopia in children and adolescents in China: a systemic review and meta-analysis. Retina. (2020) 40:399–411. doi: 10.1097/IAE.0000000000002590
6. Mu J, Zhang Z, Wu X, Chen S, Geng H, Duan J. Refraction and ocular biometric parameters in 3-to 6-year-old preschool children: a large-scale population-based study in Chengdu, China. BMC Ophthalmol. (2024) 24:207. doi: 10.1186/s12886-024-03467-w
7. Zhang Z, Mu J, Wei J, Geng H, Liu C, Yi W, et al. Correlation between refractive errors and ocular biometric parameters in children and adolescents: a systematic review and meta-analysis. BMC Ophthalmol. (2023) 23:472. doi: 10.1186/s12886-023-03222-7
8. Jin JX, Hua WJ, Jiang X, Wu XY, Yang JW, Gao GP, et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: the Sujiatun Eye Care Study. BMC Ophthalmol. (2015) 15:73. doi: 10.1186/s12886-015-0052-9
9. Meng W, Butterworth J, Malecaze F, Calvas P. Axial length of myopia: a review of current research. Ophthalmologica. (2011) 225:127–34. doi: 10.1159/000317072
10. Mu J, Zeng D, Fan J, Liu M, Zhong H, Shuai X, Zhang S. The accuracy of the axial length and axial length/corneal radius ratio for myopia assessment among Chinese children. Front Pediatr. (2022) 10:859944. doi: 10.3389/fped.2022.859944
11. Fan Y, Huang Y, Huang X. Association between axial length to corneal curvature radius ratio and myopia in adult patients. J Ophthalmol. (2024) 2024:4981095. doi: 10.1155/2024/4981095
12. Zhao X, Lu X, Yu L, Zhang Y, Li J, Liu Y, et al. Prevalence of myopia and associated risk factors among key schools in Xi'an, China. BMC Ophthalmol. (2022) 22:519. doi: 10.1186/s12886-022-02735-x
13. Shi H, Fu J, Liu X, Wang Y, Yong X, Jiang L, et al. Influence of the interaction between parental myopia and poor eye habits when reading and writing and poor reading posture on prevalence of myopia in school students in Urumqi, China. BMC Ophthalmol. (2021) 21:299. doi: 10.1186/s12886-021-02058-3
14. Li FF, Lu SY, Tang SM, Kam KW, Pancy OST, Yip WWK, et al. Genetic associations of myopia severities and endophenotypes in children. Br J Ophthalmol. (2021) 105:1178–83. doi: 10.1136/bjophthalmol-2020-316728
15. Matsumura S, Dannoue K, Kawakami M, Uemura K, Kameyama A, Takei A, et al. Prevalence of myopia and its associated factors among Japanese preschool children. Front Public Health. (2022) 10:901480. doi: 10.3389/fpubh.2022.901480
16. Zhu B, Sun Y, Wang S, Qin X, Li L, Du B, et al. Refraction and ocular biometric parameters of preschool children in the Beijing whole childhood eye study: the first-year report. BMC Ophthalmol. (2023) 23:366. doi: 10.1186/s12886-023-03112-y
17. Shi Y, Wang Y, Cui A, Liu S, He X, Qiu H, et al. Myopia prevalence and ocular biometry: a cross-sectional study among minority versus Han schoolchildren in Xinjiang Uygur autonomous region, China. Eye. (2022) 36:2034–43. doi: 10.1038/s41433-021-01506-0
18. Li T, Wan T, Yao X, Qi H, Chen X, She M, et al. Time trend of axial length and associated factors in 4- and 5-year-old children in Shanghai from 2013 to 2019. Int Ophthalmol. (2021) 41:835–43. doi: 10.1007/s10792-020-01637-5
19. Rudnicka AR, Owen CG, Nightingale CM, Cook DG, Whincup PH. Ethnic differences in the prevalence of myopia and ocular biometry in 10- and 11-year-old children: the Child Heart and Health Study in England (CHASE). Invest Ophthalmol Vis Sci. (2010) 51:6270–6. doi: 10.1167/iovs.10-5528
20. Ip JM, Huynh SC, Robaei D, Kifley A, Rose KA, Morgan IG, et al. Ethnic differences in refraction and ocular biometry in a population-based sample of 11-15-year-old Australian children. Eye. (2008) 22:649–56. doi: 10.1038/sj.eye.6702701
21. Tao L, Wang C, Peng Y, Xu M, Wan M, Lou J, et al. Correlation between increase of axial length and height growth in Chinese school-age children. Front Public Health. (2021) 9:817882. doi: 10.3389/fpubh.2021.817882
22. Saw SM, Chua WH, Hong CY, Wu HM, Chia KS, Stone RA, et al. Height and its relationship to refraction and biometry parameters in Singapore Chinese children. Invest Ophthalmol Vis Sci. (2002) 43:1408–13.
23. Zhang J, Hur YM, Huang W, Ding X, Feng K, He M. Shared genetic determinants of axial length and height in children: the Guangzhou twin eye study. Arch Ophthalmol. (2011) 129:63–8. doi: 10.1001/archophthalmol.2010.323
24. Northstone K, Guggenheim JA, Howe LD, Tilling K, Paternoster L, Kemp JP, et al. Body stature growth trajectories during childhood and the development of myopia. Ophthalmology. (2013) 120:1064–73.e1. doi: 10.1016/j.ophtha.2012.11.004
25. Tideman JWL, Polling JR, Jaddoe VWV, Vingerling JR, Klaver CCW. Growth in foetal life, infancy, and early childhood and the association with ocular biometry. Ophthalmic Physiol Opt. (2019) 39:245–52. doi: 10.1111/opo.12630
26. Li L, Liao C, Zhang X, Lu J, Zeng Y, Fu M, et al. Association between body stature with ocular biometrics and refraction among Chinese preschoolers. BMC Ophthalmol. (2024) 24:107. doi: 10.1186/s12886-024-03372-2
27. Liu YX, Sun Y. MMP-2 participates in the sclera of guinea pig with form-deprivation myopia via IGF-1/STAT3 pathway. Eur Rev Med Pharmacol Sci. (2018) 22:2541–8. doi: 10.26355/eurrev_201805_14945
28. Prashar A, Hocking PM, Erichsen JT, Fan Q, Saw SM, Guggenheim JA. Common determinants of body size and eye size in chickens from an advanced intercross line. Exp Eye Res. (2009) 89:42–48. doi: 10.1016/j.exer.2009.02.008
29. Li H, Ji CY, Zong XN, Zhang YQ. Height and weight standardized growth charts for Chinese children and adolescents aged 0 to 18 years. Zhonghua Er Ke Za Zhi (2009) 47:487–92.
30. Young TL, Metlapally R, Shay AE. Complex trait genetics of refractive error. Arch Ophthalmol. (2007) 125:38–48. doi: 10.1001/archopht.125.1.38
31. He SY, He T, Xu MY, Ni YJ, Hong CY, Shen T. Distribution and correlation of refractive parameters in children with different corneal curvatures in southeast China. Int J Ophthalmol. (2024) 17:713–20. doi: 10.18240/ijo.2024.04.16
32. Rozema J, Dankert S, Iribarren R, Lanca C, Saw SM. Axial growth and lens power loss at myopia onset in Singaporean children. Invest Ophthalmol Vis Sci. (2019) 60:3091–9. doi: 10.1167/iovs.18-26247
33. Hashemi H, Pakzad R, Khabazkhoob M, Yekta A, Emamian MH, Fotouhi A. Ocular biometrics as a function of age, gender, height, weight, and its association with spherical equivalent in children. Eur J Ophthalmol. (2021) 31:688–97. doi: 10.1177/1120672120908722
34. Momeni-Moghaddam H, Hashemi H, Zarei-Ghanavati S, Ostadimoghaddam H, Yekta A, Khabazkhoob M. Four-year change in ocular biometric components and refraction in schoolchildren: a cohort study. J Curr Ophthalmol. (2019) 31:206–13. doi: 10.1016/j.joco.2018.10.009
35. Xiao H, Jiang D, Wang Y, Sun B, Li C, Lin Y, et al. A comparative study of the prevalence of myopia and behavioral changes in primary school students. BMC Ophthalmol. (2022) 22:370. doi: 10.1186/s12886-022-02594-6
36. Li SM, Li SY, Kang MT, Zhou YH, Li H, Liu LR, et al. Distribution of ocular biometry in 7- and 14-year-old Chinese children. Optom Vis Sci. (2015) 92:566–72. doi: 10.1097/OPX.0000000000000570
37. Guo X, Fu M, Ding X, Morgan IG, Zeng Y, He M. Significant axial elongation with minimal change in refraction in 3- to 6-year-old Chinese preschoolers: the Shenzhen Kindergarten Eye Study. Ophthalmology. (2017) 124:1826–38. doi: 10.1016/j.ophtha.2017.05.030
38. Rauscher FG, Francke M, Hiemisch A, Kiess W, Michael R. Ocular biometry in children and adolescents from 4 to 17 years: a cross-sectional study in central Germany. Ophthalmic Physiol Opt. (2021) 41:496–511. doi: 10.1111/opo.12814
39. Saw SM, Carkeet A, Chia KS, Stone RA, Tan DTH. Component dependent risk factors for ocular parameters in Singapore Chinese children. Ophthalmology. (2002) 109:2065–71. doi: 10.1016/S0161-6420(02)01220-4
40. Klein AP, Suktitipat B, Duggal P, Lee KE, Klein R, Bailey-Wilson JE, Klein BEK. Heritability analysis of spherical equivalent, axial length, corneal curvature, and anterior chamber depth in the Beaver Dam Eye Study. Arch Ophthalmol. (2009) 127:649–55. doi: 10.1001/archophthalmol.2009.61
41. Demir P, Baskaran K, Theagarayan B, Gierow P, Sankaridurg P, Macedo AF. Refractive error, axial length, environmental and hereditary factors associated with myopia in Swedish children. Clin Exp Optom. (2021) 104:595–601. doi: 10.1080/08164622.2021.1878833
42. Edwards MH. Effect of parental myopia on the development of myopia in Hong Kong Chinese. Ophthalmic Physiol Opt. (1998) 18:477–83. doi: 10.1016/S0275-5408(98)00019-2
43. Jiang D, Lin H, Li C, Liu L, Xiao H, Lin Y, Huang X, Chen Y. Longitudinal association between myopia and parental myopia and outdoor time among students in Wenzhou: a 2.5-year longitudinal cohort study. BMC Ophthalmol. (2021) 21:11. doi: 10.1186/s12886-020-01763-9
44. Jiang X, Tarczy-Hornoch K, Cotter SA, Matsumura S, Mitchell P, Rose KA, et al. Association of parental myopia with higher risk of myopia among multiethnic children before school age. JAMA Ophthalmol. (2020) 138:501–9. doi: 10.1001/jamaophthalmol.2020.0412
45. He X, Zou H, Lu L, Zhao R, Zhao H, Li Q, et al. Axial length/corneal radius ratio: association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PLoS ONE. (2015) 10:e0111766. doi: 10.1371/journal.pone.0111766
46. Guo Y, Liu LJ, Tang P, Lv YY, Feng Y, Xu L, Jonas JB. Outdoor activity and myopia progression in 4-year follow-up of Chinese primary school children: the Beijing Children Eye Study. PLoS ONE (2017) 12:e0175921. doi: 10.1371/journal.pone.0175921
47. He X, Sankaridurg P, Wang J, Chen J, Naduvilath T, He M, et al. Time outdoors in reducing myopia: a school-based cluster randomized trial with objective monitoring of outdoor time and light intensity. Ophthalmology. (2022) 129:1245–54. doi: 10.1016/j.ophtha.2022.06.024
48. Deng L, Pang Y. Effect of outdoor activities in myopia control: meta-analysis of clinical studies. Optom Vis Sci. (2019) 96:276–82. doi: 10.1097/OPX.0000000000001357
49. Wong TY, Foster PJ, Johnson GJ, Klein BEK, Seah SKL. The relationship between ocular dimensions and refraction with adult stature: the Tanjong Pagar survey. Invest Ophthalmol Vis Sci. (2001) 42:1237–42.
Keywords: ocular biological parameters, preschool children, parental myopia, eye habits, growth and development
Citation: Qin X, Sun Y, Wang S, Xie X, Gao L, Li H, Wei R, Fu J and Zhu B (2025) Risk factors for ocular biological parameters in Chinese preschool children: a cohort study from the Beijing whole childhood eye study. Front. Med. 12:1510124. doi: 10.3389/fmed.2025.1510124
Received: 12 October 2024; Accepted: 20 January 2025;
Published: 07 February 2025.
Edited by:
Lei Wan, China Medical University, TaiwanReviewed by:
Thiago Gonçalves dos Santos Martins, Federal University of São Paulo, BrazilXiu-Feng Huang, The Second Affiliated Hospital and Yuying Children's Hospital of Wenzhou Medical University, China
Copyright © 2025 Qin, Sun, Wang, Xie, Gao, Li, Wei, Fu and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bidan Zhu, emJkMjAxN0BxcS5jb20=; Jing Fu, ZnVfamluZ0AxMjYuY29t
 Xi Qin
Xi Qin Yunyun Sun
Yunyun Sun Shana Wang1
Shana Wang1 Ruihua Wei
Ruihua Wei Jing Fu
Jing Fu Bidan Zhu
Bidan Zhu