- 1Andrija Štampar School of Public Health, School of Medicine, University of Zagreb, Zagreb, Croatia
- 2Department of Obstetrics and Gynecology, University Hospital Centre, Zagreb, Croatia
- 3Institute for Emergency Medicine Virovitica- Podravina County, Virovitica, Croatia
- 4Independent Consultant, Zagreb, Croatia
- 5Independent Consultant in Health System Funding Models, Eaglehawk Neck, TAS, Australia
- 6School of Medicine, University of Zagreb, Zagreb, Croatia
Background: The COVID-19 pandemic placed unprecedented pressure on healthcare systems worldwide and altered patients' perceptions of the system's ability to protect them from virus transmission. One significant consequence was a marked decline in hospital activity, a trend observed globally. This study aims to evaluate the impact of COVID-19 on hospitalization rates among patients with gynecological disorders in Croatia. It compares the number of patients treated surgically vs. conservatively before the pandemic (2017–2019) and during the pandemic (2020–2022) using the Diagnostic-Related Group (DRG) patient classification system. The DRG system is designed to group patients based on similar clinical conditions, complexity, and resource utilization. Hospital activity categorized by DRGs was analyzed to assess the impact of the COVID-19 pandemic on case volumes within DRG groups associated with gynecological and obstetric disorders.
Materials and methods: We conducted a comparative descriptive cross sectional study of the pre-post type according to STROBE guidelines to determine the impact of COVID-19 pandemic on hospital admission rates for patients with conditions associated with illnesses and abnormalities of the female reproductive system, as well as pregnancy, delivery, and the puerperium. The publicly available data collected by Croatian Institute of Public Health (CIPH) and the Croatian Health Insurance Fund (CHIF) were the main data source for this study. All gynecological hospital admissions in Croatia were grouped based on the Australian Refined Diagnosis Related Groups (AR-DRGs) and analyzed over two time periods: before (2017–2019) and during the pandemic (2020–2022).
Results: The average number of gynecological patients in all hospitals during the pandemic was 62,257 compared to pre-pandemic when the average number of patients was 71,519, a decrease of 15.5%. The results show a 10.56% decrease in the total number of non-surgical admissions and 12.8% decrease of surgical admissions across the hospital network during the pandemic (2020–2022).
Conclusion: The COVID-19 pandemic led to a significant decline in inpatient treatments in gynecology and obstetrics departments in Croatia. Our findings highlight the need for obstetrics and gynecology practitioners to develop innovative strategies to maintain or enhance patient access to appropriate care while ensuring stringent infection prevention measures for both patients and healthcare personnel. Furthermore, investing in healthcare system resilience is crucial to maintaining core functions during future crises. The lessons learned from the COVID-19 pandemic provide a valuable opportunity to fortify healthcare systems and must not be ignored.
Introduction
The COVID-19 outbreak, that originated in China, rapidly spread worldwide in 2020, culminating in a global pandemic. In response, governments urgently worked to reorganize their healthcare resources to meet the escalating demand for the treatment and management of COVID-19 patients (1).
Simultaneously, a multidisciplinary efforts and research by experts from various medical specialties led to the publication of academic papers that examined the direct impact of COVID-19 on specific illness categories and in the process proposed the postponement of non-urgent medical treatments and surgical procedures (2, 3). This recommendation was intended among other things, to alleviate the overcrowding in hospitals and healthcare facilities, and thereby the likely spread of the infection. The result of all these control activities was that governments introduced extensive public health measures which included social isolation, border closures, school closures, procedures to isolate symptomatic persons and their social contacts, and population lockdowns save for necessary internal transit (4). The duration of the lockdowns, depended on the spread of the SARS-CoV-2 pandemic in jurisdictions.
One consequence of these measures was that patients reduced or stopped seeking care and visiting medical care facilities and hospitals to minimize their risk of virus exposure. This avoidance was particularly pronounced among older age groups, who experienced heightened anxiety about COVID-19 due to their increased risk of severe outcomes. This demographic was especially proactive in adopting preventive measures, such as avoiding crowded areas, wearing protective masks, and practicing frequent handwashing (5).
As the decline in hospital activity became evident, innovative approaches were implemented to ensure continued access to healthcare services. Contactless solutions, such as telemedicine, were introduced to bridge the gap and maintain patient care (6). Telemedicine, as defined by the World Health Organization, is the use of information and communication technology to offer medical treatments where distance is a significant problem for all medical professionals (7).
Before COVID-19, the use of telemedicine in gynecology was primarily limited to activities related to prenatal care or as part of sexually transmitted disease awareness campaigns, often delivered through online learning courses or webinars. As a result, clinicians specializing in gynecology and obstetrics had minimal experience with telemedicine, with their lack of knowledge and expertise presenting a significant barrier to its broader adoption. Additionally, other challenges in implementing telemedicine within gynecology included high administrative costs and inadequate reimbursement structures, further hindering its integration into routine practice.
Therefore, the COVID-19 pandemic highlighted, among other issues, the underrepresentation of telemedicine in gynecology compared to its more established use in fields like internal medicine, anesthesia, and intensive care (8, 9). More studies into the viewpoints and preferences of doctors, patients, and other telemedicine users in gynecology are critical in the field of telemedicine. This can serve as the foundation for the specific patient and physician-tailored telemedicine solutions, as well as the development and improvement of patient triage processes for digital or analog consultation hours (8, 10, 11).
As the pandemic unfolded it became clear that COVID-19 had an adverse impact on maternal-fetal wellbeing and obstetric treatment (12), and pregnancy is being considered a risk factor for a severe course of COVID-19 (13). Furthermore, COVID-19 infection during pregnancy has been associated with changes in pregnancy management (14), an increase in miscarriage pregnancy outcomes (15, 16), and need for hospitalization (17) and preterm delivery in more than half of affected cases (18). As pregnancy is associated with a higher risk of severe COVID-19 compared with the non-pregnant population, including pneumonia, admission to the ICU and death, a thorough follow-up of pregnant women with SARS-CoV-2 infection is needed in order to identify those cases at higher risk of developing the most severe spectrum of disease (19).
Croatia's strategy for COVID-19 was generally similar to those of other European countries. According to the Government Stringency Index (GSI), Croatia's mitigation measures were initially quite stringent (with a GSI close to 100), but by late November 2020, they could be considered to be relatively mild (with a GSI around 50 and later on 30).
This study aims to evaluate the direct impact of COVID-19 on the number of hospitalized patients with gynecological illnesses contained in Chapter 2 (Neoplasms), Chapter 14 (parts related to Diseases of the female genitourinary system) and Chapter 15 (Pregnancy, Childbirth and Puerperium) of International Classification of Diseases, Tenth Revision at the secondary, and tertiary healthcare levels in Croatia, in the period before (2017–2019) and during the pandemic (2020–2022). By determining which types of patients were mostly affected may serve as a guiding principle in the process of enhancing resilience of health care system delivery.
Materials and methods
Study design and setting
This study is comparative, descriptive cross-sectional study of the pre-post type according to STROBE guidelines.
The data were acquired from databases maintained by the Croatian Institute of Public Health (CIPH) and the Croatian Health Insurance Fund (CHIF), both of which are open to the public (20). Croatian patient classification system is based on the Australian Refined–Diagnosis Related Group version 5.2 (AR-DRG). AR-DRGs is a classification that provides a clinically meaningful way to group admitted patients with similar diagnosis and similar resource consumption into the same group (21). The AR-DRG structure is based on 23 Major Diagnostic Categories (MDC) defined by the principal diagnoses, which is the primary reason for patient being admitted in hospital.
Each of the MDC representing a different body system or etiology is defined by the principle diagnosis which represent the main reason for patient being admitted in the hospital. In this study, the main interest was the MDC131 and MDC142 groups because they include diseases and disorders of the female reproductive system, as well as pregnancy, childbirth, and the puerperium, respectively (22).
Participant eligibility criteria
The Australian Refined Diagnosis-Related Groups (AR-DRG) system has been used in Croatia since 2009 as a patient classification system primarily aimed at reporting inpatient activity within the acute hospital network for reimbursement purposes. A key advantage of employing a well-structured classification system like AR-DRG is the comprehensiveness of the data collected. Each episode of care for an admitted patient is coded according to specific standards, ensuring that the principal diagnosis, additional diagnoses, and both operative and non-operative procedures, such as endoscopies, are accurately recorded.
In this system, the principal and additional diagnosis are coded using the International Classification of Diseases, Tenth Revision, Australian modification (ICD 10–AM) Tabular List of diseases that contains the disease classification itself at the three, four and five character levels. Procedures are coded using the Australian Classifications of interventions (ACHI) and the structure of procedure classifications is based on anatomy rather than surgical specialty. Every admitted patient is included in the Croatian DRG data base, and therefore only the inpatient case is included in the database used in the study.
Since the purpose of our study is to examine the impact of pandemic on inpatient admissions reported by acute hospital network, we selected the timeline for data analysis as the period 2017–2022 inclusive. These hospitals serve a population of 3.9 million people providing for 96% of all inpatient activity. The study included 24 secondary-level hospitals and nine tertiary-level hospitals and all facilities included are publicly owned. These hospitals represent almost all gynecological and maternity inpatient care.
Each episode of care related to diseases and disorders of the female reproductive system was grouped into its proper AR-DRG group based on the main reason for the patient's admission, and as a consequence, changes in acute patient admission before and during the COVID-19 pandemic were noticed. Because the data utilized in this study were anonymized and made available as public information from CHIF and the CIPH, we did not require informed consent or ethical approval.
Data and statistical analysis
The average number of inpatient cases was calculated for 3 years (2017–2019) before the pandemic and 3 years (2020–2022) during the period of the pandemic. We used DRG data grouped in MDC 13 and MDC 14 in order to determine the extent to which, and for which conditions the onset of pandemic altered the pre COVID-19 hospital activity across the hospital network. The hospital admission incidence rates were calculated by dividing the average number of cases during each period (2017–2019 for pre-pandemic years and 2020–2022 for pandemic years) by the average total population of Croatia during the respective periods. The reason why we used the average total population as denominator is related to the fact that DRG data base includes 96% of the country's inpatent activity and this was consistent during the study timeframe periods. The consistency in female population data across both time periods (51.8%) based on the Croatian Bureau of Statistics ensures comparability of the calculated incidence rates.
The hospital admission incidence rate was then determined by dividing the average number of cases during a certain period by the average total population (2017–2019 and 2020–2022). To compare the incidence rates of events (hospital admissions) occurring in pre-pandemic and pandemic period, the incidence rate ratio (IRR) was used as a relative difference measure. The incidence rate ratio (IRR) was calculated as a ratio of the incidence rate for 2020–2022 to that for 2017–2019 for each analyzed DRGs that belongs to MDC 13 and 14. Using the 2-by-2 Chi-square test, the incidence rate between the two time periods was compared.
The Wald technique was used to construct the 95% confidence intervals based on an investigation of whether the IRR was equal to one (i.e., the admission incidence rate in 2020–2022 being equal to that in 2017–2019). Microsoft Excel was used to calculate average values and rate change while every statistical analysis was carried out using R (R Core Team, Austria) (23). No adjustments for seasonal effects and autocorellation were needed as data were compared by calendar year (6 years in total) and therefore a constant variance was assumed. A p-value of 0.05 or less was considered statistically significant (two-tailed).
Results
The average number of gynecological patients in all hospitals during the pandemic (2020–2022) was 62,257 of which 34,987 (56.2%) were treated at the tertiary healthcare level, compared to pre-pandemic (2017–2019) when the average number of patients in all hospitals was 71,519 of which 40,827 (57.09%) were treated at the tertiary healthcare level. The rate change is −15.5%, similar for both health care levels (−17.5%, −12.5%, p < 0.0001, respectively).
Among all patients during the pandemic years, 27,540 (44.24%) of them were treated surgically. 15,773 (57.27%) were treated surgically at the tertiary healthcare level. Compared to pre-pandemic years, 31,578 (44.15%) patients were treated surgically. Among them, 18,793 (59.51%) were treated at the tertiary healthcare level.
During the pandemic, there were 14,110 patients treated surgically because of conditions related to pregnancy, childbirth, and puerperium. Compared to the pre-pandemic period, there is an average drop of 6.64%, when the total number of patients was 15,113. During the pandemic, 7,887 (55.9%) patients were surgically treated at the tertiary healthcare level, and 6,223 (44.1%) at the secondary. The number of patients dropped by 19% at the tertiary and by 3% at the secondary health care level.
The decrease greater than average is related to all subcategories in this group, except O03Z in which a decrease of 1% was observed (p = 0.953463), and O01B and O01C where an increase of 3% and 10% were observed (p = 0.443471, p < 0.0001, respectively).
Table 1 compares the average number of total surgical admissions during the pre-pandemic (2017–2019) and pandemic years (2020–2022) related to pregnancy, childbirth, and the puerperium.
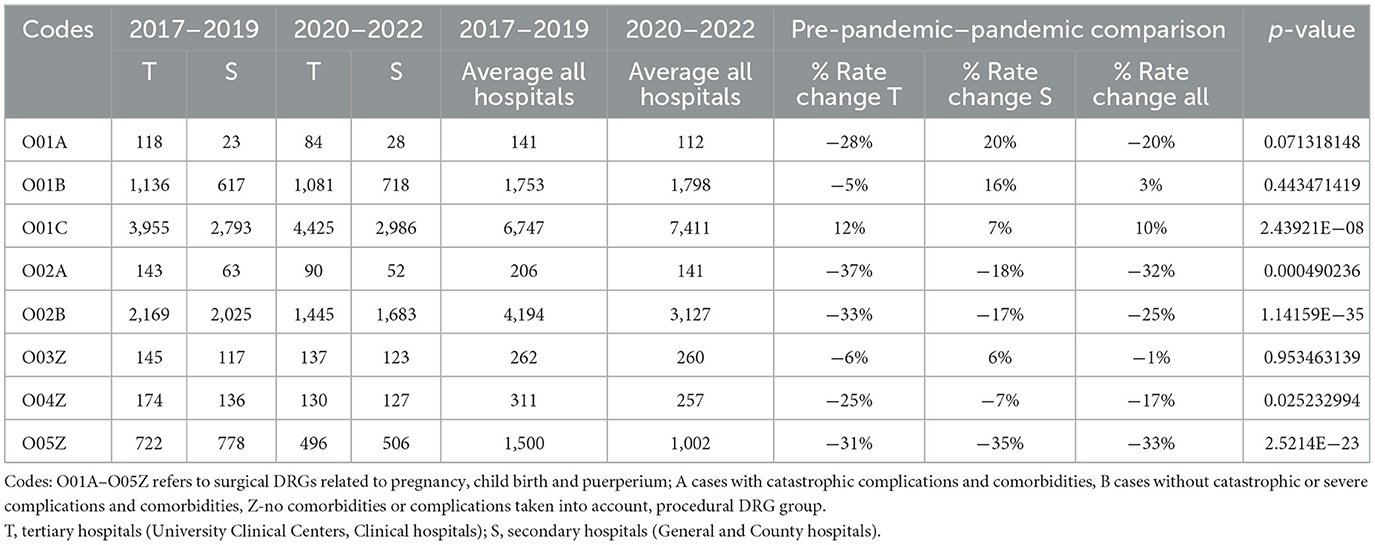
Table 1. Comparison of surgical DRGs related to pregnancy, childbirth, and the puerperium done during pre-pandemic (2017–2019) and pandemic (2020–2022).
The gynecological patients were treated surgically and conservatively at both healthcare levels. Based on AR-DRG structure, surgical cases are presented with the following ARDRG groups: N01Z-N11B, O01A-O05Z, and patients treated conservatively with groups N60A-N62B, O60A-O66B.
Figure 1 shows the corresponding IRRs calculated for surgical DRGs associated with pregnancy, childbirth, and the puerperium.

Figure 1. Incidence rate ratio (IRR) for surgical DRGs (O01A–O05Z) associated with pregnancy, childbirth, and the puerperium during the pandemic (2020–2022) compared to pre-pandemic (2017–2019); incidence rate ratio with 95% confidence limits.
During the pandemic, there were 32,191 patients treated non-surgically because of conditions related to pregnancy, childbirth, and puerperium. Compared to the pre-pandemic period, there is an average drop of 10.56% when the total number of patients was 35,991. During the pandemic, 17,781 (55.23%) patients were non-surgically treated at the tertiary health care level, and 14,409 (44.76%) at the secondary. The number of patients dropped by 17% at the tertiary and by 11.68% at the secondary health care level.
The decrease greater than average is related to all subcategories in this group, except O66B in which a decrease of 9% was observed (p = 0.450941), and O60C and O63Z where an increase of 32% and 52% were observed (p = < 0.0001).
Table 2 compares the average number of total non-surgical admissions during the pre-pandemic (2017–2019) and pandemic years (2020–2022) related to pregnancy, childbirth, and puerperium.
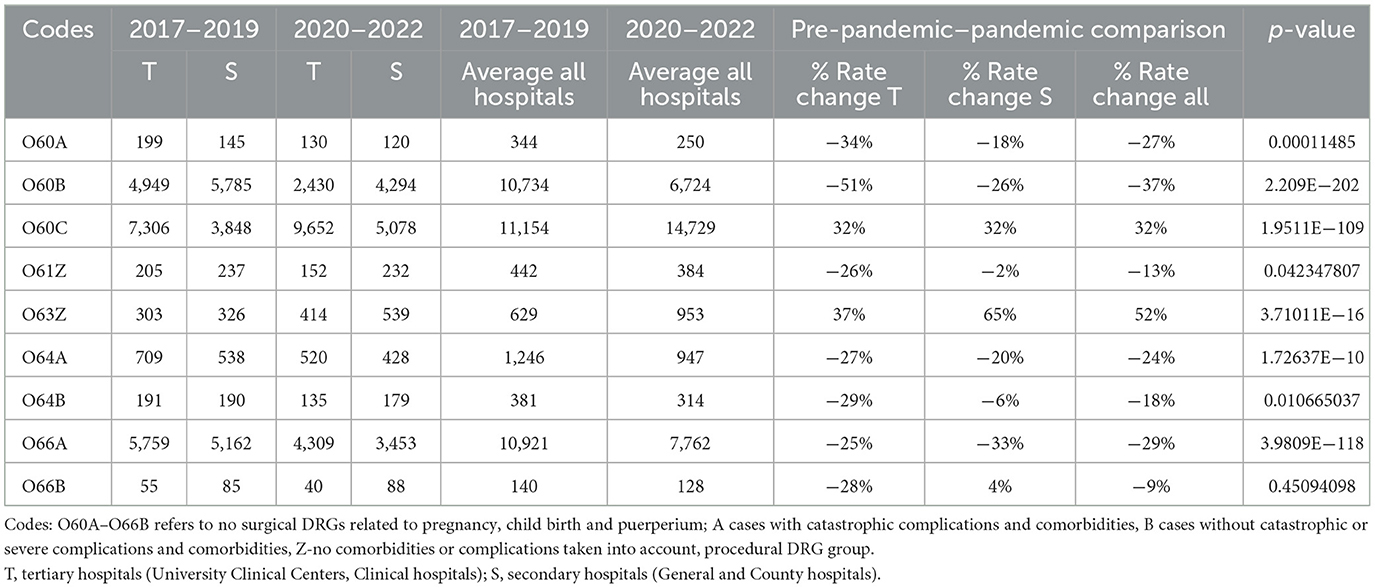
Table 2. Comparison of non-surgical DRGs related to pregnancy, childbirth, and the puerperium done during pre-pandemic (2017–2019) and pandemic (2020–2022).
Figure 2 shows the corresponding IRRs calculated for non-surgical DRGs (O60A-O66B) associated with pregnancy, childbirth, and the puerperium.
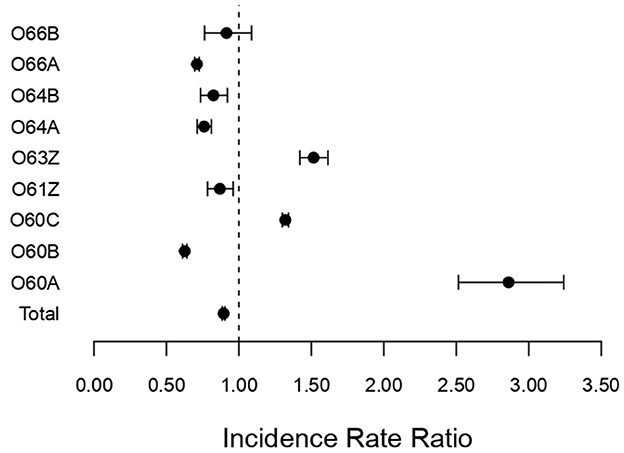
Figure 2. Incidence rate ratio (IRR) for non-surgical DRGs (O60A–O66B) associated with pregnancy, childbirth, and the puerperium during the pandemic (2020–2022) compared to pre-pandemic (2017–2019); incidence rate ratio with 95% confidence limits.
During the pandemic, there were 13,430 patients treated surgically because of diseases and disorders of the female reproductive system. Compared to the pre-pandemic period, there is an average drop of 18.43% when the total number of patients was 16,465. During the pandemic, 7,886 (58.72%) patients were surgically treated at the tertiary health care level, and 5,545 (41.28%) at the secondary. The number of patients dropped by 16% at the tertiary and by 11% at the secondary health care level.
The decrease greater than average is related to N02A by 19% (p = 0.138546), N04Z by 19% (p < 0.0001), N03A by 31% (p = 0.034861), N07Z by 24% (p < 0.0001), N09Z by 26% (p < 0.0001), N10Z by 20% (p < 0.0001), N11B by 21% (p = 0.002066). An increase of 1% and 4% was observed in groups N02B and N01Z (p = 0.793676, p = 0.718742, respectively).
Table 3 compares the average number of total surgical DRGs (N01Z-N11B) during the pre-pandemic (2017–2019) and pandemic years (2020–2022) related to diseases and disorders of the female reproductive system.
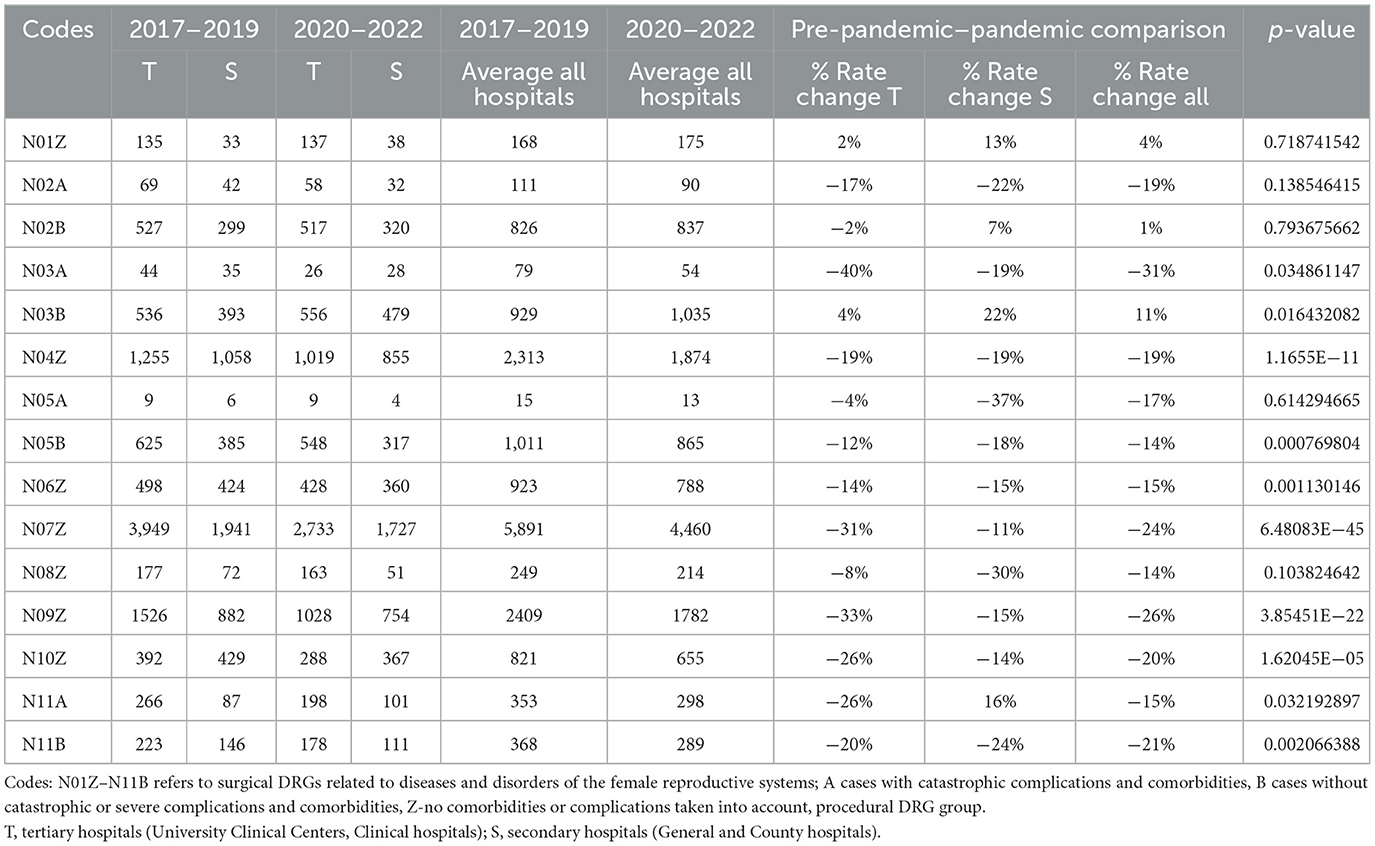
Table 3. Comparison of surgical DRGs (N01Z-N11B) related to diseases and disorders of the female reproductive system done during pre-pandemic (2017–2019) and pandemic (2020–2022).
Figure 3 shows the corresponding IRRs calculated for surgically treated diseases and disorders of the female reproductive system.
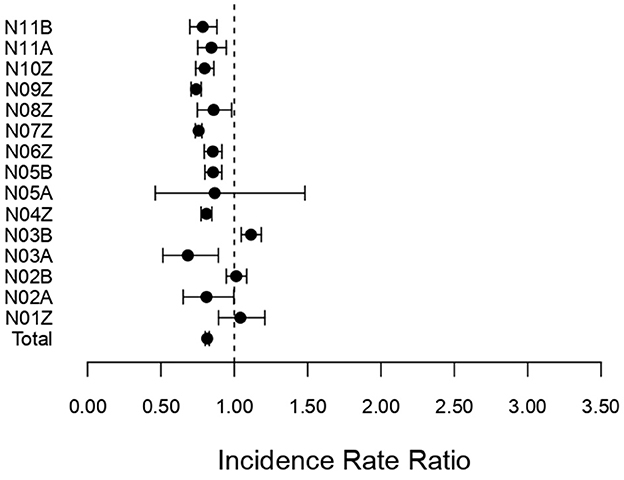
Figure 3. Incidence rate ratio (IRR) for surgical DRGs (N01Z–N11Z) associated with diseases and disorders of the female reproductive system during the pandemic (2020–2022) compared to pre-pandemic (2017–2019). Incidence rate ratio with 95% confidence limits.
During the pandemic, there were 2,523 patients treated non-surgically because of diseases and disorders of the female reproductive system. Compared to the pre-pandemic period, there is an average drop of 35.06% when the total number of patients was 3,885. During the pandemic, 1,433 (56.8%) patients were non-surgically treated at the tertiary healthcare level, compared to 1,090 (43.2%) patients at the secondary. The number of patients dropped by 35% at the tertiary and by 21% at the secondary health care level.
A decrease greater than average is observed in groups N62A by 41% (p = 0.006157) and N62B by 40% (p < 0.0001). The decrease lower than average is noticed in groups N60A by 14 % (p = 0.235858), N60B by 34% (p < 0.0001), and N61Z by 21 % (p = 0.015565).
Table 4 compares the average number of total non-surgical admissions during the pre-pandemic (2017–2019) and pandemic years (2020–2022) related to diseases and disorders of the female reproductive system.
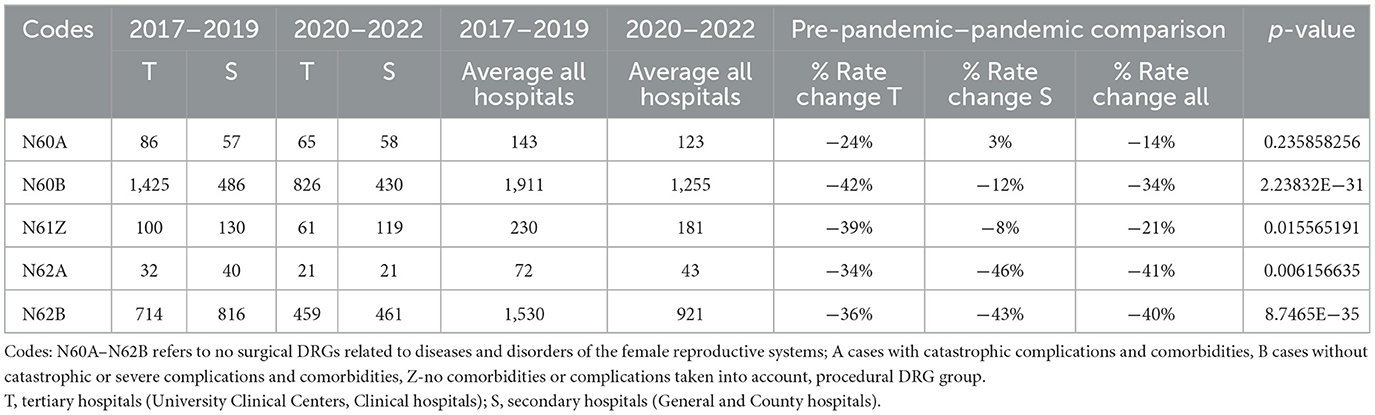
Table 4. Comparison of non-surgical DRGs (N60A-N62B) related to diseases and disorders of the female reproductive system done during pre-pandemic (2017–2019) and pandemic (2020–2022).
Figure 4 shows the corresponding IRRs calculated for non-surgically treated diseases and disorders of the female reproductive system.
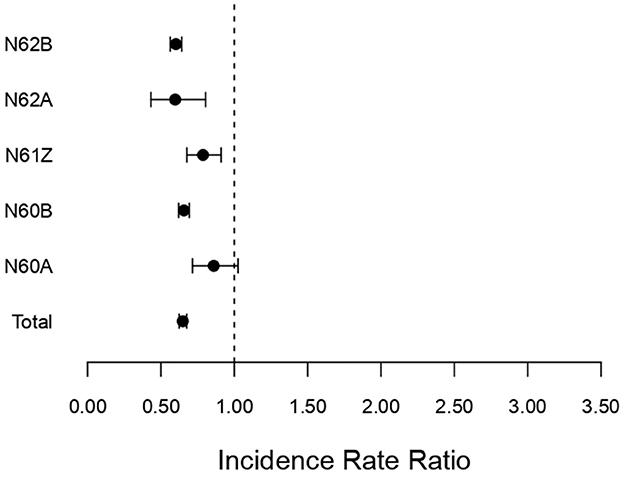
Figure 4. Incidence rate ratio (IRR) for non-surgical (N60A–N62B) associated with diseases and disorders of the female reproductive system during the pandemic (2020–2022) compared to pre-pandemic (2017–2019). Incidence rate ratio with 95% confidence limits.
Discussion
During the pandemic period in Croatia, a significant average decrease was noted across acute cases classified by DRGs. Specifically, there was a 6.64% decrease in surgically treated patients with conditions related to pregnancy, childbirth, and the puerperium, and there was a 10.56% decrease in non-surgically treated patients within the same categories.
DRG data also showed that the COVID-19 period also witnessed a significant decrease in cases related to disorders of the female reproductive system. The decrease was 18.43% for surgically treated patients and 35.06% for non-surgically treated patients.
The first COVID-19 case in Croatia was confirmed on February 25, 2020. Three weeks later, hospital care delivery was reorganized to address the growing demands of the pandemic following a significant increase in COVID-19 cases.
In Zagreb, the capital of Croatia, three hospitals were designated as COVID-19 centers, and patients with illnesses associated with the COVID-19 who require inpatient care have been admitted there. The majority of hospitals established COVID-19 isolation units, and four comparable facilities have been established around the region (24).
In addition to the reorganization of the healthcare delivery system, tougher lockdown rules were applied in 2020. Hospitals' lower priority for elective treatments, a fall in the non-emergency admission referral rate due to fewer outpatient hours, and a shortage of hospital staff are all contributing causes. Another concern is the possibility of contracting COVID-19 in a hospital environment (25).
Furthermore, Zagreb suffered a further catastrophe in March 2020: a catastrophic earthquake that devastated some hospitals and gynecology departments.
By comparison internationally, Carbone et al. (26). in Italy conducted a review and meta-analysis and they found that during the lockdown periods, the pooled proportion of hospitalizations for any obstetrical or gynecological condition increased from 22.7 to 30.6%, with delivery increasing from 48.0 to 53.9%. In particular, they discovered that the pooled proportion of pregnant women suffering from hypertensive disorders rose (2.6% vs. 1.2%), as did women experiencing imminent labor (52% vs. 43%) and early rupture of membranes (12.0% vs. 9.1%). In contrast, they discovered reductions in the proportion of women with pelvic discomfort (12.4% vs. 14.4%), suspected ectopic pregnancy (1.8% vs. 2.0%), diminished fetal movements (3.0% vs. 3.3%), and vaginal bleeding for both obstetrical (11.7% vs. 12.8%) and gynecological (7.4% vs. 9.2%) issues (26).
Another study, similar in design, examined the characteristics and outcomes of patients undergoing elective laparoscopic cholecystectomy for benign gallbladder disease in a single secondary care hospital in the UK before the COVID-19 pandemic and during the recovery phase of the pandemic (27). The authors also observed a significant delay in elective procedures due to fear of COVID-19 and hospital reorganization. Thus, a significantly lower proportion of patients underwent total cholecystectomy during the recovery phase of the pandemic (n = 49; 92.5%) compared to patients who underwent surgery before the pandemic (n = 106; 99.1%; p = 0.04) (27). In addition, another retrospective epidemiologic cohort study of a single level I trauma center in northern Italy found that overall orthopedic surgical activity decreased by 72.4% during the lockdown period (from 36 ± 6.1 to 10.7 ± 8.4 per week; p < 0.01), with the ratio of emergency to elective surgery increasing from 0.7:1 in 2019 to 3.3:1 in 2020 (28). In addition, elective surgery was almost completely suspended and was affected with a decrease of 88.9%, while emergency trauma surgery suffered a decrease of 49.7%.
During the lockdown time at the tertiary hospital level in southern Italy, it was also noticed that, similar to the Croatian pattern, there was an overall decline in the number of obstetric and gynecologist emergency visits (29). Furthermore, pregnant women declined to undergo prenatal invasive diagnostic procedures, even though the number of births remained constant and even increased during the lockdown, demonstrating that women came to the hospital when they had no other choices (14).
Carbone et al. observed a rise in hospitalizations as well, particularly for pregnancy-related hypertension problems and labor signs. Given that contractions and vaginal discharge are among the most common reasons for seeking emergency care, the discovery of increased hospitalizations for these conditions during the lockdown could be interpreted as evidence of a reduction in the number of unnecessary visits for unclear conditions, which were the cause of emergency unit overload. As a result, it appeared that people only sought medical assistance when they had true, specific labor signs and a genuine need. The studies that examined this topic found an increase in hypertensive disorders, and although this hasn't been proven, it may be due to the more sedentary lifestyle that was forced upon people during the lockdown, as well as the eventual reduction in antenatal care appointments, which resulted in missed antenatal screenings (26).
During the COVID-19 pandemic, a significant decrease in gynecologic procedures and ambulatory obstetrical and gynecologic visits at two big health systems in United States of America was observed. The decrease in surgical volume was notably noticeable from April 5 to June 27, 2020. During this time, the most stringent institutional and regional regulations were in place, preventing or severely limiting elective surgery. Despite a rise in surgery volume in the second part of the year, surgical caseload for 2020 did not return to pre-pandemic levels. Similarly, early in the pandemic, ambulatory care decreased significantly, and quantities of various forms of ambulatory care did not return to 2019 levels (30). During this public health crisis, gynecologic surgical techniques were most likely impacted by published professional society guidelines for changing surgical practice during the COVID-19 pandemic (31, 32).
Concerns have been raised in cancer, gynecologic, and obstetric literature concerning the possible unfavorable health effects linked with deferred or delayed care. Deferred or delayed treatment has been linked to more advanced breast and cervical cancers at the time of diagnosis (33). The impact of COVID-19 on breast and colon cancer screening and diagnosis over the next decade predict a 1% increase in cancer mortality (34). Furthermore, while sexual distance may initially result in a reduction in diagnosis of sexually transmitted illnesses during the pandemic, restricted access to testing and treatment is predicted to result in a subsequent rise in the rates of diagnosed sexually transmitted infections (35).
In the context of the COVID-19 outbreak, rapidly growing modern technologies have brought with them tremendous potential for many applications that will change the way we work, learn and live globally. Among them, healthcare is one such specific industry that is undergoing an interesting transformation with the integration of these telecommunication technologies. Several publications have hinted at the development and implementation of different variants of telemedicine during the COVID-19 outbreak, with the aim of offsetting the decline in hospital visits, especially for non-surgical cases (36–39). The most important examples are: telemedicine in emergency cases and triage, telemedicine in critical care, telemedicine-assisted follow-up and rehabilitation, telemedicine in palliative care and general telemedicine for elderly (36–39). Different modalities and use of telehealth technologies in the prenatal and postpartum periods during COVID-19 pandemic undoubtedly proved that integration of telehealth into maternity care is needed. The potential to reduce disparities in care and clinical outcomes should be further harnessed by step wise implementation based on the well designed policy and stakeholders engagement.
Strengths and limitations
The use of a full data set on inpatient activity for all gynecology departments in Croatia is the study's principal strength. We also discussed how the SARS-CoV-2 pandemic directly affected the number of patients with gynecological illnesses who were admitted to hospitals, as well as the number of patients who had surgery and received non-surgical care at the secondary and tertiary levels of care. However, there are some limitations to our analysis. DRG data lack detailed, granular information on potentially significant variables or confounders, such as patient age and co-morbidities. Instead, they offer large-scale, descriptive insights into the utilization of gynecology department services. Furthermore, DRG reporting in Croatia is mandatory only for hospitals contracted by the Croatian Health Insurance Fund. As a result, we were unable to include maternity data from one private hospital. However, this facility reports only ~500 inpatient maternity cases annually, and their exclusion is unlikely to significantly impact the reported results.
Finally, the study design employs a cross-sectional design, which captures data at specific points in time or aggregated over fixed periods. While this approach allows for the analysis of associations between variables (e.g. the impact of COVID-19 pandemic on gynecological and obstetric admissions), it is inherently limited in its ability to establish definitive causal relationships. The primary limitation of cross sectional studies in this regard is their inability to track temporal sequences. To improve causal inference, future research could consider longitudinal cohort studies but aggregated, publicly available DRG data can not be used for a such purpose.
Conclusion
This is the first research that, to our knowledge, demonstrates how the COVID-19 pandemic has affected inpatient treatment for patients in Croatia who have gynecological issues associated to pregnancy, delivery, and the puerperium as well as illnesses and abnormalities of the female reproductive system. At secondary and tertiary hospital levels, we noticed a statistically significant average decline in the overall number of admissions as well as the number of gynecological patients who were admitted to the hospital. In future pandemic scenarios, it will be important for obstetrics and gynecology practitioners to develop innovative strategies to maintain or improve patient access to care while ensuring stringent safety measures to prevent infection transmission among patients and healthcare personnel.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the [patients/ participants OR patients/participants legal guardian/next of kin] was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
KK: Writing – review & editing, Conceptualization, Formal analysis. MM: Conceptualization, Writing – original draft. MP: Investigation, Methodology, Writing – review & editing. AO: Formal analysis, Methodology, Writing – review & editing. RM: Supervision, Writing – review & editing. StO: Investigation, Writing – review & editing. SlO: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^MDC 13 AR-DRG groups related to diseases and disorders of female reproductive system: N01Z Pelvic Evisceration and Radical Vulvectomy; N02AUterine, Adnexa Procedure for Ovarian or Adnexal Malignancy W CC N02B Uterine, Adnexa Procedure for Ovarian or Adnexal Malignancy W/O CC N03A Uterine, Adnexa Procedure for Non-Ovarian or Adnexal Malignancy W CC N03B Uterine, Adnexa Procedure for Non-Ovarian or Adnexal Malignancy W/O CC N04ZHysterectomy for Non-Malignancy N05A Oophorectomies and Complex Fallopian Tube Procs for Non-Malig W Cat or Sev CC N05B Oophorectomies and Complex Fallopian Tube Procs for Non-Malig W/O Cat or Sev CCN06Z Female Reproductive System Reconstructive ProceduresN07Z Other Uterine and Adnexa Procedures for Non-Malignancy N08ZEndoscopic and Laparoscopic Procedures for Female Reproductive System N09Z Conisation, Vagina, Cervix and Vulva Procedures N10ZDiagnostic Curettage or Diagnostic Hysteroscopy N11A Other Female Reproductive System OR Procs Age >64 or W Malignancy or W CC N11B Other Female Reproductive System OR Procs Age < 65 W/O Malignancy W/O CC N60AMalignancy, Female Reproductive System W Catastrophic or Severe CC N60BMalignancy, Female Reproductive System W/O Catastrophic or Severe CC N61ZInfections, Female Reproductive System N62AMenstrual and Other Female Reproductive System Disorders W CC N62B Menstrual and Other Female Reproductive System Disorders W/O CC.
2. ^MDC 14 AR-DRG groups related to pregnancy, childbirth and puerperium O01ACaesarean Delivery W Catastrophic CC O01BCaesarean Delivery W Severe CC O01CCaesarean Deliver W/ Catastrophic or Severe CC O02AVaginal Delivery W OR Procedure W Catastrophic or Severe CC O02BVaginal Delivery W OR Procedure W/O Catastrophic or Severe CC O03ZEctopic Pregnancy O04Z Postpartum and Post Abortion W OR Procedure O05Z Abortion W OR Procedure O60AVaginal Delivery W Catastrophic or Severe CC O60B Vaginal Delivery W/O Catastrophic or Severe CC O60C Vaginal Delivery Single Uncomplicated W/O Other Condition O61Z Postpartum and Post Abortion W/O OR Procedure O63Z Abortion W/O OR Procedure O64A False Labour Before 37 Weeks or W Catastrophic CC O64B False Labour After 37 Weeks W/O Catastrophic CC O66AAntenatal and Other Obstetric Admission O66B Antenatal and Other Obstetric Admission, Sameday.
References
1. Jardine J, Relph S, Magee LA, von Dadelszen P, Morris E, Ross-Davie M, et al. Maternity services in the UK during the coronavirus disease 2019 pandemic: a national survey of modifications to standard care. BJOG. (2021) 128:880–9. doi: 10.1111/1471-0528.16547
2. Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. (2020) 222:415–26. doi: 10.1016/j.ajog.2020.02.017
3. Carbone IF, Conforti A, Farina A, Alviggi C. A practical approach for the management of obstetric and infertile women during the phase two of the novel coronavirus disease 2019 (COVID−19) pandemic. Eur J Obstet Gynecol Reprod Biol. (2020) 251:266–7. doi: 10.1016/j.ejogrb.2020.06.006
4. Flaxman S, Mishra S, Gandy A, Unwin HJT, Mellan TA, Coupland H, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. (2020) 584:257–61. doi: 10.1038/s41586-020-2405-7
5. Hsieh Y, Yen C, Wu C, Wang P. Nonattendance at scheduled appointments in outpatient clinics due to COVID-19 and related factors in Taiwan: a health belief model approach. Int J Environ Res Public Health. (2021) 18:4445. doi: 10.3390/ijerph18094445
6. Halatoko WA, Konu YR, Gbeasor-Komlanvi FA, Sadio AJ, Tchankoni MK, Komlanvi KS, et al. Prevalence of SARS-CoV-2 among high-risk populations in Lomé (Togo) in 2020. PLoS ONE. (2020) 15:e0242124. doi: 10.1371/journal.pone.0242124
7. WHO Group Consultation on Health Telematics (1997: Geneva Switzerland). A Health Telematics Policy in Support of WHO's Health-for-All Strategy for Global Health Development : Report of the WHO Group Consultation on Health Telematics, 11-16 December, Geneva, 1997. World Health Organization (1998). Available at: https://apps.who.int/iris/handle/10665/63857 (accessed February 22, 2023).
8. Hertling S, Hertling D, Loos F, Martin D, Graul I. Digitization in gynecology and obstetrics in times of COVID-19: results of a national survey. Internet Interv. (2021) 26:100478. doi: 10.1016/j.invent.2021.100478
9. Pullano G, Di Domenico L, Sabbatini CE, Valdano E, Turbelin C, Debin M, et al. Underdetection of cases of COVID-19 in France threatens epidemic control. Nature. (2021) 590:134–9. doi: 10.1038/s41586-020-03095-6
10. Kulcsar Z, Albert D, Ercolano E, Mecchella JN. Telerheumatology: a technology appropriate for virtually all. Semin Arthritis Rheum. (2016) 46:380–5. doi: 10.1016/j.semarthrit.2016.05.013
11. Menage J. Why telemedicine diminishes the doctor-patient relationship. BMJ. (2020) 371:m4348. doi: 10.1136/bmj.m4348
12. Putra M, Kesavan M, Brackney K, Hackney DN, Roosa KM. Forecasting the impact of coronavirus disease during delivery hospitalization: an aid for resource utilization. Am J Obstet Gynecol MFM. (2020) 2:100127. doi: 10.1016/j.ajogmf.2020.100127
13. Oakes MC, Kernberg AS, Carter EB, Foeller ME, Palanisamy A, Raghuraman N, et al. Pregnancy as a risk factor for severe coronavirus disease 2019 using standardized clinical criteria. Am J Obstet Gynecol MFM. (2021) 3:100319. doi: 10.1016/j.ajogmf.2021.100319
14. Carbone L, Raffone A, Sarno L, Travaglino A, Saccone G, Gabrielli O, et al. Invasive prenatal diagnosis during COVID-19 pandemic. Arch Gynecol Obstet. (2022) 305:797–801. doi: 10.1007/s00404-021-06276-4
15. WAPM (World Association of Perinatal Medicine) Working Group on COVID-19. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection. Ultrasound Obstet Gynecol. (2021) 57:232–41. doi: 10.1002/uog.23107
16. Di Girolamo R, Khalil A, Alameddine S, D'Angelo E, Galliani C, Matarrelli B, et al. Placental histopathology after SARS-CoV-2 infection in pregnancy: a systematic review and meta-analysis. Am J Obstet Gynecol MFM. (2021) 3:100468. doi: 10.1016/j.ajogmf.2021.100468
17. Vega M, Hughes F, Bernstein PS, Goffman D, Sheen JJ, Aubey JJ, et al. From the trenches: inpatient management of coronavirus disease 2019 in pregnancy. Am J Obstet Gynecol MFM. (2020) 2:100154. doi: 10.1016/j.ajogmf.2020.100154
18. Pierce-Williams RAM, Burd J, Felder L, Khoury R, Bernstein PS, Avila K, et al. Clinical course of severe and critical coronavirus disease 2019 in hospitalized pregnancies: a United States cohort study. Am J Obstet Gynecol MFM. (2020) 2:100134. doi: 10.1016/j.ajogmf.2020.100134
19. Di Mascio D, Buca D, Berghella V, Khalil A, Rizzo G, Odibo A, et al. Counseling in maternal-fetal medicine: SARS-CoV-2 infection in pregnancy. Ultrasound Obstet Gynecol. (2021) 57:687–97. doi: 10.1002/uog.23628
20. Dijagnostičko Terapijske Skupine (DTS) u hrvatskom bolničkom sustavu. Available at: http://www.cezih.hr/dts_rezultati_i_novosti.html (accessed February 22, 2023).
21. IHACPA. Available at: https://www.ihacpa.gov.au/ (accessed February 22, 2023).
22. Duckett SJ. The development of Australian refined diagnosis related groups: the Australian inpatient casemix classification. Casemix. (2000) 2:115–20.
23. R Core Team. European Environment Agency. (2020). Available at: https://www.eea.europa.eu/data-and-maps/indicators/oxygen-consuming-substances-in-rivers/r-development-core-team-2006 (accessed February 22, 2023).
24. Vlada Republike Hrvatske - 27. sjednica Vlade Republike Hrvatske. Available at: https://vlada.gov.hr/sjednice/27-sjednica-vladerepublike-hrvatske-30995/30995 (accessed March 28, 2023).
25. Kalanj K, Marshall R, Karol K, Tiljak MK, Orešković S. The impact of COVID-19 on hospital admissions in Croatia. Front Public Health. (2021) 9:720948. doi: 10.3389/fpubh.2021.720948
26. Carbone L, Raffone A, Travaglino A, Saccone G, Di Girolamo R, Neola D, et al. The impact of COVID-19 pandemic on obstetrics and gynecology hospitalization rate and on reasons for seeking emergency care: a systematic review and meta-analysis. J Matern-Fetal Neonatal Med. (2023) 36:2187254. doi: 10.1080/14767058.2023.2187254
27. Demetriou G, Wanigasooriya K, Elmaradny A, Al-Najjar A, Rauf M, Martin-Jones A, et al. The impact of the COVID-19 pandemic on elective laparoscopic cholecystectomy: a retrospective Cohort study. Front Surg. (2022) 9:990533. doi: 10.3389/fsurg.2022.990533
28. Turati M, Gatti S, Rigamonti L, Zatti G, Munegato D, Crippa M, et al. Impact of COVID-19 lock-down period on orthopedic and trauma surgical activity in a northern Italian hospital. Front Med. (2024) 11:1454863. doi: 10.3389/fmed.2024.1454863
29. Carbone L, Raffone A, Travaglino A, Sarno L, Conforti A, Gabrielli O, et al. Obstetric A&E unit admission and hospitalization for obstetrical management during COVID-19 pandemic in a third-level hospital of southern Italy. Arch Gynecol Obstet. (2022) 305:859–67. doi: 10.1007/s00404-021-06212-6
30. Liang AL, Turner LC, Voegtline KM, Olson SB, Wildey B, Handa VL. Impact of COVID-19 on gynecologic and obstetrical services at two large health systems. PLoS ONE. (2022) 17:e0269852. doi: 10.1371/journal.pone.0269852
31. COVID-19: Recommendations for Management of Elective Surgical Procedures. ACS. Available at: https://www.facs.org/for-medical-professionals/covid-19/clinical-guidance/elective-surgery/ (accessed May 25, 2023).
32. Borahay MA, Wethington SL, Wang KC, Christianson MS, Martin S, Lawson SM, et al. Patient-centered, gynecology-specific prioritization of nonurgent surgeries during the COVID-19 pandemic: proposal of a novel scoring system. J Minim Invasive Gynecol. (2020) 27:1429–33. doi: 10.1016/j.jmig.2020.05.026
33. Bonadio RC, Messias AP, Moreira OA, Leis LV, Orsi BZ, Testa L, et al. Impact of the COVID-19 pandemic on breast and cervical cancer stage at diagnosis in Brazil. Ecancermedicalscience. (2021) 15:1299. doi: 10.3332/ecancer.2021.1299
35. Tam MW, Davis VH, Ahluwalia M, Lee RS, Ross LE. Impact of COVID-19 on access to and delivery of sexual and reproductive healthcare services in countries with universal healthcare systems: a systematic review. PLoS ONE. (2024) 19:e0294744. doi: 10.1371/journal.pone.0294744
36. Shen Y-T, Chen L, Yue W-W, Xu H-X. Digital technology-based telemedicine for the COVID-19 pandemic. Front Med. (2021) 8:646506. doi: 10.3389/fmed.2021.646506
37. Bhaskar S, Bradley S, Chattu VK, Adisesh A, Nurtazina A, Kyrykbayeva S, et al. Telemedicine as the new outpatient clinic gone digital: position paper from the pandemic health system REsilience PROGRAM (REPROGRAM) international consortium (part 2). Front Public Health. (2020) 8:410. doi: 10.3389/fpubh.2020.00410
38. Atkinson J, Hastie R, Walker S, Lindquist A, Tong S. Telehealth in antenatal care: recent insights and advances. BMC Med. (2023) 21:332. doi: 10.1186/s12916-023-03042-y
Keywords: AR-DRG, COVID-19, data transparency, gynecology, health system response, inpatient care, obstetrics, pandemic
Citation: Kalanj K, Mikuš M, Peček M, Orbanić A, Marshall R, Orešković S and Orešković S (2025) A comparative cross-sectional study of the impact of COVID-19 pandemic on obstetrics and gynecology admissions in Croatia. Front. Med. 12:1505387. doi: 10.3389/fmed.2025.1505387
Received: 04 October 2024; Accepted: 24 January 2025;
Published: 14 February 2025.
Edited by:
Raigam Jafet Martinez-Portilla, Instituto Nacional de Perinatología (INPER), MexicoReviewed by:
Cesar Gil Armas, Scientific University of the South, PeruRodolfo Antonio Gurrola Ochoa, Autonomous University of Sinaloa, Mexico
Copyright © 2025 Kalanj, Mikuš, Peček, Orbanić, Marshall, Orešković and Orešković. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Karolina Kalanj, a2Fyb2xpbmEua2FsYW5qQHpnLnQtY29tLmhy
†These authors have contributed equally to this work
 Karolina Kalanj
Karolina Kalanj Mislav Mikuš
Mislav Mikuš Mirta Peček
Mirta Peček Ante Orbanić
Ante Orbanić Rick Marshall
Rick Marshall Stjepan Orešković
Stjepan Orešković Slavko Orešković2,6
Slavko Orešković2,6